Abstract
Objective
This study examined youth stressor reactivity in the form of links between daily stressors and adolescents’ negative affect, physical health symptoms, and cortisol patterns. We also tested whether youth gender and parental warmth moderated these linkages.
Method
Participants were the children of employees in the Information Technology division of a large company (N = 132, mean age = 13.39 years, 55% female). Youth completed daily diary telephone interviews on 8 consecutive evenings and provided saliva samples at 4 time points over 4 days to assess daily stressors and youth physiological and affective functioning. Parental warmth was assessed during in-home interviews. Multi-level modeling was used to account for interdependencies in the data.
Results
Youth who experienced more daily stressors, on average, reported more negative affect and physical health symptoms, on average. Further, on days youth reported more stressors than usual (compared to their own across-day average), they also exhibited more physical health symptoms, reduced evening cortisol decline (e.g., flatter slopes), higher bedtime cortisol, and more negative affect. Girls had stronger within-person linkages between daily stressors and daily negative affect than boys. Parental warmth moderated these within-person linkages: Youth who experienced more parental warmth had lower negative affect and steeper cortisol decline than usual on less stressful days. Yet, youth who experienced less parental warmth had higher negative affect and their cortisol levels declined less, even on days with lower-than-usual stress.
Conclusions
Daily stressors are associated with youth's affective and physiological functioning, but parental warmth can support youth's stress recovery.
Keywords: cortisol, daily stress, daily diary methods, negative affect, parent-child relationship, stressor reactivity
Childhood acute and chronic stressors are linked to increased risks for disease in adulthood, including cardiovascular disease and depression (Anda et al., 2006). Studies on adults suggest that, beyond major life stressors, daily stressors, such as interpersonal conflicts and work demands, also are linked to physical and mental health (Almeida, Piazza, Stawski, & Klein, 2011). We know little, however, about daily stressors in adolescence and their proximal ties to youth well-being. Daily stressors may impact youth functioning, including negative affect, physical health symptoms, and stress-related physiology, specifically the function of the hypothalamic-pituitary-adrenocortical (HPA) axis, such as is indexed via daily cortisol patterns (Bai & Repetti, 2015; Repetti, Robles, & Reynolds, 2011). Adults differ in their stressor reactivity, that is, their physiological and affective responses to daily stressors (Piazza et al., 2013). Responses in highly reactive individuals vary across days, such that they display greater negative affect, more physical health symptoms and less healthy cortisol patterns on days when they experience more stressors. By contrast, associations between daily stressors and affective and physiological function are less pronounced in low-reactive individuals (Piazza, et al., 2013). Importantly, individual factors, such as gender (Hankin, Mermelstein, & Roesch, 2007) and contextual factors, such as social support (Uchino, Cacioppo, & Kiecolt-Glaser, 1996) buffer adults from daily stressor effects. Yet knowledge of stressor-reactivity during adolescence is limited. Thus, this study used a daily diary approach to investigate stressor reactivity in the form of links between daily stressors and adolescents’ self-reported negative affect and physical health symptoms and biomarkers of their cortisol patterns. We also tested whether youth gender and parental warmth moderated these linkages.
We examined both affective and psychological responses to daily stressors, which may be interrelated. Healthy patterns of cortisol are marked by a diurnal rhythm wherein cortisol levels peak shortly after waking and then decline over the course of the day (McEwen, 1998). Daily stressors may trigger activity in the HPA system such that elevated levels of cortisol do not decline across the course of the day or the cortisol awakening response (CAR) is weakened. Thus in this study, high levels of youth salivary cortisol before dinner and at bedtime, a flatter decline in cortisol from dinner to bedtime (e.g., flatter slope), and a blunted next-day CAR were conceptualized as unhealthy cortisol patterns (Adam & Kamari, 2009), patterns that have been associated with an increased risk of disease and degraded immune functioning (Kemeny, 2003; Neeck, Federlin, Graef, Rusch, & Schmidt, 1990). Further, high levels of negative affect are linked to both disease and dysregulated cortisol patterns (Polk, Cohen, Doyle, Skoner, & Kirschbaum, 2005), though the causal mechanisms are unclear (Miller et al., 2011). To advance understanding of the implications of daily stressors in adolescence in this study, we investigated their links with negative affect, physical health symptoms, and cortisol patterns.
Daily Stressors and Youth Affective and Physiological Functioning
Both daily stressor frequency and stressor-reactivity are linked to affective and physiological functioning in adults. Daily stressors, such as interpersonal conflicts, work demands, and college exams are associated with more physical health symptoms, such as cold and flu, symptoms of chronic health conditions, and slower wound healing (Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Piazza et al., 2013), in addition to psychological distress and disrupted HPA functioning (Piazza et al., 2013). And, adults with stronger affective and physiological reactions to daily stressors—those with high stressor reactivity—are more likely to develop health problems, such as depression and chronic disease (Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013; Piazza et al., 2013).
Although well-studied in adults, little is known about how daily stressors are associated with physiological and affective functioning in adolescence. Adolescence is a time of biological, cognitive, and social changes (Steinberg & Morris, 2001) that may bring increased daily stress as adolescents navigate new demands and shifting peer and family dynamics (Seiffge-Krenke, 1995). Adolescents report frequent stressors (Rudolph & Hammen, 1999) and exhibit high stressor-reactivity, or strong affective and physiological responses to acute stressors (Stroud et al., 2009; Romeo, 2010). High levels of reactivity may be evident because adolescents are still developing the cognitive skills necessary to effectively cope with stress (Hampel & Peterman, 2006; Power, 2004).
The Role of Gender in Youth's Stress and Health
Gender has been implicated in adolescent stress, with girls reporting more stressors than boys (Flook, 2011; Almeida & Kessler, 1998). Girls tend to be more relationship-oriented than boys and have stronger needs for affiliation (McHale, Crouter, & Whiteman, 2003), thus relationship stressors, in particular, may lead to stronger physiological responses in girls than boys. Further, both global and daily stressors have been more strongly linked to HPA functioning, depressive symptoms, and daily mood in adolescent girls than boys (Flook, 2011; Hankin et al., 2007). In this study, we tested the hypotheses that there would be stronger linkages between daily stressors and negative affect, self-reported physical symptoms, and cortisol for girls than for boys.
The Buffering Role of Parental Warmth
In adults, contextual factors such as social support serve as a buffer against the negative effects of stress (Uchino et al., 1996), and adults with more social support have fewer physiological and affective responses to stressors (Eisenberger, Taylor, Gable, Hilmert, & Lieberman, 2007; Uchino, 2006). We know less about the role of social support in adolescents’ stress reactivity, but extant literature suggests that supports such as warm parent-child relationships -- those that are highly affectionate, supportive, and accepting -- may increase youth's feeling of security and thereby mitigate stress reactivity. Parents may also aid in cognitive restructuring, leading to youth appraisals of stressors as less threatening and decreasing youth's feelings of anxiety (Power, 2004; Eisenberger et al., 2007). Warm parents also model and promote development of emotion regulation skills (Morris, Silk, Steinberg, Myers, & Robinson, 2007). In these ways, parental warmth may dampen the links between daily stressors and youth affective and physiological functioning.
Most research on parents’ role in adolescent stress, however, focuses on traumatic events, such as parental divorce or chronic stressors such as neighborhood violence (Grant et al., 2006). We know little about how parent-child relationships may buffer youth from the effects of daily stressors, and how parental warmth relates to youth health on high or low stress days (Uchino et al., 2006). Some work on infants and toddlers documents the buffering role of parent-child relationships on the effects of experimentally-induced stressors on cortisol levels in lab settings (Blair, et al., 2008; Gunnar et al., 1992). In addition, adults who retrospectively reported warmer parent-child relationships were less likely to experience psychological distress and exhibited lower cortisol levels after exposure to stressful life events (Hagan et al., 2011; Mallers, Charles, Neupert, & Almeida, 2011).
The Current Study
In this study, we used a daily diary design to test three hypotheses. First, daily stressors will be associated with higher youth negative affect, more self-reported physical health symptoms, and less healthy cortisol patterns, including higher dinner and bedtime cortisol levels, less cortisol decline from dinner to bedtime, and blunted next day CAR. Second, gender will moderate the linkages between daily stressors and negative affect, physical symptoms, and cortisol, with stronger linkages for girls. Third, parental warmth will moderate the linkages between daily stressors and negative affect, physical symptoms, and cortisol, with weaker links (less daily reactivity) for youth with warmer parent-child relationships.
Method
Participants
The study used data from a subsample of families that participated in the daily diary component of the Work, Family Health Network Study, a study of a workplace intervention designed to reduce work-family conflict and improve the health of employees and their families (Bray et al., 2013). Participants for these analyses were 132 employees (45% female; mean age = 45.24, SD = 6.30) from the larger sample of workers in an information technology division of a Fortune 500 company, and their child, aged 9-17 who lived with them for at least four days a week. If the target employee had more than one child within this age range, the child closest to age 13 was recruited. The majority of youth were White (59%); 3% were African American, 15% were Hispanic, 18% were Asian, less than 1% were American Indian/Alaska Native or Pacific Islander, and 3% reported more than one race/ethnicity. Most parents graduated from college (78%), and their annual incomes averaged between $110,000 and $119,999. Most parents were married (81%); 6% were cohabiting, and 13% were single. Youth (55% female) averaged 13.39 years of age (SD = 2.40).
Procedures
Data were collected via three methods: in-home interviews, 8-day daily telephone interviews, and saliva sampling. Appropriate Institutional Review Boards approved study procedures. During home interviews, parents provided consent and youth provided assent. Youth were then interviewed separately about their health, adjustment, and family relationships, and parents completed computer-assisted personal interviews. Parent-child dyads who completed home interviews were eligible to also participate in the daily diary study of daily activities, emotions, and experiences via telephone calls on 8 consecutive evenings. Trained interviewers conducted a Computer Assisted Telephone Interview (CATI) with the employee and child separately on the same 8 consecutive evenings. Calls lasted approximately 15 minutes for children and 25 minutes for parents and required each to reflect on experiences in the past 24 hours.Youth reported on the previous 24-hour period (Mdn youth interview start time = 8:01 PM, SD = 1.62 hrs; 88% completed all 8 calls; all youth completed at least 6 calls).
On 4 diary days (days 2-5), saliva samples were collected from youth at 4 time points: upon awakening, before getting out of bed, 30 minutes after waking, before dinner, and before going to bed. Of the youth who participated in the diary calls, 96% (N = 126) also provided saliva samples. Our sample includes 1829 valid saliva samples (90% of 2,016 possible samples). Seventy-one percent of youth provided complete saliva data on two or more days. During home interviews, saliva collection kits with instructions were given to families. Each kit contained 16 salivettes for collecting youth cortisol (4 salivettes a day over 4 days) and a DVD demonstrating saliva collection. Youth were instructed to roll a cotton swab across their tongue for 2 minutes and return it to the tube without touching it. They also were told not to eat, drink or brush their teeth for 30 minutes prior to saliva collection. Youth recorded the time each saliva sample was taken on a separate data collection sheet on which they also recorded any medications they were taking during the saliva collection period. Instructions for saliva collection were reviewed with parents and youth during the first phone interview, and youth were reminded about the saliva collection on the evenings prior to scheduled collections.
Compliance with the saliva collection protocol was high: Noncompliance (including the time difference between samples at wake and 30 minutes post wake was less than 15 minutes or greater than 60 minutes, the child woke up later than noon, and/or the child was awake for less than 12 hours or more than 20 hours) was noted on only 10% of days that at least one cortisol sample were provided. In addition, 10% of youth received a time-stamper to record the time of cortisol collection: compliance among youth with a time-stamper did not differ from compliance among youth who self-recorded their data collection times.
Participants refrigerated the samples after each collection and, at the end of saliva collection period, mailed the samples to our laboratory using prepaid overnight delivery. Upon receipt, saliva samples were weighed and frozen at −80 °C until later assay of cortisol in the Biomarker Core Laboratory at The Pennsylvania State University using commercially available EIA kits (Salimetrics, LLC, State College, PA) on a rolling basis throughout the study period. The assay had a lower limit of sensitivity of 0.003 ug/dL, with average inter- and intra-assay covariances (%) of less than 7% and 4%. Of the bedtime samples, 54 were below 0.003 ug/dL and were designated as off-the-curve low and set to the lowest level of sensitivity of the assay.
Measures
Daily stressors were measured with an adapted version of the Daily Inventory of Stressful Events (DISE, Almeida, Wethington, & Kessler, 2002; Almeida & Davis, 2011). During each call, youth were asked if they had experienced five stressors (0 = no; 1 = yes) from the time of the previous call until the time of the current call. An example item is, “Did you have any arguments or disagreements with anyone else, other than (target parent) since this time yesterday, including other people in your family or people outside your family?” Stressors included relationship stressors (e.g., with friends, relatives) as well as non-relationship stressors (e.g., at work/school). Items were summed with higher scores indicating more daily stressors.
Daily negative affect was assessed using a 6-item scale adapted from the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988; e.g., “How much of the time today did you feel upset?”). Items were rated on a five-point scale (1 = none of the time to 5 = all of the time) and averaged within each day for use in our analysis.
Youth daily physical health symptoms were assessed via a 6-item scale adapted from Larson and Kasimatis (1991). For each item (headache, cold/ flu, tired, allergies, stomachache, other physical problems) youth reported whether they had or had not experienced that symptom on the day of the call (0 = no; 1 = yes). The items were summed within each day so that higher scores indicated more daily physical health symptoms.
Youth cortisol, a marker of HPA-axis function was indexed by four measures: level of cortisol before dinner, level at bedtime, the evening slope from before dinner to bedtime, and next-morning CAR. We focused on end of the day and next morning measures, reasoning they would best reflect youth reactions to stressors they experienced on a given day. The evening slope was calculated by subtracting the before dinner from the bedtime cortisol score and dividing by the duration of time between the samples. CAR was calculated from the cortisol at wake and 30 minutes after wake (Stawski, Cichy, Piazza, & Almeida, 2013). Cortisol data were converted to nmol/l (ug/dL X 27.59) and log transformed before analysis (Adam & Kumari, 2009).
Parental warmth was rated by youth in the home interviews using 8 items from the Child's Report of Parental Behavior Inventory (CRPBI; Schaefer, 1965). Youth were asked to rate their parents’ behavior over the past month. Example items include “Your [parent]... tells or shows you that s/he likes you just the way you are” and “Almost always speaks to you with a warm and friendly voice” (1 = not at all to 5 = very much). The 8 items were averaged, with high scores signifying greater parental warmth. Cronbach's alpha = .85.
Control variables included youth age (centered at the grand mean), youth gender (0 = male, 1 = female) and parent education (0 = not a college graduate, 1= college graduate). Cortisol models also controlled for the time of sample collection, race/ethnicity (0 = White; 1= Non-white), and whether or not the youth was taking any medications that can influence cortisol (0 = no medications, 1= 1 or more medications) (Adam & Kumari, 2009). In addition, in order to account for non-compliance in timing of saliva collection, our models included a control variable that flagged potential cortisol time non-compliance on a particular day (0 = all samples compliant; 1= 1 or more sample noncompliant). Youth were given a score of 1 on this noncompliance variable if any of the following conditions were noted during the day of saliva collection: the time difference between samples at wake and 30 minutes post wake was less than 15 minutes or greater than 60 minutes, the child woke up later than noon, and/or the child was awake for less than 12 hours or more than 20 hours. If no compliance issues were noted, the child received a score of 0 on this non-compliance variable.
Plan of analysis
We used multi-level modeling to account for the non-independence of observations (Raudenbush & Bryk, 2002). Daily diary designs allow testing of typically examined questions about between-person differences, such as whether youth with more stressors exhibit poorer functioning, on average. In addition, they allow for tests of within-person associations, such as whether on days when youth have more stressors than usual, they also have more negative affective and physiological functioning than usual that same day. Conceptually, our analytic approach allows us to assess the proximal within-person linkages between stress and youth outcomes. Further, within-person analyses allow for stronger inferences about the linkages between stressors and well-being because they control for stable between-person differences, such as genetic or larger social environmental, “third variables” that might otherwise account for the associations between stressors and well-being (Almeida, 2005; Jacobs et al., 2002).
Two level models were estimated in SAS 9.3 using Proc Mixed, with days (level 1, within-person) nested within individuals (level 2, between-person). At level 1, we included person-mean centered measures of the time varying daily stressor measures. For the analyses of cortisol, we also included the time-varying controls (i.e., time of saliva collection). At level 2, we entered the between-person variables, which were grand mean centered, including the cross-day averages of daily stressors (person-mean) and time-invariant controls (e.g., race, age, gender).
| (1a) |
| (1b) |
| (1c) |
At Level 1 (daily level, equation 1a), youth i's health outcomes on day t were modeled as a function of their daily intercept (B0i) and daily slope (B1i), and residual variance (eti.). The daily slope reflects changes in youth outcomes on days when youth have more daily stressors than usual (within-person). At Level 2 (person-level), the level 1 intercept (equation 1b) was modeled as a function of the sample average intercept (π00), and slope (π01), as well as random effects (u0i). The Level 2 slope (π01) reflects differences in youth outcomes associated with the cross-time averages of daily stressors (between-person), that is, differences in youth outcomes as a function of the average number of their daily stressors (as compared to other youth). The level 1 slope (equation 1c) was modeled as the sample average daily within-person effect (π10) and random effects (u1i). Lagged models were run for morning rise (CAR), where we investigated the linkages between daily stressors and morning rise on the following days.
We estimated three models for each outcome variable. First, we tested the main effects of daily stressors on youth functioning (Table 2, Model 1). Then, we tested whether the links between daily stressors and youth functioning were moderated by youth gender (Table 2, Model 2). Finally, we assessed whether the links between daily stressors and youth functioning were moderated by global reports of parental warmth (Table 2, Model 3). Moderation by gender was tested at the between-person level by adding an interaction term with gender and between-person stressor frequency to Level 2 (Gender *π01 added to equation 1b). Moderation was also tested at the within-person level by adding gender to equation 1c, resulting in a cross-level interaction term with gender (Level 2) moderating the within-person effects of stressors (Level 1). Similar procedures were followed to test for moderation by parental warmth. Follow-up tests of the simple slopes were conducted when interaction terms were p < .05 or lower (Aiken & West, 1997).
Results
Table 1 shows means and correlations for study variables. Most variation was within individuals across study days: Intra-class correlations ranged from .02 to .33 indicating more within-person variation than between-person variation.
Table 1.
Means, Standard Deviations, and Between-Person Correlations between Study Variables
| Mean | BP SD | WP SD | ICC | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Number of daily stressors | .35 | .35 | .63 | .10 | ||||||||
| 2. | Physical health symptoms | .61 | .57 | .94 | .26 | .40*** | |||||||
| 3. | Before dinner cortisol levels | 2.35 | 2.30 | 3.76 | .34 | .09 | .00 | ||||||
| 4. | Bedtime cortisol levels | 1.55 | 1.54 | 2.50 | .29 | .18* | .02 | .61** | |||||
| 5. | Dinner to bedtime slope | −.39 | 1.80 | 3.06 | .07 | −.05 | .01 | −.23* | .31* | ||||
| 6. | Morning rise (CAR) | .28 | .42 | .65 | .17 | .12 | −.03 | .23* | .11 | −.08 | |||
| 7. | Negative affect | 1.27 | .43 | .40 | .39 | .61*** | .23* | .11 | .16 | −.04 | .06 | ||
| 8. | Parental warmth | 1.03 | .64 | .64 | -- | −.23* | −.14 | −.10 | −.11 | .05 | .03 | −.22* | |
| 9. | Youth gender (% female) | 55% | -- | .50 | -- | .05 | .19* | .07 | .06 | .02 | .26 | .04 | .33 |
Note: BP= between-person. WP = within person. All Cortisol values were log transformed before calculating correlations.
p < .05
p < .01
p < .001.
Daily stressors and youth health
Beginning with the main effects (Table 2, Model 1), the frequency of youth daily stressors was associated with youth functioning at both the between- and within-person levels. At the between-person level, youth with more daily stressors, on average, experienced more self-reported physical health symptoms and more negative affect than other youth. Within-person analyses revealed that, controlling for average number of stressors, on days when youth reported more stressors than usual, they also experienced more negative affect, physical health symptoms, and flatter cortisol slopes. A marginal within-person finding emerged for bedtime cortisol levels (p = .06), which tended to be higher on days with more stressors than usual. No effects of daily stressors were found for next day CAR (not shown).
Table 2.
Daily Stressors and Youth Health Outcomes
| Negative Affect | Physical Health Symptoms | Before Dinner Level of Cortisol | Bedtime Level of Cortisol | Before Dinner to Bedtime Slope | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Est | SE | Est | SE | Est | SE | Est | SE | Est | SE | |
| Model 1: Main Effects | ||||||||||
| Fixed Effects | ||||||||||
| BP Daily Stressors | 0.49*** | 0.06 | 0.60*** | 0.13 | 0.17 | 0.1 | 0.14 | 0.09 | −0.04 | 0.11 |
| WP Daily Stressors | 0.14*** | 0.02 | 0.33*** | 0.05 | −0.02t | 0.05 | 0.09t | 0.04 | 0.20* | 0.08 |
| Random Effects | ||||||||||
| Intercept | 0.03*** | 0.01 | 0.18*** | 0.03 | 0.09*** | 0.02 | .06*** | 0.01 | 0.01 | 0.03 |
| Residual | 0.09*** | 0.00 | 0.60*** | 0.03 | 0.19*** | 0.02 | .19*** | 0.12 | 0.43** | 0.04 |
| Model 2: Moderation by Youth Gender | ||||||||||
| Fixed Effects | ||||||||||
| BP Daily Stressors | 0.43*** | 0.08 | 0.64** | 0.18 | 0.19 | 0.14 | 0.11 | 0.09 | −0.09 | 0.15 |
| WP Daily Stressors | 0.09** | 0.02 | 0.34*** | 0.07 | −0.08 | 0.07 | 0.08t | 0.04 | 0.07* | 0.03 |
| Youth gender | −0.01 | 0.04 | 0.16t | 0.09 | −0.05 | 0.2 | 0.05 | 0.07 | 0.01 | 0.08 |
| BP Daily Stressors × Youth Gender | 0.12 | 0.12 | −0.11 | 0.26 | −0.05 | 0.2 | 0.07 | 0.05 | 0.11 | 0.21 |
| WP Daily Stressors × Youth Gender | 0.08* | 0.04 | −0.02 | 0.09 | 0.11 | 0.09 | 0.02 | 0.02 | −0.07 | 0.15 |
| Model 3: Moderation by Parental Warmth | ||||||||||
| Fixed Effects | ||||||||||
| BP Daily Stressors | 0.47*** | 0.06 | 0.55*** | 0.13 | 0.15 | 0.11 | 0.10 | 0.10 | 0.03 | 0.12 |
| WP Daily Stressors | 0.14*** | 0.02 | 0.32*** | 0.05 | −0.03 | 0.05 | 0.11 | 0.05 | 0.27* | 0.09 |
| Parental Warmth | −0.05 | 0.04 | −0.11 | 0.07 | −0.05 | 0.06 | −0.06 | 0.06 | 0.00 | 0.07 |
| BP Daily Stressors × Parental Warmth | 0.06 | 0.08 | −0.02 | 0.18 | 0.01 | 0.15 | −0.04 | 0.14 | 0.23 | 0.16 |
| WP Daily Stressors × Parental Warmth | 0.08** | 0.03 | −0.05 | 0.06 | −0.00 | 0.06 | 0.11t | 0.06 | 0.20* | 0.10 |
Note. BP indicates between-person effects. WP indicates within person effects. All models control for child gender, child age, and parent education. Cortisol models also control for medication use, race, and time of sample. Moderation models include random effects (not shown).
p < .10
p < .05
p < .01
p < .001
Moderation of stressor effects
The test of gender moderation revealed that the within-person linkages between number of stressors and negative affect differed for girls versus boys (Table 2, Model 2). Tests of the simple slopes (not shown) revealed that the links between daily stressors and negative affect were stronger for girls, B = 0.17 SE = 0.02, p < .001, than for boys, B = .09, SE = 0.03, p < .01. No gender moderation effects emerged for physical health symptoms or the cortisol measures.
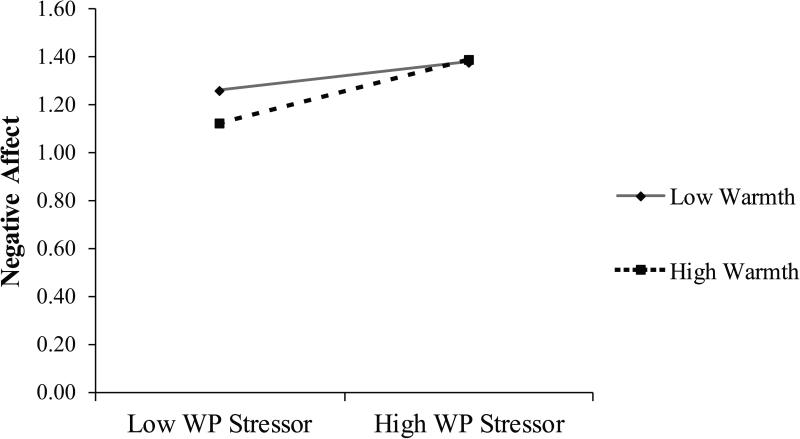
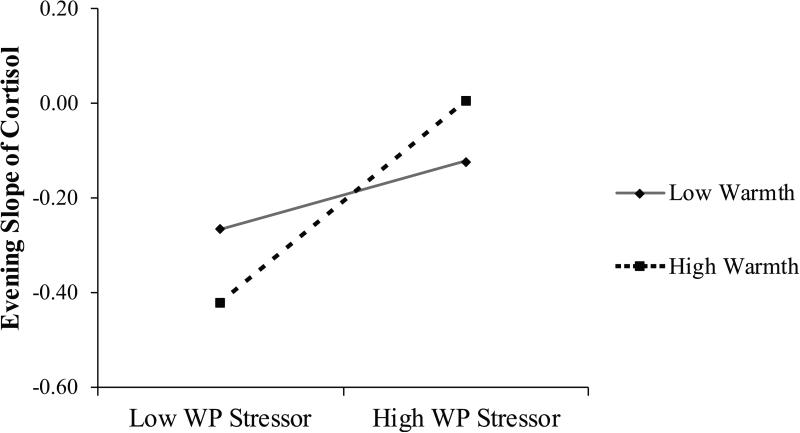
Parental warmth also moderated the within-person linkage between daily stressors and youth negative affect (Table 2, Model 3). Follow-up tests of the simple slopes (+ / − 1 SD) revealed that the within-person link between daily stressors and negative affect was stronger for youth with higher, B = 0.20 SE = 0.03, p < .001, as compared to lower parental warmth, B = 0.10 SE = 0.02, p < .001. Examination of the means revealed that, in contrast to our hypothesis, youth who reported lower parental warmth had higher levels of negative affect even on days when they experienced fewer stressors than usual (Figure 1a). Youth with the lowest levels of negative affect were those with high parental warmth on low stress days. A similar pattern was found for the within-person associations between stressors and the slope of cortisol from dinner to bedtime (Table 2, Model 3; Figure 1b). On days when youth with warmer parent-child relationships experienced more stressors than usual, their cortisol levels declined less between dinner and bedtime (i.e., the slope was flatter), B = 0.40 SE = 0.12, p < .01. However the within-person linkage between stressors and cortisol slopes was not significant for youth with less warm parent-child relationships, B = 0.15 SE = 0.09, ns. Examination of the means suggests that youth who had the steepest declines in cortisol were those who had high parental warmth on low stress days. No moderation effects for parental warmth were found for physical symptoms, before dinner or bedtime cortisol levels, or next-day CAR.
Figure 1a. Parental warmth moderates the within-person linkage between daily stressors and youth negative affect.
Follow-up tests revealed that the within-person linkages between stressors and negative affect were stronger for youth who experienced high parental warmth than youth who experienced low parental warmth.
Figure 1b. Parental warmth moderates the within-person linkage between daily stressors and evening cortisol slopes.
Follow-up tests revealed that the within-person linkages between stressors and evening cortisol slopes were significant for youth who experienced high parental warmth, but not for youth who experienced low parental warmth. Youth with warm parents had flatter slopes (e.g., closer to zero) than usual on days they experienced more stressors than usual. However, youth who experienced low parental warmth did not differ across high and low stress days.
Discussion
Considerable evidence has accumulated showing that daily stressors are linked to health in adulthood (Almeida et al., 2011). Our study suggests that daily stressors also are associated with affective and physiological functioning during adolescence. As hypothesized, at the between-person level, youth who reported more daily stressors, on average, experienced more self-reported physical health symptoms and more negative affect. Importantly, we also found that, controlling for the across-day average number of stressors, on days youth reported more stressors than usual, they also exhibited more physical health symptoms, flatter evening slopes, higher bedtime cortisol levels, and more negative affect than usual. Such within-person effects are notable given they emerge from analyses in which individuals serve as their own controls, and allow the researcher to rule out other stable third variable explanations, measured or not (Almeida, 2005). Consistent with findings from research on adults, not only major life events, but daily stressors have proximal linkages with youth health. Importantly, however, the associations between daily stressors and youth affective and physiological functioning were not homogenous, but varied as a function of youth gender and parental warmth. A direction for research is to explore other individual and contextual characteristics that may serve as risk and protective factors in daily stress processes.
Studies of adults show both immediate and longer-term associations between stressors and physical and psychological health (Piazza et al., 2013). Our research suggests that daily stressors may have proximal linkages to physiological functioning during adolescence, as evidenced by significant within-person relations between daily stressors and youth physical symptoms and diurnal patterns of cortisol. Our findings revealed that, on days when youth experienced more stressors than usual, they exhibited higher levels of cortisol at bedtime and flatter evening slopes-- compared to days with fewer stressors. Repeated activation of the HPA system may lead to wear and tear on the body, and eventually failure of the system to activate in response to stressful situations (Piazza et al., 2010). Although we saw no evidence of a blunted CAR, such a response may emerge over an extended period of time (Adam, Hawkley, Kudielka, & Cacioppo, 2006). Interestingly, our cortisol outcomes were associated with stressors at the within- but not the between-person level. As with findings on adults (Kiecolt-Glaser, et al., 2002; Piazza et al., 2013), daily stressors were also linked to more physical health symptoms, such as cold and flu. Higher average stressor frequency across the 8 days was associated with more physical symptoms and negative affect, but not with the cortisol indicators. This pattern suggests that stressors had more immediate effects on HPA functioning, but did not accumulate across the course of the week to create detectable between-person differences. Further study is needed to understand how the effects of daily stressors in adolescence accumulate over time to impact later chronic disease conditions (Repetti et al., 2011). Given the proximal links between stressors and physiological functioning, promoting adolescents’ strategies for coping with daily stressors and stress management techniques may have important and proximal associations with their HPA functioning and physical symptoms.
Consistent with our hypothesis, we found gender differences in the links between daily stressors and negative affect. Although significant for both genders, the within-person linkages between daily stressors and negative affect were stronger for girls. These findings extend prior work showing stronger linkages between stressors and depression for girls (Hankin et al., 2007) in documenting that daily stressors are associated with daily negative affect (Flook, 2011). More studies are needed to document whether and how experiences of daily stressors and negative affect accumulate over time to affect clinical levels of depression. In this study, many of the targeted stressors were interpersonal, one possible reason why associations were stronger in girls given their stronger social orientations (Hankin et al., 2007). Our findings support other research suggesting stressors may be more strongly linked to affect and depression for girls than boys (Flook, 2011). However, at least one study suggests that gender moderation may vary based on the type of stressor. Specifically, the linkages between school/achievement-related stressors and youth depression may be stronger for boys (Shih et al., 2006). Future research on larger samples should examine a range of daily stressor domains, such as achievement and peer domains and how stressors in different domains may have differential impacts for boys and girls (Shih et al., 2006). Youth gender did not moderate the linkages between physical health symptoms or cortisol levels, highlighting the importance of collecting multiple measures of youth functioning in studies of stress processes. Our findings suggest that stressors may have similar effects on HPA functioning and physical health for boys and girls. Future studies are needed to explore how stress processes may differ for girls and boys, gender differences in reactivity to stressors in different domains, and the role of mediating processes like coping skills.
As predicted, parental warmth moderated the within-person linkages between daily stressors and both cortisol daily decline and negative affect. However, contrary to expectations, the role of parental warmth was most evident on days with fewer stressors. Youth who experienced high parental warmth exhibited the healthiest profiles on low stressor days (low negative affect and steeper cortisol slopes). Thus parental warmth did not weaken the links between daily stressors and physiological and affective functioning, as we hypothesized. However, our findings are consistent with a recovery pattern: warmth may play a role in youth's ability to recover from stressors on non-stress days. In a healthy HPA system, physiological and emotional responses increase under stress, but decrease after the stressor exposure is over (Sapolsky et al., 2006). Thus, in this study, stress recovery may be evident in the form of lower levels of physiological and emotional responses on low stress as compared to highly stressful days. And, our findings are consistent with a recovery pattern for youth with high parental warmth but not those with low parental warmth. Specifically, youth with higher parental warmth had higher levels of negative affect and flatter cortisol slopes on stressful days, but lower levels of negative affect and steeper cortisol decline on less stressful days, indicating effective stress-recovery processes. In contrast, youth with low parental warmth exhibited higher levels of negative affect and flatter cortisol slopes on both high and low stress days, suggesting that they were less well able to recover from high stress days. It will be important to replicate these findings using data collection procedures with greater temporal resolution and specific measures of recovery, in response to a greater variety of stressors, and in other populations. Inability to recover after a daily stressor may be a cause for concern, given that stress recovery processes have been linked over time to a host of health outcomes in adults (Smyth & Heron, 2014).
Warm parents may promote youth's coping skills, assist in problem-solving, provide support and advice for how to handle stressors, and serve as role models for self-regulation, all of which may foster youth's own self-regulation capacities and thereby enable recovery on days of lower stress (Power, 2004). Interestingly, moderation effects were only evident for within-person effects; we were unable to detect parental warmth effects on the links between average number of stressors and youth outcomes. Studies with short time scales may be needed to capture the linkages between stress and health and to assess more immediate indicators of stress recovery. It also may be that, in this relatively privileged sample, stressors were not sufficiently strong or frequent to give rise to more stable between-person differences. Further, there was more variability in stressors at the within- than between-person level, which may also have made it more difficult to detect between-person effects. Future studies should include samples of youth from a wider range of family circumstances to better capture between individual differences in stressor-outcome linkages.
Several other limitations of our study also imply directions for research. First, participants were well-educated, primarily Caucasian youth. The relations between stress, health, and parenting may differ based on demographic or contextual factors, such as race, neighborhood conditions, or income, and thus research is needed to replicate our results with other samples. We relied on youth self-reports of stressors, physical health symptoms, negative affect, and parental warmth, and thus mono-reporter biases may underlie some of the associations we observed. Future studies should include measurement approaches, such as biomarkers of immune system function, observations of parent-child interactions, and measures of other aspects of parenting. In addition, future studies with larger, more diverse samples should aim to unpack how specific types of stressors, such as school stressors or socio-cultural stressors such as discrimination and poverty, are related to youth outcomes (Shih et al, 2006). Finally, our correlational design means that direction of effects cannot be discerned: Youth with more physical health symptoms, higher cortisol and/or more negative affect may perceive and/or elicit more daily stressors rather than the other way around, or a bidirectional process linking youth health and daily stressors may be at play (Flook, 2011). Future studies of daily stressors in which data are collected at many points in time across the day, such as with ecological momentary assessments, can help to establish the direction of effects underlying these associations.
In the face of some limitations, this study contributes to the literature on stress and well-being in adolescence by moving beyond the field's prior focus on chronic stress and major life events to study youth's experiences of daily stressors. Consistent with predictions, daily stressors were linked in the short term to indices of youth's physical symptoms, unhealthy cortisol patterns, and negative affect. Taking advantage of our repeated measures design, we also established that a number of these linkages emerged at the within person level, allowing us to rule out stable third variables as explanations of the associations we observed. These effects were not universal, however: both youth gender and parental warmth moderated some associations. Future research should be directed at delineating the conditions under which daily stressors are linked to adolescents’ well-being. Such studies may identify potentially malleable factors and target populations for prevention and intervention programs aimed at mitigating the deleterious effects of stressors during this important developmental period.
Acknowledgements
This research was conducted as part of the Work, Family and Health Network (www.WorkFamilyHealthNetwork.org), which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant # U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (Grant # U01AG027669), Office of Behavioral and Science Sciences Research, and National Institute for Occupational Safety and Health (Grant # U01OH008788, U01HD059773). Grants from the National Heart, Lung and Blood Institute (R01HL107240), William T. Grant Foundation, Alfred P. Sloan Foundation, and the Administration for Children and Families have provided additional funding. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices. Special acknowledgement goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, Ph.D. and Lynne Casper, Ph.D. for the design of the original Workplace, Family, Health and Well-Being Network Initiative. We also wish to express our gratitude to the worksites, employers, and employees who participated in this research as well as to Lauren Camuso for her assistance with this manuscript. Full acknowledgements: http://www.kpchr.org/wfhn
References
- Adam E, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen.2009.06.011. doi: 10.1016/j.psyneuen.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience–cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Thousand Oaks, California: 1991. [Google Scholar]
- Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science. 2005;14(2):64–68. doi: 10.1111/j.0963-7214.2005.00336.x. [Google Scholar]
- Almeida DM, Davis KD. Workplace flexibility and daily stress processes in hotel employees and their children. The Annals of the American Academy of Political and Social Science. 2011;638(1):123–140. doi: 10.1177/0002716211415608. doi: 10.1177/0002716211415608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, Kessler RC. Everyday stressors and gender differences in daily distress. Journal of Personality and Social Psychology. 1998;75:670–680. doi: 10.1037//0022-3514.75.3.670. doi: 10.1037//0022-3514.75.3.670. [DOI] [PubMed] [Google Scholar]
- Almeida DM, McGonagle K, King H. Assessing daily stress processes in social surveys by combining stressor exposure and salivary cortisol. Biodemography and Social Biology. 2009;55(2):219–237. doi: 10.1080/19485560903382338. doi: 10.1080/19485560903382338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, Piazza JR, Stawski RS, Klein LC. The speedometer of life: Stress, health and aging. In: Schaie KW, Levey R, editors. The Handbook of the psychology of aging. Elsevier; New York, NY: 2011. [Google Scholar]
- Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events an interview-based approach for measuring daily stressors. Assessment. 2002;9(1):41–55. doi: 10.1177/1073191102091006. doi: 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai S, Repetti RL. Short-term resilience processes in the family. Family Relations. 2015;64(1):108–119. doi: 10.1111/fare.12101. doi: 10.1111/fare.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, Granger DA, Kivlighan KT, Mills-Koonce R, Willoughby M, Greenberg MT, Fortunato CK. Maternal and child contributions to cortisol response to emotional arousal in young children from low-income, rural communities. Developmental Psychology. 2008;44(4):1095–1109. doi: 10.1037/0012-1649.44.4.1095. doi: 10.1037/0012-1649.44.4.1095. [DOI] [PubMed] [Google Scholar]
- Bray JW, Kelly EL, Hammer LB, Almeida DM, Dearing JW, King RB, Buxton OM. An integrative, multi-level, and transdisciplinary research approach to challenges of work, family, and health. RTI Press publication No. MR-0024-1303. RTI Press; Research Triangle Park, NC: 2013. [PubMed] [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski MJ, Almeida DM. The wear and tear of daily stressors on mental health. Psychological Science. 2013;24(5):733–741. doi: 10.1177/0956797612462222. doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Taylor SE, Gable SL, Hilmert CJ, Lieberman MD. Neural pathways link social support to attenuated neuroendocrine stress responses. Neuroimage. 2007;35(4):1601–1612. doi: 10.1016/j.neuroimage.2007.01.038. doi: 10.1016/j.neuroimage.2007.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flook L. Gender differences in adolescents’ daily interpersonal events and well-being. Child Development. 2011;82(2):454–461. doi: 10.1111/j.1467-8624.2010.01521.x. doi: 10.1111/j.1467-8624.2010.01521.x. [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY, Campbell AJ, Westerholm RI. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clinical Psychology Review. 2006;26(3):257–283. doi: 10.1016/j.cpr.2005.06.011. doi: 10.1016/j.cpr.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Larson MC, Hertsgaard L, Harris ML, Brodersen L. The stressfulness of separation among nine-month-old infants: Effects of social context variables and infant temperament. Child Development. 1992;63(2):290–303. doi: 0.1111/j.1467-8624.1992.tb01627.x. [PubMed] [Google Scholar]
- Hagan MJ, Roubinov DS, Gress-Smith J, Luecken LJ, Sandler IN, Wolchik S. Positive parenting during childhood moderates the impact of recent negative events on cortisol activity in parentally bereaved youth. Psychopharmacology. 2011;214(1):231–238. doi: 10.1007/s00213-010-1889-5. doi: 10.1007/s00213-010-1889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel P, Petermann F. Perceived stress, coping, and adjustment in adolescents. Journal of Adolescent Health. 2006;38(4):409–415. doi: 10.1016/j.jadohealth.2005.02.014. doi:10.1016/j.jadohealth.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Mermelstein R, Roesch L. Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development. 2007;78(1):279–295. doi: 10.1111/j.1467-8624.2007.00997.x. doi: 10.1111/j.1467-8624.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- Jacobs JE, Lanza S, Osgood DW, Eccles JS, Wigfield A. Changes in children's self-competence and values: Gender and domain differences across grades one though twelve. Child Development. 2002;73:509–527. doi: 10.1111/1467-8624.00421. [DOI] [PubMed] [Google Scholar]
- Kemeny ME. The psychobiology of stress. Current Directions in Psychological Science. 2003;12(4):124–129. doi: 10.1111/1467-8721.01246. [Google Scholar]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology: Psychological influences on immune function and health. Journal of Consulting and Clinical Psychology. 2002;70(3):537.–547. doi: 10.1037//0022-006x.70.3.537. doi: 10.1037/0022-006X.70.3.537. [DOI] [PubMed] [Google Scholar]
- King RB, Karuntzos GT, Casper LM, Moen P, Davis KD, Berkman L, Durham M, Kossek EE. Work-family balance issues and work-leave policies. In: Gatchel RJ, Schultz IZ, editors. Handbook of occupational health and wellness. Springer; New York, NY: 2012. pp. 323–339. [Google Scholar]
- Larson RJ, Kasimatis M. Day-to-day physical symptoms: Individual differences in the occurrence, duration, and emotional concomitants of minor daily illnesses. Journal of Personality. 1991;59(3):387–423. doi: 10.1111/j.1467-6494.1991.tb00254.x. doi: 10.1111/j.1467-6494.1991.tb00254.x. [DOI] [PubMed] [Google Scholar]
- Mallers MH, Charles ST, Neupert SD, Almeida DM. Perceptions of childhood relationships with mother and father: daily emotional and stressor experiences in adulthood. Developmental Psychology. 2010;46(6):1651–1661. doi: 10.1037/a0021020. doi: 10.1037/a0021020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. doi:10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McHale SM, Crouter AC, Whiteman SD. The family contexts of gender development in childhood and adolescence. Social Development. 2003;12(1):125–148. doi: 10.1111/1467-9507.00225. [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–995. doi: 10.1037/a0024768. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16(2):361–388. doi: 10.1111/j.1467-9507.2007.00389.x. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neeck G, Federlin K, Graef V, Rusch D, Schmidt KL. Adrenal secretion of cortisol in patients with rheumatoid arthritis. Journal of Rheumatology. 1990;17(1):24–29. [PubMed] [Google Scholar]
- Piazza JR, Almeida DM, Dmitrieva NO, Klein LC. Frontiers in the use of biomarkers of health in research on stress and aging. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65(5):513–525. doi: 10.1093/geronb/gbq049. doi: 10.1093/geronb/gbq049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Sliwinski MJ, Mogle J, Almeida DM. Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine. 2013;45(1):110–120. doi: 10.1007/s12160-012-9423-0. doi: 10.1007/s12160-012-9423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polk DE, Cohen S, Doyle WJ, Skoner DP, Kirschbaum C. State and trait affect as predictors of salivary cortisol in healthy adults. Psychoneuroendocrinology. 2005;30(3):261–272. doi: 10.1016/j.psyneuen.2004.08.004. doi: 10.1016/j.psyneuen.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Power TG. Stress and coping in childhood: The parents’ role. Parenting: Science and Practice. 2004;4(4):271–317. doi: 10.1207/s15327922par0404_1. [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical linear models: Applications and data analysis methods. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Repetti RL, Robles TR, Reynolds B. Allostatic processes in the family. Development and Psychopathology. 2011;23(3):921–938. doi: 10.1017/S095457941100040X. doi: 10.1017/S095457941100040X. [DOI] [PubMed] [Google Scholar]
- Romeo RD. Adolescence: a central event in shaping stress reactivity. Developmental Psychobiology. 2010;52(3):244–253. doi: 10.1002/dev.20437. doi: 10.1002/dev.20437. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70(3):660–677. doi: 10.1111/1467-8624.00048. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. doi: http://dx.doi.org/10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. Children's reports of parental behavior: An inventory. Child Development. 1965;36(2):413–424. doi: 10.2307/1126465. [PubMed] [Google Scholar]
- Seiffge-Krenke I. Stress, coping, and relationships in adolescence. Erlbaum; Mahwah, New Jersey: 1995. [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, Brennan PA. Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2006;35(1):103–115. doi: 10.1207/s15374424jccp3501_9. doi: 10.1207/s15374424jccp3501_9. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Heron KE. Ecological momentary assessment (EMA) in family research. In: McHale SM, Amato P, Booth A, editors. Emerging methods in family research. Urban Institute; Washington, D.C.: 2014. pp. 145–161. [Google Scholar]
- Stawski RS, Cichy KE, Piazza JR, Almeida DM. Associations among daily stressors and salivary cortisol: Findings from the National Study of Daily Experiences. Psychoneuroendocrinology. 2013;38(11):2654–2665. doi: 10.1016/j.psyneuen.2013.06.023. doi:10.1016/j.psyneuen.2013.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Morris AS. Adolescent development. Journal of Cognitive Education and Psychology. 2001;2(1):55–87. doi: /10.1891/19458950178738344. [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, Niaura R. Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology. 2009;21(1):47–68. doi: 10.1017/S0954579409000042. doi: 10.1017/S0954579409000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychological Bulletin. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. doi: 10.1037/00332909.119.3.488. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]