Abstract
Loneliness is a common condition in older adults and is associated with increased morbidity and mortality, decreased sleep quality, and increased risk of cognitive decline. Assessing loneliness in older adults is challenging due to the negative desirability biases associated with being lonely. Thus, it is necessary to develop more objective techniques to assess loneliness in older adults. In this paper, we describe a system to measure loneliness by assessing in-home behavior using wireless motion and contact sensors, phone monitors, and computer software as well as algorithms developed to assess key behaviors of interest. We then present results showing the accuracy of the system in detecting loneliness in a longitudinal study of 16 older adults who agreed to have the sensor platform installed in their own homes for up to 8 months. We show that loneliness is significantly associated with both time out-of-home ( and
and  ) and number of computer sessions (
) and number of computer sessions ( and
and  ).
).  for the model was 0.35. We also show the model’s ability to predict out-of-sample loneliness, demonstrating that the correlation between true loneliness and predicted out-of-sample loneliness is 0.48. When compared with the University of California at Los Angeles loneliness score, the normalized mean absolute error of the predicted loneliness scores was 0.81 and the normalized root mean squared error was 0.91. These results represent first steps toward an unobtrusive, objective method for the prediction of loneliness among older adults, and mark the first time multiple objective behavioral measures that have been related to this key health outcome.
for the model was 0.35. We also show the model’s ability to predict out-of-sample loneliness, demonstrating that the correlation between true loneliness and predicted out-of-sample loneliness is 0.48. When compared with the University of California at Los Angeles loneliness score, the normalized mean absolute error of the predicted loneliness scores was 0.81 and the normalized root mean squared error was 0.91. These results represent first steps toward an unobtrusive, objective method for the prediction of loneliness among older adults, and mark the first time multiple objective behavioral measures that have been related to this key health outcome.
Keywords: In-home monitoring, loneliness, longitudinal models, ambient assessment, older adults
In this paper, we describe an in-home sensor platform that detects daily behaviors such as detailed computer use, total hours spent outside the home, in-home walking speed, and total sleep time. We use this system to relate in-home behavior to loneliness, and show that loneliness (as measured using the 20-item UCLA loneliness scale) is closely related to in-home behavior (R₂
I. Introduction
Loneliness is a painful and debilitating state typically arising due to a perceived deficit in social relationships [1]–[3]. Loneliness may be situationally induced (state loneliness) but can also be a chronic condition [4]. Among older adults in particular, the experience of loneliness can be especially traumatic, giving rise to numerous negative health outcomes including increased morbidity and mortality [5], reduced sleep quality [6], increased daytime dysfunction [7], and increased rates of cognitive decline [8]. The problem of loneliness among older adults is especially challenging as the number of persons over the age of 65 is expected to nearly double between 2012 and 2035 [9]. Thus, detection and mitigation of loneliness in older adults is critical as the deleterious effects of loneliness can be reversed with an appropriate intervention [10].
Identifying lonely individuals is critical to mitigating loneliness among older adults, yet the detection of loneliness can be challenging. While direct self-report methods may be used to assess loneliness using the self-labeling approach [11], people may avoid reporting loneliness even when they are lonely due to the numerous social stigmas associated with being lonely. For this reason, several scales have been developed to indirectly assess loneliness levels [12], [13]. While these scales may overcome the negative stigmas associated with being lonely, they still depend on episodic self-report which is subject to desirability bias [14], [15], memory problems [16], and under or over estimation [17]. Thus, the development of an objective and continuous method to assess loneliness in older adults may enable identification of loneliness as it occurs, thereby assisting in the mitigation of loneliness at the earliest possible stages. An objective model of loneliness would allow for more precise inferences regarding the impact of loneliness on health while enhancing our understanding of loneliness in older adults.
Recently, ambient in-home sensors have been used to continuously and unobtrusively monitor individuals in their own homes [18]–[22]. These systems may be designed to help seniors remain independent and healthy as long as possible by capturing meaningful behavioral measures which relate to health outcomes of interest. The nature and type of sensors used in such platforms can vary widely. For example, several research groups have proposed video cameras [23], [24] and body worn tags [25], [26] as viable options in in-home monitoring. Video cameras [23] installed in key areas of the home enable assessment of various gait parameters, may be used to detect falls, and allow the identification of different individuals moving through the home. However, many individuals consider the use of video monitoring to be a violation of privacy even when discriminating features of the video data are removed prior to processing. Body-worn tags (e.g. RFID, UWB, and WiFi) [25], [26] have also been proposed for in-home assessment as they track how an individual moves throughout the home and are sensitive to multiple individuals at the same time. However, among older adults this technology poses challenges to long term tracking as seniors forget to wear sensors or take them off when they become uncomfortable. In contrast, inexpensive wireless movement detectors and contact sensors can detect a subject’s activities in the home on a daily basis without being overly intrusive or requiring participants to remember to wear or charge devices. However, they give no information about who (or what) is causing the sensor to fire, and may be subject to high levels of noise. Thus, they are most effective in single resident homes. Because older adults living alone are the most vulnerable to feelings of loneliness or social isolation, this technology is ideal for unobtrusive monitoring of loneliness and isolation in older adults [27].
There are several aspects of behavior that can be assessed using these in-home sensing technologies which may also relate to loneliness levels. For example, our preliminary research shows that both time out-of-home [28], [29] and telephone use [30] are associated with loneliness levels among older adults. Other behaviors that may be related to loneliness include computer use [31]–[33], sleep quality [6], [10], and measures of daytime dysfunction [7] which include in-home mobility [34] and in-home walking speed [35], [36].
This paper represents a proof of concept of a system to estimate loneliness using an array of in-home sensors. We first describe the system, including the sensors used and the metrics developed to measure key behaviors of interest from the sensor platform. Next, we describe our preliminary research on the relationship between in-home behavior and loneliness using data from participants monitored in their own homes for up to 8 months.
II. System Development
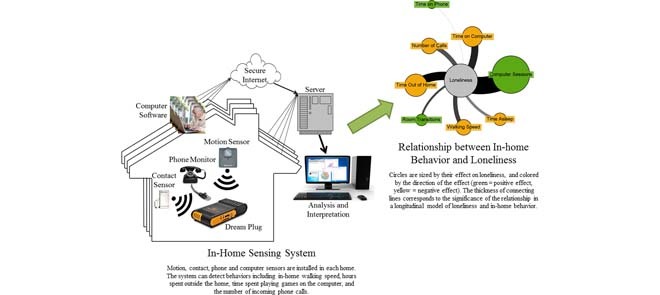
In this section, we describe the sensor platform, including the array of sensors we install in the homes of older adults to capture behaviors of interest. Then we describe our system to pull the data from each home and store it on our local servers. Finally, we discuss our development of algorithms to assess key behaviors using the in-home sensing platform.
A. Sensor Platform Components
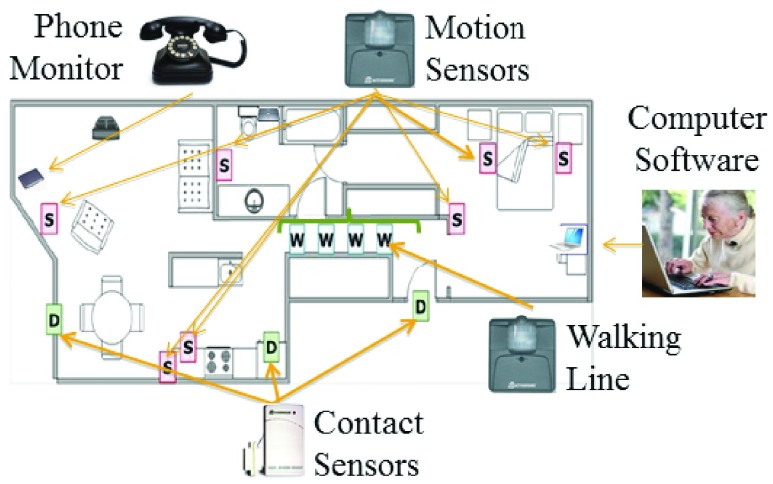
Each home is installed with an array of sensors designed to capture key behaviors of interest. The various sensors and their location in the home are shown in Fig 1. We now describe each sensor in more detail.
FIGURE 1.
Typical floor plan showing the types of sensors included in the in-home monitoring platform and their distribution throughout the home.
1). Wireless Motion Sensors
Pyroelectric infrared motion sensors (MS16A,  .com) are installed in each room of the home. These sensors function by firing a signal each time movement is detected, with a refractory period after firing of about 6 seconds. The signal captures the time of day motion was detected and the room of the home the sensor is in.
.com) are installed in each room of the home. These sensors function by firing a signal each time movement is detected, with a refractory period after firing of about 6 seconds. The signal captures the time of day motion was detected and the room of the home the sensor is in.
Each home also receives an array of 4 motion sensors placed in a straight line approximately 60 cm apart from each other in a corridor of the home the resident regularly walks through. This array of sensors which we call a “walking line” is designed specifically to capture the in-home walking speed, discussed in more detail below.
2). Contact Sensors
Contact sensors (DA10A,  .com) are installed on each external door to the home. The contact sensors are magnetic, and are installed so the main portion of the sensor is on the door frame, and the secondary portion of the sensor is on the door itself. Thus, the sensor fires a different signal when the two magnets are together (the door is closed) than when they are apart (the door is open). Each time there is a state change (e.g. transition from closed to open), the contact sensor fires a signal corresponding to the time of day the state change occurred, which door the sensor was installed on, and the new state. The sensors also fire heartbeats such that if no event occurs within about an hour, the contact sensor emits a signal corresponding to whatever state it is in at present.
.com) are installed on each external door to the home. The contact sensors are magnetic, and are installed so the main portion of the sensor is on the door frame, and the secondary portion of the sensor is on the door itself. Thus, the sensor fires a different signal when the two magnets are together (the door is closed) than when they are apart (the door is open). Each time there is a state change (e.g. transition from closed to open), the contact sensor fires a signal corresponding to the time of day the state change occurred, which door the sensor was installed on, and the new state. The sensors also fire heartbeats such that if no event occurs within about an hour, the contact sensor emits a signal corresponding to whatever state it is in at present.
3). Phone Monitors
Phone monitoring devices are installed in each home to unobtrusively assess daily phone use. The monitors (Shenzhen Fiho Electronic, Fi3001B) plug directly into the phone line, and are designed to record all signals on the line including ‘on hook’, ‘off hook’, ‘ring start’, and ‘dtmf’ (number dialed).
4). Computer Software
While many computer monitoring software programs exist, few provide the infrastructure necessary to transmit all data to a remote server. In our work, we use two different programs that allow this retrieval and storage of all computer activities: WorkTime Corporate (Nestersoft Inc., Ontario Canada), which functions on Windows-based platforms up to Windows 7 and Rescue Time Professional (RescueTime, Seattle WA), which functions on Apple OS X computers. Thus, WorkTime is installed on all personal computers with Windows-based operating systems and RescueTime on all Apple computers.
B. Data Retrieval
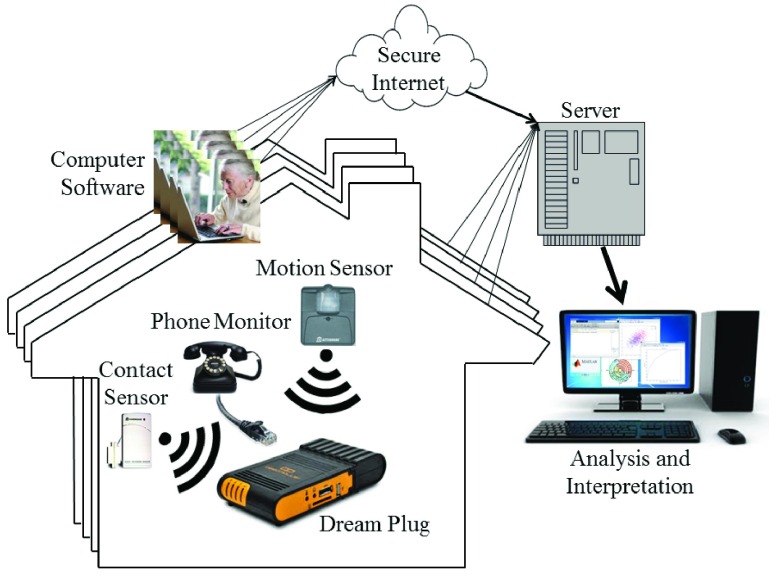
Fig. 2 shows a diagram of the data retrieval process. In each home, data from all sensors except the computer software is transmitted to a local Linux computer (DreamPlug, GlobalScale Technologies, Anaheim, CA). For all motion and contact sensors, data transfer to the DreamPlug occurs over WiFi, while the phone monitor data is transferred via USB. Once a day the aggregated data is transferred over an encrypted connection to servers located at a secure data center where it is stored in a local database. Data collected on the subject’s personal computing device is encrypted and cached locally until it can be transmitted over the internet to the secure servers. Once transferred to the secure servers, the data are decrypted and stored in a local database according to the associated subject.
FIGURE 2.
Schematic diagram of the data retrieval process. Motion and contact sensors transmit data via WiFi to a DreamPlug PC in each home, while the phone monitor data is transferred via USB. The DreamPlug transmits all the sensor data across a secure wireless connection to our servers each night. In addition, data from the personal computing device is encrypted and transmitted over the internet (represented as a cloud) to the secure servers. Data accessed from the server is time-aligned across subjects and used for analysis and interpretation.
In order to ensure high data integrity, we developed an automated system to alert technicians when any of our sensors or equipment appeared to be malfunctioning. Once a sensor is known to be malfunctioning for a given period of time (for example, an X10 sensor’s battery died so we did not collect any data from that sensor until the battery was replaced), we record the type of malfunction, the sensors that were affected and the dates. This information is appended to the data as a bit flag in the SQL tables.
All data are stored in MySQL (Oracle, Redwood Shores, CA) tables, and scripts have been developed in Matlab (Mathworks, MA, USA) to query the SQL tables and implement the developed algorithms.
C. Algorithms Developed to Assess Behavior
There are several aspects of behavior that can be assessed using this in-home sensing platform which may also relate to loneliness levels. For example, our preliminary research shows that both time out-of-home [28] and telephone use [30] are associated with loneliness levels among older adults. Other behaviors that may be related to loneliness include computer use [31]–[33], visitors to the home, sleep quality [6], [10], and measures of daytime dysfunction [7] which include in-home mobility [34] and in-home walking speed [35], [36]. We will discuss our developed algorithms to assess each of these behaviors in this section.
1). Daily Hours Spent Outside the Home
Time spent outside the home has been shown to relate to overall mental wellbeing as well as cognitive health and physical ability [29]. In addition, the total time spent outside the home may be related to negative health events [37]. To detect this important aspect of everyday behavior, we developed a logistic regression classifier designed to probabilistically determine whether anyone is present in the home for each 5-minute interval using key features calculated from the motion and contact sensors [28]. This technique has high sensitivity (94%) and specificity (98%) in identifying periods where no one is present in the home.
2). Number of Incoming and Outgoing Phone Calls
Telephone use is an important measure of independence [38] and socialization [39], and is therefore an important behavior to measure among older adults. While our phone-monitor functions by recording phone signals on the phone line, it may record spurious events and occasionally fails to record a true event (see Table 1). As a result, it was necessary to build a classifier to detect the number of incoming and outgoing phone calls. To that end, we collected the landline phone records for one month from six subjects living in 3 different retirement communities. Using these data, we built a logistic regression classifier using the data from three participants to train the classifier and the data from the remaining three participants to test the classifier. Because the noise in the telephone line differs by retirement community, we trained our classifier on data from one retirement community and tested on the data from the remaining two retirement communities to understand how the classifier would perform on data from a random retirement community. Our classifier performed well, with an average of 88% sensitivity and 99.9% specificity on the training data, and 76% sensitivity and 99.8% specificity on the testing data.
TABLE 1. Example data from an in-home phone monitor showing an example of both a spurious event: the additional ‘off hook’ signal at 23:01:12, and a missed event: there should be an ‘on hook’ signal after the off hook at 18:10:20.
| Date | Time | Description |
|---|---|---|
| 08-Jun | 18:09:43 | ring start |
| 08-Jun | 18:09:46 | ring stop |
| 08-Jun | 18:10:20 | ring start |
| 08-Jun | 18:10:20 | off hook |
| 08-Jun | 23:01:11 | off hook |
| 08-Jun | 23:01:12 | off hook |
| 08-Jun | 23:03:23 | on hook |
3). Walking Speed
Older adults suffering from loneliness may also experience daytime dysfunction [7], which may manifest as a slower in-home walking speed. Walking speed has also repeatedly been shown to be related to cognitive health and wellbeing [20], [35], [40], [41]. To continuously capture this key health variable, we developed a technique to assess in-home walking speed using the walking line described above. The field of view of the sensors in the walking line is restricted so they fired only when the participant passed directly underneath them and the distance between sensors recorded to allow adequate calculation of velocity as the participant passed through the line of sensors [36], [42]. While the data from these sensors is highly correlated with true walking speed [36], the variability in sensor placement and refractory period means there is typically a constant offset between true walking speed and calculated walking speed for each line of sensors. Thus, it is necessary to normalize the gait speed estimate for each participant to allow cross-sectional comparison of changes in gait speed relative to a normal gait.
4). Mobility
Similar to in-home walking speed, in-home mobility may drop when people are experiencing daytime dysfunction, a common side effect of loneliness [7]. In-home mobility was computed by first assuming that the motion sensors only fire when they detect movement from the participant. Thus, consecutive firings from the same sensor indicate movement within a room (indicative of activity levels), and consecutive sensor firings from different sensors indicate the participant is moving throughout the home. Under this assumption, total daily mobility can be estimated by summing the total number of consecutive firings from two different sensors each day [34]. However, this measure of mobility will be influenced by the number of hours spent inside the home [43]. That is, the more hours spent outside the home each day, the smaller the opportunity for mobility. To get a meaningful measure of in-home mobility, it is therefore necessary to divide the mobility estimate by the total hours spent inside the home. This number represents the estimated level of mobility per hour inside the home. In addition, we have previously demonstrated that this in-home mobility measure may be affected by time of day, physical ability of the individual, and the structure of the home [34], [43]. To account for factors that would influence the mobility estimate outside of the true mobility of the individual (e.g. home layout), it is necessary to normalized each subject’s mobility scores by their median number of sensor firings and the interquartile range of the number of sensor firings. In this way, the estimates of in-home mobility represent the change in mobility for a given individual, and can thus be compared cross-sectionally.
III. Relationship Between Behavior and Loneliness
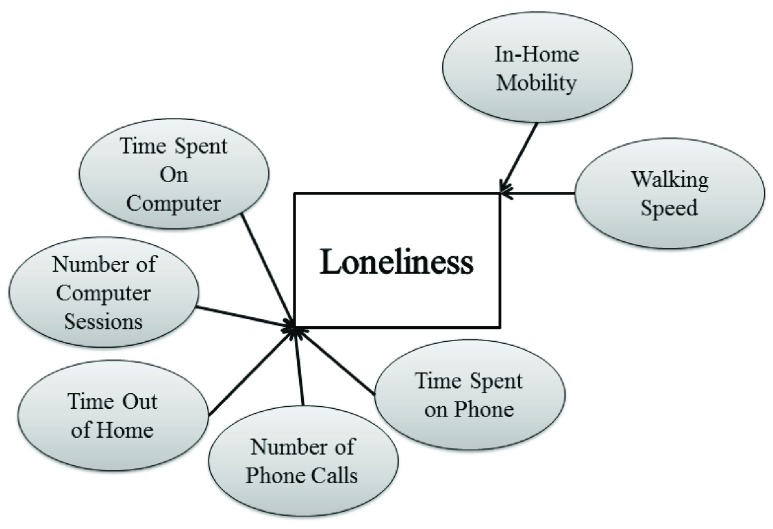
This section will describe the experiment to determine the relationship between in-home behavior and loneliness over time. We hypothesize that there will be a significant relationship between in-home behavior and loneliness, and that the variables most closely associated with social behaviors (those on the left of the graph in Fig. 3), will be most strongly associated with loneliness.
FIGURE 3.
Diagram of in-home behaviors used in the model of in-home behavior and loneliness. The variables on the left are hypothesized to be significantly related to loneliness.
A. Participants
To analyse the longitudinal relationship between in-home behavior and loneliness, we recruited 16 subjects from low-income apartment communities and by word of mouth and followed them using the in-home sensing platform for 8 months. The minimum age for participation in the study was 62 years. Participant inclusion criteria included living alone and independently and a minimum score of 26 on the Mini Mental State Examination [44]. Participants were also required to be ambulatory and in average health for their age, have internet in their apartments, and know how to use a computer. Eligible participants who knew how to use a computer but did not already own one were given a computer to use for the duration of the study. All participants agreed to have the entire sensor platform installed in their own homes for an 8 month period and signed informed consent prior to participating in any study activities. This protocol was approved by the Oregon Health & Science University Institutional Review Board (IRB #9631). The mean age of participants was 71.0 ± 6.3 years; 81% were female and all had completed high school (see Table 2). Despite recruiting from low-income retirement communities, the average socioeconomic status (SES) score was 45 using the Hollingshead Four Factor Index of Social Status [45], which assigns scores based on the education level and occupation of the household. The range of the scale is from 8 to 66; thus some of the participants scored high in this measure of SES despite living in a low income retirement community.
TABLE 2. Baseline demographic and clinical characteristics of the population.
| Characteristic | Statistic | Range (Min, Max) |
|---|---|---|
| Age (years) | 71.0 ± 6.3 | (62, 80) |
| Gender (% Female) | 81% | - |
| Education (years) | 15 ± 1.5 | (12, 18) |
| MMSE | 29.3 ± 0.95 | (27, 30) |
| Socioeconomic Status | 45.1 ± 9.75 | (33, 62) |
| Race (% Caucasian) | 100% | - |
| UCLA Loneliness Score | 43.8 | (29, 60) |
B. Methods
We assessed loneliness using the University of California Los Angeles (UCLA) Loneliness Scale [12], [46]. This survey asks questions such as “I feel part of a group of friends” and “I feel like others are around me but not with me” where response options are: (1) Never, (2) Rarely, (3) Sometimes and (4) Often. To generate a composite loneliness score, the value of all positive questions ( ) was first reversed and then scores on all 20 questions were summed to give a loneliness score ranging from 20 to 80, with 80 being the loneliest. A validation study among older adults demonstrated that this survey has high internal reliability (
) was first reversed and then scores on all 20 questions were summed to give a loneliness score ranging from 20 to 80, with 80 being the loneliest. A validation study among older adults demonstrated that this survey has high internal reliability ( ) [46]. In this cohort, the average loneliness score was 43.9±9.5 (max: 64; min: 28), which is higher than the average reported by Russell [46], likely because we specifically recruited individuals from low-income retirement communities where loneliness is likely to be higher [47].
) [46]. In this cohort, the average loneliness score was 43.9±9.5 (max: 64; min: 28), which is higher than the average reported by Russell [46], likely because we specifically recruited individuals from low-income retirement communities where loneliness is likely to be higher [47].
Participants were queried regarding their loneliness at a minimum of 4 distinct time points: baseline, follow up period 1 which fell 8 weeks after the last participant was recruited, follow-up period 2 which fell 9 weeks after follow up period 1, and finally follow up period 3 which fell 12 weeks after follow up period 2. We computed the internal reliability of the scale at each time point, and found high internal consistency for the cohort (mean Cronbach’s alpha: 0.9489; min: 0.9432, max: 0.9535).
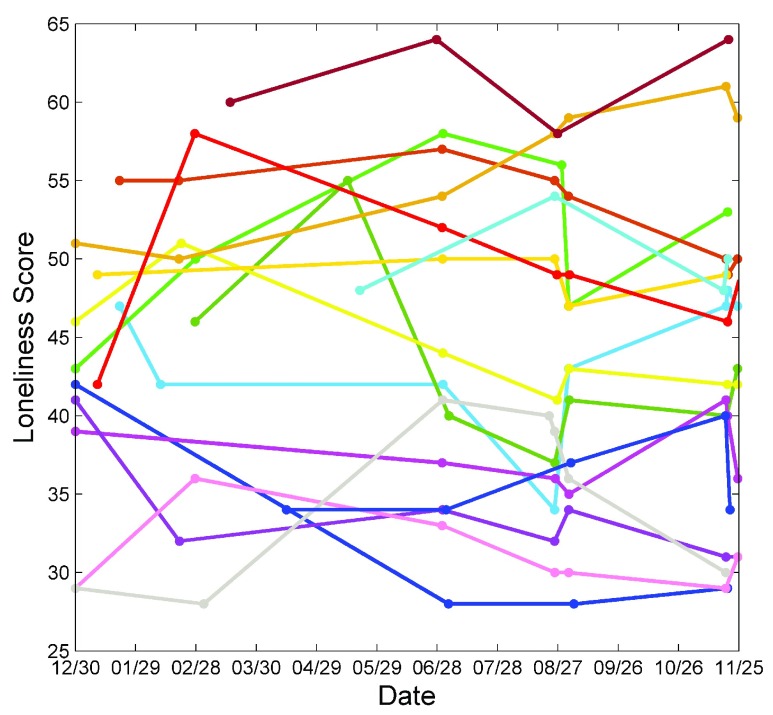
At baseline, the loneliness survey was administered in-person: participants were asked to fill out a paper copy of the survey. After consenting to be in the study, participants were added to an email list and study information was gathered through on-line surveys. That is, the UCLA Loneliness survey was emailed to each participant with a subject-specific link to the survey at all follow up waves. Due to technical difficulties with the survey, some participants were emailed a link to the survey on two consecutive weeks and completed the survey on both weeks. Thus, the maximum number of loneliness observations possible per individual was 6 (mean 4.8). Participants completed the form online in their own homes. One participant who did not know how to use email completed a paper copy of the survey in the first follow up, and completed the survey over the phone in the subsequent follow up periods. The loneliness scores over time are shown in Fig. 4.
FIGURE 4.
A spaghetti plot of UCLA Loneliness Scores from baseline through the monitoring period. Each different color of line represents loneliness scores from one participant. Note that the baseline data point is not included in the model for any subject as the sensor system had not yet been installed at this point.
While we developed a technique to assess the total number of incoming and outgoing phone calls, the majority of participants in this study used cell phones ( ). For these participants, we collected raw phone logs from the phone carrier. Since some of the phone carriers did not keep track of whether the call was incoming or outgoing, we were only able to include total number of calls in our model of loneliness and behavior. For the remaining subjects who used landline phones, we collected phone logs using our developed algorithm.
). For these participants, we collected raw phone logs from the phone carrier. Since some of the phone carriers did not keep track of whether the call was incoming or outgoing, we were only able to include total number of calls in our model of loneliness and behavior. For the remaining subjects who used landline phones, we collected phone logs using our developed algorithm.
C. Results
1). Longitudinal Linear Mixed Effects Regression
To assess the relationship between in-home behavior and loneliness, we ran a longitudinal linear mixed effects regression model with random offset using the in-home data from the same day the participants completed the UCLA Loneliness scale. Because our data is clustered by subject (e.g. multiple data points are included from the same subject), we used a mixed effects model as it explicitly accounts for repeated measures within the same subject and subject specific effects by including a random offset. The mixed effects framework also handles missing observations without needing to drop observations [48]. This is in contrast to a standard linear model, for example, in which standard errors, confidence intervals, and  -values are all estimated incorrectly when applied to correlated data.
-values are all estimated incorrectly when applied to correlated data.
The mixed effects model with random offset for  subjects with
subjects with  independent variables is given by the following equation:
independent variables is given by the following equation:
 |
where  is the reported UCLA Loneliness score for a given subject
is the reported UCLA Loneliness score for a given subject  at time
at time  ,
,  is the vector of
is the vector of  independent variables for subject
independent variables for subject  at time
at time  ,
,  is the p-length vector of fixed effects regression coefficients (coefficients that are constant across subjects), and
is the p-length vector of fixed effects regression coefficients (coefficients that are constant across subjects), and  is the m-length vector of random effects, in this case a random intercept for each subject which is assumed to be normally distributed with mean 0. In addition, the noise term
is the m-length vector of random effects, in this case a random intercept for each subject which is assumed to be normally distributed with mean 0. In addition, the noise term  is assumed to be normally distributed with mean 0.
is assumed to be normally distributed with mean 0.
Due to the small sample size, we did not control for any demographic characteristics to avoid overfitting the data. Instead, we allowed these characteristics to be captured in the person-specific offset,  . We included six behavioral variables in our model: the hours spent outside the home, the total number of calls (both incoming and outgoing), the total number of computer sessions, the hours spent on the computer, the normalized in-home walking speed, and the normalized in-home mobility. Missing data on any of these behavioral measures occurred due to technical difficulties with the sensor platform. That is, the sensors occasionally stopped collecting data due to a device failure or software issue, and would begin collecting data again until a technical research assistant visited the home to fix the issue. Thus, the missing data mechanism was not related in any way to the study participants or their characteristics. As a result, we assumed the all data were missing completely at random, and dropped days with missing data from the model. In the final model, 24.6% of the data points were missing in at least one behavioral variable.
. We included six behavioral variables in our model: the hours spent outside the home, the total number of calls (both incoming and outgoing), the total number of computer sessions, the hours spent on the computer, the normalized in-home walking speed, and the normalized in-home mobility. Missing data on any of these behavioral measures occurred due to technical difficulties with the sensor platform. That is, the sensors occasionally stopped collecting data due to a device failure or software issue, and would begin collecting data again until a technical research assistant visited the home to fix the issue. Thus, the missing data mechanism was not related in any way to the study participants or their characteristics. As a result, we assumed the all data were missing completely at random, and dropped days with missing data from the model. In the final model, 24.6% of the data points were missing in at least one behavioral variable.
In order to ensure coefficient estimates were not biased by multicollinearity, the variance inflation factor (VIF), a standard diagnostic tool for multicollinearity, was calculated for each independent variable included in the model. The VIF for a given predictor in the model is calculated by performing a linear regression with the given predictor as the dependent variable and the remaining predictors as the independent variables. Using the  from that regression, the VIF is calculated as
from that regression, the VIF is calculated as  . The VIF for all variables included in the model was below 2.5, indicating any multicollinearity can safely be ignored [49]. A p-value of 0.05 was considered significant.
. The VIF for all variables included in the model was below 2.5, indicating any multicollinearity can safely be ignored [49]. A p-value of 0.05 was considered significant.
The results of the mixed effects regression between loneliness and in-home behavior are presented in Table 3. A total of 58 data points were included in this model, representing an average of 3.6 data points per participant. As can be seen, loneliness is negatively associated with the total hours spent outside the home, such that a unit increase in hours spent outside the home results in a corresponding drop in loneliness of 0.83 points. Loneliness was also found to be significantly related to the total number of computer sessions, such that each additional computer session is associated with an increase in loneliness score of 0.77 points. The fixed offset (Constant) was also significant in the mixed effects regression, and its value of 46 indicates that if all in-home variables are zero (e.g. no time out-of-home, no computer sessions) the model will predict a UCLA Loneliness Score of 46. The subject-specific offsets are not shown. Aside from time out-of-home and number of computer sessions, the other in-home behavioral variables were not significant in predicting loneliness. Still, the beta coefficients for time on computer, walking speed, and number of calls were all in the anticipated direction, and all had a relatively large effect on loneliness. The overall  for the model was 0.358, demonstrating a measureable relationship between behavior and loneliness.
for the model was 0.358, demonstrating a measureable relationship between behavior and loneliness.
TABLE 3. Results of the mixed effects linear regression between UCLA Loneliness and in-home behavior. Variables are not centered so the relationship between each independent variable and loneliness can be directly interpreted from the coefficient.
| Coefficient | Standard Error | z | 95% | Confidence Interval | |
|---|---|---|---|---|---|
| Time Out of Home (hours) | −0.825** | 0.268 | −3.08 | −1.35 | −0.30 |
| Number of Calls | −0.146 | 0.101 | −1.44 | −0.34 | 0.05 |
| Number of Computer sessions | 0.767* | 0.300 | 2.55 | 0.18 | 1.35 |
| Time on Computer (hours) | −0.939 | 0.560 | −1.68 | −2.04 | 0.16 |
| Normalized Median Walking Speed | −2.05 | 1.713 | −1.20 | −5.41 | 1.31 |
| Normalized Room Transitions | 0.825 | 0.727 | 1.13 | −0.60 | 2.25 |
| Constant | 46.22*** | 2.628 | 17.59 | 41.07 | 51.37 |
p<0.05,
p<0.01,
p<0.001
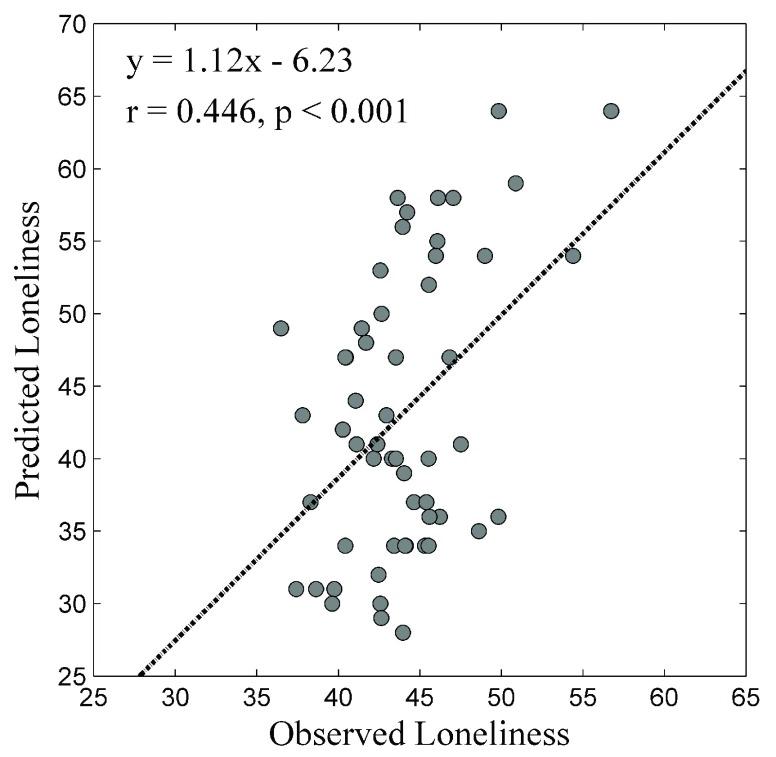
2). Out of Sample Cross-Validation of Loneliness
In order to ensure the model is not overfitting the data, we performed an out-of-sample cross-validation and computed the correlation between out-of-sample predictions of loneliness and reported loneliness levels. That is, we trained our regression model on data from all but one participant, and then used the coefficients from that model to predict the loneliness of the remaining participant. By iteratively doing this for each participant, we were able to obtain out-of-sample loneliness scores for all participants, and relate these scores to the reported UCLA loneliness scores. The correlation between the reported loneliness and out-of-sample loneliness (using leave one out cross-validation) was 0.42, as shown in Fig. 5. In this figure, it is clear that the model tends to over-estimate the loneliness of individuals whose reported loneliness is low, and under-estimate the loneliness of those whose reported loneliness is high. This suggests the model is not capturing all of the variation in loneliness scores as it tends to estimate too close to the mean. Adding additional model variables which capture additional variation in behaviors associated with loneliness or additional person-specific characteristics may improve the model’s ability to predict out-of-sample loneliness scores.
FIGURE 5.
Scatter plot of the observed and predicted loneliness scores. As can be seen, the predicted loneliness score correlates highly with the reported UCLA Loneliness score.
We also calculated the normalized mean absolute error (MAE) and the normalized root mean squared error (RMSE) between the reported UCLA Loneliness Score and the predicted out-of-sample loneliness scores where we normalized these error terms by the standard deviation of the UCLA Loneliness Scores to give an indicator of the relative error. That is, the normalized RMSE was calculated using the following equation:
 |
The normalized MAE was 0.81 while the normalized RMSE was 0.91.
IV. Discussion
This paper presents a first approach toward a comprehensive system to assess loneliness in older adults using an in-home assessment process that is unobtrusive and objective. We demonstrate the close relationship between in-home behavior and loneliness, an important health outcome which is difficult to measure by self-report because of the social stigmas associated with being lonely. This paper marks the first time multiple objective behavioral measures have been related to loneliness and underscores the possibility of using smart home sensor platforms to objectively and continuously monitor loneliness levels among older adults. In the future, models such as that presented in Table 3 could be trained on longitudinal data and implemented using continuous in-home data streams from older adults. In this fashion, daily estimates of an older adult’s loneliness could be determined and trajectories of increases in loneliness over time could be detected. Thus, it may be possible to sense a decline into loneliness at the earliest possible time point, enabling intervention and prevention of many of the negative consequences associated with loneliness.
In our longitudinal regression model, daily time out-of-home was significantly associated with loneliness. This result is consistent with previous studies on time out-of-home and loneliness. For example, older adults themselves report that leaving the home helps ward off feelings of loneliness [50]. Studies using objective measures of time out-of-home such as GPS monitors have also found a relationship between emotional wellbeing and total hours spent outside the home [29], [51]. In addition, previous work has demonstrated that the onset of mobility limitations that make leaving the home challenging are associated with loneliness [52].
The total number of computer sessions was also significantly associated with loneliness (p < 0.05). Previous work analyzing the relationship between computer use and loneliness has found conflicting results, with some suggesting that computer use helps ward off loneliness [33], [53]–[55] and others (especially those among young adults) demonstrating that increased computer use is associated with increased loneliness [56]–[58]. These conflicting results may be because the computer can be used for both social and anti-social activities. That is, if used to improve communication with the social network, increased computer use may reduce loneliness. On the other hand, if used to perform isolating activities such as online games, increased computer use may be associated with increased loneliness. While we installed software that can determine the exact activities performed on the computer on all subject computers, we were not able to include these variables in this model due to the small sample size. Follow up work with assess the longitudinal relationship between specific social and anti-social computer activities and loneliness.
Phone use and hours on the computer were not significantly associated with loneliness. The lack of significance in these social variables may be in part because of the high correlation between the social variables. That is, the number of phone calls was highly correlated with the amount of time spent on the phone (r = 0.6), and the number of computer sessions was highly correlated with the amount of time spent on the computer (r = 0.5). Including variables that are highly correlated in a model can result in multicollinearity, which can inflate the variance of coefficients. While we tested all variables included in the model for non-ignorable multicollinearity using the VIF, it is possible that these high correlations still resulted in biases in the variables or their significance. Indeed, removing the total time spent on the phone from the model altogether increases the significance of the total number of phone calls (p = 0.181) while the coefficient remains nearly the same ( ) indicating the presence of at least some bias from multicollinearity. One way to overcome biases associated with multicollinearity is to increase the sample size, highlighting the need to test these results in a larger, more diverse cohort.
) indicating the presence of at least some bias from multicollinearity. One way to overcome biases associated with multicollinearity is to increase the sample size, highlighting the need to test these results in a larger, more diverse cohort.
It may also be that telephone use was not significant because a major aspect of phone use, texting, was not captured in this cohort. Ad-hoc interviews with participants revealed that many of these older adults prefer texting to calling, and do most of their communication this way. Future studies on the relationship between loneliness and behavior should incorporate variables that capture texting in the models. We were also not able to differentiate between incoming calls and outgoing calls in this study as not all the phone companies we collected logs from stored this information. This was unfortunate as previous work has demonstrated that loneliness is more closely linked to the number of incoming calls than outgoing calls [39]. Future studies on loneliness in older adults should include incoming and outgoing calls separately.
This study was also not able to accurately capture the number dialed for all participants. Collecting numbers dialed would enable the incorporation of variables related to the social network such as the overall size of the network (number of contacts), the loss of a contact, or the addition of a new contact. Longitudinal analyses on the effect of network change revealed that losing a network member is associated with depressive symptoms and changes in network composition (both positive and negative) are associated with health outcomes [59]. Thus, monitoring network change using telephone data may not only improve the ability to unobtrusively assess loneliness levels, but also enable the identification of network changes (e.g. the loss of a network member) which herald upcoming health consequences.
Total time on the computer may not have been significant due to our inability to track computer use on tablets and smart phones. Several participants owned tablets, and two indicated their tablet was their primary device for browsing the internet and playing games, highlighting the importance of including tablet monitoring software in future studies of loneliness in older adults.
While the results presented here are promising, there are several ways the longitudinal model of loneliness could be improved using in-home data. First, due to the small and relatively homogeneous nature of our cohort, our behavioral model of loneliness did not utilize demographic and subject characteristic data that have been shown to be associated with loneliness in previous research on loneliness in older adults. Such demographic variables influencing loneliness include gender [60], income [61], marital status (widows are particularly vulnerable to loneliness) [62]–[64], and number of children [65]. Other studies have indicated that childhood experiences may play a large role in the perception of loneliness in adulthood [66], [67]. Personality may also affect the perception of loneliness: individuals who are highly neurotic on personality inventories are more likely to experience loneliness [68], as are those with high anxiety levels [69]. In addition, pet ownership is likely to influence loneliness. For example, pets have been used in multiple interventions designed to ameliorate loneliness as they provide a level of companionship that may be otherwise lacking [70]–[72]. Future larger studies on loneliness and behavior should account for such demographic variables thought to be associated with loneliness. In addition, various diseases and health states may affect the independent variables used in the model. For example, walking speed may be related not only to daytime dysfunction but also mobility limitations in diseases such as Parkinson’s disease or dementia. In this study, the effects of such diseases were not accounted for as all participants were required to be in average health for their age and without major mobility limitations. Future studies should assess the performance of the developed model in a more diverse population that includes individuals suffering from such neurocognitive diseases.
This study has several limitations. Notably, the study spanned less than one year, with an average of 3.4 complete observations per participant. Future studies should also assess the relationship between loneliness and behavior over a longer time period to better understand the time course of loneliness, the seasonal effects of loneliness, and the complex relationship between behavior and loneliness. In addition, all participants included in this model volunteered to be part of the study, and agreed to have the sensor system installed in their homes. There may be key differences in characteristics between those who are or are not willing to participate in research studies, especially those involving in-home sensors. Some work has been done to identify the differences between these groups indicating that those who participate are more likely younger and more highly educated older adults [73]. To overcome some of this bias, this study specifically targeted individuals living in low-income retirement communities for recruitment.
V. Conclusion
While future studies are required to validate these results in a larger, more diverse cohort, these results show potential for using behavioral measures to objectively assess loneliness levels among older adults. An objective model of loneliness has the potential to improve outcomes for older adults as it would provide the opportunity to enhance our understanding of the relationship between loneliness and health through longitudinal, objective monitoring of loneliness [74]. An objective model would also help in the evaluation of interventions designed to improve loneliness by not only reducing the number of participants necessary to demonstrate statistically significant improvement in loneliness but also providing insight into behaviors that changed or improved over the course of the intervention. This approach is best suited to detect changes in behavior within an individual that may herald the onset of loneliness. Differences in home layout or personal norms across individuals make comparison of behaviors such as in-home mobility and walking speed across individuals challenging. In the long term, unobtrusive in-home sensor platforms employed in various community settings may assist in the identification of lonely individuals, preventing them from becoming isolated and ignored. Of course, in such environments, stringent safeguards would have to be put in place regarding who can access the data and what can be done with it. For example, it may be possible to send data directly to the participant’s doctor or nurse, but security measures would need to be in place to ensure the data was delivered to the correct doctor and that the doctor could correctly interpret and understand the data received. It would also be important to ensure that older adults fully understood the technology they are accepting, especially among those with cognitive decline. In this population, a legal guardian or authorized representative may need to sign consent on behalf of the individual.
Taken together, this objective model of loneliness has the potential to dramatically impact the mental wellbeing of older adults as a whole.
Acknowledgment
The authors thank all the participants and research staff of the Capturing Time project. J. Austin also thanks Professor Todd Leen, who provided guidance and support in computing model statistics and generating descriptive figures.
Biographies

Johanna Austin received the B.S. and Ph.D. degrees in bioengineering from Washington State University, Pullman, WA, USA, in 2010, and the Ph.D. degree in biomedical engineering from the Oregon Health & Science University, Portland, OR, USA, in 2015.
She is currently a Post-Doctoral Fellow in neurology with Oregon Health & Science University, where she is involved in developing a system to unobtrusively assess loneliness among caregivers of patients with cognitive decline. Her research interests include unobtrusive, longitudinal measurement with applications to health care, emphasizing socialization and loneliness in the elderly population.

Hiroko Dodge received the Ph.D. degree in demography and statistics from Pennsylvania State University. She is currently Associate Professor of Neurology with Oregon Health and Science University (OHSU) and a Kevreson Research Professor of Neurology with the University of Michigan (UM). She directs two Alzheimer’s disease (AD) Centers’ Biostatistics and Data Cores with OHSU and UM.
Her research interests cover a wide range of conceptual areas, including epidemiology of dementia and healthy aging process, the latter using data collected in Okinawa, Japan. She is currently examining whether stimulations through social interactions using modern communication technologies could improve cognitive functions. She holds fellow status with the Gerontological Society of America and serves as a Statistical Editor and an Associate Editor for several dementia related journals.

Thomas Riley received the bachelor’s degree in physics from the University of Portland, Portland, OR, USA. He is currently the Technical Lead with the Oregon Center for Aging and Technology, Oregon Health and Science University, Portland.
His interests include system design, development and management of large scale deployments of unobtrusive sensors, distributed databases, big data analytics, and implementation of emerging sensor technologies.
Peter G. Jacobs received the bachelor’s degree in engineering from Swarthmore College, Swarthmore, PA, USA, the master’s degree in electrical and computer engineering from the University of Wisconsin, Madison, WI, USA, and the Ph.D. degree in electrical engineering from Oregon Health & Science University, Portland, OR, USA.
His interests are in the area of researching, designing, and translating novel medical devices and systems for use within natural living environments. Numerous projects are ongoing in the lab, which fit broadly within the areas of medical device and algorithm development primarily in the area of diabetes technologies and ubiquitous computing for delivering home-based health care solutions including wearable and ambient systems.

Stephen Thielke received the M.D. degree. He is currently a Geriatric Psychiatrist and Health Services Reseracher with the University of Washington and the Puget Sound VA Geriatric Research, Education, and Clinical Center (GRECC).
He is the GRECC Associate Director for Education and Evaluation. He conducts research about dementia medications, depression and pain in older adults, and the use of monitoring technologies in healthcare.

Jeffrey Kaye received the M.D. degree from New York Medical College, New York, USA. He trained in neurology with Boston University, Boston, MA, USA, subsequently completing a fellowship in movement disorders and neuropharmacology. He was a Medical Staff Fellow of brain aging with the National Institute on Aging, National Institutes of Health, Bethesda, MD, USA.
He is currently the Layton Professor of Neurology and Biomedical Engineering, the Director of the Oregon Center for Aging and Technology, and the Director of the Layton Aging and Alzheimer’s Disease Center with Oregon Health & Science University, Portland, OR, USA. His research interests include the design, study, and application of ubiquitous unobtrusive technologies and systems for community-based health research, clinical trials, and the identification of behavioral and biological biomarkers of healthy aging.
Funding Statement
This work was supported in part by the National Institute of Health and the National Institute on Aging under Grant P30AG008017 and Grant P30AG024978 and the Oregon Arts Commission.
References
- [1].Peplau L. A., “Loneliness research: Basic concepts and findings,” in Social Support: Theory, Research and Applications, Sarason I. G. and Sarason B. R., Eds. The Netherlands: Springer, 1985, pp. 269–286. [Google Scholar]
- [2].Peplau L. A. and Perlman D., Eds., “Perspectives on loneliness,” in Loneliness: A Sourcebook of Current Theory, Research and Therapy. New York, NY, USA: Wiley, 1982, pp. 1–18. [Google Scholar]
- [3].Sermat V., “Sources of loneliness,” Essence, Issues Study Ageing, Dying, Death, vol. 2, no. , pp. 271–276, 1978. [Google Scholar]
- [4].Hector-Taylor L. and Adams P., “State versus trait loneliness in elderly New Zealanders,” Psychol. Rep., vol. 78, pp. 1329–1330, Jun. 1996. [DOI] [PubMed] [Google Scholar]
- [5].Luo Y., Hawkley L. C., Waite L. J., and Cacioppo J. T., “Loneliness, health, and mortality in old age: A national longitudinal study,” Soc. Sci. Med., vol. 74, pp. 907–914, Mar. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cacioppo J. T., et al. , “Do lonely days invade the nights? Potential social modulation of sleep efficiency,” Psychol. Sci., vol. 13, pp. 384–387, Jul. 2002. [DOI] [PubMed] [Google Scholar]
- [7].Hawkley L. C., Preacher K. J., and Cacioppo J. T., “Loneliness impairs daytime functioning but not sleep duration,” Health Psychol., vol. 29, pp. 124–129, Mar. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wilson R. S., et al. , “Loneliness and risk of Alzheimer disease,” Arch. General Psychiatry, vol. 64, pp. 234–240, Feb. 2007. [DOI] [PubMed] [Google Scholar]
- [9].Ortman J. M., Velkoff V. A., and Hogan H., An Aging Nation: The Older Population in the United States. Washington, DC, USA: U.S. Census Bureau, 2014, pp. 1125–1140. [Google Scholar]
- [10].Hawkley L. C. and Cacioppo J. T., “Loneliness matters: A theoretical and empirical review of consequences and mechanisms,” Ann. Behavioral Med., vol. 40, pp. 218–227, Oct. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shiovitz-Ezra S. and Ayalon L., “Use of direct versus indirect approaches to measure loneliness in later life,” Res. Aging, vol. 34, pp. 572–591, 2011. [Google Scholar]
- [12].Russell D., Peplau L. A., and Cutrona C. E., “The revised UCLA loneliness scale: Concurrent and discriminant validity evidence,” J. Pers. Soc. Psychol., vol. 39, pp. 472–480, Sep. 1980. [DOI] [PubMed] [Google Scholar]
- [13].de Jong-Gierveld J. and Kamphuls F., “The development of a Rasch-type loneliness scale,” Appl. Psychol. Meas., vol. 9, no. 3, pp. 289–299, 1985. [Google Scholar]
- [14].Salthouse T. A., “Mental exercise and mental aging,” Perspect. Psychol. Sci., vol. 1, pp. 68–87, Mar. 2006. [DOI] [PubMed] [Google Scholar]
- [15].Herzog A. R., Franks M. M., Markus H. R., and Holmberg D., “Activities and well-being in older age: Effects of self-concept and educational attainment,” Psychol. Aging, vol. 13, pp. 85–179, Jun. 1998. [DOI] [PubMed] [Google Scholar]
- [16].Bielak A. A., “How can we not ‘lose it’ if we still don’t understand how to ‘use it’? Unanswered questions about the influence of activity participation on cognitive performance in older age—A mini-review,” Gerontology, vol. 56, no. 5, pp. 507–519, 2009. [DOI] [PubMed] [Google Scholar]
- [17].Liang J., “Self-reported physical health among aged adults,” J. Gerontol., vol. 41, pp. 248–260, Mar. 1986. [DOI] [PubMed] [Google Scholar]
- [18].Hayes T. L., Pavel M., and Kaye J., “An approach for deriving continuous health assessment indicators from in-home sensor data,” in Technology and Aging, vol. 21, Mihailidis A., Boger J., Kautz H., and Normie L., Eds. Amsterdam, The Netherlands: IOS Press, 2008, pp. 130–137. [Google Scholar]
- [19].Skubic M., Alexander G., Popescu M., Rantz M., and Keller J., “A smart home application to eldercare: Current status and lessons learned,” Technol. Health Care, vol. 17, no. 3, pp. 183–201, 2009. [DOI] [PubMed] [Google Scholar]
- [20].Lyons B. E., et al. , “Pervasive computing technologies to continuously assess Alzheimer’s disease progression and intervention efficacy,” Frontiers Aging Neurosci., vol. 7, p. 102, Jun. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kaye J. A., et al. , “Intelligent systems for assessing aging changes: Home-based, unobtrusive, and continuous assessment of aging,” J. Gerontol. B, Psychol. Sci. Soc. Sci., vol. 66, no. 1, pp. i180–i190, Jul. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cook D. J., Schmitter-Edgecombe M., and Dawadi P., “Analyzing activity behavior and movement in a naturalistic environment using smart home techniques,” IEEE J. Biomed. Health Inform., vol. 19, no. 6, pp. 1882–1892, Nov. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Heath K. and Guibas L., “Multi-person tracking from sparse 3D trajectories in a camera sensor network,” in Proc. 2nd ACM/IEEE Int. Conf. Distrib. Smart Cameras (ICDSC), 2008, pp. 1–9. [Google Scholar]
- [24].Wang F., Skubic M., Stone E., Abbott C., Rantz M., and Keller J. M., “Toward a passive low-cost in-home gait assessment system for older adults,” IEEE J. Biomed. Health Inform., vol. 17, no. 2, pp. 346–355, Mar. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hayes T. L., Pavel M., Larimer N., Tsay I. A., Nutt J., and Adami A. G., “Distributed healthcare: Simultaneous assessment of multiple individuals,” IEEE Pervasive Comput., vol. 6, no. 1, pp. 36–43, Jan-Mar 2007. [Google Scholar]
- [26].Joshua R. S., et al. , “RFID-based techniques for human-activity detection,” Commun. ACM, vol. 48, pp. 39–44, Sep. 2005. [Google Scholar]
- [27].Victor C., Scambler S., Bond J., and Bowling A., “Being alone in later life: Loneliness, social isolation and living alone,” Rev. Clin. Gerontol., vol. 10, no. 4, pp. 407–417, 2000. [Google Scholar]
- [28].Petersen J., Austin D., Kaye J. A., Pavel M., and Hayes T. L., “Unobtrusive in-home detection of time spent out-of-home with applications to loneliness and physical activity,” IEEE J. Biomed. Health Inform., vol. 18, no. 5, pp. 1590–1596, Sep. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Petersen J., Austin D., Mattek N., and Kaye J., “Time out-of-home and cognitive, physical, and emotional wellbeing of older adults: A longitudinal mixed effects model,” PLoS ONE, vol. 10, no. 10, p. e0139643, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Petersen J., Austin D., Yeargers J., and Kaye J., “Unobtrusive phone monitoring as a novel measure of cognitive function,” Alzheimer’s Dementia, J. Alzheimer’s Assoc., vol. 10, no. 4, pp. P366–P367, 2014. [Google Scholar]
- [31].Amichai-Hamburger Y. and Ben-Artzi E., “Loneliness and Internet use,” Comput. Human Behavior, vol. 19, no. 1, pp. 71–80, 2003. [Google Scholar]
- [32].Matanda M., Jenvey V. B., and Phillips J. G., “Internet use in adulthood: Loneliness, computer anxiety and education,” Behavior Change, vol. 21, no. 2, pp. 103–114, 2004. [Google Scholar]
- [33].Morahan-Martin J. and Schumacher P., “Loneliness and social uses of the Internet,” Comput. Human Behavior, vol. 19, no. 6, pp. 659–671, 2003. [Google Scholar]
- [34].Austin D., Cross R. M., Hayes T., and Kaye J., “Regularity and predictability of human mobility in personal space,” PLoS ONE, vol. 9, no. 2, p. e90256, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Dodge H. H., Mattek N. C., Austin D., Hayes T. L., and Kaye J. A., “In-home walking speeds and variability trajectories associated with mild cognitive impairment,” Neurology, vol. 78, pp. 1946–1952, Jun. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Hagler S., Austin D., Hayes T. L., Kaye J., and Pavel M., “Unobtrusive and ubiquitous in-home monitoring: A methodology for continuous assessment of gait velocity in elders,” IEEE Trans. Biomed. Eng., vol. 57, no. 4, pp. 813–820, Nov. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Skubic M., Guevara R. D., and Rantz M., “Automated health alerts using in-home sensor data for embedded health assessment,” IEEE J. Transl. Eng. Health Med., vol. 3, 2015, Art. no. 2700111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Barberger-Gateau P., Commenges D., Gagnon M., Letenneur L., Sauvel C., and Dartigues J. F., “Instrumental activities of daily living as a screening tool for cognitive impairment and dementia in elderly community dwellers,” J. Amer. Geriatrics Soc., vol. 40, no. 11, pp. 1129–1134, 1992. [DOI] [PubMed] [Google Scholar]
- [39].Petersen J., Thielke S., Austin D., and Kaye J., “Phone behaviour and its relationship to loneliness in older adults,” Aging Mental Health, pp. 1–8, Jul. 2015. [DOI] [PMC free article] [PubMed]
- [40].Buracchio T., Dodge H. H., Howieson D., Wasserman D., and Kaye J., “The trajectory of gait speed preceding mild cognitive impairment,” Arch. Neurol., vol. 67, no. 8, pp. 980–986, Aug. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kaye J., et al. , “One walk a year to 1000 within a year: Continuous in-home unobtrusive gait assessment of older adults,” Gait Posture, vol. 35, no. 2, pp. 197–202, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hayes T. L., Hagler S., Austin D., Kaye J., and Pavel M., “Unobtrusive assessment of walking speed in the home using inexpensive PIR sensors,” in Proc. 31st Annu. Int. Conf. IEEE Eng. Med. Biol. Soc., Minneapolis, MN, USA, 2009, pp. 7248–7251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Campbell I. H., et al. , “Measuring changes in activity patterns during a norovirus epidemic at a retirement community,” presented at the Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. (EMBC), Boston, MA, USA, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Folstein M. F., Folstein S. E., and McHugh P. R., “‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician,” J. Psychiatric Res., vol. 12, no. 3, pp. 189–198, 1975. [DOI] [PubMed] [Google Scholar]
- [45].Hollingshead A., unpublished. [Google Scholar]
- [46].Russell D. W., “UCLA loneliness scale (version 3): Reliability, validity, and factor structure,” J. Pers. Assess, vol. 66, pp. 20–40, Feb. 1996. [DOI] [PubMed] [Google Scholar]
- [47].Burholt V. and Scharf T., “Poor health and loneliness in later life: The role of depressive symptoms, social resources, and rural environments,” J. Gerontol. B, Psychol. Sci. Soc. Sci., vol. 69, pp. 311–324, Mar. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Rabe-Hesketh S. and Skrondal A., Multilevel and Longitudinal Modeling Using Stata, vol. 1 College Station, TX, USA: STATA Press, 2008. [Google Scholar]
- [49].Allison P. (Nov. 1, 2012). When Can You Safely Ignore Multicollinearity? [Online]. Available: http://www.statisticalhorizons.com/multicollinearity [Google Scholar]
- [50].Ziegler F. and Schwanen T., “‘I like to go out to be energised by different people’: An exploratory analysis of mobility and wellbeing in later life,” Ageing Soc., vol. 31, pp. 758–781, Jul. 2011. [Google Scholar]
- [51].Kaspar R., Oswald F., Wahl H.-W., Voss E., and Wettstein M., “Daily mood and out-of-home mobility in older adults: Does cognitive impairment matter?” J. Appl. Gerontol., Nov. 2012. [DOI] [PubMed]
- [52].Petersen J., et al. , “Longitudinal relationship between loneliness and social isolation in older adults: Results from the cardiovascular health study,” J. Aging Health, Oct. 2015. [DOI] [PMC free article] [PubMed]
- [53].Fokkema T. and Knipscheer K., “Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults,” Aging Mental Health, vol. 11, pp. 496–504, Sep. 2007. [DOI] [PubMed] [Google Scholar]
- [54].Shapira N., Barak A., and Gal I., “Promoting older adults’ well-being through Internet training and use,” Aging Mental Health, vol. 11, pp. 477–484, Sep. 2007. [DOI] [PubMed] [Google Scholar]
- [55].White H., et al. , “A randomized controlled trial of the psychosocial impact of providing Internet training and access to older adults,” Aging Mental Health, vol. 6, pp. 213–221, Aug. 2002. [DOI] [PubMed] [Google Scholar]
- [56].Caplan S. E., “Relations among loneliness, social anxiety, and problematic Internet use,” CyberPsychol. Behavior, vol. 10, no. 2, pp. 234–242, 2006. [DOI] [PubMed] [Google Scholar]
- [57].Ceyhan A. A. and Ceyhan E., “Loneliness, depression, and computer self-efficacy as predictors of problematic Internet use,” Cyberpsychol. Behavior, vol. 11, no. 6, pp. 699–701, 2008. [DOI] [PubMed] [Google Scholar]
- [58].Morahan-Martin J., “The relationship between loneliness and Internet use and abuse,” Cyberpsychol. Behavior, vol. 2, no. 5, pp. 431–439, 1999. [DOI] [PubMed] [Google Scholar]
- [59].Cornwell B. and Laumann E. O., “The health benefits of network growth: New evidence from a national survey of older adults,” Soc. Sci. Med., vol. 125, pp. 94–106, Jan. 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Pinquart M. and Sorensen S., “Influences on loneliness in older adults: A meta-analysis,” Basic Appl. Soc. Psychol., vol. 23, no. 4, pp. 245–266, Jan. 2013. [Google Scholar]
- [61].Savikko N., Routasalo P., Tilvis R. S., Strandberg T. E., and Pitkälä K. H., “Predictors and subjective causes of loneliness in an aged population,” Arch. Gerontol. Gerontol., vol. 41, pp. 223–233, Nov-Dec 2005. [DOI] [PubMed] [Google Scholar]
- [62].Cohen-Mansfield J., Shmotkin D., and Goldberg S., “Loneliness in old age: Longitudinal changes and their determinants in an Israeli sample,” Int. Psychogeriatrics, vol. 21, pp. 1160–1170, Dec. 2009. [DOI] [PubMed] [Google Scholar]
- [63].Stewart M., Craig D., MacPherson K., and Alexander S., “Promoting positive affect and diminishing loneliness of widowed seniors through a support intervention,” Public Health Nursing, vol. 18, pp. 54–63, Jan-Feb 2001. [DOI] [PubMed] [Google Scholar]
- [64].Wenger G. C., Davies R., Shahtahmasebi S., and Scott A., “Social isolation and loneliness in old age: Review and model refinement,” Ageing Soc., vol. 16, no. 3, pp. 333–358, 1996. [Google Scholar]
- [65].Segrin C. and Passalacqua S. A., “Functions of loneliness, social support, health behaviors, and stress in association with poor health,” Health Commun., vol. 25, pp. 312–322, Jun. 2010. [DOI] [PubMed] [Google Scholar]
- [66].Tornstam L., “Dimensions of loneliness,” Aging Clin. Experim. Res., vol. 2, no. 3, pp. 259–265, Sep. 1990. [DOI] [PubMed] [Google Scholar]
- [67].Ernst J. M. and Cacioppo J. T., “Lonely hearts: Psychological perspectives on loneliness,” Appl. Preventive Psychol., vol. 8, no. 1, pp. 1–22, 2000. [Google Scholar]
- [68].Schnittger R. I., Wherton J., Prendergast D., and Lawlor B. A., “Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults,” Aging Mental Health, vol. 16, no. 3, pp. 335–346, 2012. [DOI] [PubMed] [Google Scholar]
- [69].Fees B. S., Martin P., and Poon L. W., “A model of loneliness in older adults,” J. Gerontol. B, Psychol. Sci. Soc. Sci., vol. 54, pp. P231–P239, Jul. 1999. [DOI] [PubMed] [Google Scholar]
- [70].Banks M. R. and Banks W. A., “The effects of animal-assisted therapy on loneliness in an elderly population in long-term care facilities,” J. Gerontol. A, Biol. Sci. Med. Sci., vol. 57, pp. M428–M432, Jul. 2002. [DOI] [PubMed] [Google Scholar]
- [71].Masi C. M., Chen H. Y., Hawkley L. C., and Cacioppo J. T., “A meta-analysis of interventions to reduce loneliness,” Pers. Soc. Psychol. Rev., vol. 15, pp. 219–266, Aug. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Keil C. P., “Loneliness, stress, and human-animal attachment among older adults,” in Companion Animals in Human Health. 1998, pp. 123–134.
- [73].Dodge H. H., et al. , “Characteristics associated with willingness to participate in a randomized controlled behavioral clinical trial using home-based personal computers and a webcam,” Trials, vol. 15, p. 508, Dec. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Giger J. T., et al. , “Remote patient monitoring acceptance trends among older adults residing in a frontier state,” Comput. Human Behavior, vol. 44, pp. 174–182, Mar. 2015. [Google Scholar]