Abstract
Study Design
Narrative review.
Objective
The study aims to critically review the outcomes associated with the surgical repair or conservative management of spondylolysis in athletes.
Methods
The English literature listed in MEDLINE/PubMed was reviewed to identify related articles using the term “spondylolysis AND athlete.” The criteria for studies to be included were management of spondylolysis in athletes, English text, and no year, follow-up, or study design restrictions. The references of the retrieved articles were also evaluated. The primary outcome was time to return to sport. This search yielded 180 citations, and 25 publications were included in the review.
Results
Treatment methods were dichotomized as operative and nonoperative. In the nonoperative group, 390 athletes were included. A combination of bracing with physical therapy and restriction of activities was used. Conservative measures allowed athletes to return to sport in 3.7 months (weighted mean). One hundred seventy-four patients were treated surgically. The most common technique was Buck's, using a compression screw (91/174). All authors reported satisfactory outcomes. Time to return to play was 7.9 months (weighted mean). There were insufficient studies with suitably homogenous subgroups to conduct a meta-analysis.
Conclusion
There is no gold standard approach for the management of spondylolysis in the athletic population. The existing literature suggests initial therapy should be a course of conservative management with thoracolumbosacral orthosis brace, physiotherapy, and activity modification. If conservative management fails, surgical intervention should be considered. Two-sided clinical studies are needed to determine an optimal pathway for the management of athletes with spondylolysis.
Keywords: spondylolysis in athletes, surgical treatment, conservative treatment
Introduction
Spondylolysis is a defect of the pars interarticularis of the lumbar vertebrae causing between 70 and 80% of low back pain within adolescent athletes.1 2 3 It predicates spondylolisthesis and long-term complications including neural compression.4 Although genetic factors have been implicated, the major etiologic factor of spondylolysis remains repetitive stress fractures associated with sport. Sports such as cricket,5 gymnastics,6 and athletics,7 8 which particularly involve hyperextension and rotation of the lumbar vertebrae, expose the posterior elements of the immature spine to develop spondylolysis.1 Although definitive nonsurgical therapy remains the treatment of choice for most patient groups, athletes may require structural repair of their defect to allow for rapid return to normal activities with minimal recovery time.9
There is a relatively robust body of studies reporting on nonoperative and surgical treatment of spondylolysis in the subpopulation of athletes; however, the quality and strength of the data vary. We provide a targeted narrative review of the current state of literature to help provide guidance toward a more streamlined management pathway since Buck first described his surgical procedure for treatment of spondylolysis in 1970.18
This study aims to review the outcomes for the athletic population with spondylolysis following surgical repair or conservative management.
Materials and Methods
The literature listed in PubMed was reviewed to identify related articles using the keywords “spondylolysis AND athlete.” All retrieved abstracts were reviewed by two authors (P.P. and N.S.N.) and assessed with regards to inclusion criteria. These included all studies investigating the management of radiologically diagnosed (using computed tomography [CT], magnetic resonance imaging [MRI], or single-photon emission computed tomography) spondylolysis (unilateral, bilateral, single or multiple levels) of the lumbar spine in athletes (individuals competing in any regular organized sporting activities, at any level, e.g., high school/college/professional). The management techniques considered are explained in detail. Studies had to be published in English, with no restrictions regarding year of publication. Although the ideal follow-up period when assessing outcomes following spondylolysis treatment would be 2 years, we chose a more inclusive approach and did not specify a minimum follow-up period. However, the length of study follow-up and other methodological limitations were highlighted in the results. Furthermore, due to the paucity of research in this area, all study designs were considered for inclusion, including randomized controlled trials, nonrandomized controlled trials, quasi-experimental, pre- and posttreatment studies, prospective and retrospective cohort studies, case–control studies, analytical cross-sectional studies, and descriptive epidemiologic study designs such as case series, individual case reports, and descriptive cross-sectional studies.
Titles and abstracts of all citations were reviewed. Full articles of citations adhering to inclusion criteria and those that were uncertain were reviewed. The references of these retrieved articles were also evaluated to identify further appropriate studies to be included in the review.
The data extracted included patient demographics (age, gender, athlete type, and sport); sample size; follow-up period; conservative or operative management; bilateral or unilateral defects; number of levels involved; fusion rates (number of cases fused); complications; and time to return to sport. Function and pain were secondary outcomes for this review. Not all studies included this data, but the data was extracted where available. Study-specific outcomes included level of sporting activity after treatment, radiographic results (poor, fair, good), and reported pain levels. Various functional pain and disability scales specific to this injury were also included (e.g., Short Form 36 [SF-36]; Japanese Orthopaedic Association (JOA) score; Oswestry Disability Index [ODI] for low back pain). All objective and subjective measures were included.
The electronic search yielded 180 citations, which were reviewed with relevant references, and 25 publications met our stated inclusion criteria. We had planned to undertake meta-analyses if three or more studies with sufficiently homogenous two-sided subgroups were found. However, such studies were not found, so meta-analyses were not undertaken.
Overview of Management Techniques
Conservative Treatment
Orthoses, defined as external devices applied to the body to restrict motion,10 have played an integral role in management of different spine pathologies for a long time.11 Thoracolumbosacral orthoses (TLSOs) and lumbosacral orthoses (LSOs) are available in flexible and rigid variations. LSOs extend from the pelvis to the xiphoid anteriorly and the inferior angle of the scapula posteriorly. TLSOs extend higher, generally to the midscapular level.12
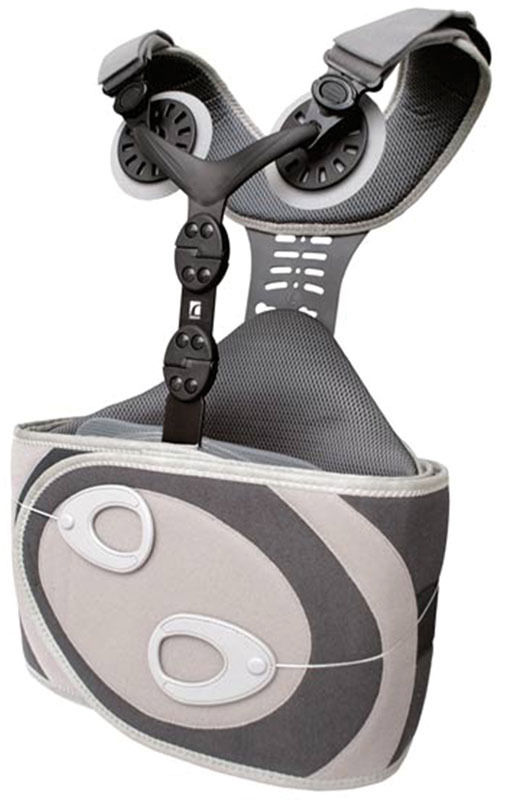
Flexible (nonrigid) TLSOs and LSOs (Fig. 1) have been frequently prescribed for the treatment of low back pain. These corset-style devices are adjustable by means of laces, hooks, or Velcro straps. It is believed that these types of orthoses decrease the myoelectric activity of the paraspinal and abdominal muscles and increase intra-abdominal pressure.13 14
Fig. 1.

Non rigid lumbar brace. (Reproduced with permission, from Ossur UK Ltd.)
Rigid TLSOs (Fig. 2) and LSOs (Fig. 3) are effective in limiting motion in the sagittal plane but have limited control over rotation and lateral bending.15 They can be broadly categorized into molded (prefabricated, custom made) and nonmolded (over-the-shelf) types. The Jewett hyperextension brace (Fig. 4) is an example of a nonmolded TLSO brace. It applies three-point fixation to the torso through anterior pads on the symphysis pubis and sternum and a posterior pad midway between the anterior pads and places the spine in slight extension. If immobilization distal to L4 is necessary, a thigh cuff should be added to the orthosis to control pelvic motion.13 16
Fig. 2.
Thoracolumbosacral orthosis brace. (Reproduced with permission, from Ossur UK Ltd.)
Fig. 3.

Lumbosacral orthosis brace. (Reproduced with permission, from Ossur UK Ltd.)
Fig. 4.

Jewett brace. (Reproduced with permission, from Ossur UK Ltd.)
LSOs are often prescribed for treatment after arthrodesis for degenerative conditions. Several studies demonstrated little or no immobilizing effect from wearing LSOs and possibly an increase in L4–L5, L5–S1 motion after application of these orthoses.13 17
Surgical Treatment
Current recommended practice requires that patients first undergo a period of conservative treatment prior to surgical intervention.
The Buck procedure,18 the first surgical technique designed specifically to repair a defect in the pars interarticularis, utilizes a 3.5-mm lag screw fixation technique passing through the pars interarticularis to compress the defect (Figs. 5 and 6).
Fig. 5.
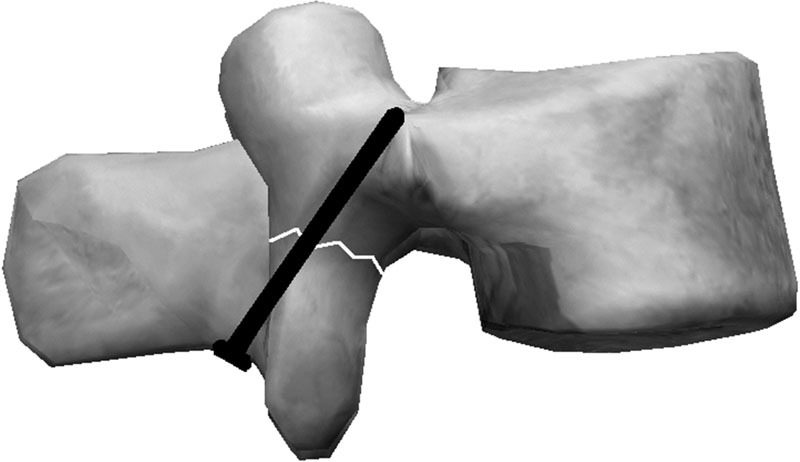
Buck procedure.
Fig. 6.
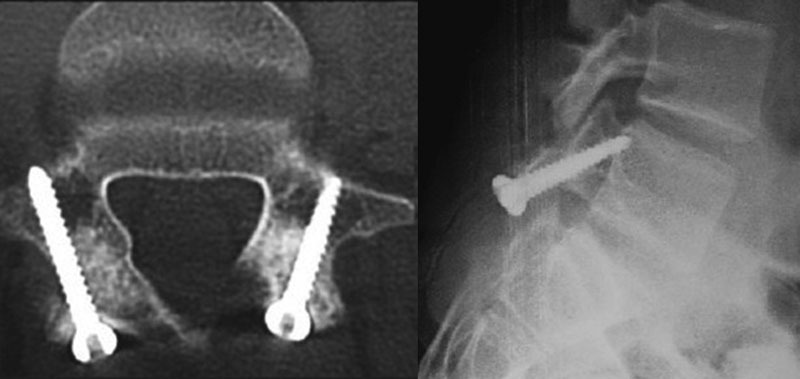
Buck procedure. Axial computed tomography and lateral X-ray. (Reproduced with permission from The Indian Journal of Orthopaedics, Wolters Kluwer.)
Adaptations to this technique have been made for patients with low bone density or dysplastic lamina. Morscher et al described using hook screw fixation to correct spondylolysis defects19; however, this technique has been described as technically difficult.20 The technique involves bone grafts to fill the pars defect followed by screws inserted into the superior articular processes bilaterally. These screws are altered such that they accommodate a hook, which hangs over the lamina, which is later secured by a lock nut. This apparatus is fixed to adequately reduce the defect.21
A further variant of the screw fixation, the pedicle screw hook fixation, involves the pedicle as a reference of fixation.22 A pedicle screw is inserted and sublaminar hooks are joined to the pedicle screws using titanium rods.
Conversely, the Scott technique (Fig. 7) involves a wire passed through the transverse processes of the vertebrae and tightened around the spinous processes to supplement autologous bone graft repair of the defect by providing compression and stabilization to the defect.23
Fig. 7.
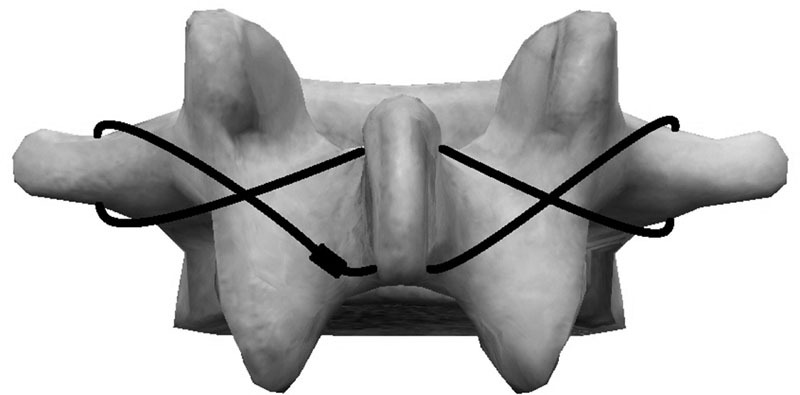
Scott procedure.
A combination of cable and wire fixation has been described by both Salib and Pettine24 and Songer and Rovin.25 This pedicle screw cable fixation technique utilizes pedicle screws as an anchor to hold an iliac crest graft within the pars defect. A cable is then fed from underneath the contralateral lamina around the ipsilateral pedicle screw head and finally secured around the spinous process. This cable fixation is repeated bilaterally and cable ends are tightened together to reduce the defect under tension.
Results
Twenty-five studies met our inclusion criteria for this narrative review. The treatment methods were dichotomized into operative and conservative. The outcomes were evaluated clinically as listed in Table 1.26
Table 1. Criteria for clinical evaluation.
| Excellent | No pain |
| No brace requirement | |
| Full activities, including sports | |
| Good | Occasional aching with vigorous activity |
| No brace requirement | |
| Full activities, including sports | |
| Fair | Pain with vigorous activity |
| Occasional use of brace | |
| Activities of daily living without pain | |
| Poor | Pain during activities of daily living even with brace |
Nonoperative Management
Eleven publications described nonoperative management of spondylolysis in athletes,6 7 27 28 29 30 31 32 33 34 35 totaling 390 athletes with a mean age of 16.2 years (Table 2). Two authors did not mention sex in their studies; despite this omission, the ratio of men to women was ∼2:1 (201:109). The four most common sports mentioned were soccer, basketball, American football, and gymnastics.
Table 2. Conservative management of athletes with spondylolysis.
| Authors and year | No. of patients | Method | Average duration of treatment (mo) | Mean age (y) | Average F/U (mo) | Patients with bilateral, unilateral defects | No. of vertebral level | Union rates | Outcomes | Average return to play (mo) |
|---|---|---|---|---|---|---|---|---|---|---|
| Micheli et al 198030 | 12 | TLSO brace (Boston) | 4–24 | Adolescent | 15 | N/A | N/A | N/A | 67% excellent, 33% good | N/A |
| Pettine et al 199332 | 1 | TLSO brace and electric stimulation | 6 | 17 | 22 | 1 bilateral | 1 L4 | 100% | Excellent | 6 |
| Blanda et al 19937 | 62 | Lumbosacral bracec | 4 | 15.5 | 50.4 | 37 bilateral; 23 unilateral | 53 L5, 9 L4 | 37% | 84% excellent, 12% good, 4% fair | N/A |
| Fellander-Tsai and Micheli 199828 | 2 | TLSO brace (Boston) and electric stimulation | 21 | 16 | 15.5 | 2 bilateral | 2 L5 | 100% | 100% excellent | 16.5 |
| Sys et al 200135 | 28 | TLSO brace (Boston) | 4 | 17.2 | 13.2 | 9 bilateral; 11 unilateral; 8 pseudobilaterala | 19 L5, 5 L4, 2 L3, 1 L2, 1 L4 and L5 | Bilateral 57%; unilateral 25%; nonunion 18% | 82% excellent, 11% good, 7% fair | 89.3% in 5.5 |
| d'Hemecourt et al 200227 | 73 | TLSO brace (Boston) | 6 | 15.7 | 48 | 35 bilateral; 30 unilateral | 48 L5, 9 L4, 8 L3, 8 PEOb | N/A | 77% good or excellent | N/A |
| Miller et al 200431 | 32 | Combination of nonrigid and rigid braces | 2.5 | 24 | 108 | Patients 11/32; 7 bilateral; 4 unilateral | Patients 11/32; 7 L5, 3 L4, 1 L3 | Patients 11/32; 7 bilateral nonunion; 4 unilateral union | 91% good or excellent, 9% fair | 2.5 |
| Iwamoto et al 200429 | 40/104 | Patents: 40/104; lumbosacral brace | Patents: 40/104; 5.4 | 20.7 | Patents: 40/104; 11.4 | 93 bilateral; 11 unilateral | 92 L5, 9 L4, 2 L3, 1 L2 | N/A | Patients 40/104; 87.5% good or excellent | Patients 35/104; 5.4 |
| Vrable and Sherman 20096 | 1 | LSO brace, PEMF bone stimulation | 1.5 | 15 | 24 | 1 bilateral | 1 L5 | 100% | 100% excellent | 3 |
| Sutton et al 201234 | 7 | TLSO braced | 3 | 20 | 24 | N/A | N/A | N/A | 29% excellent, 71% fair or poord | 3 |
| El Rassi et al 201333 | 132 | Bracing/activity modification | 3 | 13 | 48 | Bilateral 105; unilateral 27 | 110 L5, 14 L4, 3 L3, 1 L2, 4 multiple | 35% | 36.4% excellent, 56.1% good, 4.5% fair, 3% poor | 3 |
Abbreviations: F/U, follow-up; N/A, not applicable; PEMF, pulsed electromagnetic field; TLSO, thoracolumbosacral orthosis.
If tracer uptake on single-photon emission computed tomography was present on both sides of one vertebra and uptake was clearly asymmetrical, the lesion was called “pseudobilateral.”
Posterior element overuse. Single-photon emission computed tomography scan: diffuse posterior element uptake.
Nine patients underwent posterolateral fusion after failure of conservative management.
Five patients underwent surgical repair because they remained symptomatic.
The different nonoperative treatment methods that were used in these publications included TLSO and LSO braces, bone growth stimulation methods, and nonrigid braces. Most studies used a combination of methods with physical therapy and restriction of activities.
The duration of treatment ranged from 1.5 to 24 months and the mean follow-up was 45.3 months. A bilateral defect was more common than a unilateral defect. Two authors who looked at 19 patients did not report any data on the laterality of the defect. A total of 404 defects were reported: 298 were bilateral and 104 were unilateral. L5 was the most common vertebrae involved (n = 332). The union rates varied greatly, and many authors did not report it specifically because there was no radiologic confirmation. Good or excellent outcomes were reported in 344 of 390 patients. Eight publications (235/390) reported the mean return to play of the athletes; thus, the weighted mean was 3.7 months.
Outcomes of Specific Modalities
Thoracolumbosacral Orthosis
The TLSO brace was the most common method used in the conservative group. A total of 123 patients were treated with a TLSO brace. Four of the six authors (120/390) who used TLSO bracing as a treatment published results on the average return to play. These athletes returned to play in a weighted average of 5.6 months with the majority having good or excellent results. Sutton et al treated seven patients with a TLSO and physiotherapy. Five of them had surgical intervention after 3 months because their symptoms persisted.34
Lumbosacral Orthosis
Iwamoto et al,29 Blanda et al,7 and Vrable and Sherman6 used an LSO brace in their studies (103/390 patients). Iwamoto et al reported average time to return to play of 5.4 months, and all three authors presented good or excellent results in more than 80% of subjects.29
Bone Growth Stimulation
Two case reports used bone growth stimulation in the form of electric32 and pulsed electromagnetic field.6 Both studies showed excellent results.
Clinical Results of Nonoperative Management
Athletes treated conservatively returned to play in a weighted average of 3.7 months. Different conservative regimens have been described, most commonly involving use of the TLSO brace.
Micheli et al treated 12 athletes with spondylolysis using a TLSO brace and achieved good or excellent results with a treatment duration of 4 to 24 months.30 Similarly, Sys et al reported treating 28 athletes with a TLSO brace for an average treatment period of 4 months; 89.3% of these athletes returned to previous levels of competitive activities in an average of 5.5 months.35 Union of defects was found to occur more often in unilateral, active spondylolysis, and bilateral and pseudobilateral defects often failed to heal; however, interestingly, nonunion did not compromise overall morbidity or time to sport resumption in the short term.35 D'Hemecourt and colleagues have shown that acute onset of pain, hamstring tightness, and high-risk sports were associated with worse outcomes when treated with a TLSO brace.27
Treatment with an LSO brace has also been investigated as part of a study by Iwamoto et al, who looked at 104 patients with low back pain and spondylolysis.29 Forty of them were unable to continue sporting activities and were treated with LSO brace and activity modification. Of the 40 athletes, 35 were able to return to sporting activities within 5.4 months. The authors stated that bony union is not necessary to achieve a good clinical outcome as a fibrous union can provide pain relief and be acceptable for an athlete.29 Blanda et al also used LSO braces with activity modification and physiotherapy to treat 62 athletes with spondylolysis. They reported excellent results in 84% of the athletes.7
Miller et al used a protocol to treat 32 athletes. Initially the athletes used a nonrigid brace.31 For the ones who improved, a flexion-only trunk-strengthening program was started. The subjects who complained of pain were prescribed a rigid brace. Overall, the authors reported excellent or good results in 91% of the cases with an average time to return to sports of 2.5 months.
The most direct comparison between various modalities of nonoperative management including bracing, sport modification, and physical therapy was by El Rassi et al, who followed 132 athletes with spondylolysis.33 Despite poor compliance in this group, it was concluded that cessation of sporting activities for at least 3 months resulted in the most improved outcomes.
Other combination therapies have been proposed, with case reports describing union and return to play in acute spondylolysis after pulsed electromagnetic field bone stimulation6 and a small study of TLSO brace with electrical stimulation (resulting in 100% union rates in spondylolysis)28 32; however, sample sizes remained too low to demonstrate efficacy. Although a thigh cuff should be added to the orthosis to control movement if immobilization below L4 is needed, none of the studies reported any results on this technique. A thigh cuff could potentially improve the results of conservative management.
Operative Management
A total of 15 studies met the inclusion criteria describing surgical management of spondylolysis in athletes (Table 3).5 8 23 24 34 36 37 38 39 40 41 42 43 44 45 There were 174 athletes with a mean age of 22.3 years. Two authors did not mention sex. There were 117 male and 51 female athletes. The most frequent sports were cricket, soccer, and baseball.
Table 3. Operative management of athletes with spondylolysis.
| Authors and year | No. of patients | Method | Mean age (y) | Average F/U (mo) | Patients with bilateral, unilateral defects | No. of vertebral level | Complications | Union rates | Outcomes | Average return to play (mo) |
|---|---|---|---|---|---|---|---|---|---|---|
| Roca et al 198945 | 15 | Compression screw (Buck) and bone graft | 21.4 | 12–120 | N/A | 10 L5, 7 L4 | N/A | 93% | 86% good or excellent, 7% fair, 7% poor | 9 |
| Salib and Pettine 199324 | 1 | Pedicle screw with segmental wire fixation (modified Scott) and bone graft | 20 | 6 | Bilateral | L3 | N/A | 100% | 100% excellent | 6 |
| Hardcastle 19935 | 10 | Compression screw (Buck) and bone graft | 20.9 | 17.9 | 5 bilateral; 5 unilateral | 9 L5, 1 L4 | 2 wound infections | 100% | 100% excellent | N/A |
| Jarolem et al 199740 | 1 | Pedicle screws with hooks and bone graft | 15 | 24 | bilateral | L3 | N/A | N/A | 100% excellent | 12 |
| Reitman and Essis 20028 | 4 | Compression screw (Buck) and bone graft | 17.7 | 26 | N/A | 4 L5 | 1 screw breakage | N/A | 75% excellent, 25% good | 6 |
| Nozawa et al 200342 | 20 | Segmental wire fixation (Scott) and bone graft | 23.7 | 42 | N/A | 19 L5, 2 L4 | 1 wire pullout, 2 wire breakage | 100% | 75% excellent, 25% good | 12 |
| Debnath et al 200323 | 22 | 19 patients compression screw (Buck) and bone graft; 3 patients segmental wire fixation (Scott) | 20.2 | 24 | 15 bilateral; 7 unilateral | 15 L5, 3 L4, 3 L3, 1 L4 and L5 | 2 nonunions | N/A | 82% good or excellent, 18% fair or poor | 7 |
| Ranawat et al 200344 | 9/18a | Compression screw (Buck) and bone graft | 21.7 | 68 | N/A | N/A | N/A | N/A | 100% excellent | N/A |
| Ogawa et al 200743 | 7 | Segmental wire fixation (Scott) and bone graft | 26.7 | 51 | 7 bilateral | 5 patients 2 levels, 2 patients 3 levels | 1 wire breakage with pseudarthrosis | 81% | 72% excellent, 14% good, 14% fair | N/A |
| Bozarth et al 200736 | 2 | Pedicle screw with segmental wire fixation (modified Scott) and bone graft | 16.5 | 12 | 2 bilateral | 2 L5 | N/A | 100% | 100% excellent | 8 |
| Debnath et al 200738 | 8/42b | Compression screw (Buck) and bone graft | N/A | 24 | 8 unilateral | 5 L5, 1 L4, 2 L3 | N/A | N/A | ODI 39.4 to 6.4, SF-36 (PCS) 29.6 to 49.2, SF-36 (MCS) 38.7 to 54.5 | 6 |
| Brennan et al 200837 | 1 | Compression screw (Buck) | 17 | N/A | Bilateral | L5 | N/A | 100% | 100% excellent | 6 |
| Sutton et al 201234 | 5/7c | Pedicle screws with hooks and bone graft | 20 | 24 | N/A | N/A | 1 iliac crest donor site pain | N/A | 100% excellent | 6 |
| Hioki et al 201239 | 44 | Segmental wire fixation (Scott) and bone graft | 24.2 | 85 | Bilateral | 42 L5, 2 L4 and L5 | 4 wire breakage, 1 TP fracture | 73% | JOA scores improved in 93% of cases | N/A |
| Menga et al 201441 | 25 | Compression screw (Buck) and bone graft | 16 | 60 | N/A | N/A | 1 pars screw fracture | N/A | Improved postoperative VAS score by 5.76 points | 6 |
Abbreviations: F/U, follow-up; JOA, Japanese Orthopaedic Association; N/A, not applicable; SF-36, Short Form 36; PCS, physical component summary; MCS, mental component summary; ODI, Oswestry Disability Index; TP, transverse process; VAS, visual analog scale.
The rest were treated by activity limitation and physiotherapy.
The rest of the patients were treated conservatively, and it was a mixed group of athletes and nonathletes.
Two patients had success with conservative treatment.
The most common technique was the one described by Buck using a compression screw.5 8 23 37 38 41 44 45 Four studies used segmental wire fixation as described by Scott23 39 42 43 and two studies used a Scott technique but modified by using pedicle screw and wire.24 36 Finally, two studies used pedicle screws with hooks.34 40 The most common complication was the breakage of the wire used in segmental wire fixation.
The mean reported follow-up was 52 months. For the conservatively treated group, the most common level was L5, and bilateral defects were more common than unilateral. Eight publications (100/174) mentioned the union rates, which varied from 71 to 100%, all of which reported satisfactory outcomes. Twenty-six of these athletes were treated with a compression screw (Buck technique) and 74 with the Scott technique. The union was assessed with a CT scan in 55 athletes, with X-ray in 15, and with a combination of CT scan and X-ray in 30. Eleven publications (104/174) reported the average time to return to play, and the weighted mean was 7.9 months.
Results of Surgical Management
A large number of patients appear to have continued restricted mobility and pain despite the implementation of conservative treatments.41 Operative interventions in the form of compression screw (Buck) or segmental wire fixation (Scott) produced positive outcomes in this subset of patients. Convention dictates that pars repairs be performed in patients with nondegenerate intervertebral disks at the lysis segment and that it is contraindicated in severe disk disease and spondylolisthesis at the affected level. There is evidence to support these indications, demonstrating lower success rates in repairs of patients over the age of 25,46 a group with a greater incidence of degenerative disk disease and concomitant spondylolysis and spondylolisthesis.47 This literature review showed that the Buck procedure is the predominant operative method with the Scott procedure and modifications of this procedure used less often. Two studies reported on results using the pedicle screw with hook and bone grafting.34 40
Buck Procedure with Pedicle Screws
Seven of the reviewed publications for operative management looked at outcomes following the Buck procedure (Table 2).5 8 37 38 41 44 45 All studies showed good outcomes in their patient groups. A direct comparison between publications is difficult due to differing outcome measures; however, trends can certainly be observed. Roca et al demonstrated solid defect healing within 6 months in 14 of 15 patients in their case series.45 This finding was mirrored in a similar study by Hardcastle, who showed union in all treated patients at 6 months and the majority at 3 months.5 A case report of a modified Buck procedure using three-dimensional image guidance for minimally invasive fixation of the pars interarticularis also showed resolution of the pars fracture at 3 months.37
Similar trends were also shown in return to sport in the publications by Roca et al and Hardcastle, with 86 and 90% of patients able to return to previous participation rate in their sport, respectively.5 45 An improvement in functional outcomes was shown using validated outcome scores (ODI and SF-36) by Debnath et al using a modified Buck technique.38 Improvement was also shown using more subjective scoring methods (visual analog scale) by Menga et al.41 In addition to demonstration of functional improvement, Menga et al tried to correlate outcomes with size of the pars defect (on CT), preoperative disk morphology (on MRI), and patient age. No correlation was seen, although this lack is likely due to the small sample size and the outcome measurement used.
Ranawat et al demonstrated excellent outcomes in nine professional cricketers with Buck correction of their spondylolysis.44 However, unlike the other mentioned studies, the authors credited the positive outcomes to reeducation of bowling action, adequate rest, and physiotherapy input rather than the choice of surgical method. Multidisciplinary input is undoubtedly important but is resource intensive and may not be available in every center.
Scott Procedure with Wire Fixation
In comparison with the Buck procedure, reviewed papers that investigated the use of the Scott procedure showed a lower rate of fracture union, poorer outcomes, and increased complications predominantly due to wire breakage. The modified Scott procedure showed excellent outcomes in all patients without technical failures as shown with the original procedure; however, this result was only shown in case reports of three patients, making any conclusive judgment regarding this procedure very difficult.
Nozawa et al were the first group to publish data on the use of the Scott technique in athletes. They looked at 20 young athletes presenting with spondylolysis of the L4 or L5 vertebra. They achieved bony fusion in all cases, a statistically significant increase in the JOA score, and a 75% excellent outcome rate. However, three cases were complicated by wire breakage.42
Similarly, Ogawa et al presented one patient complicated by wire breakage, who developed pseudarthrosis.43 The authors attributed the mechanical failures to patients returning to sport too quickly or lack of postoperative adherence to the lumbar corset. Unlike Nozawa et al,42 Ogawa et al achieved union in only 81% of cases, which is substantially less than the union rates described in a comparable study by Roca et al (who looked at the Buck procedure).45
Hioki et al followed 44 patients who had repair using a Scott procedure; the group found that bilateral bony union was achieved in 67.4% of cases, unilateral union in 13% of cases, and nonunion in 19.6%. The group found that the greater the rate of union, the larger the improvement in JOA score postoperatively. The extremely high rate of nonunion using the Scott method in this study should also be noted.39
Excellent outcomes with 100% union were shown with the modified Scott procedure (a pedicle screw in addition to wires for fixation).24 36 The authors explained that this method avoids damaging the exiting nerve root below the transverse process; however, no other studies have listed this complication.
The only other variation from the Buck or Scott procedure was published as two case reports by Jarolem et al40 and Sutton et al.34 These groups used pedicle screws with hooks and bone grafts. Outcomes were described as excellent with the justification that hooks produced a more rigid construct than wire fixation and the construct would allow greater visualization of the pars defect, thereby preventing screw misalignment. Of note, only one study mentioned bone graft donor site morbidity in the form of pain at the iliac crest, suggesting it is not a major consideration when using autologous bone.34
Debnath et al found a gross disparity in outcomes when following a cohort of 22 athletes requiring surgical intervention, with 19 treated by the Buck procedure and 3 by the Scott procedure.23 Of the patients undergoing Buck procedure, 18 returned to sport within an average of 7 months, with the majority returning to the previous level of competition; moreover, there was an improvement in ODI and SF-36 scores. Of the group treated by the Scott technique, two had malunion, which required posterolateral fusion, and a third patient showed no significant improvement in ODI or SF-36 scores postoperatively. This study suggested superior results of the Buck procedure compared with the Scott procedure for repair of pars fractures.
Complications
Of the 15 studies that described operative management of spondylolysis, 8 reported the complication rate. A total of 140 athletes were treated in these 8 publications. Sixty-one athletes were treated with a compression screw, and 4 complications, 2 wound infections, and 2 cases of screw breakage were reported. Seventy-four athletes were treated with segmental wire fixation, and a total of 12 complications were reported. There were 7 cases of wire breakage, 3 nonunions, 1 wire pullout, and 1 transverse process fracture. Sutton et al treated 5 athletes with pedicle screws with hooks and bone graft and reported 1 case of iliac crest donor site pain. The group treated with compression screw had a lower risk of complications (p = 0.011).34
Discussion
Athletes are a unique population and require fast rehabilitation and a highly skilled surgeon to have the best possible results and return to preinjury level of competition. A review of the current literature shows overall good outcomes with the discussed methods other than surgical management with the pure wire technique. The evidence leans toward treatment with conservative measures prior to moving to surgical options in those who do not adequately respond. The involvement of skilled surgeons in the treatment of athletes likely was associated with a reduced complication rate, and the increased physical fitness and motivation levels of this group are likely to improve results compared with the average patient.
In our narrative review of the major treatment options in athletes with symptomatic spondylolysis, we attempted some overall comparisons. Overall, we found a weighted mean return to sports activities of 3.7 months for those receiving conservative treatment and 7.9 months for operative care. Outside of continued symptoms, nonoperative care was not associated with complications, as opposed to surgical treatment where the complication rates ranged from 6 to 15%. It has to be noted that surgical intervention was only attempted after conservative management had failed, thus a higher figure might be expected.
Spondylolysis is highly associated with low back pain in young athletes. Mihara et al described that the mechanism of back pain in patients with lumbar spondylolysis is caused by hypermobility of the posterior arch. Furthermore, they noted that degenerative changes in the intervertebral disk and facet joints can result in persistent back pain after union has been achieved.48 Early diagnosis and treatment may prevent or limit premature disk degeneration due to limited translational hypermobility and may also result in better clinical outcomes. The latter statements, however, are not based upon the current state of the literature and are largely conjecture by the authors.
There are substantial limitations within the current literature that impeded our original intent to develop some form of guideline toward management in athletes. These limitations are related mostly to methodological shortcomings, small numbers in case series, uncertainty how bone healing was established, and inconsistent outcomes reported across the reviewed studies. According to the evidence levels, the majority of reviewed studies represented level IV or V evidence, and therefore the weight of their conclusions is debatable.49 In addition, the reviewed studies lack consensus in several areas. There was no common patient-reported outcomes measure score, many studies had a mixed population of athletes and nonathletes, and furthermore the level of athletic activity was not mentioned. In light of this heterogeneity, a more formal meta-analyses was not appropriate, because sufficiently homogenous two-sided subgroups were not available. Finally, data collection in this specific population to perform a high-level study will be very difficult, as “athletes” might not participate.
Conclusion
Spondylolysis is a commonly reported injury among athletes. It is a recognized cause of low back pain that can adversely affect athletes' performance. There is no gold standard approach for the management of spondylolysis in the athletic population. The existing literature indicates that athletes with spondylolysis should undergo conservative management in the form of TLSO brace for 4 to 6 months complemented by activity modification and physiotherapy. Surgical intervention should be considered for cases that have not responded to conservative management. Based on outcome measures specific to each publication and reported complications, the Buck procedure appears to have fewer complications and improved patient outcomes, although it is technically more challenging.
Further clinical studies are needed to determine a pathway for the management of athletes with spondylolysis to optimize outcomes in athletes and their ability to return in the preinjury athletic performance in the shortest time. A formal randomized controlled trial is unlikely to be feasible because athletes are a “special” group of patients. A multicenter prospective cohort study looking at the specific method of treatment and recording the pre- and posttreatment function as well as the duration of treatment and the time to return to sport would be a great addition in the literature and an invaluable help to treat this group of patients.
Disclosures
Pavlos Panteliadis: none
Navraj S. Nagra: none
Kimberley L. Edwards: none
Eyal Behrbalk: none
Bronek Boszczyk: none
Editorial Perspective
This study was accepted by our reviewers under the premise of providing a narrative review of the literature on athletes and the preferred treatment of spondylolysis. Although the originally intended meta-analysis was not possible due to limitations on the reported data, the reviewers appreciated the comprehensive literature overview provided by the authors. The authors identified only 25 publications as being worthy for inclusion in the review with 390 patients in the nonoperative category and only 174 patients in the surgically treated category.
The big question posed by the authors at the onset of their project—whether nonoperative or surgical treatment offered better return to unrestricted function—could unfortunately not be answered conclusively due to the inherent study limitations.
In general, most patients seemed to return to function faster if treated with a period of rigid immobilization. That said, true bone healing of the pars defect was not clearly established, and acuity of the lesions prior to starting treatment as an important variable was not really established. Other factors include patient compliance with brace wear, body habitus, and of course the vertebral level affected by spondylolysis, with attempts at bracing for pars defects below L3 not really effective. Ultimately, the question of the actual effect of bracing remains unresolved: does lumbar bracing promote an actual stabilizing—or even bone-healing effect—or does it simply help settle down an irritated pars defect through activity restriction?
In light of these many variables, the cumulative current number of reported cases and the employed methodology for assessment really does not allow for a more formal comparative assessment of treatments.
For surgical treatments, there seems to be a general trend that more stable fixation and use of iliac crest interpositional grafts probably lead to more predicable healing results than the less invasive alternatives. Attention to details, such as matching the instrumentation construct to the actual biomechanical needs of the athlete, remains unclear.
Important nonoperative care aspects of pars defects were only tangentially addressed in this narrative review: what should be done with the notoriously tight hamstrings and what should be done about adjuvant medication management (i.e., vitamin D and hormonal treatment, for instance, teriparatide1 2)?
In a nutshell, the authors' question—what to do with a pars defect in an athlete—still remains firmly mired in the empirical rather than evidential era of medicine.
References
- 1.Iwamoto J, Sato Y, Takeda T, Matsumoto H. Return to sports activity by athletes after treatment of spondylolysis. World J Orthod. 2010;1(1):26–30. doi: 10.5312/wjo.v1.i1.26. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Iwamoto J, Abe H, Tsukimura Y, Wakano K. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school and college football players: a prospective study. Am J Sports Med. 2004;32(3):781–786. doi: 10.1177/0363546503261721. [DOI] [PubMed] [Google Scholar]
- 3.Standaert C J, Herring S A. Spondylolysis: a critical review. Br J Sports Med. 2000;34(6):415–422. doi: 10.1136/bjsm.34.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mazel C. [Spondylolisthesis in athletes] Presse Med. 1991;20(13):596–600. [PubMed] [Google Scholar]
- 5.Hardcastle P H. Repair of spondylolysis in young fast bowlers. J Bone Joint Surg Br. 1993;75(3):398–402. doi: 10.1302/0301-620X.75B3.8496207. [DOI] [PubMed] [Google Scholar]
- 6.Vrable A, Sherman A L. Elite male adolescent gymnast who achieved union of a persistent bilateral pars defect. Am J Phys Med Rehabil. 2009;88(2):156–160. doi: 10.1097/PHM.0b013e31819515c0. [DOI] [PubMed] [Google Scholar]
- 7.Blanda J, Bethem D, Moats W, Lew M. Defects of pars interarticularis in athletes: a protocol for nonoperative treatment. J Spinal Disord. 1993;6(5):406–411. doi: 10.1097/00002517-199306050-00007. [DOI] [PubMed] [Google Scholar]
- 8.Reitman C A, Esses S I. Direct repair of spondylolytic defects in young competitive athletes. Spine J. 2002;2(2):142–144. doi: 10.1016/s1529-9430(02)00179-1. [DOI] [PubMed] [Google Scholar]
- 9.Eddy D, Congeni J, Loud K. A review of spine injuries and return to play. Clin J Sport Med. 2005;15(6):453–458. doi: 10.1097/01.jsm.0000186681.13416.0c. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Orthopaedic Surgeons . St. Louis, MO: C. V. Mosby Co.; 1975. Atlas of Orthotics: Biomechanical Principles and Application. [Google Scholar]
- 11.Smith G E The most ancient splints BMJ 190812465732–736., 2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herkowitz H N, Garfin S R, Eismont F J, Bell G R, Balderston R A. Royal Oak, MI: Elsevier Health Sciences; 2011. Rothman-Simeone The Spine: Expert Consult. [Google Scholar]
- 13.Nachemson A, Schultz A, Andersson G. Mechanical effectiveness studies of lumbar spine orthoses. Scand J Rehabil Med Suppl. 1983;9:139–149. [PubMed] [Google Scholar]
- 14.Waters R L, Morris J M. Effect of spinal supports on the electrical activity of muscles of the trunk. J Bone Joint Surg Am. 1970;52(1):51–60. [PubMed] [Google Scholar]
- 15.Lumsden R M II, Morris J M. An in vivo study of axial rotation and immoblization at the lumbosacral joint. J Bone Joint Surg Am. 1968;50(8):1591–1602. [PubMed] [Google Scholar]
- 16.Axelsson P, Johnsson R, Strömqvist B. Effect of lumbar orthosis on intervertebral mobility. A roentgen stereophotogrammetric analysis. Spine. 1992;17(6):678–681. doi: 10.1097/00007632-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Brown T Norton P L The immobilizing efficiency of back braces; their effect on the posture and motion of the lumbosacral spine J Bone Joint Surg Am 195739-A1111–139., passim [PubMed] [Google Scholar]
- 18.Buck J E. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52(3):432–437. [PubMed] [Google Scholar]
- 19.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg. 1984;103(3):175–178. doi: 10.1007/BF00435550. [DOI] [PubMed] [Google Scholar]
- 20.Pai V S, Hodgson B, Pai V. Repair of spondylolytic defect with a cable screw reconstruction. Int Orthop. 2008;32(1):121–125. doi: 10.1007/s00264-006-0277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drazin D, Shirzadi A, Jeswani S. et al. Direct surgical repair of spondylolysis in athletes: indications, techniques, and outcomes. Neurosurg Focus. 2011;31(5):E9. doi: 10.3171/2011.9.FOCUS11180. [DOI] [PubMed] [Google Scholar]
- 22.Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis by segmental pedicular screw hook fixation. A preliminary report. Spine. 1996;21(17):2041–2045. doi: 10.1097/00007632-199609010-00023. [DOI] [PubMed] [Google Scholar]
- 23.Debnath U K, Freeman B JC, Gregory P, de la Harpe D, Kerslake R W, Webb J K. Clinical outcome and return to sport after the surgical treatment of spondylolysis in young athletes. J Bone Joint Surg Br. 2003;85(2):244–249. doi: 10.1302/0301-620x.85b2.13074. [DOI] [PubMed] [Google Scholar]
- 24.Salib R M, Pettine K A. Modified repair of a defect in spondylolysis or minimal spondylolisthesis by pedicle screw, segmental wire fixation, and bone grafting. Spine. 1993;18(4):440–443. [PubMed] [Google Scholar]
- 25.Songer M N, Rovin R. Repair of the pars interarticularis defect with a cable-screw construct. A preliminary report. Spine. 1998;23(2):263–269. doi: 10.1097/00007632-199801150-00023. [DOI] [PubMed] [Google Scholar]
- 26.Steiner M E, Micheli L J. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine. 1985;10(10):937–943. doi: 10.1097/00007632-198512000-00013. [DOI] [PubMed] [Google Scholar]
- 27.d'Hemecourt P A, Zurakowski D, Kriemler S, Micheli L J. Spondylolysis: returning the athlete to sports participation with brace treatment. Orthopedics. 2002;25(6):653–657. doi: 10.3928/0147-7447-20020601-15. [DOI] [PubMed] [Google Scholar]
- 28.Fellander-Tsai L, Micheli L J. Treatment of spondylolysis with external electrical stimulation and bracing in adolescent athletes: a report of two cases. Clin J Sport Med. 1998;8(3):232–234. doi: 10.1097/00042752-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Iwamoto J, Takeda T, Wakano K. Returning athletes with severe low back pain and spondylolysis to original sporting activities with conservative treatment. Scand J Med Sci Sports. 2004;14(6):346–351. doi: 10.1111/j.1600-0838.2004.00379.x. [DOI] [PubMed] [Google Scholar]
- 30.Micheli L J, Hall J E, Miller M E. Use of modified Boston brace for back injuries in athletes. Am J Sports Med. 1980;8(5):351–356. doi: 10.1177/036354658000800511. [DOI] [PubMed] [Google Scholar]
- 31.Miller S F, Congeni J, Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med. 2004;32(4):928–933. doi: 10.1177/0363546503262194. [DOI] [PubMed] [Google Scholar]
- 32.Pettine K A, Salib R M, Walker S G. External electrical stimulation and bracing for treatment of spondylolysis. A case report. Spine. 1993;18(4):436–439. [PubMed] [Google Scholar]
- 33.El Rassi G, Takemitsu M, Glutting J, Shah S A. Effect of sports modification on clinical outcome in children and adolescent athletes with symptomatic lumbar spondylolysis. Am J Phys Med Rehabil. 2013;92(12):1070–1074. doi: 10.1097/PHM.0b013e318296da7e. [DOI] [PubMed] [Google Scholar]
- 34.Sutton J H, Guin P D, Theiss S M. Acute lumbar spondylolysis in intercollegiate athletes. J Spinal Disord Tech. 2012;25(8):422–425. doi: 10.1097/BSD.0b013e318236ba6c. [DOI] [PubMed] [Google Scholar]
- 35.Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Eur Spine J. 2001;10(6):498–504. doi: 10.1007/s005860100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bozarth G R, Fogel G R, Toohey J S, Neidre A. Repair of pars interarticularis defect with a modified cable-screw construct. J Surg Orthop Adv. 2007;16(2):79–83. [PubMed] [Google Scholar]
- 37.Brennan R P, Smucker P Y, Horn E M. Minimally invasive image-guided direct repair of bilateral L-5 pars interarticularis defects. Neurosurg Focus. 2008;25(2):E13. doi: 10.3171/FOC/2008/25/8/E13. [DOI] [PubMed] [Google Scholar]
- 38.Debnath U K, Freeman B JC, Grevitt M P, Sithole J, Scammell B E, Webb J K. Clinical outcome of symptomatic unilateral stress injuries of the lumbar pars interarticularis. Spine. 2007;32(9):995–1000. doi: 10.1097/01.brs.0000260978.10073.90. [DOI] [PubMed] [Google Scholar]
- 39.Hioki A, Miyamoto K, Sadamasu A. et al. Repair of pars defects by segmental transverse wiring for athletes with symptomatic spondylolysis: relationship between bony union and postoperative symptoms. Spine. 2012;37(9):802–807. doi: 10.1097/BRS.0b013e318232303a. [DOI] [PubMed] [Google Scholar]
- 40.Jarolem K L, Tucker W A, Fulp T, Guyer R D. Rigid intrasegmental fixation for repair of a pars defect in a young athlete: case report and description of technique. J Spinal Disord. 1997;10(3):253–255. [PubMed] [Google Scholar]
- 41.Menga E N, Kebaish K M, Jain A, Carrino J A, Sponseller P D. Clinical results and functional outcomes after direct intralaminar screw repair of spondylolysis. Spine. 2014;39(1):104–110. doi: 10.1097/BRS.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 42.Nozawa S, Shimizu K, Miyamoto K, Tanaka M. Repair of pars interarticularis defect by segmental wire fixation in young athletes with spondylolysis. Am J Sports Med. 2003;31(3):359–364. doi: 10.1177/03635465030310030601. [DOI] [PubMed] [Google Scholar]
- 43.Ogawa H, Nishimoto H, Hosoe H, Suzuki N, Kanamori Y, Shimizu K. Clinical outcome after segmental wire fixation and bone grafting for repair of the defects in multiple level lumbar spondylolysis. J Spinal Disord Tech. 2007;20(7):521–525. doi: 10.1097/BSD.0b013e3180335c1f. [DOI] [PubMed] [Google Scholar]
- 44.Ranawat V S, Dowell J K, Heywood-Waddington M B. Stress fractures of the lumbar pars interarticularis in athletes: a review based on long-term results of 18 professional cricketers. Injury. 2003;34(12):915–919. doi: 10.1016/s0020-1383(03)00034-2. [DOI] [PubMed] [Google Scholar]
- 45.Roca J, Moretta D, Fuster S, Roca A. Direct repair of spondylolysis. Clin Orthop Relat Res. 1989;(246):86–91. [PubMed] [Google Scholar]
- 46.Winter M, Jani L. Results of screw osteosynthesis in spondylolysis and low-grade spondylolisthesis. Arch Orthop Trauma Surg. 1989;108(2):96–99. doi: 10.1007/BF00932163. [DOI] [PubMed] [Google Scholar]
- 47.Szypryt E P, Twining P, Mulholland R C, Worthington B S. The prevalence of disc degeneration associated with neural arch defects of the lumbar spine assessed by magnetic resonance imaging. Spine. 1989;14(9):977–981. doi: 10.1097/00007632-198909000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Mihara H, Onari K, Cheng B C, David S M, Zdeblick T A. The biomechanical effects of spondylolysis and its treatment. Spine. 2003;28(3):235–238. doi: 10.1097/01.BRS.0000042226.59713.0E. [DOI] [PubMed] [Google Scholar]
- 49.Bhandari M, Giannoudis P V. Evidence-based medicine: what it is and what it is not. Injury. 2006;37(4):302–306. doi: 10.1016/j.injury.2006.01.034. [DOI] [PubMed] [Google Scholar]
References
- 1.Gomberg S J, Wustrack R L, Napoli N, Arnaud C D, Black D M. Teriparatide, vitamin D, and calcium healed bilateral subtrochanteric stress fractures in a postmenopausal woman with a 13-year history of continuous alendronate therapy. J Clin Endocrinol Metab. 2011;96(6):1627–1632. doi: 10.1210/jc.2010-2520. [DOI] [PubMed] [Google Scholar]
- 2.Dizdarevic I, Bishop M, Sgromolo N, Hammoud S, Atanda A Jr. Approach to the pediatric athlete with back pain: more than just the pars. Phys Sportsmed. 2015;43(4):421–431. doi: 10.1080/00913847.2015.1093668. [DOI] [PubMed] [Google Scholar]


