Abstract
Purpose
To investigate primary physician awareness of the California Breast Density Notification Law and its impact on primary care practice.
Materials and Methods
An online survey was distributed to 174 physicians within a single primary care network system 10 months after California’s breast density notification law took effect. The survey assessed physicians’ awareness of the law, perceived changes in patient levels of concern about breast density, and physician comfort levels in breast density management issues.
Results
The survey was completed by 77 physicians (45%). Roughly half of those surveyed (49%) reported no knowledge of the breast density notification legislation. Only 32% of respondents noted an increase in patient levels of concern about breast density compared to prior years. The majority were only “somewhat comfortable” (52%) or “not comfortable” (10%) with breast density questions, and almost one-third (32%) had referred patients to a breast health clinic for these discussions. 75% of those surveyed would be interested in more specific education on the subject.
Conclusion
Awareness of California’s Breast Density Notification Law among primary care clinicians is low, and many do not feel comfortable answering breast density related patient questions. Breast imagers and institutions may need to devote additional time and resources to primary physician education in order for density notification laws to have significant impact on patient care.
Keywords: dense breasts, legislation, mammography, screening
Summary sentence
Enactment of breast density notification laws without the provision of adequate primary physician education and resources is unlikely to significantly impact patient care.
INTRODUCTION
Patient notification of breast density is controversial. In 2009, Connecticut was the first state to mandate patient notification of dense breast tissue. Since then, 18 additional states have enacted similar laws, although unlike Connecticut, the vast majority of these states do not require health insurance reimbursement for supplemental screening tests. Many additional states are currently in the process of passing similar legislation, and federal legislation regarding breast density notification is currently under review by a congressional committee. [1,2]
The California Breast Density Notification Law (SB 1538), effective April 2013, requires the following language be included in the lay letter sent to patients notifying them of their mammogram results:
“Your mammogram shows that your breast tissue is dense. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer.
This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your doctor. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.” [3]
Dense tissue is defined as either “heterogeneously dense” or “extremely dense” BI-RADS categories based on a qualitative assessment by the radiologist [4]. Roughly 50% of women in national studies have breast tissue that is classified as mammographically “dense”; thus approximately 2 million women in the state of California receive this notification annually.[5–7]
With the enactment of breast density notification laws, primary physicians are expected to encounter increased patient concerns regarding their breast density as well as new related management dilemmas. The issues related to breast density include: 1) increased breast cancer risk associated with dense breasts [8,9], 2) decreased sensitivity of mammograms in women with dense breasts, also known as “masking” [10,11] and 3) the utility of supplemental screening modalities, such as ultrasound, MRI and tomosynthesis [12–16]. These are not topics that have traditionally been included in primary physician training programs or even in continuing medical education courses.
The breast density laws enacted in California and other states require an action by radiologists which has little impact on patient care unless it is apprehended and understood by primary clinicians. While radiologist compliance with the law is straightforward and presumably very high, the actual consequences for patients and primary physicians have not been studied. With that in mind, our study investigates primary physicians’ awareness of the law, its impact on patient concerns regarding breast density, and physician comfort level in discussing issues of breast density.
METHODS
Survey Design and Contents
A multiple-choice question survey was designed with a combination of yes/no, multiple-choice, and Likert style questions progressionally ordered in highest to lowest response degree (Table 1). Respondents remained anonymous, but demographic data including gender, subspecialty, and years in practice were collected.
Table 1.
California Breast Density Legislation Survey Questions and Response Options
| # | Question | Response Options |
|---|---|---|
| 1 | Were you aware, prior to this survey, of the recent (2013) California state law requiring that patients be informed of their breast density in their mammogram result letters? |
|
| 2 | Have you noticed any change in patient levels of concern about breast density in the last 6 months compared with prior years? |
|
| 3 | How often do you answer questions about breast density related to a mammogram letter? |
|
| 4 | In the last 6 months, have patients asked you about (choose all that apply) |
|
| 5 | Do you perform quantitative breast cancer risk assessments (ie assessments using Gail, Claus, BRCAPRO or other standard risk models) in your office? |
|
| 6 | Do you refer patients to the UCD Breast Health Clinic if you think they would benefit from a risk assessment? |
|
| 7 | Do you refer patients to the UCD Breast Health Clinic to discuss questions related to their mammographic breast density? |
|
| 8 | If yes, how often? |
|
| 9 | How comfortable do you feel answering patient questions about breast density? |
|
| 10 | Would you be interested in attending a brief educational presentation about breast density and its impact on breast cancer screening? |
|
Survey Sample and Administration
The survey was distributed to 174 Internal Medicine, Family Medicine, and Obstetric-Gynecology outpatient physicians at a single academic medical center in February 2014, 10 months after California’s breast density law took effect. Survey data collection and analysis was performed using SurveyMonkey (Palo Alto, California) web-based software. Additional analyses were conducted using SAS® software version 9.3 (SAS Institute, Cary, NC) using Fishers Exact Test to test for an association between gender and years of practice to survey responses. A P value of <0.05 value was considered statistically significant.
RESULTS
The survey was completed by 77 physicians, representing a 44% response rate. 39% of respondents were from Internal Medicine, 47% were from Family Medicine, and 9% were from Obstetrics-Gynecology departments. A slight majority (53%) were female. 72% had been practicing for greater than 10 years.
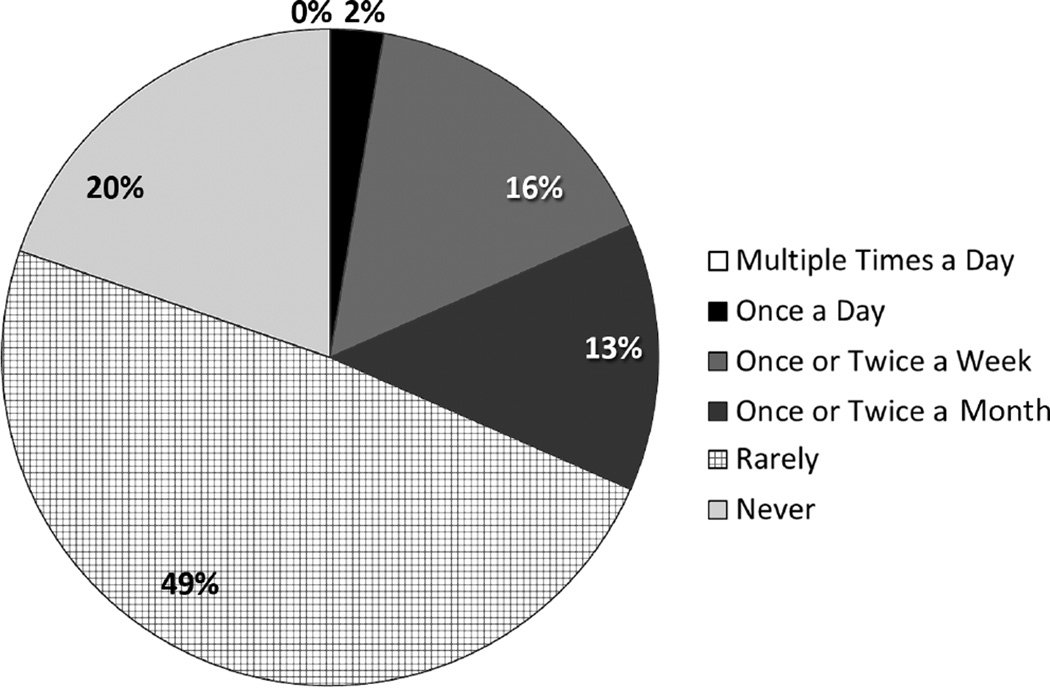
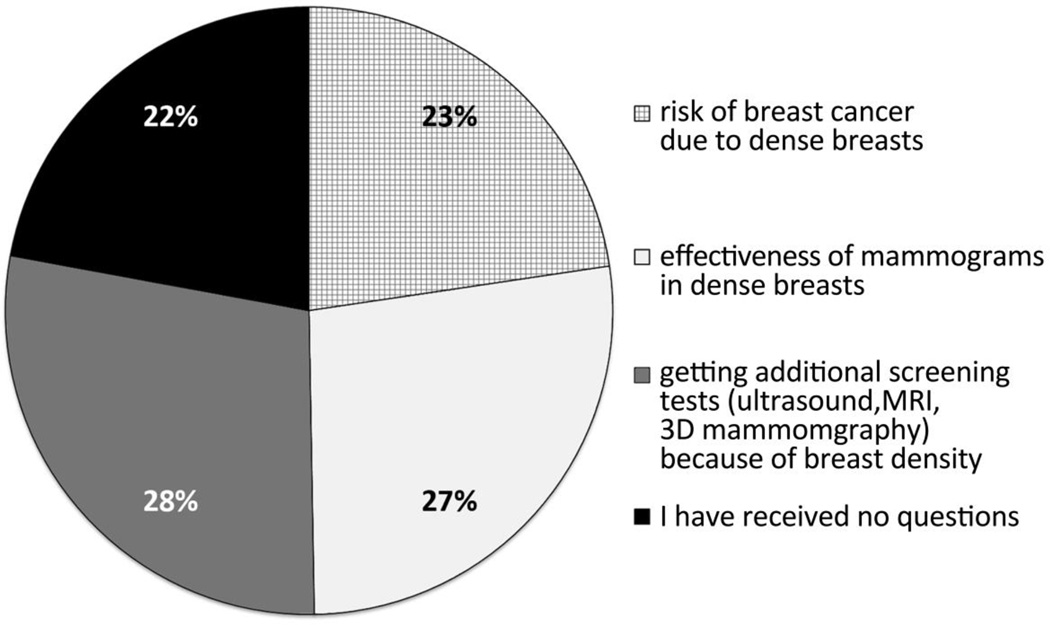
49% of responding physicians were not aware of the Breast Density legislation prior to taking the survey. Only about a third (32%) reported a change in patient levels of concern about breast density after April 1, 2013 compared to prior years. Most rarely answered questions regarding breast density related to a mammography result letter (Fig 1) and nearly a quarter of responding physicians reported that they never answer questions related to breast density. The number of patient questions related to the subjects of breast cancer risk, effectiveness of mammograms, additional screening tests were roughly equivalent. (Fig 2)
Figure 1.
Frequency that primary care physicians reported answering questions about breast density related to a mammogram letter. No respondents answered “multiple times a day” (white box in chart legend).
Figure 2.
Subjects that primary care physicians reported being asked about by patients. Multiple selections were allowed.
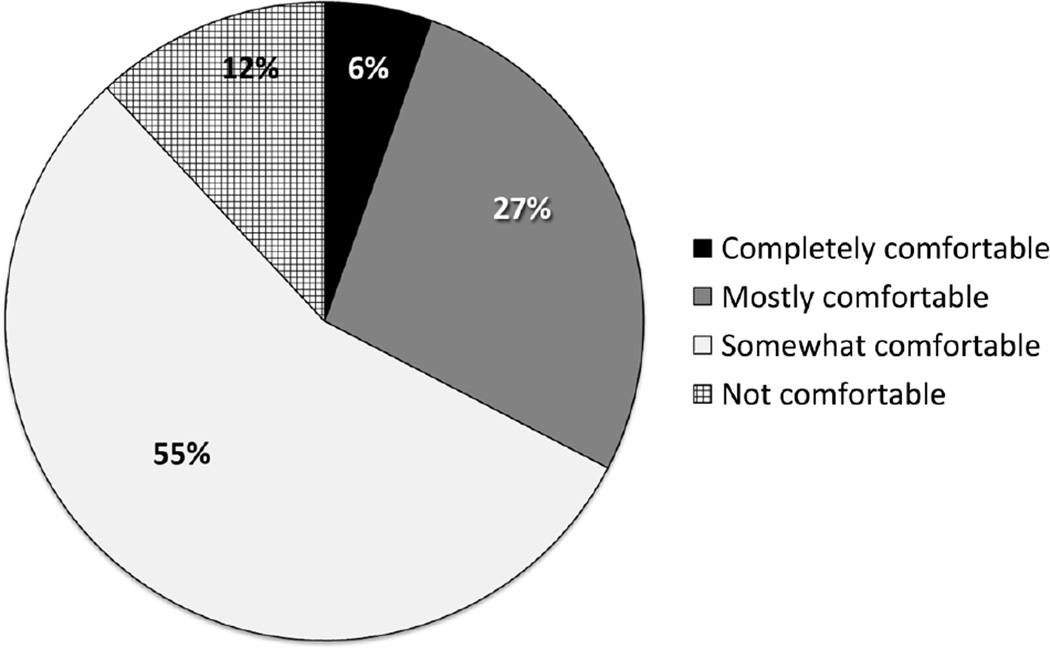
When asked about their comfort level in responding to patient questions regarding breast density, only 6% of surveyed primary physicians describe themselves as “completely comfortable” (Fig 3). About a third of physicians (32%) referred patients to the health network’s subspecialty Breast Health Clinic, which is staffed by physicians with special expertise in benign and malignant breast disease to discuss questions related to their mammographic breast density. Approximately one quarter of primary care physicians (26%) reported performing breast cancer risk assessments themselves, without statistically significant differences based on specialty. The remainder referred women to the Breast Health Clinic when they thought a risk assessment would be beneficial. The majority (75%) of surveyed primary care physicians were interested in attending a brief education presentation about breast density and its impact on breast cancer screening.
Figure 3.
Primary care physician comfort level in answering patient questions about breast density.
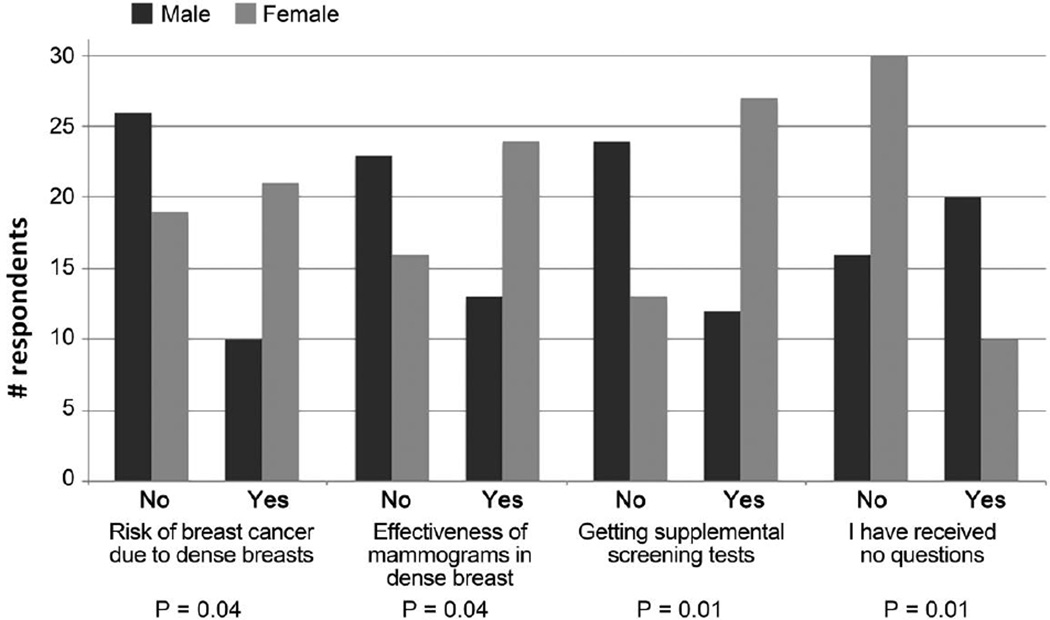
A greater percentage of female respondents (43%) compared to male (19%) respondents noticed a change in patient levels of concern about breast density in the last 6 months compared with prior years (P=0.05). Female clinician respondents reported that patients had asked more breast density specific questions during clinic visits (Fig 4). No statistically significant differences in any survey responses were seen based on years of practice.
Figure 4.
Breast density topics primary care clinicians reported patients asking in the 6 months prior to the survey (multiple selections were allowed). More female than male primary care clinicians reported that patients asked questions during clinic visits in each of these topic categories, with statistical significance (P values reported above for each question topic).
DISCUSSION
The results of this study suggest that 10 months after enactment of the California Breast Density Notification Law (SB 1538), the intent of the legislation has not been fully realized. Half of all primary physician respondents were not aware of the law’s existence and two thirds reported no change in patient levels of concern about breast density compared with prior years. The primary responsibility for compliance with the law lies with the radiologist who must add the required language to patient results letters, yet the purpose of the law is to increase patient awareness of breast density and its effect on both mammographic sensitivity and breast cancer risk. Our results suggest the law has had less success in promoting discussions between patients and primary physicians than had been anticipated.
There are likely several factors which hinder patient-physician conversations regarding breast density concerns. First, patients with dense breast tissue may not absorb the law’s mandated language in the patient letter because they are focused on their mammogram result. Those who do read and appreciate the mandated language may not be motivated to schedule a separate doctor’s appointment to discuss breast density or may have forgotten about the issue by the time of their next regular appointment. Breast density awareness and physician familiarity may also be hampered by universal factors affecting primary care, including high patient volumes, increased documentation requirements leading to shortened patient care visits, and the ever-expanding demands of staying current with scientific knowledge.
When patients do bring forward questions about breast density, the results of this survey show that many providers feel ill-equipped to fully address them. Only 30% of clinicians were completely or mostly comfortable answering breast density related questions and the vast majority of respondents felt they would benefit from educational sessions about breast density. However, primary clinicians did express strong interest in further education, which potentially could be provided to small group sessions by breast imagers, or by online resources such as those developed by the California Breast Density Information Group (CBDIG) [5].
One of the areas that such educational sessions could address is the complex issue of breast cancer risk assessment. Risk assessment aids primary clinicians in deciding which of the many women with dense breasts would benefit from supplemental screening, which is ultimately the goal of the legislation [5]. However, the majority (74%) of primary clinicians did not report performing quantitative risk assessments on their own, rather deferring them to a breast health specialist.
Our survey also highlighted the gender gap in the physician comfort levels related to breast health. We found that significantly more female physicians noted increased concern among their patients regarding breast density. Studies have shown that female physicians spend more time with patients [17–19] and are more prevention-focused compared to male physicians [20]. Primary clinicians should be aware of these gender-based differences and should seek to reduce them.
This study has limitations. First, it was conducted at a single institution and may not be generalizable. Since the respondents are all affiliated with an academic medical center, it is possible that the reported physician familiarity with the law and comfort level in dealing with patient queries may be higher than in general practice. This center also has a Breast Health Clinic, staffed by experts, to which patients can be referred for formal risk assessment and breast density questions, and this resource may impact the way that primary clinicians handle breast related patient questions. Finally, the survey asked respondents to recall their general practice pattern over the previous 10 months, which might lead to inaccuracies.
In conclusion, our study indicates that the enactment of a breast density notification law alone has not resulted in familiarity of the issues related to breast density among primary care clinicians in California. Our findings have implications for similar laws now under consideration and for whether California’s law should be reauthorized after its sunset date in 2019. In order for such laws to have an impact on health practices, increased time and resources will need to be devoted to primary physician education, or institutions may need to consider alternative strategies for managing and assisting patients with issues related to breast density.
TAKE-HOME POINTS.
Half of all primary physician respondents were unaware of the California breast density law’s existence and only 5% felt “completely comfortable” answering patient breast density questions, 10 months after enactment.
The majority of primary physician respondents surveyed were more comfortable referring complex questions regarding breast cancer risk assessments and breast density to a dedicated breast health clinic.
Increased patient awareness is beneficial only if primary care clinicians feel they have sufficient knowledge to counsel patients regarding their risk of breast cancer and the advisability of supplemental screening. Primary physicians desire education about breast density. Methods of education deserve further attention and study.
Footnotes
No disclosures
REFERENCES
- 1.Dehkordy SF, Carlos RC. Dense breast legislation in the United States: state of the states. J Am Coll Radiol. 2013;10:899–902. doi: 10.1016/j.jacr.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 2. [Accessed July 17, 2014];House Resolution 3403: Breast Density and Mammography Reporting Act of 2013. Available at: http://www.govtrack.us/congress/bills/113/hr3404 http://www.govtrack.us/congress/bills/113/hr3403.
- 3. [Accessed July 17, 2014];California Senate Bill No. 1538 Healthcare: mammograms. Available at: http://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201120120SB1538&search_keywords.
- 4.D'Orsi CJ, Mendelson EB, Ikeda DM. ACR breast imaging and reporting data system : breast imaging atlas. Reston, VA: American College of Radiology; 2003. [Google Scholar]
- 5.Price ER, Hargreaves J, Lipson JA, et al. The California breast density information group: a collaborative response to the issues of breast density, breast cancer risk, and breast density notification legislation. Radiology. 2013;269:887–892. doi: 10.1148/radiol.13131217. [DOI] [PubMed] [Google Scholar]
- 6. [Accessed on May 11 2014];U.S. Census Bureau state and county quickfacts. Available at http://quickfacts.census.gov/qfd/states/06000.html.
- 7. [Accessed on May 11 2014];NCI-funded Breast Cancer Surveillance Consortium Web site. Available at http://breastscreening.cancer.gov/data/mammography_data.html.
- 8.McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1159–1169. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 9.Vacek PM, Geller BM. A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomarkers Prev. 2004;13:715–722. [PubMed] [Google Scholar]
- 10.Whitehead J, Carlile T, Kopecky KJ, et al. Wolfe mammographic parenchymal patterns. A study of the masking hypothesis of Egan and Mosteller. Cancer. 1985;56:1280–1286. doi: 10.1002/1097-0142(19850915)56:6<1280::aid-cncr2820560610>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 11.Jackson VP, Hendrick RE, Feig SA, Kopans DB. Imaging of the radiographically dense breast. Radiology. 1993;188:297–301. doi: 10.1148/radiology.188.2.8327668. [DOI] [PubMed] [Google Scholar]
- 12.Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology. 2012;265:59–69. doi: 10.1148/radiol.12120621. [DOI] [PubMed] [Google Scholar]
- 13.Leconte I, Feger C, Galant C, et al. Mammography and subsequent whole-breast sonography of nonpalpable breast cancers: the importance of radiologic breast density. AJR Am J Roentgenol. 2003;180:1675–1679. doi: 10.2214/ajr.180.6.1801675. [DOI] [PubMed] [Google Scholar]
- 14.Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75–89. doi: 10.3322/canjclin.57.2.75. [DOI] [PubMed] [Google Scholar]
- 15.Berg WA, Zhang Z, Lehrer D, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. Jama. 2012;307:1394–1404. doi: 10.1001/jama.2012.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mainiero MB, Lourenco A, Mahoney MC, et al. ACR Appropriateness Criteria Breast Cancer Screening. J Am Coll Radiol. 2013;10:11–14. doi: 10.1016/j.jacr.2012.09.036. [DOI] [PubMed] [Google Scholar]
- 17.Roter D, Lipkin M, Jr, Korsgaard A. Sex differences in patients' and physicians' communication during primary care medical visits. Med Care. 1991;29:1083–1093. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 19.Hall JA, Blanch-Hartigan D, Roter DL. Patients' satisfaction with male versus female physicians: a meta-analysis. Med Care. 2011;49:611–617. doi: 10.1097/MLR.0b013e318213c03f. [DOI] [PubMed] [Google Scholar]
- 20.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993;329:478–482. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]