Abstract
PURPOSE
We assessed whether longitudinal changes in body mass index (BMI) is positively associated with changes in 10-year AHA/ACC atherosclerotic cardiovascular disease (ASCVD) risk scores in middle-aged blacks compared to whites.
METHODS
Data were from 1,691 participants enrolled in CARDIA aged ≥40 years in 2000–2001, who had follow-up exams 5 and 10 years later.
RESULTS
The prevalence of obesity increased from 32.3% in 2000–2001(mean age: 42.8 years) to 41.7% in 2010–2011, higher in blacks than whites. The corresponding change in 10-year ASCVD risk was significantly higher for blacks (men: 4.5 to 9.6%, women: 1.7 to 5.0%) than whites (men: 2.4 to 5.2%, women: 0.7 to 1.6%). In 2010–2011, 57.5% of black men had ASCVD risk scores ≥ 7.5% compared to white men (14.7%), black women (17.4 %) and white women (1.6%). Although BMI trends were positively associated with 10-year change in ASCVD risk scores (0.07% per 1 kg/m2 increase), it explained very little variance in risk score trends in all race-sex groups.
CONCLUSIONS
In middle-aged adults, longitudinal changes in BMI had little independent influence on changes in 10-year ASCVD risk scores as its effect may be largely mediated through ASCVD risk factors already accounted for in the risk score.
Keywords: Obesity, cardiovascular disease, risk prediction
INTRODUCTION
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of death in the United States, accounting for 31.3% of all deaths (1). Since 1950, a significant decline in age-adjusted mortality from ASCVD has been observed with the rate of decline greater in whites than blacks (2, 3). This decline has been attributed, in part, to positive changes in the prevalence of risk factors such as smoking (4, 5). However, in the same time frame, the prevalence of some ASCVD risk factors, i.e., hypertension (6), diabetes (7) and obesity (8) have increased with the latter reaching epidemic levels. The prevalence of obesity has stabilized in recent years, however more than 1 in 3 adults are considered to be obese with the estimate higher among blacks (47.8%) compared to whites (33.4%) (9).
Obesity is positively associated with many ASCVD risk factors including hypertension and diabetes as well as clinical CVD events and raises the risk of future ASCVD in young and middle-aged adults (10). However, results from studies incorporating BMI in ASCVD risk prediction models are equivocal (11–14). The Framingham Heart Study, a study made up entirely white participants, observed a weak independent association between BMI and CVD events which was lost when other CVD risk factors were updated every 4 years (14). ASCVD and obesity are disproportionately high among middle-aged blacks than whites (15) with the adverse health effects of obesity especially elevated for black women (16). Therefore, accurately estimating ASCVD risk in this racial group in the face of the current obesity epidemic is of great importance especially among middle-aged adults 40–59 years who bear the greatest burden of obesity.
Recent clinical practice guidelines from the American College of Cardiology/American Heart Association (ACC/AHA) recommend the use of the newly derived Pooled Cohort risk equation, which have the ability to estimate 10-year risk for broader-based ASCVD outcomes more relevant to women and blacks (11). Additionally, it has the unique advantage of providing risk estimates specific to blacks. Given the current obesity epidemic which is high among blacks and the known negative effect of obesity on ASCVD risk, we aimed to assess whether longitudinal changes in BMI levels over a 10 year period was associated positively with longitudinal changes in AHA/ACC ASCVD risk scores in middle-aged black adults compared to whites.
MATERIAL AND METHODS
Study population
The Coronary Artery Risk Development in Young Adults (CARDIA) study is a community-based longitudinal study designed to examine cardiovascular risk trends in young black and white men and women from four US communities (Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California). Details of the study design and methods are described elsewhere (17). Briefly, in 1985–1986, 5,115 healthy adults were recruited from the general population to be balanced on sex, race (white or black), age (18–24 or 25–30 years) and education (≤12, >12 years). To date, seven follow-up examinations have occurred after baseline with 72% of the surviving cohort attending the 2010–2011 exams. Data collection and follow-up protocols were approved by the Institutional Review Boards of each field center and the Coordinating Center.
Of the 3672 participants attending the 2000–2001 exams, we excluded participants who were < 40 years of age (lower limit for age based on the Pooled Risk equations cut-off) (n=1508), had prevalent CHD (n=18), did not attend the 2005–2006 or 2010–2011 exams (n= 413) or had missing values for BMI or components of the Pooled Cohort risk equation (n=42), resulting in an analytic sample of 1,691 men and women. Participants excluded from the analytic sample were more likely to be blacks, younger (by design), current smokers and have fewer years of education at 2000–2001.
Pooled Cohort risk equations
The ACC/AHA Pooled Cohort equation is a sex- and race-specific risk prediction model calculated using data from several cohort studies funded by the National Heart, Lung, and Blood Institute namely CARDIA, the Atherosclerosis Risk in Communities (ARIC) study, the Cardiovascular Health Study (CHS) and the Framingham Original and Offspring Study (11). This model, derived on individuals at least 40 years old using state-of-the-art statistical methods, incorporates age, sex, race, total cholesterol, HDL-cholesterol, blood pressure, antihypertensive medication, diabetes and smoking status to estimate absolute 10-year risk (expressed as a percentage) for ASCVD defined as nonfatal myocardial infarction or CHD death, nonfatal or fatal stroke. Unlike most conventional cardiovascular disease (CVD) risk equations, the Pooled Cohort risk equation was validated among black men and women, enhancing its ability to predict ASCVD in this racial group.
Measures
Sociodemographic factors (age, sex and race) and medication were all self-reported at each clinic visit. Cigarette smoking was assessed by means of an interviewer-administered tobacco questionnaire (18). Blood pressure was measured using a random-zero sphygmomanometer at 2000–2001 and an Omron aneroid device at years 2005–2006 and 2010–2011 with participants seated and after five minutes of rest. The average of the second and third consecutive measurements was used for analysis. Fasting plasma total cholesterol and high-density lipoprotein (HDL) cholesterol were measured enzymatically by Northwest Lipid Research Clinic Laboratory (19). Diabetes was defined by one or more of the following: elevated fasting plasma glucose levels ≥ 126 mg/dL, 2-hour oral glucose tolerance test ≥ 200 mg/dL, hemoglobin A1C ≥ 6.5%; or reported use of diabetes medications (insulin or oral hypoglycemics). Body weight was measured by trained and certified technicians to the nearest 0.2 kg using a calibrated scale with participants wearing light clothing. Height (without shoes) was measured to the nearest 0.5 cm using a vertical ruler. BMI was calculated by dividing weight in kilograms by height in meters squared with obesity defined as BMI ≥ 30 kg/m2).
Statistical Analysis
Race- and sex-specific descriptive statistics were calculated at 2000–2001 and 2010–2011 with comparisons undertaken using t-test and analysis of variance (ANOVA) for continuous variables and Chi-square test for categorical variables. Participants were also categorized according to 10-year ASCVD risk scores ≥ 7.5% as this threshold is recommended by the cholesterol guidelines (20) for consideration of statins treatment. Bivariate general linear regression models were used to assess the cross sectional association of ASCVD risk factors at 2000–2001 and 2010–2011 with BMI. Repeated-measures regression, which accounts for lack of independence between repeated observations on an individual, was used to model the association between ASCVD risk scores trends and longitudinal measures of BMI which were both assessed at years 2000–2001. 2005–2006 and 2010–2011. Trends in ASCVD risk scores were modeled first as a function of time and then with BMI added. Due to differences in the ASCVD risk by race and sex, all analyses were stratified to obtain sex- and race-specific estimates. Unstructured covariance was found to best specify the structure of the within-person error covariance based on the finite-population corrected Akaike Information Criteria (AICC) and the Schwarz’s Bayesian Information Criterion (BIC) (21). We compared all race- and sex-specific predicted means estimates obtained from models with and without BMI adjustment using the paired t-test and Wilcoxon signed-rank test to inform whether unadjusted ASCVD risk trends were significantly different from BMI-adjusted ASCVD trends. Finally, values of participants who developed CVD during follow-up (n=44) were set to missing at the time of event and after since ASCVD risk for such participants is 100% and the risk equations do not apply to them anymore. All statistical tests were two-sided and performed at the 0.05 level of significance using SAS9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
In 2000–2001, the mean age of the 1,691 participants was 42.8 ± 1.8 years (range: 40–46) with 55.9% and 37.5% being females and blacks, respectively. Additionally, a greater percentage of women reported black race compared to men (41.2 vs. 32.8%). While men had higher systolic blood pressure (115.3 vs. 111.8 mmHg) and total cholesterol (189.7 vs. 183.7 mg/dL), women had higher HDL-cholesterol levels (55.7 vs. 44.9 mg/dL). There were significant differences in the distributions of ASCVD risk factors by race and sex (Table 1). Black men had higher systolic blood pressure and HDL cholesterol, with a greater proportion of them being current smokers and on antihypertensive medication compared to white men. Similarly, black women also had higher systolic blood pressure and lower HDL cholesterol with a greater proportion being current smokers, on antihypertensive medication and having a history of diabetes.
Table 1.
Characteristics of study participants at year 15 and year 25, the CARDIA study
| Year 15 (2000–2001)
|
Year 25 (2010–2011)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||
|
| ||||||||
| Black (n = 245) | White (n= 501) | Black (n= 389) | White (n = 556) | Black (n = 245) | White (n= 501) | Black (n= 389) | White (n = 556) | |
|
| ||||||||
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | |
| Age (years) | 42.7 (1.7) | 42.7 (1.7) | 42.9 (1.8) | 42.8 (1.8) | 52.7 (1.8) | 52.7 (1.8) | 52.8 (1.8) | 52.8 (1.8) |
| Systolic blood pressure (mmHg) | 117.9 (15.4) | 114.0 (13.0)* | 117.9 (16.9) | 107.5 (12.4)* | 124.1 (13.8) | 119.3 (13.6)† | 124.5 (17.7) | 112.4 (14.1) † |
| Antihypertensive medication use | 12.2 | 5.6 * | 15.9 | 3.1 * | 42.0 | 23.0 † | 44.7 | 16.2 † |
| Total cholesterol (mg/dl) | 187.5 (44.5) | 190.8 (36.9) | 184.6 (32.0) | 183.0 (32.1) | 183.1 (36.8) | 189.4 (37.4) † | 196.1 (38.0) | 200.6 (34.6) |
| HDL cholesterol (mg/dl) | 47.1 (14.0) | 43.8 (12.2) * | 53.9 (13.8) | 56.9 (14.9)* | 53.0 (17.7) | 50.5 (14.5) † | 62.1 (17.0) | 67.4 (18.3) † |
| Current smoking status | 30.2 | 15.4 * | 25.2 | 12.4 * | 24.5 | 11.6 † | 20.1 | 8.1 † |
| Diabetes | 3.7 | 4.2 | 3.9 | 1.3 * | 21.6 | 10.2 † | 19.3 | 6.5 † |
| Lipid-lowering medication use | 2.9 | 5.0 | 1.3 | 1.3 | 22.0 | 22.8 | 22.1 | 12.2 † |
| Body mass index (kg/m2) | 29.4 (6.5) | 27.7 (4.8) * | 31.9 (7.7) | 26.6 (6.3) * | 30.8 (7.5) | 28.5 (4.7) † | 33.3 (7.8) | 28.0 (7.0) † |
| Obesity (BMI ≥ 30 kg/m2) | 36.3 | 23.6 * | 53.3 | 23.6 * | 46.5 | 32.6 † | 64.2 | 32.2 † |
Values are mean (standard deviation) for continuous variables and percentages for categorical variables.
HDL: High density lipoprotein
Significant differences (p <0.05) by race among men and women at year 15.
Significant differences (p <0.05) by race among men and women at year 25.
In 2010–2011, the average age of participants was 52.7±1.8 years. Similar to 2000–2001, several race-sex disparities in ASCVD risk factors were observed with black men and women having more adverse ASCVD risk factor profiles than whites. Systolic blood pressure levels as well as the prevalence of diabetes, current smoking and use of blood pressure medications were found to be significantly higher among black men and women. Of note, levels of HDL cholesterol and total cholesterol were significantly lower in black men than white men while a greater percentage of black women reported use of lipid-lowering medications compared to white women (22.1 vs. 12.2%).
The mean BMI of participants increased from 28.6 kg/m2 (blacks: 30.9; whites: 27.2) at 2000–2001 to 29.8 kg/m2 (blacks: 32.4, whites: 28.3) at 2010–2011 with black women having the highest values at both time points (Table 1). BMI was associated with adverse levels of all ASCVD risk factors at 2000–2001 and 2010–2011 with the exception of smoking (Table 2). The overall prevalence of obesity among the analytic cohort at year 2000–2001 was 32.3 % (27.8 % for men and 35.9 % for women) which increased to 41.7% by 2010–2011 (37.2 % for men and 45.3% for women). The prevalence of obesity was significantly higher among blacks regardless of sex at both 2000–2001 and 2010–2011 (Table 1). In 2010–2011, the prevalence of obesity among black men and women was 46.5% and 64.2% respectively, compared to 32.6% and 32.2% among white men and women.
Table 2.
Bivariate associations between components of the ASCVD risk score equation and BMI at Year 15 and 25: The CARDIA study
| ASCVD risk score components | Year 15
|
P value | Year 25
|
P value |
|---|---|---|---|---|
| β (95% CI) | β (95% CI) | |||
| Age (years) | 0.24 (0.06, 0.42) | 0.010 | 0.13 (−0.05, 0.32) | 0.161 |
| Systolic blood pressure (mmHg) | 0.15 (0.13, 0.17) | 0.001 | 0.10 (0.08, 0.12) | 0.001 |
| Total cholesterol (mg/dl) | 0.02 (0.01, 0.03) | 0.001 | −0.012 (−0.022, −0.003) | 0.009 |
| High density lipoprotein cholesterol (mg/dl) | −0.13 (−0.15, −0.11) | 0.001 | −0.11 (−0.13, −0.10) | 0.001 |
| Race (black) | 3.78 (3.16, 4.41) | 0.001 | 4.07 (3.40, 4.74) | 0.001 |
| Current smoking status | −0.39 (−1.20, 0.42) | 0.343 | −0.92 (−1.88, 0.04) | 0.060 |
| Lipid-lowering medication use | 1.31 (−0.67, 3.29) | 0.194 | 3.43 (2.59, 4.27) | 0.001 |
| Antihypertensive medication use | 6.40 (5.29, 7.52) | 0.001 | 5.22 (4.52, 5.93) | 0.001 |
| Diabetes | 6.16 (4.36, 7.96) | 0.001 | 6.00 (5.03, 6.96) | 0.001 |
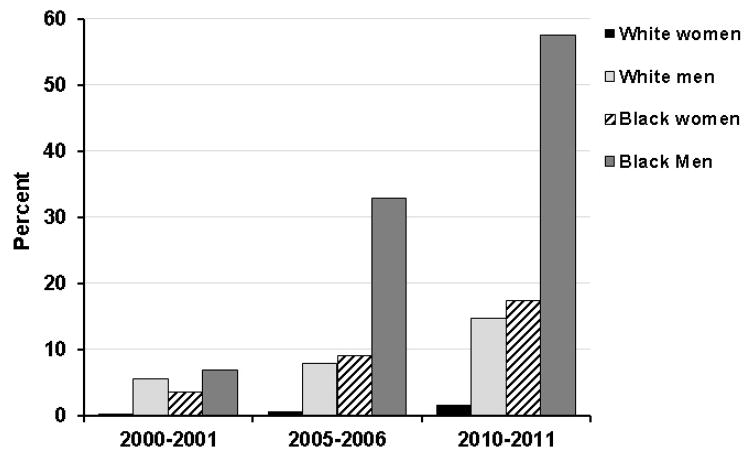
The average 10-year ASCVD risk increased from 2.0% at 2000–2001 to 4.6% at 2010–2011, as the average ages increased from 42.8 to 52.7 years. This 10-year change in ASCVD risk scores was significantly higher for men (3.1 to 6.8%) than women (1.1 to 3.1 %), p<0.001. Among men, blacks had a greater 10-year increase in ASCVD risk than whites (4.5 to 9.6% vs. 2.4 to 5.2%, p <0.001) with black women also having a higher 10-year change than white women (1.7 to 5.0% vs. 0.7 to 1.6%, p =0.005). By 2010–2011, 57.5% of black men were found to have 10-year ASCVD risk score ≥ 7.5% that was nearly fourfold higher than the equivalent percentage for white men (Figure 1). The proportion of middle-aged black women (17.4 %) with 10-year ASCVD risk score ≥ 7.5% was higher than those for white men (14.7%) and women (1.6%).
Figure 1.
Proportion of participants with ASCVD risk scores ≥ 7.5% by race, the CARDIA study.
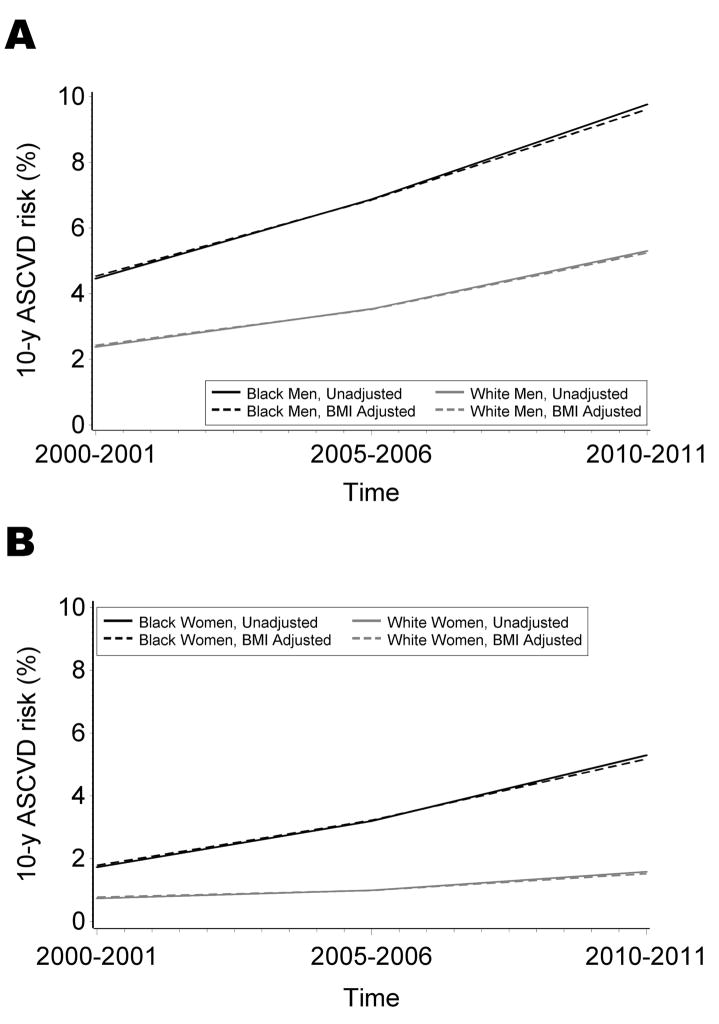
In repeated measures regression analysis, BMI (modeled as a time-varying covariate with measurements undertaken at 2000–2001, 2005–2006 and 2010–2011) was associated with minimal increase in ASCVD risk scores (0.07% per 1 kg/m2 increase, 95%CI: 0.06 – 0.09). However, comparison of unadjusted and BMI-adjusted ASCVD risk score trends for men (blacks, p = 0.699; whites, p = 0.829) or women (blacks, p = 0.828; whites. p = 0.830) did not approach statistical significance (Figure 2). Additionally, longitudinal trends of BMI did not explain the race-related differences in 10-year estimated ASCVD risk scores among men or women.
Figure 2.
Estimated 10-year ASCVD risk scores among men and women by race, the CARDIA study. Comparison of unadjusted and adjusted risk trends: black men: p = 0.669; white men: p = 0.829; black women p = 0.82; white women: p = 0.830.
DISCUSSION
In this community-based sample of middle-aged US adults observed from 2000–2001 to 2010–2011, a significantly greater proportion of blacks were observed to have higher obesity prevalence and 10-year ASCVD risk than whites. Black women had the highest prevalence of obesity with a greater proportion of them having 10-year risk ASCVD risk ≥ 7.5% compared to white men and women. Although BMI trends were positively associated with 10-year change in ASCVD risk scores, it explained very little variance in risk score trends in all race-sex groups, possibly due to its influence being largely mediated through risk factors already included in the risk score equation. The findings of this study do not in any way downplay the importance of obesity as a modifiable risk factor for atherosclerotic cardiovascular disease as obesity predicts diabetes, hypertension, and dyslipidemia (22–24).
The incorporation of BMI or obesity in CVD risk prediction models has received much attention due to the rising prevalence of obesity and CVD events worldwide. However, results from studies incorporating baseline BMI in ASCVD risk prediction models are equivocal (11–13). Although the present study estimated risk scores trends and not incident events, longitudinally assessed BMI was not significantly associated with changes in 10-year ASCVD estimated risk trends. Some possible explanations for the discrepancies in results include differences in risk prediction models used to estimate 10-year cardiovascular disease risk which have differing covariates, the functional form for modeling obesity, and variations in the population sampled and as well as CVD events of interest. We speculate that the omission of diabetes from some risk prediction models (11) may have resulted in obesity contributing to CVD risk prediction since obesity is a strong predictor of diabetes (10). As seen in this present study and the collaborative analysis of 58 prospective studies (13), when the relation of diabetes and other ASCVD risk factors associated with obesity are adequately accounted for, the independent predictive ability of obesity on ASCVD is attenuated. This idea is supported by results from the ARIC study (12) in which the addition of BMI alone to the base prediction model minimally improved CHD risk prediction.
ASCVD and obesity are disproportionately high among middle-aged black men and women, which may in part explain the greater morbidity and mortality from diseases associated with obesity among blacks than whites (15). However, we observed that, BMI did not explain the differences in 10-year ASCVD risk between whites and blacks. In the present study the prevalence of obesity among white men and women in 2010–2011 was 21% and 11% lower than the 2011–2012 national averages from the National Health and Nutrition Examination Survey among white men and women aged 40–59 years, respectively (9). On the other hand, the prevalence of obesity in black men and women was 22% and 10% higher than national averages for middle-aged black men and women, respectively. Reasons for the underlying causes for the racial differences in obesity and cardiovascular health are not well understood. A recent review of genome-wide association studies concluded that genetic factors do not provide explanations for the disparity in ASCVD incidence among blacks and whites (25), suggesting that differences in exposure to environmental and behavioral factors as well as differences in diagnosis, management and outcomes of many ASCVD risk factors by race may play important roles in explaining the black-white disparity (26). ASCVD risk factors tend to cluster more in blacks than whites, which puts them at an increased risk for ASCVD events (27, 28). Multiple trials have shown safety and efficacy of statins and antihypertensive medications in reducing LDL cholesterol and blood pressure in blacks and whites, although blacks were less likely to achieve the recommended treatment targets (29–31). This has been attributed to poor adherence to antihypertensive and lipid-lowering therapies among blacks (31). Increasing racial differences in ASCVD risk trends attributable to established risk factors namely hypertension and diabetes have been reported in the ARIC study (32), which suggests that population-wide interventions to improve ASCVD risk factor modification may not be benefiting blacks as much as whites (32).
The adverse health effects of obesity are especially elevated for black women (16). In the present study, almost 2 in 3 middle-aged black women (64%) were observed to be obese compared to 1 in 3 for white women, which confirms earlier CARDIA reports (28). This obesity gap between black and white women has been suggested to be one of the significant contributors to the racial disparity in health among women (16). In the present study, the proportion of black women with 10-year risk for ASCVD risk ≥ 7.5% was 10 fold higher than that for white women. Factors that have been suggested to contribute to the high obesity rate in black women include differences in diet (e.g. energy intake) and exercise (e.g. energy expenditure) (33). Despite similar adherence to diet intake and exercise among black and white women enrolled in intervention trials, less weight loss has been reported among blacks (34, 35). Therefore, reducing obesity prevalence to enhance cardiovascular health among blacks especially women, will require substantial public health efforts. These may include adapting culturally-tailored intensive lifestyle interventions (15, 33), implementing programs that improve ASCVD risk education, ensuring access to healthy foods and enhancing the built environment to promote physical activity.
The strengths of this study are its population-based design and the use of standardized ASCVD risk factors with high degree of quality control across all exam years that allow more accurate assessment of longitudinal trends in ASCVD risk factors. The use of the race-specific pooled cohort equation also enhanced the recognition and quantification of ASCVD risk among black men and women. Limitations for the study are as follows. First, some components of the ASCVD risk equation were self-reported. Second, the guideline writing committee and other studies have reported overestimation of ASCVD risk using the pooled cohort equations in other cohorts (36–40). However, recent results from the Multi-Ethnic Study of Atherosclerosis reports overestimation of risk among previously derived risk equations as well (37). This overestimation of risk by prediction models may be due to changing secular trends in unmeasured risk factors such as salt and trans fat intake, statins use and environmental pollution that are not accounted for in risk prediction models (37). Third, the presence of confounding by inflammation cannot be ruled out. Fourth, due to the eligibility criteria implemented in this study, only a subsample of the CARDIA cohort was included which may lead to potential selection bias. However, the prevalence of obesity among this subsample and the whole cohort was similar. Finally, results of this study may not be generalizable to other races beyond blacks and whites.
CONCLUSION
In this cohort of black and white middle-aged adults, the prevalence of obesity and 10-year risk of ASCVD was higher among blacks than whites regardless of sex. Adjusting for longitudinal trends of BMI did not significantly alter ASCVD risk prediction. This study provides valuable information as data on ASCVD risk among young adults transitioning to middle-age are sparse.
Acknowledgments
FUNDING SOURCES
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging (NIA), an intra-agency agreement between NIA and NHLBI (AG0005). ). Dr. Appiah was supported by NHLBI training grant T32HL007779.
LIST OF ABBREVIATIONS
- ACC
American College of Cardiology
- AHA
American Heart Association
- AICC
Corrected Akaike Information Criteria
- ANOVA
Analysis of variance
- ARIC
Atherosclerosis Risk in Communities Study
- ASCVD
Atherosclerotic cardiovascular disease
- BIC
Bayesian Information Criterion
- BMI
Body mass index
- CARDIA
Coronary Artery Risk Development in Young Adults Study
- CHS
Cardiovascular Health Study
- CVD
Cardiovascular disease
- HDL-c
High-density lipoprotein cholesterol
- SD
Standard deviation
Footnotes
DISCLOSURES
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Levi F, Lucchini F, Negri E, La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart. 2002;88(2):119–24. doi: 10.1136/heart.88.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2009;16(3):333–50. doi: 10.1097/HJR.0b013e328325d67d. [DOI] [PubMed] [Google Scholar]
- 4.Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annual review of public health. 2011;32:5–22. doi: 10.1146/annurev-publhealth-031210-101211. [DOI] [PubMed] [Google Scholar]
- 5.Sytkowski PA, Kannel WB, D’Agostino RB. Changes in risk factors and the decline in mortality from cardiovascular disease. The Framingham Heart Study. The New England journal of medicine. 1990;322(23):1635–41. doi: 10.1056/NEJM199006073222304. [DOI] [PubMed] [Google Scholar]
- 6.Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annual review of public health. 2006;27:465–90. doi: 10.1146/annurev.publhealth.27.021405.102132. [DOI] [PubMed] [Google Scholar]
- 7.Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA : the journal of the American Medical Association. 2014;312(12):1218–26. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 8.Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960–1962 through 2009–2010. Center of Disease Control and Prevention; Oct, 2013. [Google Scholar]
- 9.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA : the journal of the American Medical Association. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. The New England journal of medicine. 2007;357(23):2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63(25 Pt B):2935–59. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chambless LE, Folsom AR, Sharrett AR, Sorlie P, Couper D, Szklo M, et al. Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. Journal of clinical epidemiology. 2003;56(9):880–90. doi: 10.1016/s0895-4356(03)00055-6. [DOI] [PubMed] [Google Scholar]
- 13.Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–95. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pencina MJ, D’Agostino RB, Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the framingham heart study. Circulation. 2009;119(24):3078–84. doi: 10.1161/CIRCULATIONAHA.108.816694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, Van Horn L, et al. Obesity reduction black intervention trial (ORBIT): six-month results. Obesity (Silver Spring) 2009;17(1):100–6. doi: 10.1038/oby.2008.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morrison JA, Payne G, Barton BA, Khoury PR, Crawford P. Mother-daughter correlations of obesity and cardiovascular disease risk factors in black and white households: the NHLBI Growth and Health Study. American journal of public health. 1994;84(11):1761–7. doi: 10.2105/ajph.84.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. Journal of clinical epidemiology. 1988;41(11):1105–16. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 18.Wagenknecht LE, Cutter GR, Haley NJ, Sidney S, Manolio TA, Hughes GH, et al. Racial differences in serum cotinine levels among smokers in the Coronary Artery Risk Development in (Young) Adults study. American journal of public health. 1990;80(9):1053–6. doi: 10.2105/ajph.80.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donahue RP, Jacobs DR, Jr, Sidney S, Wagenknecht LE, Albers JJ, Hulley SB. Distribution of lipoproteins and apolipoproteins in young adults The CARDIA Study. Arteriosclerosis. 1989;9(5):656–64. doi: 10.1161/01.atv.9.5.656. [DOI] [PubMed] [Google Scholar]
- 20.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 21.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2. Hoboken, N.J: Wiley-Interscience; 2011. [Google Scholar]
- 22.Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. Journal of the American College of Surgeons. 2008;207(6):928–34. doi: 10.1016/j.jamcollsurg.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 23.Bloomgarden ZT. Obesity, hypertension, and insulin resistance. Diabetes care. 2002;25(11):2088–97. doi: 10.2337/diacare.25.11.2088. [DOI] [PubMed] [Google Scholar]
- 24.Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. Journal of the American College of Cardiology. 2009;53(21):1925–32. doi: 10.1016/j.jacc.2008.12.068. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman JS, Dolman L, Rushani D, Cooper RS. The contribution of genomic research to explaining racial disparities in cardiovascular disease: a systematic review. American journal of epidemiology. 2015;181(7):464–72. doi: 10.1093/aje/kwu319. [DOI] [PubMed] [Google Scholar]
- 26.Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. Medical care research and review : MCRR. 2007;64(5 Suppl):29S–100S. doi: 10.1177/1077558707305416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baruth M, Wilcox S, Egan BM, Dowda M, Laken M, Warren TY. Cardiovascular disease risk factor clustering among African American adults. Ethnicity & disease. 2011;21(2):129–34. [PMC free article] [PubMed] [Google Scholar]
- 28.Norman JE, Bild D, Lewis CE, Liu K, West DS, Study C. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA study. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2003;27(3):369–76. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- 29.Morris A, Ferdinand KC. Hyperlipidemia in racial/ethnic minorities: differences in lipid profiles and the impact of statin therapy. Clinical Lipidology. 2009;4(6):741–54. [Google Scholar]
- 30.Wong ND, Lopez V, Tang S, Williams GR. Prevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United States. The American journal of cardiology. 2006;98(2):204–8. doi: 10.1016/j.amjcard.2006.01.079. [DOI] [PubMed] [Google Scholar]
- 31.Flack JM, Victor R, Watson K, Ferdinand KC, Saunders E, Tarasenko L, et al. Improved attainment of blood pressure and cholesterol goals using single-pill amlodipine/atorvastatin in African Americans: the CAPABLE trial. Mayo Clin Proc. 2008;83(1):35–45. doi: 10.4065/83.1.35. [DOI] [PubMed] [Google Scholar]
- 32.Cheng S, Claggett B, Correia AW, Shah AM, Gupta DK, Skali H, et al. Temporal trends in the population attributable risk for cardiovascular disease: the Atherosclerosis Risk in Communities Study. Circulation. 2014;130(10):820–8. doi: 10.1161/CIRCULATIONAHA.113.008506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnston DW, Lee WS. Explaining the female black-white obesity gap: a decomposition analysis of proximal causes. Demography. 2011;48(4):1429–50. doi: 10.1007/s13524-011-0064-x. [DOI] [PubMed] [Google Scholar]
- 34.DeLany JP, Jakicic JM, Lowery JB, Hames KC, Kelley DE, Goodpaster BH. African American women exhibit similar adherence to intervention but lose less weight due to lower energy requirements. Int J Obes (Lond) 2014;38(9):1147–52. doi: 10.1038/ijo.2013.240. [DOI] [PubMed] [Google Scholar]
- 35.Tussing-Humphreys LM, Fitzgibbon ML, Kong A, Odoms-Young A. Weight loss maintenance in African American women: a systematic review of the behavioral lifestyle intervention literature. Journal of obesity. 2013;2013:437369. doi: 10.1155/2013/437369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burke GL, Bertoni AG, Shea S, Tracy R, Watson KE, Blumenthal RS, et al. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Archives of internal medicine. 2008;168(9):928–35. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, Blumenthal RS, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Annals of internal medicine. 2015;162(4):266–75. doi: 10.7326/M14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762–5. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 39.Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA : the journal of the American Medical Association. 2014;311(14):1416–23. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 40.Muntner P, Colantonio LD, Cushman M, Goff DC, Jr, Howard G, Howard VJ, et al. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA : the journal of the American Medical Association. 2014;311(14):1406–15. doi: 10.1001/jama.2014.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]