Abstract
Objective
Inadequate sleep and heavy alcohol use have been associated with negative outcomes among college students; however, few studies have examined the interactive effects of sleep and drinking quantity in predicting alcohol-related consequences. This study aimed to determine if adequate sleep moderates the prospective association between weekly drinking quantity and consequences.
Method
College students (N = 568) who were mandated to an alcohol prevention intervention reported drinks consumed per week, typical sleep quantity (calculated from sleep/wake times), and perceptions of sleep adequacy as part of a larger research trial. Assessments were completed at baseline and one-, three-, and five-month follow-ups.
Results
Higher baseline quantities of weekly drinking and inadequate sleep predicted alcohol-related consequences at baseline and one-month follow-up. Significant interactions emerged between baseline weekly drinking quantity and adequate sleep in the prediction of alcohol-related consequences at baseline, one-, three-, and five-month assessments. Simple slopes analyses revealed that weekly drinking quantity was positively associated with alcohol-related consequences for those reporting both adequate and inadequate sleep, but this association was consistently stronger among those who reported inadequate sleep.
Conclusion
Subjective evaluation of sleep adequacy moderates both the concurrent and prospective associations between weekly drinking quantity and consequences, such that heavy-drinking college students reporting inadequate sleep experience more consequences as a result of drinking. Research needs to examine the mechanism(s) by which inadequate sleep affects alcohol risk among young adults.
Keywords: alcohol, drinking, college students, sleep, intervention
1. Introduction
Excessive alcohol use places many college students at risk for academic difficulties, injury, or even death (Blanco et al., 2008; Hingson, Zha, & Weitzman, 2009; Johnston, O'Malley, Bachman, & Schulenberg, 2012). Although some college students consume alcohol without experiencing negative consequences (Barnett et al., 2014; Barnett, Merrill, Kahler, & Colby, 2015; Hingson, 2010), many students who drink alcohol report health concerns, including mental health problems, risky sexual behaviors, and weight concerns (Oswalt, Lederer, & Schrader, 2015). Research is needed to understand the behavioral patterns that increase risk of adverse alcohol consequences among young adults.
One potential risk factor for negative drinking-related outcomes is sleep. Poor sleep has been linked to greater alcohol misuse among adolescents (Wong, Robertson, & Dyson, 2015), college students (Kenney, LaBrie, Hummer, & Pham, 2012; Kenney, Lac, LaBrie, Hummer, & Pham, 2013), community samples (Weissman, Greenwald, Nino-Murcia, & Dement, 1997), and alcohol-dependent patients (Brower, Krentzman, & Robinson, 2011). College students, in particular, tend to report irregular and insufficient sleep (Gellis, Park, Stotsky, & Taylor, 2014; Tsai & Li, 2004), with 12 to 14 percent of students reporting clinically significant symptoms of a sleep disorder (Gellis et al., 2014; Petrov, Lichstein, & Baldwin, 2014) and as many as 60 percent reporting poor sleep quality (Kenney et al., 2012; Lund, Reider, Whiting, & Prichard, 2010).
Inadequate sleep may increase risk for alcohol-related consequences among young adults. One mechanism to explain this association involves the tendency for sleep deprivation to decrease inhibition (Anderson & Platten, 2011) and impair decision-making (Killgore, Balkin, & Wsensten, 2006; Schnyer, Zeithamova, & Williams, 2009). Consistent with this hypothesis, poor sleep has been linked to increased alcohol-related consequences among college students after accounting for demographic variables and psychiatric problems (Kenney et al., 2013). Moreover, self-reported global sleep quality has been shown to moderate the association between alcohol use and related consequences in cross-sectional research, such that heavy-drinking college students experiencing worse sleep quality reported a significantly greater number of alcohol-related problems (Kenney et al., 2012). When interpreting these data, however, it is not clear whether sleep difficulty precedes alcohol-related consequences or vice versa.
The current study extends previous research by determining if inadequate sleep moderates the association between weekly drinking quantity and alcohol-related consequences both concurrently and prospectively. Consistent with previous cross-sectional research (Kenney et al., 2012), we hypothesized that subjective reports of inadequate sleep would moderate the association between drinks consumed per week and alcohol-related consequences, such that individuals who drank more and reported inadequate sleep would report a greater number of alcohol-related consequences as a result of drinking. Because sleep difficulty has been identified a predictor of problematic alcohol use in longitudinal studies of adolescents (Wong et al., 2015), we also hypothesized that this moderating effect would endure over time.
2. Materials and Methods
2.1 Participants and Procedure
All study procedures were approved by the university's Institutional Review Board. Undergraduate students at a public, four-year, research university in the Northeast were recruited to participate in a larger research project (Carey et al., 2015). Students who violated campus alcohol policy and were mandated to participate in an alcohol education program by the Office of Community Standards between November 2011 and December 2013 were presented with the option of either participating in the research study (evaluating two brief interventions for alcohol use) or participating in the standard sanction. All students who consented to participate in the larger study were included in current analyses. Data for this study were collected at baseline, one-, three-, and five-month assessments. The baseline and one-month assessments were online surveys, which were completed in a private suite and facilitated by a research assistant; the two subsequent assessments were completed online from remote locations. The final sample consisted of 568 students (72% male, 84% White) with a mean age of 19.18 years (SD = 1.16). Participants included freshmen (38%), sophomores (35%), juniors (18%), and seniors (9%).
2.2 Measures
2.2.1 Descriptive information
Participants provided information regarding their gender, age, height, weight, year in school, race/ethnicity, and fraternity/sorority (‘Greek’) affiliation. They also responded to four items estimating their typical bedtimes and waketimes on weekends and weekdays in the past month (e.g., “What time do you usually go to bed on week days?”) (Wolfson & Carskadon, 1998). Self-reported sleep times were used to estimate total sleep time per night but did not account for time spent awake in bed (i.e., sleep onset latency or wake after sleep onset).
2.2.2 Sleep Adequacy
Participants indicated how often they experience adequate sleep by responding to the item, “How often do you think that you get enough sleep?” on a scale from 0 (never) to 4 (always) (Wolfson & Carskadon, 1998). Subjective perception of sleep adequacy, rather than total sleep time, was used in analyses to account for individual differences in sleep need (i.e., some individuals may wake feeling rested after seven hours of sleep, while others may need nine hours to achieve the same subjective experience of restfulness) (Blunden & Galland, 2014; Carskadon & Short, 2014).
2.2.3 Alcohol use
The Daily Drinking Questionnaire (DDQ) (Collins, Parks, & Marlatt, 1985) was used to assess alcohol use over the past month. The DDQ was used to calculate typical drinks per week. A standard drink was defined as 12 oz. of beer, 5 oz. of 12% table wine, 12 oz. of wine cooler, or 1.25 oz. of 80-proof liquor.
2.2.4 Alcohol-related consequences
The Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ) (Kahler, Strong, & Read, 2005) is a 24-item self-administered assessment of problems related to drinking; responses are dichotomous (yes/no) and refer to the past month. The B-YAACQ has demonstrated strong psychometric properties and is free of gender bias (Kahler et al., 2005). Example items include, “I have felt very sick to my stomach or thrown up after drinking,” and, “I have woken up in an unexpected place after heavy drinking.” Reliability in this sample was high (α = .84).
2.3 Data Screening & Analysis
Data were screened for missing values, outliers, and normality prior to analysis. No imputation procedures were used for missing values; therefore, Ns vary across analyses. For count variables, we trimmed outliers above three times the interquartile range from the 75th percentile plus one unit (Tukey, 1977). After accounting for outliers in this way, skewness and kurtosis estimates were within the normal range (Kline, 2011).
Hierarchical multiple regression analyses were used to test the hypothesized interactions. All analyses were conducted in SAS 9.4, and separate analyses were performed for each of the four outcomes. Prior to conducting the regression analyses, predictor variables, drinks consumed per week, and sleep adequacy were mean centered to aid in interpretation of interactions. In all models, participants' gender (0 = female, 1 = male), age, ethnicity (0 = non-White, 1 = White), and Greek (fraternity/sorority) affiliation (0 = no, 1 = yes) were included as covariates.1 When modeling one-, three-, and five-month alcohol-related consequences, baseline consequences score was added as a covariate. Moderation analyses were conducted in two steps. First, drinks per week and sleep adequacy were regressed onto alcohol-related consequences at baseline, one, three, and five months. Next, the interaction between drinks per week and sleep adequacy and their respective main effects were regressed on each alcohol-related problems outcome. When significant interactions emerged, tests of simple slopes were used to evaluate the association between drinks per week and alcohol-related consequences at high (+1 SD) and low (-1 SD) levels of adequate sleep (Cohen, Cohen, West, & Aiken, 2003).
3. Results
3.1 Descriptive Statistics
Correlations, means, and standard deviations for study variables are presented in Table 1. At baseline, participants reported having an average of 12.49 (SD = 9.25) standard drinks over 2.42 (SD = 1.22) days in a typical week and experiencing 5.44 (SD = 4.25) alcohol-related consequences in the past month. The majority of participants reported ‘sometimes’ (38%) getting enough sleep, while smaller numbers of participants reported ‘never’ (2%), ‘rarely’ (18%), ‘usually’ (37%), or ‘always’ (5%) obtaining adequate amounts of sleep. These subjective reports corresponded with an average total sleep time of 8.27 hours of sleep per night (SD = 1.02; range 4.8-11.0), not accounting for time spent awake in bed. Overall, 2% of participants reported less than 6 hours of sleep per night, 6% reported 6 to 6.9 hours, 27% reported 7 to 7.9 hours, 40% reported 8 to 8.9 hours, 20% reported 9 to 9.9 hours, and 5% reported 10 to 11 hours per night.
Table 1. Descriptive statistics and zero-order correlations among study variables (N = 568).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Male gender | -- | |||||||||
| 2. Age | -.05 | -- | ||||||||
| 3. White race | -.08 | .03 | -- | |||||||
| 4. Greek affiliation | -.04 | .03 | -.01 | -- | ||||||
| 5. Baseline drinks per week | -.28*** | .14** | .20*** | .18*** | -- | |||||
| 6. Baseline sleep adequacy | -.10* | .12** | .14** | -.01 | .06 | -- | ||||
| 7. Problems at baseline | .04 | .04 | .02 | .09* | .43*** | -.17*** | -- | |||
| 8. Problems at 1 month | -.08 | .01 | .17** | .11* | .32*** | -.07** | .40*** | -- | ||
| 9. Problems at 3 months | -.06 | .01 | .03 | .08 | .32*** | -.06 | .37*** | .50*** | -- | |
| 10. Problems at 5 months | -.02 | .11 | .08 | .03 | .28*** | -.18** | .36*** | .57*** | .55*** | -- |
|
| ||||||||||
| N or Mean | 407 | 19.18 | 475 | 94 | 12.49 | 2.23 | 5.44 | 3.05 | 3.28 | 3.16 |
| % or SD | 71.7 | 1.16 | 83.6 | 16.5 | 9.25 | 0.88 | 4.25 | 3.88 | 4.04 | 4.20 |
Note.
p < .05,
p < .01,
p < .001.
Zero-order correlations revealed significant positive associations between baseline drinks consumed per week and alcohol-related consequences at baseline, one month, three months, and five months. Though it was not significantly related to drinks per week at baseline, adequate sleep at baseline was negatively associated with alcohol-related consequences at baseline and one-month follow-up (see Table 1).
3.2 Main Effects
Complete data for all main effects and interactions are presented in Table 2. Greater baseline drinks per week (DPW) and lower baseline levels of adequate sleep predicted alcohol-related consequences at baseline [BDPW = .23, SE = .02, t(536) = 12.34, p < .001; Bsleep = -0.87, SE = .18, t(536) = -4.70, p < .001] and one-month follow-up [BDPW = .07, SE = .02, t(518) = 4.16, p < .001; Bsleep = -0.39, SE = .16, t(518) = -2.46, p = .01]. At three- and five-month follow-ups, drinks per week [B3mo = 0.07, SE = .02, t(375) = 3.03, p = .003; B5mo = 0.10, SE = .03, t(328) = 3.58, p < .001], but not sleep adequacy [B3mo = -0.13, SE = .21, t(375) = -0.62, p = .54; B5mo = -0.09, SE = .24, t(328) = -0.37, p = .71], predicted alcohol-related consequences.
Table 2. Main effects and interactions for alcohol-related consequences.
| Baseline Alcohol-Related Consequences | |||||
|---|---|---|---|---|---|
|
| |||||
| B | SE | β | t | p | |
|
|
|
|
|
||
| Step 1: Main Effects | |||||
| Age | -0.03 | .14 | -.01 | -.18 | .85 |
| Male gender | 1.59 | .37 | .17 | 4.35 | <.001 |
| White race | -0.48 | .44 | -.04 | -1.08 | .28 |
| Greek affiliation | 0.09 | .44 | .01 | .20 | .84 |
| Drinks per week | 0.23 | .02 | .50 | 12.34 | < .001 |
| Sleep adequacy | -0.87 | .18 | -.18 | -4.70 | < .001 |
| Step 2: Interactions | |||||
| Sleep × Drinks per week | -0.05 | .02 | -.10 | -2.59 | .01 |
|
| |||||
| 1-Month Alcohol-Related Consequences | |||||
|
| |||||
| Step 1: Main Effects | |||||
| Age | -0.16 | .12 | -.05 | -1.40 | .16 |
| Male gender | 0.01 | .31 | .002 | .04 | .97 |
| White race | 0.42 | .38 | .04 | 1.10 | .27 |
| Greek affiliation | 0.97 | .36 | .10 | 2.66 | .008 |
| Baseline alcohol consequences | 0 .25 | .04 | .30 | 6.78 | < .001 |
| Drinks per week | 0.07 | .02 | .20 | 4.16 | < .001 |
| Sleep adequacy | -0.39 | .16 | -.10 | -2.46 | .01 |
| Step 2: Interactions | |||||
| Sleep × Drinks per week | -0.03 | .02 | -.08 | -2.02 | .04 |
|
| |||||
| 3-Month Alcohol-Related Consequences | |||||
|
| |||||
| Step 1: Main Effects | |||||
| Age | -0.12 | .16 | -.04 | -.81 | .42 |
| Male gender | -0.17 | .40 | -.02 | -.43 | .67 |
| White race | 1.28 | .48 | .12 | 2.65 | .009 |
| Greek affiliation | 0.35 | .48 | .03 | .72 | .47 |
| Baseline alcohol consequences | 0.26 | .05 | .30 | 5.57 | < .001 |
| Drinks per week | 0.07 | .02 | .18 | 3.03 | .003 |
| Sleep adequacy | -0.13 | .21 | -.03 | -0.62 | .54 |
| Step 2: Interactions | |||||
| Sleep × Drinks per week | -0.05 | .02 | -.11 | -2.34 | .02 |
|
| |||||
| 5-Month Alcohol-Related Consequences | |||||
|
| |||||
| Step 1: Main Effects | |||||
| Age | -0.19 | .18 | -.06 | -1.07 | .28 |
| Male gender | -0.22 | .45 | -.03 | -.49 | .62 |
| White race | -0.28 | .57 | -.03 | -.51 | .61 |
| Greek affiliation | 0.26 | .58 | .02 | .45 | .65 |
| Baseline alcohol consequences | 0.24 | .05 | .26 | 4.42 | <.001 |
| Drinks per week | 0.10 | .03 | .23 | 3.58 | < .001 |
| Sleep adequacy | -0.09 | .24 | -.02 | -0.37 | .71 |
| Step 2: Interactions | |||||
| Sleep × Drinks per week | -0.05 | .02 | -.10 | 2.00 | < .05 |
3.3 Moderated Effects2
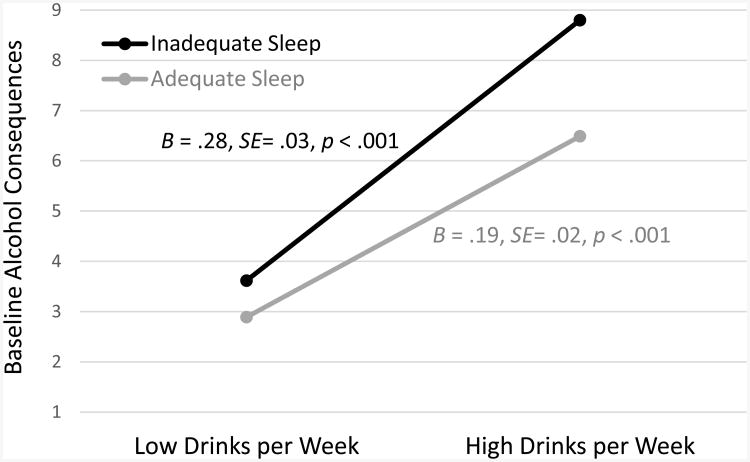
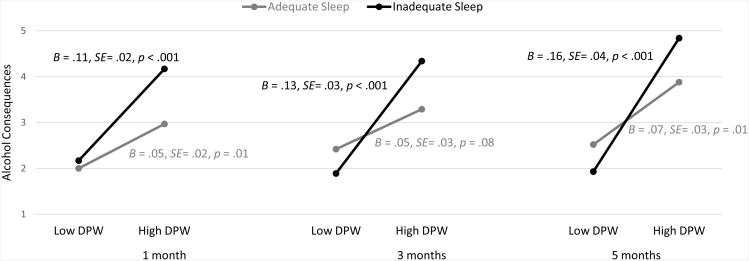
At baseline, there was a significant interaction between DPW and adequate sleep in the prediction of alcohol-related problems [B = -.05, SE = .02, t(535) = -2.59, p = .01]. Results of simple slopes analyses indicated that DPW was positively associated with alcohol-related consequences for those with both adequate (B = .19, SE= .02, p < .001) and inadequate (B = .28, SE= .03, p < .001) sleep. However, the association between drinking and alcohol-related consequences was stronger among those who reported inadequate sleep (see Figure 1). The interaction between DPW and adequate sleep remained a significant predictor of alcohol-related problems at one-month [B = -.03, SE = .02, t(517) = -2.02, p = .04], three-month [B = -.05, SE = .02, t(374) = -2.34, p = .02], and five-month follow-ups [B = -.05, SE = .02, t(327) = -2.00, p < .05], with simple slopes analyses revealing trends similar to those found cross-sectionally (see Figures 1-2).
Figure 1.
Regression lines for the drinks per week by inadequate sleep interaction on alcohol-related consequences at baseline.
Figure 2.
Regression lines for the drinks per week (DPW) by inadequate sleep interaction on alcohol-related consequences at one-, three-, and five-month follow-ups.
4. Discussion
This study extends the previous literature by establishing prospective associations between alcohol use, adequate sleep, and subsequent drinking outcomes. The majority of participants reported ‘sometimes’ getting enough sleep each night. Consistent with previous research (Kenney et al., 2012), sleep adequacy and typical weekly drinking quantity were unrelated; however, sleep adequacy moderated the association between alcohol use and consequences, such that those reporting less adequate sleep experienced a greater number of alcohol-related consequences as a result of drinking. Moreover, this finding was maintained at one-, three-, and five-month follow-ups, indicating that insufficient sleep can have a long-lasting, albeit indirect, effect on alcohol use outcomes.
Given the lack of direct associations between typical weekly drinking quantity and subjective reports of adequate sleep, the precise manner by which sleep influences alcohol-related consequences remains unclear. Sleep deprivation has been associated with impaired integrative decision-making among young adults (Schnyer et al., 2009), in which case heavy-drinking college students who are not receiving adequate sleep may have difficulty implementing protective behaviors (e.g., pacing alcohol consumption, drinking water or eating between drinks, staying with a buddy) that might buffer the association between alcohol use and consequences. Alternatively, because sleep deprivation has been associated with impulsive responses to negative stimuli (Anderson & Platten, 2011) and weakened ability to inhibit aggression (Kahn-Greene, Lipizzi, Conrad, Kamimori, & Killgore, 2006), inadequate sleep may heighten risk for aggressive behaviors while drinking. Sleep disturbance has also been associated with decreased positive mood (Acheson, Richards, & de Wit, 2007; Jean-Louis, von Gizycki, Zizi, & Nunes, 1998; Lund et al., 2010) and may precede the onset of depression in adolescents and young adults (Lovato & Gradisar, 2014). Therefore, it is possible that inadequate sleep leads to changes in mood that lead to changes in motives for drinking (e.g., drinking to cope). There is preliminary evidence for this hypothesis, as drinking to cope has been associated with increased alcohol-related harm among those receiving inadequate sleep (Kenney, Paves, Grimaldi, & LaBrie, 2014). Thus, in the presence of inadequate sleep, alcohol intoxication may result in failures of self-regulation that may subsequently result in negative alcohol-related consequences.
The prevalence of chronically inadequate sleep among the mandated students in the current sample is disconcerting. Approximately 20 percent reported never or rarely obtaining enough sleep, and an additional 38 percent reported receiving adequate sleep only ‘sometimes.’ These findings are consistent with data that up to 50 percent of college students report daytime sleepiness (DeMartini & Fucito, 2014) and 12 to 13 percent report clinically significant symptoms of insomnia (Gellis et al., 2014). Interestingly, the average total sleep time reported by participants in the current study was higher than that reported in previous research (Lund et al., 2010); however, these estimates do not account for sleep onset latency or wake after sleep onset and, therefore, may overestimate actual sleep duration. Although college students tend to minimize the importance of mild sleep problems (Orzech, Salafsky, & Hamilton, 2011), chronically disrupted sleep may alter individuals' cognitive and emotional perceptions of, and therefore responses to, stressful life events (Meerlo, Sgoifo, & Suchecki, 2008). Thus, efforts to enhance college students' sleep quality in service of better mental health may be warranted.
Our findings replicate a previous study showing that sleep difficulty moderates the associations between heavy alcohol use and consequences (Kenney et al., 2012) and demonstrate that this associations persists over time. These findings suggest that improving the adequacy of sleep among heavy-drinking college students may decrease their risk for negative alcohol consequences. The majority of college students are interested in receiving information about sleep difficulties (Wagner & Rhee, 2013), and sleep habits can be improved as a result of sleep education (Orzech et al., 2011); however, few published studies have examined the efficacy of sleep interventions for college students.
Several limitations of this study should be noted when interpreting results. First, data were collected as part of a larger trial examining the effects of a brief motivational intervention for college student drinking; therefore, only brief measures of sleep duration and adequacy were available for secondary data analysis. Because the current study replicated findings of a study that used a reliable and valid measure of global sleep quality (Kenney et al., 2012), however, it is unlikely that outcomes were spurious. Given the design of the current study, we cannot determine why inadequate sleep predicts alcohol-related consequences several months later. Although our findings mirror those obtained with adolescents (Wong et al., 2015), use of an event-level (or similarly detailed) methodology is needed to determine how sleep difficulty impacts subsequent alcohol use. Additional research examining the impact of alcohol use on sleep is also needed, as the nature of ‘inadequate sleep’ is ambiguous (e.g., insufficient sleep duration, inadequate slow-wave sleep). Similarly, although research is consistent in documenting decreases in REM sleep as a function of alcohol use, the impact of alcohol on sleep onset latency in late adolescents is mixed (Chan, Trinder, Andrewes, Colrain, & Nicholas, 2013; Ebrahim, Shapiro, Williams, & Fenwick, 2013; Van Reen, Jenni, & Carskadon, 2006; Van Reen, Rupp, Acebo, Seifer, & Carskadon, 2013). Given the effects of both alcohol use and daytime sleepiness on GPA (Singleton & Wolfson, 2009), research may also examine the synergistic effect of these factors on academic performance. Our data were also limited by the use of self-reported outcomes. However, self-reported estimates of both alcohol use (Leffingwell et al., 2013) and sleep patterns (Wolfson et al., 2003) correlate with more objective measures of these health behaviors among young adults. Finally, participants were recruited from one campus, were predominantly White underclassmen, and were mandated to participate in an alcohol education program. It is important to replicate these findings with more diverse and non-college-attending young adults.
4.1 Conclusion
The results of this study suggest that the subjective experience of sleep adequacy helps to explain the association between alcohol use and alcohol-related consequences among college students, such that heavy-drinking individuals reporting inadequate sleep experience a greater number of consequences as a result of drinking. This effect persisted up to five months, indicating that insufficient sleep may have a relatively long-lasting, indirect effect on the likelihood of alcohol-related consequences. We encourage research that examines the mechanism(s) by which insufficient sleep affects alcohol risk among young adults, as well as research evaluating the feasibility and efficacy of sleep interventions for college students.
Highlights.
Sleep adequacy moderates the association between drinking quantity and consequences.
Moderated effects exist concurrently and prospectively (up to five months).
Research examining the mechanism(s) by which sleep affects alcohol risk are needed.
Research regarding the efficacy of college sleep interventions is warranted.
Acknowledgments
Role of Funding Sources: This research was supported by grant numbers R01-AA012518 (PI: Kate B. Carey) and T32-AA007459 (PI: Peter Monti) from the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health. NIH had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Results were unchanged when study condition from the parent trial (i.e., a brief motivational intervention with either normative feedback email boosters or health promotion email boosters) was included in the model. When controlling for average total sleep time at baseline, the moderating effect of sleep adequacy on the association between drinking and consequences was also largely maintained (all ps ≤ .05).
Total sleep time (averaged across weekday and weekend nights) did not significantly moderate the association between drinking and consequences at baseline [B = -.02, SE = .02, t(529) = -0.97, p = .33], one-month [B = -.01, SE = .01, t(512) = -0.73, p = .47], three-month [B = -.001, SE = .02, t(371) = -0.07, p = .94], or five-month follow-ups [B = -.04, SE = .02, t(326) = -1.62, p = .11].
Contributors: Authors MPC and KBC designed the study and wrote the protocol. Authors MBM and SAL conducted literature searches and provided summaries of previous research studies. Author AMD conducted the statistical analysis. Author MBM wrote the first draft of the manuscript, and all authors contributed to and have approved the final manuscript.
Conflict of Interest: The authors have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acheson A, Richards JB, de Wit H. Effects of sleep deprivation on impulsive behaviors in men and women. Physiology & Behavior. 2007;91(5):579–587. doi: 10.1016/j.physbeh.2007.03.020. [DOI] [PubMed] [Google Scholar]
- Anderson C, Platten CR. Sleep deprivation lowers inhibition and enhances impulsivity to negative stimuli. Behav Brain Res. 2011;217(2):463–466. doi: 10.1016/j.bbr.2010.09.020. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Clerkin EM, Wood M, Monti PM, Tevyaw TOL, Corriveau D, et al. Kahler CW. Description and predictors of positive and negative alcohol-related consequences in the first year of college. Journal of Studies on Alcohol and Drugs. 2014;75(1):103–114. doi: 10.15288/jsad.2014.75.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Merrill JE, Kahler CW, Colby SM. Negative evaluations of negative alcohol consequences lead to subsequent reductions in alcohol use. Psychology of Addictive Behaviors. 2015 doi: 10.1037/adb0000095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blunden S, Galland B. The complexities of defining optimal sleep: empirical and theoretical considerations with a special emphasis on children. Sleep Med Rev. 2014;18(5):371–378. doi: 10.1016/j.smrv.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Brower KJ, Krentzman A, Robinson EA. Persistent insomnia, abstinence, and moderate drinking in alcohol-dependent individuals. American Journal of Addictions. 2011;20(5):435–440. doi: 10.1111/j.1521-0391.2011.00152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Walsh JL, Merrill JE, Lust SA, Kalichman SC, Carey MP. Using email boosters to maintain change after brief alcohol interventions for mandated college students: A randomized controlled trial. 2015 doi: 10.1037/ccp0000339. Manuscript in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Short MA. Measuring sleep need. Sleep Med Rev. 2014;18(5):369–370. doi: 10.1016/j.smrv.2014.06.007. [DOI] [PubMed] [Google Scholar]
- Chan JKM, Trinder J, Andrewes HE, Colrain IM, Nicholas CL. The acute effects of alcohol on sleep architecture in late adolescence. Alcoholism: Clinical and Experimental Research. 2013;37:1720–1728. doi: 10.1111/acer.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Fucito LM. Variations in sleep characteristics and sleep-related impairment in at-risk college drinkers: A latent profile analysis. Health Psychology. 2014;33(10):1164–1173. doi: 10.1037/hea0000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: Effects on normal sleep. Alcoholism: Clinical and Experimental Research. 2013;37:539–549. doi: 10.1111/acer.12006. [DOI] [PubMed] [Google Scholar]
- Gellis LA, Park A, Stotsky MT, Taylor DJ. Associations between sleep hygiene and insomnia severity in college students: Cross-sectional and prospective analyses. Behavior Therapy. 2014;45(6):806–816. doi: 10.1016/j.beth.2014.05.002. [DOI] [PubMed] [Google Scholar]
- Hingson RW. Magnitude and prevention of college drinking and related problems. Alcohol Research & Health. 2010;33(1-2):45–54. [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. Journal of Studies on Alcohol and Drugs. 2009;(16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, von Gizycki H, Zizi F, Nunes J. Mood states and sleepiness in college students: Influences of age, sex, habitual sleep, and substance use. Perceptual and Motor Skills. 1998;87(2):507–512. doi: 10.2466/pms.1998.87.2.507. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg J. Monitoring the Future National Survey Results on Drug Use, 1975-2011 Volume II: College Students and Adults Ages 19-50. Institute for Social Research. The University of Michigan; Ann Arbor, MI: 2012. [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kahn-Greene ET, Lipizzi EL, Conrad AK, Kamimori GH, Killgore WDS. Sleep deprivation adversely affects interpersonal responses to frustration. Personality and Individual Differences. 2006;41(8):1433–1443. doi: 10.1016/j.paid.2006.06.002. [DOI] [Google Scholar]
- Kenney SR, LaBrie JW, Hummer JF, Pham AT. Global sleep quality as a moderator of alcohol consumption and consequences in college students. Addictive Behaviors. 2012;37(4):507–512. doi: 10.1016/j.addbeh.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Lac A, LaBrie JW, Hummer JF, Pham A. Mental health, sleep quality, drinking motives, and alcohol-related consequences: A path-analytic model. Journal of Studies on Alcohol and Drugs. 2013;74(6):841–851. doi: 10.15288/jsad.2013.74.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Paves AP, Grimaldi EM, LaBrie JW. Sleep quality and alcohol risk in college students: Examining the moderating effects of drinking motives. Journal of American College Health. 2014;62(5):301–308. doi: 10.1080/07448481.2014.897953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WDS, Balkin TJ, Wsensten NJ. Impaired decision making following 49 h of sleep deprivation. Journal of Sleep Research. 2006;15(1):7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 3rd. New York, NY: Guilford Press; 2011. [Google Scholar]
- Leffingwell TR, Cooney NJ, Murphy JG, Luczak S, Rosen G, Dougherty DM, Barnett NP. Continuous objective monitoring of alcohol use: twenty-first century measurement using transdermal sensors. Alcohol Clin Exp Res. 2013;37(1):16–22. doi: 10.1111/j.1530-0277.2012.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Medicine Reviews. 2014;18:521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008;12(3):197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Orzech KM, Salafsky DB, Hamilton LA. The state of sleep among college students at a large public university. Journal of American College Health. 2011;59(7):612–619. doi: 10.1080/07448481.2010.520051. [DOI] [PubMed] [Google Scholar]
- Oswalt SB, Lederer AM, Schrader LT. Institutional characteristics and the connection to college student health. American Journal of Health Behavior. 2015;39(4):475–486. doi: 10.5993/AJHB.39.4.4. [DOI] [PubMed] [Google Scholar]
- Petrov ME, Lichstein KL, Baldwin CM. Prevalence of sleep disorders by sex and ethnicity among older adolescents and emerging adults: Relations to daytime functioning, working memory, and mental health. Journal of Adolescence. 2014;37(5):587–597. doi: 10.1016/j.adolescence.2014.04.007. [DOI] [PubMed] [Google Scholar]
- Schnyer DM, Zeithamova D, Williams V. Decision-making under conditions of sleep deprivation: Cognitive and neural consequences. Military Psychology. 2009;21(Suppl 1):S36–S45. doi: 10.1080/08995600802554607. [DOI] [Google Scholar]
- Singleton RA, Jr, Wolfson AR. Alcohol consumption, sleep, and academic performance among college students. Journal of Studies on Alcohol and Drugs. 2009;70(3):355–363. doi: 10.15288/jsad.2009.70.355. [DOI] [PubMed] [Google Scholar]
- Tsai LL, Li SP. Sleep patterns in college students. Journal of Psychosomatic Research. 2004;56(2):231–237. doi: 10.1016/s0022-3999(03)00507-5. [DOI] [PubMed] [Google Scholar]
- Tukey JW. Exploratory Data Analysis. Reading, MA: Addison-Wesley; 1977. [Google Scholar]
- Van Reen E, Jenni OG, Carskadon MA. Effects of alcohol on sleep and the sleep electroencephalogram in healthy young women. Alcoholism: Clinical and Experimental Research. 2006;30:974–981. doi: 10.1111/j.1530-0277.2006.00111.x. [DOI] [PubMed] [Google Scholar]
- Van Reen E, Rupp TL, Acebo C, Seifer R, Carskadon MA. Biphasic effects of alcohol as a function of circadian phase. SLEEP. 2013;36:137–145. doi: 10.5665/sleep.2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner M, Rhee Y. Stress, sleep, grief: Are college students receiving information that interests them? College Student Journal. 2013;47(1):24–33. [Google Scholar]
- Weissman MM, Greenwald S, Nino-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. General Hospital Psychiatry. 1997;19(4):245–250. doi: 10.1016/S0163-8343(97)00056-X. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69(4):875–887. doi: 10.2307/1132351. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey for adolescents. Sleep: Journal of Sleep and Sleep Disorders Research. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcoholism: Clinical & Experimental Research. 2015;39(2):355–362. doi: 10.1111/acer.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]