Abstract
Standardization of Inflammatory Bowel Disease (IBD) care through participation in the ImproveCareNow (ICN) Network has improved outcomes for pediatric patients with IBD, but under the current care model, our improvements have plateaued. Current ICN model care guidelines recommend health supervision visits every six months. We identified a gap in our practice's ability to ensure either a routine six month follow-up or a rapid follow-up after a disease flare, and a significant number of patients with active disease status during a six month period lacked timely reassessment after interventions or medication changes. Telemedicine provides an alternative method of care delivery to address these gaps, but has had limited use in patients with IBD.
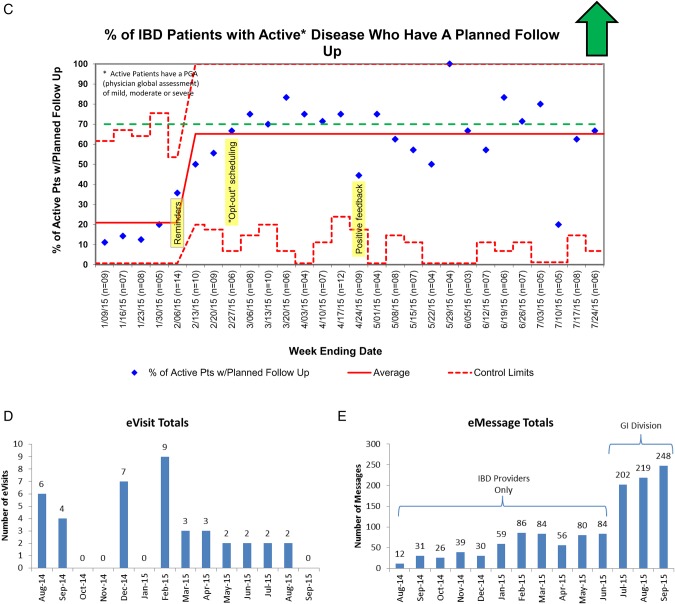
A multi-step approach to offer alternative follow-up care options via telemedicine was developed with potential impact on remission rates and quality of life. Short term goals of the pilot were to improve telemedicine access for patients with IBD were to 1) increase the percent of patients with active disease with a follow-up completed within two months of a visit from 40% to 70%, 2) increase the percent of patients with a visit scheduled within two months of their last sick visit from 20% to 70% (interim measure), 3) increase the number of eVisits from zero visits per month to two visits per month during pilot phase, 4) increase electronic communication with patients from zero messages per month to 200 messages per month, 5) no change in complications or adverse events (defined as an unplanned visit or ED (emergency department) encounter within 30 days of an eVisit. The expected outcomes of the e-visit model were to: maintain baseline care standards and health screening capabilities, improve access to care, and provide equivalent care delivery (no increase in the number of unplanned clinical encounters).
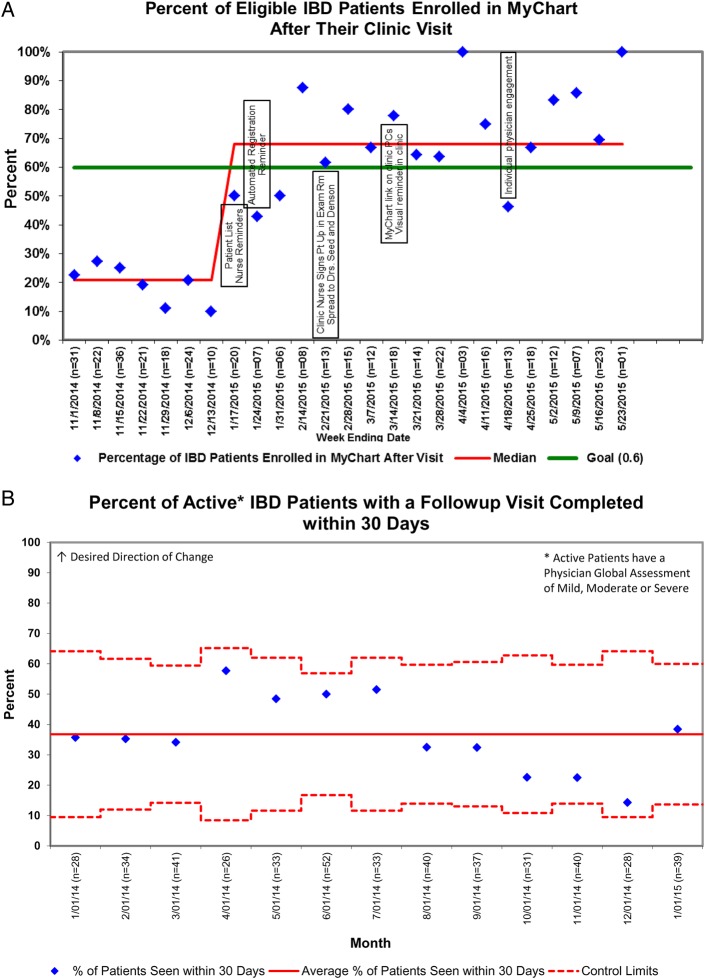
Using the IHI model for improvement (Plan-Do-Study-Act) we have seen a progressive increase in the rate of patient signups for the electronic medical record patient portal, with a baseline median of 20% per clinic compared with a current median of approximately 70% after six months. We successfully implemented e-messaging in its pilot form among five providers and have seen steady uptake in patient use from 5 patient initiated messages during the first month to 76 messages/month over the past three months. E-visits have replaced a total of 32 visits to date. Medications, nutrition, and disease activity were appropriately screened and managed electronically without the need for a physical office visit by the treating gastroenterologist. Access to care was improved in that all patients completed their e-visits from their homes without missing school or work and did not require a physical office visit. One visit successfully identified worsening of the patient's clinical course and resulted in a scheduled office visit request, but no unplanned office visits or ED visits have occurred.
This report represents the first description of telemedicine use in routine clinical care in children with IBD. We anticipate continuing use of this novel mode of health care delivery in pediatrics in an effort to increase the proportion of patients seen for interval follow-up, after IBD diagnosis, or mild flare in an effort to target early treatment changes that should result in improved remission and patient reported outcomes. E-visits are less expensive and time consuming than traditional visits and may serve as an additional method of cost savings by matching care to a patient's individual needs.
Problem
Standardization of Inflammatory Bowel Disease (IBD) care through participation in a large multi-center improvement collaborative called ImproveCareNow (ICN) has resulted in improvement in outcomes for pediatric patients with IBD in the United States and Great Britain, but under the current care model, our improvements have plateaued. Response to medications for IBD varies but may be improved by targeted dose adjustments or addition of secondary medications if done in a systematic way using therapeutic drug monitoring.1 2 Current ICN model care guidelines do not specify the ideal timing of visits after illness when dose and treatments might be changed, but recommend health supervision visits every six months for well patients. In our IBD program at Cincinnati Children's Hospital Medical Center, a large quaternary care facility with about 700 IBD patients, we identified a wide range of practice patterns after illness, which hampered our ability to make targeted treatment changes for at-risk patients via timely reassessment.
Background
Inflammatory Bowel Diseases (IBD), such as ulcerative colitis (UC) and Crohn Disease (CD), are chronic gastrointestinal diseases. Up to 25% of cases begin during childhood, and are associated with a variety of psychosocial and medical complications related to progressive disease.3 The goal of therapy is to decrease inflammation in the gastrointestinal tract in order to reduce flares and induce “remission,” or a state of quiet or inactive disease. Patients with a recent flare and active disease (i.e., not in remission) have not achieved healing of the intestinal mucosa, which remains the ultimate non-clinical goal of therapy, and may be at risk for another flare.4 While patients with active disease may benefit from medication adjustments, particularly if not working well, in the current practice model, there is no standard way to know when patients should be reassessed after flares, while transferring the responsibility of contacting the medical team onto the patients.
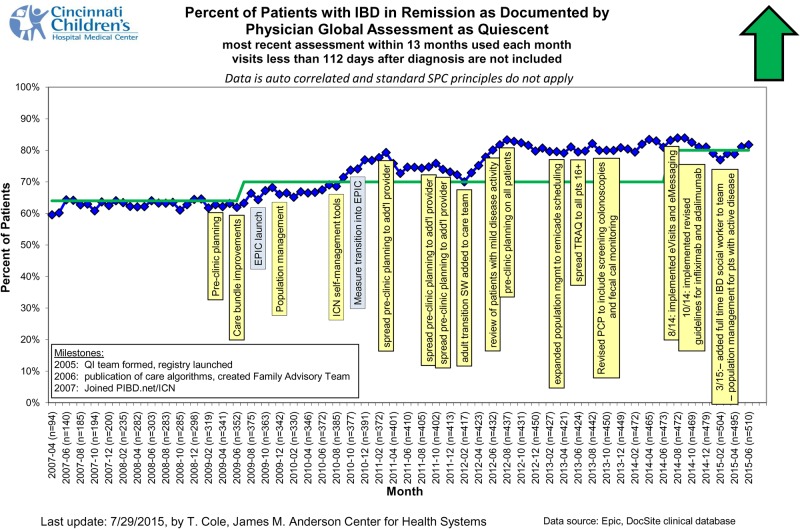
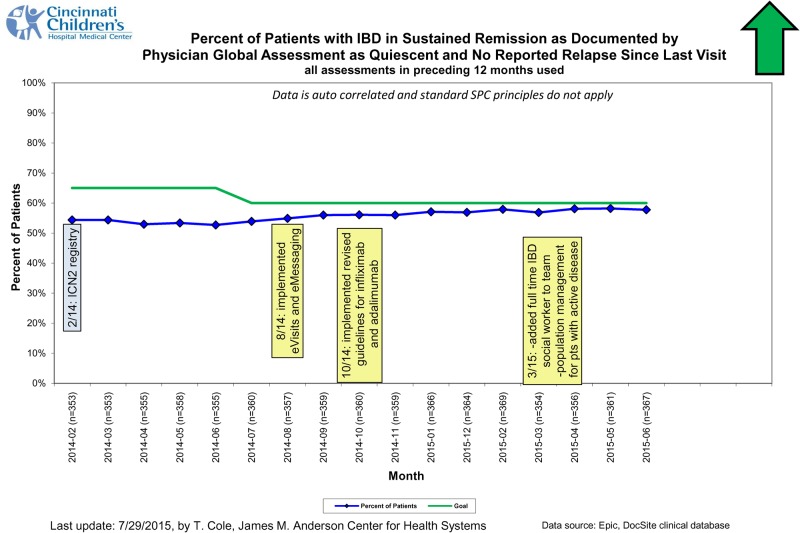
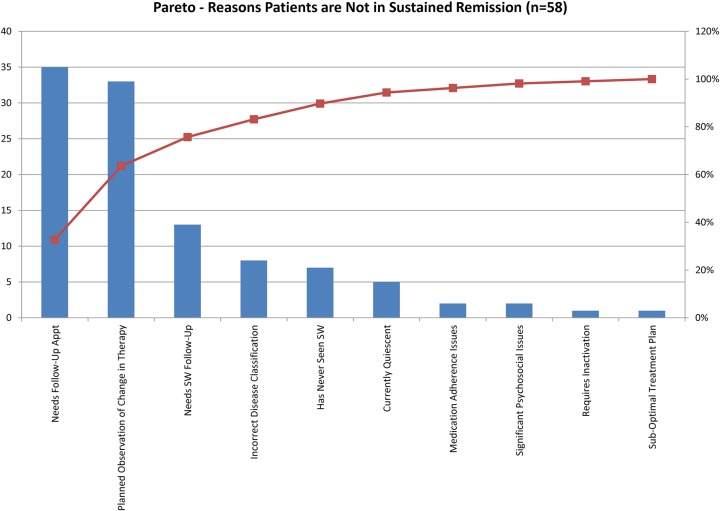
After instituting a formal quality improvement system for our IBD patients (including pre-visit planning and developing standard care guidelines), remission rate (remission defined as no active signs of disease or “quiescent disease” at a clinical encounter) improved from approximately 60% to now around 80% and has remained stable over the past several years (Figure 1). Sustained remission (absence of active disease at the most recent clinic visit or at any other point in time over the past year) has also remained stable at about 50% (Figure 2). In order to improve remission rates by an additional 10% in our current population of about 500 pediatric patients, 20 more patients need to achieve remission per year. We reviewed patients who were recently classified as having “active disease” (a categorization defined by “Physician Global Assessment” or “PGA” as per ICN Model Care Guidelines) to assess the reasons for not being in remission after six months. Of 58 patients with active disease, a Pareto analysis (Figure 3) revealed lack of follow-up (27%), or having a planned observation of therapy with no documentation that it worked or failed (14%). Only a very small number of patients were rated as still actively ill because of medication nonadherence (1%). At our last measurement prior to making changes to our current system, there were 80 patients who were actively ill at their last visit, but 78% had not been seen for over two months. Of these, at least 30% had actually not been seen in more than six months. Even well patients did not consistently have the recommended six month follow-up visit, with up to 80 patients per year being over-due for a visit. Analysis of this gap in follow-up served as the basis to try to improve our current model of care delivery to better meet the needs of our patients by expanding our care delivery system to allow standardized follow-up care as well as alternative communication and care delivery models using telemedicine, specifically eVisits and electronic messaging.
Figure 1.
Figure 2.
Figure 3.
Office visits to reassess symptoms may be time consuming or inconvenient, telephone calls may be difficult to coordinate, and the current model of care in our clinic tends toward episodic, intermittent care as opposed to patient-centered, collaborative, continuous assessment of symptoms. Assuring complete care according to IOM guidelines in the book “Crossing the Quality Chasm”, in which patient and physician communication and collaboration is optimized, has proven difficult to achieve in the current care delivery system. In adult IBD, a Swedish group has shown improved outcomes by creating a more coordinated care system with “virtual” phone visits.5 The use of telemedicine has been well received in studies of small numbers of patients with IBD and identified as an important component of future improvement efforts, but has not yet been implemented as a routine part of clinical care for pediatric IBD patients.6 7 Telemedicine, and in particular e-Visits (a clinical visit performed via a computerized interface) and e-Messaging, could serve as a way to improve communication and timely follow-up, improve outcomes related to remission and quality of life, and decrease financial and time costs associated with office visits, flares of disease, and time away from activities.6
Baseline measurement
Our “SMART” (specific, measurable, achievable, realistic, timely) aim was that by May, 2015 we would 1) increase the percent of patients with active disease with a follow-up completed within two months of a visit from 40% to 70%, 2) increase the percent of patients with a visit scheduled within two months of their last sick visit from 20% to 70% (interim measure), 3) increase the number of eVisits from zero visits per month to two visits per month during pilot phase, 4) increase electronic communication with patients from zero messages per month to 200 messages per month, 5) no change in complications or adverse events (defined as an unplanned visit or ED (emergency department) encounter within 30 days of an eVisit.
Longer term outcome measures and aims include:
Remission: aim to maintain or increase remission rate (currently at about 80%). Remission is measured monthly (since 2007) based on each patient's last physician assessment of disease activity.
Maintain or increase quality of life and confidence in managing disease. Current measures include “PedsQL” (a validated pediatric quality of life instrument instituted for our center in 2013 for all IBD patients), and the TRAQ (a validated self-management questionnaire) which is being implemented for our IBD patients over the past three years.
Value measure: Measure to be determined, but will include an aim to improve patient outcomes mentioned above while decreasing costs (time associated with being sick, time lost due to illness, medical expenses, work/school days missed).
Design
Prior to making changes to the current system, we identified drivers that would optimize our system's ability to achieve the goals of the chronic care model. These drivers included: appropriate technology, patient access to e-Messaging and eVisits, correct identification of patients, appropriate communication regarding eligibility and cost of eVisits, ability to maintain standard of care, and provide patient centered care. The main interventions included a visit protocol for eVisits, guideline for visit timing after flare, and development of e-Messaging and eVisit technologies. Many of these changes were grouped changes and necessary for the redesign of our current practice. Prior to beginning other work, technology and protocol development for eVisits were developed to ensure appropriate functioning within the electronic medical record. Ongoing work to enable patients access to their electronic medical record has been undertaken (this is a necessary step to use other electronic resources) and accounted for about six months of work.
The backbone of the eVisit process is founded in development of a follow-up protocol to account for the deficiencies we observed in clinical practice for the actively ill patients who were not being seen for many months after illness. Changes included clinician and patient education regarding the need for more frequent interaction, notification of team members about patients needing a follow-up visit incorporated the inclusion of an external scheduler to facilitate scheduling patients for follow-up visits, and positive reinforcement for physician-nurse teams who scheduled appropriate follow-up. These changes were developed over a series of six months and are now sustainable.
Strategy
Several PDSA (Plan,Do,Study,Act) cycles were carried out at several critical steps to ensure successful achievement of our SMART aims. These included:
“MyChart” electronic medical record registration:
Access to MyChart was necessary for both messaging and eVisit platforms and included access to customized disease specific information. Registration for MyChart is a two-step process where a patient and family get an activation code at registration and then complete registration on a separate computer. First PDSAs to increase MyChart activation were ineffective because they focused on education and notification to teams regarding who needed to be enrolled in MyChart at each visit. These PDSAs helped with conversations surrounding registration and increased awareness, but did not significantly increase percentage of patients enrolled. The most effective PDSAs resulted from process changes that were automated at key steps of the process (prompts to ask the patient to register for MyChart when they arrived to clinic, having the link to complete registration on the computer in the exam room, and having clinic nurses include MyChart activation into the normal clinic triage and discharge education process).
Follow-up visits:
After consensus was obtained within our group regarding timing of follow-up visits after flare since no published guidelines exist, the first PDSA cycles were centered on education about the new guidelines to physicians and nurses. Teams seemed on board with the work, but the percent of visits scheduled did not change (as their work-flow had not changed). Subsequent PDSAs focused on increasing physicians awareness of patients who needed follow-ups with an “opt-in” to have a scheduler make the patient's appointment (which helped very little), and then shifted to an “opt-out” where the visits were arranged through a scheduler unless the team declined (which made a substantial improvement). We also performed PDSAs surrounding positive reinforcement given as weekly written commendation for teams complying with the follow-up visit protocol without the need for intervention.
eVisits:
First PDSA was aimed at the clinic “ask” of the patient to complete an eVisit for their next follow-up. The provider was asked to prompt patients regarding their interest in an eVisit during their clinical encounter. This was not effective as it lacked an automated process to prompt providers to discuss timing and type (eVisit or traditional visit) of follow-up at the time of clinical encounter. For the second PDSA cycle, if a visit had not been scheduled after a recent sick visit, a reminder about eVisit options was included in the after-visit notification being sent as part of the follow-up visit PDSAs. If eligible per the eVisit protocol, the provider could ask that a patient be offered an eVisit. This was effective, and did result in some eVisits being offered, but was cumbersome to complete since the initial opportunity to discuss eVisit with the patient and provider was missed in clinic.
Patient eVisit reminders:
Separate from the “ask” of patients to complete eVisits was the actual work of getting eVisits completed. After a few eVisits were offered, we learned that patients needed reminders to complete eVisits on time. The first PDSA was to remind patients by eMessage to complete the visit. This was cumbersome and not effective because as the list of patients to complete eVisits grew, tracking of patient status became difficult. The second PDSA was to create automated reminders or “flags” through the medical record that could serve two purposes: 1) to let the patients know when their visit was due and 2) to create a searchable list of patients with upcoming visits due. So far these flags are easy to enter and search. Next PDSAs will surround creating patient lists to know who needs special reminders to complete their visit. (see supplementary file “Notable PDSAs executed for enrollment in “MyChart”, follow-up visit protocol, and eVisit use”)
Results
Measurements of our progress toward our “SMART” aims are seen in Figure 4 and have all demonstrated improvement. The MyChart, follow-up, and eMessaging processes are relatively stable and reproducible processes with the entire division currently involved, but the eVisit process is likely to experience the largest degree of change going forward, since currently only a few providers have been involved with the pilot. As we are able to transition the eVisits into the larger process of patient follow-up, we hope that we will be able to simplify workflow by offering eVisits and traditional follow-up visits in a seamless and automated way to a greater number of patients. We have seen good improvement in the MyChart enrollment process, which was not specifically a SMART aim, but was a necessary interim improvement project to achieve prior to beginning other telemedicine avenues (Figure 4a). Looking specifically at our “SMART” aims, we have not yet recorded the percent of patients with completed 2 month visits (smart aim 1, Figure 4b) which has served as background data, but have met our smart aim 2 goal which was the interim measure of improving scheduled follow-ups from 20% to 70% (Figure 4c). Aim 3 centered around increasing eVisits from zero visits to two visits per month (on average) and has been achieved though still with some variation month to month (Figure 4d). Aim 4 has been far surpassed with a goal of 200 messages sent per month, and now with a steady increase upwards of 200 messages each month (Figure 4e). Aim 5 was meant as a balancing measure, and we have not seen any unplanned visits or ED visits as a result of an eVisit missing a change in clinical condition, though one eVisit did identify a clinical worsening which was not communicated outside of the eVisit and resulted in a planned office visit.
Figure 4.
Patient experience was evaluated informally through our parent IBD advisory group for the messaging and follow-up programs and have been reviewed favorably. Specifically they have reported that they appreciate having closer contact with the medical teams and feel that their care has improved. The eVisit component of the work was evaluated via anonymous surveys. To date only five patients have completed these surveys. Of these, four of the five reported that they felt comfortable with the visits and the level of care provided, appreciated being able to avoid an office visit, and would choose eVisit again if it were available. The one patient who did not feel satisfied with the visit did not comment on what they did not like about the visit or how they would improve it.
Our main longer term outcome measure is remission and sustained remission (Figures 1 and 2). Both have achieved some improvement and are showing a trend upward in the last months since introducing the follow-up and eVisit processes as well as new drug monitoring guidelines.
Lessons and limitations
One of the major limitations encountered in the system surrounded lack of automated processes. Successful PDSAs reduced cumbersome extra steps, eliminated the need for providers or patients to remember things on their own, and allowed for automated process completion rather than manual work. There are still a number of steps that are not automated (initial code generation for access to the electronic medical record, follow-up visits scheduled at time of clinic visit, patients offered eVisit at time of clinic visit) that will continue to be part of future work. A second limitation has been building the new technology into the current workflow at our center in terms of understanding, availability, and patient acceptance. Now that tracking of patients between visits is able to be automated, we are hopeful that this option for follow-up will be easier to spread as an option for more patients.
Other lessons surround culture change. As with any project, there were those who were early adopters and were eager to respond to new processes or who participated because they truly valued the shared purpose of improved patient outcomes. Others were more difficult because of ingrained habits, skepticism that a new way was better, or because they did not believe that this would improve outcomes. Some simply felt that the workflow changes were too cumbersome and chose not to participate. Going forward, as these technologies and processes spread, we will continue to try to focus on the late adopters to help make these changes meaningful for them and their patients.
With any improvement initiative, sustainability should be a priority in order to guarantee long-term success. In its current form, the work of this project is sustainable but our next phase of improvements will focus on automation, time-effectiveness, and incorporation of these efforts into “care algorithms” in order to assure a seamless process that does not depend on an individual or group of individuals to do the work. These results should be applicable to other groups looking to streamline processes for follow-up and inter-visit care for complex, chronic medical conditions as the ultimate goal of the work was done to coincide with the Wagner Chronic Care Model.
Conclusion
The gap we intended to address with this work centered on a lack of an efficient way to communicate with patients and to reassess them on a timely, standardized basis after flares. While the use of telehealth for inter-visit follow-up for IBD is not widely described outside of a research setting in the literature, the model described here is closely aligned with the Wagner Chronic Care Model. Other groups who have used care redesign (as part of Accountable Care Organizations (ACOs) for example) to provide novel approaches to health care delivery aimed at improving inter-visit care, using information systems to improve communication, and utilizing a team approach to health care keeping high-risk patients in their homes have demonstrated significant improvement in outcomes and costs leading to improvement in value for the patients.8 The interventions we implemented have allowed us a variety of ways to communicate with and reassess patients virtually or in person. We have been able to begin to customize the patient experience, allow more continuous communication, and provide demand-directed care. While some of the interventions (particularly eVisits) are in the pilot stage, we feel confident that the new model of care, will be able to be scaled up to the rest of our practice, with the ultimate goal of improving patient outcomes, such as remission and sustained remission, while decreasing costs associated with illness.
Footnotes
Declaration of interests: Nothing to declare
Ethical approval: This project was designed as an extension of clinical care, with the goal of improving our ability to provide standard care for all patients. In this setting we sought to improve care delivery and access. The project was discussed with the head of the hospital IRB, who felt that since the intent of the work was improvement of routine care delivery, that it was not considered human subjects research and was exempt from ethical approval.
References
- 1.Dubinsky MC, Reyes E, Ofman J, Chiou CF, Wade S, Sandborn WJ. A cost-effectiveness analysis of alternative disease management strategies in patients with Crohn's disease treated with azathioprine or 6-mercaptopurine. Am J Gastroenterol. 2005;100:2239–47. [DOI] [PubMed] [Google Scholar]
- 2.Joosse ME, Samsom JN, van der Woude CJ, Escher JC, van Gelder T. The Role of Therapeutic Drug Monitoring of Anti-Tumor Necrosis Factor Alpha Agents in Children and Adolescents with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:2214–21. [DOI] [PubMed] [Google Scholar]
- 3.Baldassano RN, Piccoli DA. Inflammatory bowel disease in pediatric and adolescent patients. Gastroenterol Clin North Am. 1999;28:445–58. [DOI] [PubMed] [Google Scholar]
- 4.Pineton de Chambrun G, Peyrin-Biroulet L, Lemann M, Colombel JF. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010;7:15–29. [DOI] [PubMed] [Google Scholar]
- 5.Rejler M, Spangeus A, Tholstrup J, Andersson-Gare B. Improved population-based care: Implementing patient-and demand-directed care for inflammatory bowel disease and evaluating the redesign with a population-based registry. Qual Manag Health Care. 2007;16:38–50. [DOI] [PubMed] [Google Scholar]
- 6.Aguas Peris M, Del Hoyo J, Bebia P, Faubel R, Barrios A, Bastida G et al. . Telemedicine in inflammatory bowel disease: opportunities and approaches. Inflamm Bowel Dis. 2015;21:392–9. [DOI] [PubMed] [Google Scholar]
- 7.Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010;16:125–33. [DOI] [PubMed] [Google Scholar]
- 8.Davis K, Buttorff C, Leff B, Samus QM, Szanton S, Wolff JL et al. . Innovative care models for high-cost Medicare beneficiaries: delivery system and payment reform to accelerate adoption. Am J Manag Care. 2015;21:e349–56. [PubMed] [Google Scholar]