Editor:
Let us thank Mjøen et al.1 for their kind words about our paper.2 I (RCW) apologize for using the word “recent” when referring to the clinical community’s increasing success in allograft transplantation. For someone first trained in HLA in 1973, and in the last year of his seventh decade, the last 25 years are in my recent memory and experience. However I suspect they are suggesting that HLA mismatching is not as important in 2013 as it was in 1987, when UNOS first created this data set. They further encourage us to subdivide the first adult kidney transplants into 5 year intervals and repeat our analyses which, they contend, will demonstrate the decreasing role of HLA.
First, the purpose of our paper was to determine the role of HLA matching among the many variables that affect kidney allograft failure. This required a complex statistical model with a large amount of information. To maximize the power of our Cox multivariate regressions we used all adult first kidney transplants from deceased donors between 1987 and 2013. We selected many covariates for the regressions so that any conclusion about our primary explanatory variable, HLA, would not be biased by an incomplete or ill-fitted model. A typical fully adjusted regression had 16 covariates with 68 variable values while 52 parameters and their errors were simultaneously estimated and appeared in the output. Therefore great power in the form of many transplants was needed to minimize the error of the estimates and to accommodate the complexity of the model’s design. This implies that subdividing the data in the manner that the authors suggest runs directly counter to our purpose. Looking at 5 year intervals would decrease the power of each analysis, lead to larger error, and lower the precision of the hazard ratios. Therefore we chose to use the most robust analysis for our paper and used an era variable with 5 values to control for the changing nature of clinical practice during this time.
Second, with the previous comments as a caution, I looked at the fully adjusted Cox regression for the 66,971 procedures performed during years 2009-2013. To maximize the sample size I incorporated all donor sources. Using 0 HLA mismatch as the reference, 1 mismatch has a hazard ratio (HR) = 1.17, 95% C.I. (0.82, 1.69), p = 0.3894, 2 mismatches [HR = 1.25 (0.98, 1.60), p = 0.0760], 3 mismatches [HR = 1.36 (1.10, 1.67), p = 0.0039], 4 mismatches [HR = 1.40 (1.14, 1.71), p = 0.0011], 5 mismatches [HR = 1.44 (1.18, 1.75), p = 0.0003], and 6 mismatches [HR= 1.54 (1.25, 1.89), p <.0001]. A line fitted to the HRs has a statistically significant linear fit (Figure 1). This is very close to the pattern that we reported in Figure 1 and Table 2 of our paper. With a sample size close to what we used in the robust analysis, 189,141 allografts, the error for the 2-mismatch value would almost certainly be smaller and the result statistically significant. While the 1-mismatch HR is close to the significant value that we reported in our paper, 1.13, there is not enough power in the analysis of this 5-year period to demonstrate a statistically significant effect for the smallest mismatch category.
Figure 1.
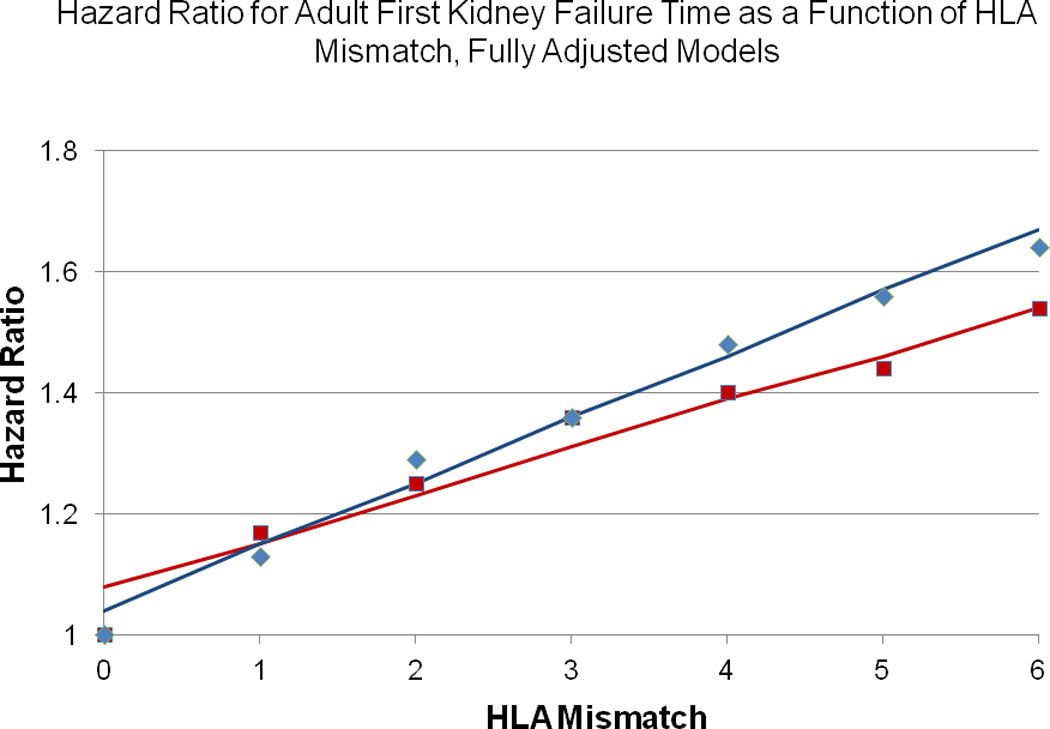
A line was fitted to the hazard ratios from a fully adjusted Cox regression for transplants in the UNOS data set for first adult kidney transplants with HLA mismatch as the primary explanatory variable. Blue diamonds are the observed HRs for deceased donors 1987-2013 with the blue fitted line; the intercept is 1.04 (0.98, 1.10), p < 0.0001, while the slope is 0.11 (0.09, 0.12), p < 0.0001.2 Red squares are observed HRs for all transplants 2009-2013 with the fitted red line; the intercept is 1.08 (0.98, 1.17), p <0.0001 while the slope of the line is 0.08 (0.06, 0.10), p = 0.0003. Adjustment was for recipient age, donor age, donor sex, transplant era, recipient ethnicity, recipient diabetes, cold ischemia time, recipient peak PRA, recipient education, recipient BMI, donor BMI, recipient working for income at transplant, recipient COPD, recipient dialysis type, induction and immunosuppression at discharge.
In summary, this sub-analysis is consistent with the pattern reported for all deceased-donor data. We are confident that HLA continues to have an important role in kidney transplantation.
Abbreviations
- UNOS
United Network for Organ Sharing
- HLA
Human Leukocyte Antigen
- HR
Hazard Ratio
- CI
Confidence Interval
Biographies
Robert C. Williams: Is responsible for the design and performance of the statistical analysis, wrote the first draft, acts as corresponding author, and is responsible for the accuracy and integrity of the work.
Gerhard Opelz: Participated in the design of the analysis, revises the drafts, has final approval on the submission manuscript, and is responsible for the integrity of the work.
E. Jennifer Weil: Participated in the design of the analysis, revises the drafts, has final approval on the submission of the manuscript, and is responsible for the integrity of the work.
Chelsea McGarvey: Revises the drafts, has final approval on the submission of the manuscript, and is responsible for the integrity of the work.
Harini Chakkera: Provided the UNOS STAR files for the work, participated in the design of the analysis, revises the drafts, has final approval on the submission of the manuscript, and is responsible for the integrity of the work.
Footnotes
Disclosures: The authors declare no conflict of interest.
References
- 1.Mjøen G, Reisaeter AV, Dahle DO. HLA mismatch and allograft survival. Transplantation. 2016 doi: 10.1097/TP.0000000000001366. XXX:XXXX-XXXX. [DOI] [PubMed] [Google Scholar]
- 2.Williams RC, Opelz G, McGarvey CJ, Weil EJ, Chakkera HA. The risk of transplant failure with HLA mismatch in first adult kidney allografts from deceased donors. Transplantation. 2016;100:1094–1102. doi: 10.1097/TP.0000000000001115. [DOI] [PMC free article] [PubMed] [Google Scholar]


