Abstract
Inpatient falls (IF) are the most commonly reported safety incidents. The high rate of inpatient falls was reported in a newly built hospital, within Aneurin Bevan University Health Board, Wales (UK). The aim of the project is to reduce the incidence of IF and associated adverse clinical outcomes in a hospital with 100% single rooms.
The key mechanism for improvement was education and training of nursing staff around falls risk factors. A Plan-Do-Study-Act methodology was used and a geriatrician-led, systematic nurse training programme on the understanding and correct use of existing multifactorial falls risk assessment (FRA) tool was implemented in April 2013.
Pre-training baseline data revealed inadequate falls assessment and low completion rates of the FRA tool. Subsequent, post-training data showed improvement in compliance with all aspects of FRA. Concurrent with nurse training, the actual falls incidence/1000 patient-bed-days fell significantly from the baseline of 18.19±3.46 (Nov 2011-March 2013) to 13.36±2.89 (p<0.001) over next 12 months (April 2013-March 2014) and remained low (mean falls 12.81±2.85) until November 2015. Improved clinical outcomes have been observed in terms of a reduction of length of stay and new care home placements, making total annualised savings of £642,055.
Problem
Ysbyty Ystrad Fawr (YYF) is the newly built, local general hospital providing 100% single rooms with an ensuite facility within Aneurin Bevan University Health Board (Wales, UK). The hospital replaced two previous hospital sites which were mostly comprised of multi-bedded wards (MB-W) in November 2011. The new hospital (YYF) has a medical assessment unit, an acute medical ward, one general medical ward and three care of the elderly (CoTE) wards in addition to an adult and old age Psychiatry, adult Psychiatry, and elective surgical unit.
The quality and patient safety team noticed increased incidents of inpatient falls (IF) in the new hospital and the report was shared with medical and nursing teams. The immediate response was to analyse the IF data for five general medical and CoTE wards with a total of 144 beds providing acute/general medical care and/or geriatric rehabilitation. Most patients admitted to these five wards were older adults (mean age = 72 years). The mean incidence of IF in the new hospital over a period of 12 months was 16.79/1000 patient-bed-days.
This IF incidence in the new hospital was high when compared to the two previous multi-bedded hospitals where falls rate was 6.75/1000 patient-bed-days.1 A similar falls rate (6.7 falls/1000 patient-days) has been reported from a 300 traditional multi-bedded hospital providing both acute medical care and geriatric rehabilitation.2
Both the previous and new hospital sites continued to admit acute and sub-acute patients. There was no change in demographics, size, and characteristics of the population except the change in the geography of the new hospital. The new hospital has 144 medical beds and all are single rooms as compared to the previous two hospitals which had 124 medical beds and only 10 were single rooms.
Therefore, the new hospital with 100% single rooms provided enhanced dignified and personalised care but this was at the expense of an IF rate almost 2.5 times higher as compared to the two previous hospitals.
This was clearly a quality and patient safety issue in the new hospital and action in terms of a hospital falls prevention program was urgently needed to prevent harm. Current evidence does not support the use of the fall risk prediction tools in the hospital setting,3 therefore, a team comprised of a consultant geriatrician, ward sister, nurses, and managers were established to explore alternate options to reduce the incident of IF.
The initiative used were quality improvement methods to test, implement, and measure the impact of systematic nurse training on falls risk assessment (FRA). The FRA is a nursing tool to assess and mitigate the multiple factors that pose a risk of IF in the hospital setting. The FRA is part of the Health Board Falls Policy and all inpatients above the age of 65 should have falls risk assessment completed on admission.
The primary aim of this quality initiative was to reduce the incidence of falls by 25% in the next 12 months. The secondary aim was to reduce any associated adverse outcomes related to falls in the new hospital with 100% single rooms.
Background
Worldwide populations are ageing.4 The prevalence of falls increases with age, from 35% in older adults (>65 years) to 45% in adults over the age of 80.5–6 Older patients admitted to hospital are at greater risk of falling.7 IF are a major concern for patient safety and a marker of care quality and account for almost two-fifths of the patient safety incidents reported to the National Reporting and Learning System.8
In literature, the falls rate among hospitalised older adults has varied from 2% in an acute setting9 to 12.5% in a rehabilitation setting.10 Overall, the intensity of falls/1000 patient-bed-days can vary depending on the ward type and hospital population11 and it has been reported as 2.2 in acute setting,12 9.2 at the geriatric rehabilitation wards,13 and 17.1 in the psychogeriatric ward setting.13
Falls among those in the hospital also tend to result in more serious complications; with 10 - 25% of such falls resulting in fracture or laceration.14 Inpatient hip fractures have higher mortality when compared to those from the community.15 After adjustment for age and gender, the odds of inpatient mortality was 2.25 times higher for inpatient hip fracture and the odds ratio was raised for both 90-day and one-year mortality.15 IF in single rooms has been associated with a significantly higher incidence of hip fracture in a hospital design with single rooms as compared with a multi-bedded facility.16 In multivariate analyses, IF had been independently correlated with significantly higher length of stay (LoS) and substantially increased utilization of resources following injurious falls.17 The extra cost of caring to NHS for patients who have suffered a fall amounts to an estimated £2.3 billion/year.18 Falls also result in pain, distress, loss of independence and confidence, in addition to affecting the patient's family and carers.
Over the last decade, there has been a trend of constructing single rooms in many parts of the world to deliver a high level of patient care whilst minimizing hospital-acquired infections.19–20 The proportion of single-occupancy rooms in NHS hospitals is rising and new hospital design includes greater ratios of single-bedded accommodation, in some cases 100% single rooms.21 However, adverse outcomes of single rooms including reduced social interaction, less surveillance by the staff, and increased IF have been reported.1 11 22
Multi-bedded wards (MB-W) are often in the line of vision of the staff and there is added benefit of increased surveillance by other patients or relatives, thus preventing IF. In comparison, the observed significant increase of IF rate in single rooms could be due to several factors: room size, easy access to ensuite toilet facility, patients being less visible from nursing stations, delay in responding to call bell due to increased walking distance in corridor, or inability to safeguard patients who fall due to hospital design.16
Currently, nurses are caring for more adults over 65 than any other patient population and hospital admission is associated with increased risk of falls.1 In order to provide safe, affordable, and patient-centred care, nursing education needs to be enhanced fundamentally.23 Nursing education is available in most health care settings, but it can be difficult to participate in such training events due to time and service constraints. The inability to keep up to date with training and development not only results in high-stress levels but also compromised patient care.24–25 Nurse education has also been shown to reduce work-related stress.26
Falls could be prevented by 18-31% through multifactorial assessments and interventions.27 A Cochrane review (2010) on interventions for preventing falls in older people, suggested that multifactorial interventions resulted in a statistically significant reduction in the rate of falls and risk of falling in the hospitals.28 Recent studies on falls prevention initiatives in acute care/tertiary hospitals have shown effectiveness in reducing falls and fall-related injury rates significantly.29–30 However, there is a dearth of studies exploring falls reduction in the single room setting.
Baseline measurement
The main outcome measures employed in this project included the incidence of falls expressed as a rate per 1000 patient-bed-days. Data around the incidence of falls was gathered using standard hospital data for critical incidents where IF is recorded on Datix. Datix is web-based patient safety software for healthcare risk management which provides a comprehensive oversight of risk management activities and includes incidents of IF or adverse events.
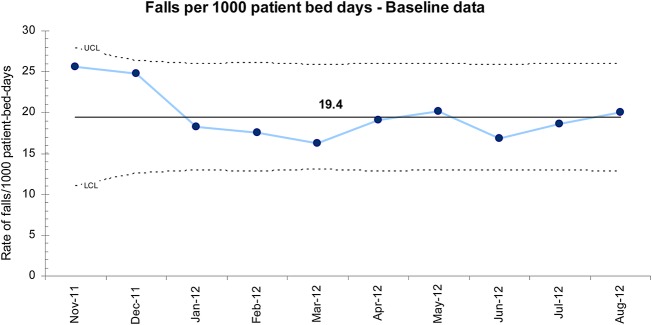
The U-control chart (figure 1) shows the falls incidence per 1000 patient bed days immediately after the new hospital was opened in November 2011. This demonstrates a stable but high rate of IF of 19.4/1000 patient-bed-days over 10 months. This was higher than a very similar elderly care unit in the UK comprised of eight single rooms and four four-bedded wards (13.3/1000 patient-bed-days).11 The falls rate observed in the new hospital was even higher than a psychogeriatric ward (17.1/1000 patient-bed-days).13
Figure 1.
Baseline statistical process U-control chart displaying incidents of inpatient falls over 10 months.
Design
The team including a ward manager, two registered nurses, a healthcare support worker, geriatric medicine registrar, senior nurse, hospital manager, and consultant geriatrician met to discuss the root cause for the high incidence of IF in the new hospital with 100% single rooms. The new hospital and two previous hospitals provided care to the same geographic and demographic population. The permanent nursing and medical firms from the two previous hospitals were transferred to the new hospital site, and new nursing staff and healthcare assistants were recruited to provide similar 1:7 nurse/patient ratio.
The team undertaking the quality improvement project also acknowledge the fact that single rooms have been associated with higher falls risk based on the incident reporting but no clear mechanism for single rooms causing falls has either been reported or researched.
Further brainstorming using fish bone analysis highlighted issues with lack of nurses' awareness of falls, insufficient falls training, and knowledge; poor compliance with completion of the multifactorial FRA; lack of engagement with therapists; increased work related pressure with single rooms.
The team agreed to implement an intervention to raise the nurses falls awareness by introducing opportunistic informal falls teaching on completing the multi-factorial FRA tool. The decision of the team to raise nurse awareness through training was justified on the basis of health board guidance recommending reliable completion of the FRA tool, availability of resources, time constraints, and no extra cost was involved.
The statistical process control (SPC), also known as control chart was used to plot the data in time order to demonstrate the evidence of improvement. An SPC chart has a central line for the mean values, an upper line for the upper control limit (UCL) and a lower line for the lower control limit (LCL).
Strategy
The project team used Plan-Do-Study-Act (PDSA) cycles to test the effects of the interventions employed. The initial PDSA cycles tested opportunistic informal falls awareness in one ward. The initial structure for repetitive testing of change was ‘a reminder to complete FRA during weekly multidisciplinary meeting’. This was studied by four weeks and team agreed to implement a reminder on daily ward manager led ‘patient status at a glance board rounds’. This was implemented on a small-scale to test in the same ward but no change in reduction of incidents of IF was noted. The team tested to include ‘a prompt for completion of the FRA during nurse's handover’ in the morning and evening. The results showed inconsistency among nursing staff and the team agreed to introduce ‘registrar led weekly teaching’ on falls awareness. The teaching was well received, raised the falls awareness amongst nurses, and some reduction of recurrent falls was observed. However, teaching sessions were missed due to other on-call and training commitments of the registrar. All the PDSA were studied and agreed action was to commence the ‘consultant led weekly teaching’ and invite nursing staff from all the five medical wards to spread and drive the improvement.
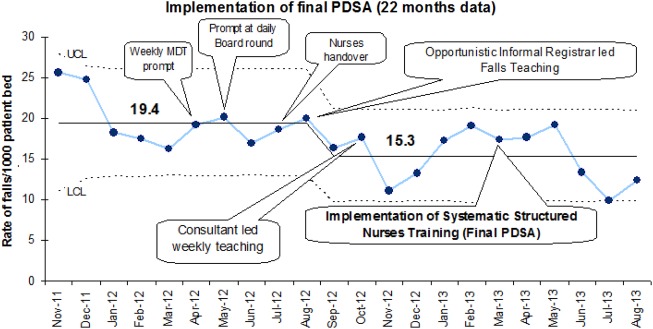
The data was plotted on an annotated U-control chart in order to demonstrate progress over time. Despite observing a slight reduction in the incidence of IF over initial 16 months, it started regressing towards the mean (Figure 2).
Figure 2.
Implementation of final PDSA – Statistical process U-control chart displaying reduced incidents of inpatient falls over 22 months.
Following evaluation of the initial repetitive PDSA cycles and learning achieved through interventional experiments, the team agreed that the intervention has shown some improvement on initial small scale testing but further changes should be made.
The project team met several times to gain an understanding of staff perception, attitude, and factors leading to the high rate of IF in the new hospital. Whilst numerous solutions were explored such as having a day room or modifying the FRA, the prevailing issue agreed was the lack of systematic and structured nurse training around understanding and mitigation of risk factors leading to falls in the hospital setting. The team acknowledged the challenges to deliver training sessions to all grades of nursing staff but this decision was justified based on inadequate audit findings on the compliance with the use of the FRA tool and the fact that nurses are the first point of contact with patients and initiate FRA. These challenges were overcome through team commitment to a shared agenda to prevent falls and improve patient safety.
The new strategy was to introduce ‘formal systematic structured nurses training on falls’ every two weeks from April 2013. A consultant geriatrician with a special interest in falls, senior nurses, and ward managers were consulted to develop the structure of falls training. All nurses on the CoTE and general medical wards were enrolled in the falls training and it was agreed to commence formal teaching in the education centre. Teaching was done based on the national UK guidelines published by NICE around prevention of falls and National Service Framework for older people.
The structured teaching was delivered by a consultant geriatrician (IS) with a special interest in falls or a geriatric medicine trainee (SA, MK, JO) at regular intervals (fortnightly) in small groups. This was done to ensure each staff member attended at least one teaching session.
Each training session lasted 45 minutes and included discussion on the definition of falls, understanding complications of in-patient falls, interactive case-based discussion to underpin falls, risk factors from nurse's experience, and reflective practice. Each session ended with formal teaching on falls risk factors including dementia, delirium, nutrition and continence, and guidance on completion of the formal health board document: A multifactorial FRA tool.
Printed handouts of key learning points were given at the end of the session.
The standard incident data on IF was collated from November 2011 to August 2013. The data did not only show a further reduction of falls incidence but also the special cause variation (one point touching the LCL - July-13) was observed for the first time. (Figure 2)
Following the improvement observed with the final PDSA, the team agreed to continue to deliver the structured training on falls for the next six months and review the incidence of falls. In addition, the team also agreed to review the FRA process by auditing compliance with completion rates of the FRA tool in November 2013 and compare with the previous audit completed in January 2013. The pre-training assessment revealed inadequate assessment and low completion rates of the FRA tool. The post-training assessments showed some improvement in compliance with all aspects of FRA, with particular improvements in cognitive and environment hazard assessment, and osteoporosis risk. (Table 1)
Table 1:
Audit on compliance of the FRA tool
| Risk Assessment Compliance | Pre-training (n=105) (January 2013) |
Post-training 1 (n=107) (November 2013) |
Post-training 2 (n=102) (November 2014) |
|---|---|---|---|
| Falls assessment trigger questions | 69% | 82% | 86% |
| Falls prevention care plan | 47% | 62% | 45% |
| Medication | 52% | 55% | 66% |
| Postural Hypotension | 45% | 53% | 63% |
| Vision | 47% | 51% | 67% |
| Hearing | 50% | 53% | 67% |
| Gait & Balance | 47% | 52% | 69% |
| Continence | 42% | 48% | 66% |
| Environmental Hazard | 39% | 46% | 64% |
| Cognition | 27% | 45% | 57% |
| Osteoporosis | 32% | 27% | 50% |
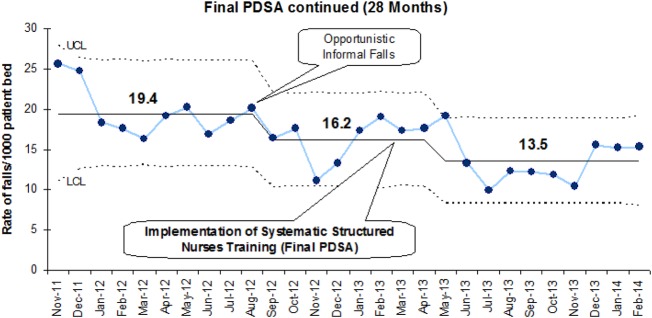
The IF incidence continues to decline with regular systematic structured nurses training on falls. The special cause-effect was observed again as demonstrated by a run of seven points all below the centre line and mean IF rate dropped from 19.4 to 13.5 (30% reduction). (Figure 3)
Figure 3.
Implementation of final PDSA continued – Statistical process U-control chart displaying reduction in incidence of inpatient falls
Based on the findings of the improvement cycles, the team agreed to continue structured nurses training on falls fortnightly for the next 12 months and repeat the audit on the compliance of FRA in November 2014. The rationale of fortnightly teaching was to ensure that each staff member has attended at least one teaching session over 12 months. The team also explored long-term sustainability and the general consensus was to deliver teaching sessions once a month from 2015.
The existing strategy to measure the improvement was the continuous analysis of the incidence of the in-patient falls via falls incidents reported on the in-house Datix system and to regularly audit the process (compliance with the falls assessment tool).
In addition, further data collection was planned by reviewing routine hospital electronic data retrospectively to assess any improvements in clinical outcomes and benefits to the organisation.
The clinical outcomes were analysed retrospectively in terms of any injury, hip fracture, the LoS, and mortality via the Myrddin patient administration system. The data collection on falls-related injury and clinical outcome was completed for three years (November 2011-November, 2014). Regular systematic structured nurse training on falls and on the use of a multifactorial FRA tool was commenced in April 2013 (Final PDSA). Therefore, the whole cohort was divided into two samples to evaluate clinical outcomes: before intervention (November 2011 to March 2013 – 17 months) and after intervention (April 2013 to November 2014 – 20 months). The index admission was defined as any one episode of admission until discharge or death.
Mortality data were also collected on all patients for up to a minimum of six months and a maximum of up to two years following the first incident of IF and also discharge from the hospital. Mortality analyses were done for 30 days following the date of discharge, six months from the first incident of fall in the hospital and also from the date of discharge from the hospital.
The benefits were assessed through bed savings and reduction in the discharge to the new care home placements. The formal complaints received by the health board related to in-patient falls during the study period were also evaluated.
All statistical analyses were conducted using STATISTICA StatSoft data analysis software system, version 9.1 (Statistica Inc., 2010). Data are presented as means ± standard deviation (SD). The difference in scores before and after an intervention was summarised with the independent sample t-test. The level of statistical significance at which the null hypothesis was rejected was chosen as 0.05.
See supplementary file: ds9061.doc – Figure 2 and 3 (Improvement cycles)
Results
Pre-training baseline data revealed inadequate falls assessment and low completion rates of the FRA tool. Subsequent, post-training data showed improvement in compliance with all aspects of FRA, with particular improvements in cognitive and environment hazard assessment, and osteoporosis risk. The results are presented in table 1.
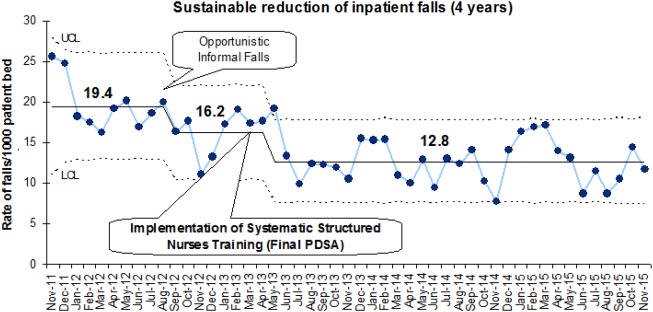
Concurrently with nurses training, actual fall incidence/1000 patient-bed-days fell significantly from the baseline of 18.19±3.46 (Nov 2011 to March 2013) to 13.36±2.89 (p<0.001) over the next 12 months (April 2013 to March 2014). The results were shared with the staff in subsequent training sessions using run charts to share the improvement. The results have been sustained and a shift downwards in the mean incidence of IF has been observed (mean falls 12.81±2.85 over last 32 months from April 2013 to November 2015) as shown in the U-control chart which displays IF in a time sequence. (Figure 4)
Figure 4.
Statistical process U-control chart displaying sustainable reduction of the incidents of inpatient falls in a time sequence over 4 years
A total of 9445 patients (mean age ± SD = 72±17 years; female 58%, the mean LoS ± SD = 17±24 days) were admitted to the hospital during the study period (07 November 2011 to 30 November 2014). The total number of in-patient falls incidents reported during this period was 2349, affecting a total of 11% (1046) patients (82 incidents were excluded due to missing data). 86% (902/1046) patients (mean age 80.82±10.40 years) were admitted from their homes requiring formal or informal care support. Only 5.06% (53/1046) were admitted from care homes or other hospitals and they were comparatively older (mean age 86.42±7.11 years). 53% (554/1046) were females and the mean age of females (82.66±10.38 years) was significantly higher as compared to males (79.56±9.90 years, p<0.001).
The detailed clinical outcomes following an IF before and after intervention are shown in table 2. A significant reduction of 30-day post-discharge and six-months mortality has been observed which could be related to the reduction in LoS or a new care home placement but this needs further evaluation. We have also observed increased incidence of hip fracture following intervention, which is not statistically significant, but warrants sub-analysis.
Table 2:
Clinical outcomes for all the in-patient fallers before and after intervention
| Pre-training 17 months data | Post-training 20 months data | P value | |
|---|---|---|---|
| Demographics | |||
| Age | 82±10 | 81±10 | 0.02 |
| Sex (females, %) | 51.7 | 54.1 | 0.45 |
| Profile of falls | |||
| Falls incidents | 1241 | 1108 | N/A |
| Mean falls/1000 patient-bed-days | 18.19±3.46 | 12.66±2.84 | <0.01 |
| Number of patients affected % (n) | 46.9 (491/1046) | 53.1 (555/1046) | N/A |
| Mean falls/in-patient faller | 2.54±3.14 | 1.84±1.72 | <0.01 |
| Recurrent falls: Range | 1-33 | 1-20 | N/A |
| Interquartile range□ | 2 | 1 | N/A |
| Median falls/in-patient faller | 1.00±3.14 | 1.00±1.72 | N/A |
| Discharge destination | |||
| Own Home % (n) | 50.7% (249/491) | 51.6% (286/555) | 0.67 |
| New Care Home% (n) Inpatient Death% (n) |
20.5% (87/425) | 17.5% (83/475) | 0.23 |
| All Care Home % (n) | 27.9% (137/491) | 23.5% (130/555) | 0.10 |
| Injury | |||
| No Fracture% (n) | 96.1% (472/491) | 94.2% (523/555) | 0.15 |
| Non-Hip Fracture% (n) | 2.0% (10/491) | 2.3% (13/555) | 0.12 |
| Hip Fracture% (n) | 1.8% (9/491) | 3.4% (18/555) | 0.11 |
| Length of stay (days) | |||
| Mean | 43±39 | 41±36 | 0.7 |
| Median | 34±39 | 32±36 | 0.7 |
| Inter-quartile Range | 41 | 36 | N/A |
| Mortality | |||
| In-patient (IP) | 18.9% (93/491) | 15.7% (87/555) | 0.16 |
| 30-day Post discharge | 8% (32/398) | 4.7% (22/471) | 0.04 |
| 6 months Post discharge | 25.1% (100/398) | 18% (85/471) | 0.01 |
The existing resources including education centre facility and equipment were used and expenses arising of this, other expense from previous PDSA, staff or consultant time were not measured. The cost benefits were only done based on bed days saved calculated from the reduction in the LoS and prevention of the new care home placements after the intervention (Final PDSA). These analyses were completed by the Assistant Director of Planning. This gave annualised bed savings of 1100 bed-days and average bed cost/day of £300, resulting in total annualised savings of £330,247. The savings were also made from preventing new care home placements in 10 patients and based on annual care home cost of £31212, a total annualised saving of £311,808 was made. The total annualised savings of £642,055 were made with this quality initiative to prevent IF. The formal complaints received by the health board related to IF during the study period were reduced to half from nine complaints over 17 months before training to five complaints over 20 months post training. Therefore, the unmeasured savings from fewer complaints handling and saving staff time, likely less litigation cost has not been calculated. The cost savings from a likely reduction in the need for Continuing Health Care funding was also not calculated.
See supplementary file: ds9066.doc – Table 1 (FRA tool Audit), Figure 4 (inpatient falls over 4 years), Table 2 (Clinical outcomes before and after intervention)
Lessons and limitations
Lessons have been learnt. The commonly associated themes resulting in hip fractures in single rooms were not studied. Training sessions did not include physiotherapists, occupational therapists, and medical staff, and adjustments have not been made if other multidisciplinary team members have received falls training during the study period. Therefore, our findings must be interpreted with some caution because this is a comparative study and adjustments have not been made for these confounding variables. We are not aware of the other measures were taken by the health board to reduce IF during the study period, other than our training intervention.
In addition, in spite of the substantial reduction of the IF, higher incidence of hip fracture post intervention raises new questions. Therefore, we have completed sub-analyses which suggest that that IF reduction is primarily by avoiding recurrent falls, which is also supported by the fact that the number of patients who were affected by IF before and after the intervention remained the same. The high-risk patients are often identified following a first IF and staff could take appropriate measures to avoid recurrent falls. As reported previously, we also noted no reduction in falls-related injury or hip fracture with our intervention.31 This can be explained by the fact that 66.6% (18/27) hip fractures occurred following the first IF and the number of people affected remains the same despite falls training. Therefore, the biggest lesson for us is to avoid the ‘First Fall’ in the hospital to prevent ‘Hip Fracture’.
Our next step, in addition, to continue to nursing awareness is to engage with the physiotherapist to provide enhanced targeted exercises to those with high falls risk to avoid the ‘First Fall’. Further improvement work using plan-do-study-act methodology is currently being planned with enhanced physiotherapist intervention in a pilot ward. The group is also considering modifying existing FRA tool to include planned mitigation of falls risk factors, which will be developed using multiple PDSA cycles.
We acknowledge that this was a single-centre quality improvement project based on incident reporting and outcome data has been analysed retrospectively. This limits the scope of generalisability of our intervention to different hospital settings. Although the patient population during the study period remains consistent, we have not studied many complex patient characteristics like acute illness, concurrent de-conditioning, co-morbidities, dementia, incontinence, or polypharmacy. We acknowledge that we did not formally assess any change in attitudes, perceptions, or competencies of those undergoing the falls training. The detailed evaluation pre and post training will be addressed in future training sessions. We also acknowledge cost savings have only been analyzed based on bed savings and prevention of care home placement but other confounding factors such as the introduction of new hospital or community services to enhance discharge from hospital have not been included. A falls nurse specialist has been proposed to develop a more sustainable model of nursing support, education and training on falls.
Our improvement project has certain strengths. Project team discussions led by the nursing ward manager were the key component in planning the falls training programme and staff engagement to meet their learning needs. We achieved complete follow-up for IF and mortality for up to two years to evaluate the impact of nurses training on falls. We have also measured the sustainable effect of an educational intervention in reducing IF up to one year. Although few studies have reported a reduction of incidence of IF with nursing teaching, we are not aware of any other study which has reported a comprehensive evaluation of clinical outcome and cost-effectiveness to measure the impact of nurses training on falls in a single room setting.
The improvements and positive feedback have been shared with the staff and ward managers. The falls training has not only developed a culture of good medical practice but has also resulted in changes to practice in the hospital including prompt medication reviews, improved dementia care, and osteoporosis assessment. The project team has proposed spreading similar falls training to other sites within the same organisation to improve the quality of care and patient safety.
This project has evolved over the last two years and the initial measurements were around compliance with completion with the fall risk assessment and incidence of falls. Eighteen months each of outcome data of IF were evaluated and compared retrospectively for both the two previous hospitals and the new hospital site. We found associated adverse clinical outcomes at the new hospital which included significantly higher incidence of hip fracture and higher inpatient and 30-days mortality.16 This brought new problems and challenges for the multidisciplinary team, and, therefore, it becomes a priority to collect data for new measures. Therefore, we introduced new metrics, particularly clinical outcomes including LoS, new care home placement following fall, hip fracture, and mortality as part of this quality improvement project.
This quality improvement project was undertaken in a hospital with 100% single rooms, which is a relatively new concept in the UK. The benefits of single rooms in terms of enhanced dignity and privacy; improved sleep hygiene; meeting the expectations of the public and government policy; reduced healthcare-associated infections16 22 32 and better interaction between family and staff16 has been reported. There is not much research undertaken for risk of falls in the single room setting. Although reduced incidence of IF has been observed among older people with the implementation of systematic falls training, caring for frail older people in single rooms will remain challenging due to lack of companionship and loneliness,33 suggesting further research to policy making and quality of care in such settings. Therefore, new hospitals need to be designed to meet the needs of old and frailer populations and a generalized ‘one size fits all’ guideline should not be applied.1 16 22 32 33 34
Conclusion
In summary, the nurse training programme on falls risk assessment has improved nurse knowledge of falls risk and actual completion of Falls Risk Assessments. This is especially in areas of cognition, environmental hazard, osteoporosis risk. The collaborative quality improvement work has led to a reduction of IF by 34% in a high-risk 100% single room environment. The latest actual falls rate as of November 2015 was 11.7/1000 patient-bed-days, despite 100% single rooms. This is accompanied by improved clinical outcomes as suggested by reduced length of stay and need of new care home placements making a total annualised savings of £642,055. In addition, this intervention has indicated mortality benefits. We propose comprehensive outcome evaluation of the existing inpatient falls data by all organisations with a similar setting and considering appropriate interventions to reduce the impact of inpatient falls on older people in the hospitals.
Acknowledgments
The authors are grateful to all the nursing staff members for attending training sessions and to the Department of Geriatric Medicine, Ysbyty Ystrad Fawr (ABUHB) for continued support for research activities. The authors are also grateful to Dr. Danny Antebi, Dr. John Boulton, Aneurin Bevan Continuous improvement (ABCi) team and Aneurin Bevan University Health Board - Research and Development team for their support with this quality improvement work. The authors would also like to express their gratitude to Mr. David Higgs (DATIX Project Coordinator, Health and Safety) for providing DATIX data. We acknowledge contributions from YYF education centre for organising and supporting training sessions, Mr Ian Morris (Assistant Director of Planning) for doing cost saving analysis, Senior Nurses (Jacqui Mould, Anita Davies, Sue Pearce), Hospital Managers (Mrs Trisha Edwards and Mrs Jane Thornton), Quality and patient safety team (Sian Hughes and Kate Hooton) and Putting things Right team (Jane Dale), geriatric medicine registrars (Dr Manju Krishnan/Dr Shridhar Aithal for delivering teaching sessions, and Dr Shridhar Aithal/Dr Zahid Subhan for helping with data collection), and all others not included in the list.
Footnotes
Declaration of interests: No external funding was applied; nurses training were done during contracted hours at cost neutral basis within health board. None of the authors has any financial or any other kind of personal conflicts with this article.
Ethical approval: This work does not constitute a research study, and is classed as a service improvement project according to the Health Research Authority decision tool, however, all questions and forms required to carry out the study and service evaluation were sent to the research and development (R & D) department, to assess risks to patient identification and the health board. R & D approved the study and confirmed that no further need for ethical approval is required as no patients were directly involved.
References
- 1.Singh I, Okeke J. Risk of inpatient falls is increased with single rooms. BMJ. 2013;347:f6344. [DOI] [PubMed] [Google Scholar]
- 2.Schwendimann R. [Frequency and circumstances of falls in acute care hospitals: a pilot study.] Pflege. 1998;11:335–41. German. [PubMed] [Google Scholar]
- 3.Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33:122–30. [DOI] [PubMed] [Google Scholar]
- 4.Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health. 2005;5:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30 Suppl 4:3–7. [DOI] [PubMed] [Google Scholar]
- 6.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: a systematic review. Int J Nurs Pract. 2001;7:38–45. [DOI] [PubMed] [Google Scholar]
- 8.National Patient Safety Agency. Essential care after an inpatient fall. NPSA/2011/RRR001. NPSA, 2010. Available from: http://www.npsa.nhs.uk/corporate/news/essential-care-after-an-inpatient-fall/ (accessed 21 Sep 2015). [Google Scholar]
- 9.Mahoney JE. Immobility and falls. Clin Geriatr Med. 1998;14:699–726. [PubMed] [Google Scholar]
- 10.Vlahov D, Myers AH, al-Ibrahim MS. Epidemiology of falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil. 1990;71:8–12. [PubMed] [Google Scholar]
- 11.Ugboma I, Drahota AK, Higgins B, Severs M. Effect of bedroom size on falls in hospital: does one size fit all? Jam Geriatr Soc. 2011;59:1153–4. [DOI] [PubMed] [Google Scholar]
- 12.Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients. J Clin Epidemiol, 2001;54:1258–66. [DOI] [PubMed] [Google Scholar]
- 13.Nyberg L, Gustafson Y, Janson A, Sandman PO, Eriksson S. Incidence of falls in three different types of geriatric care: a Swedish prospective study. Scand J Soc Med. 1997;25:8–13. [DOI] [PubMed] [Google Scholar]
- 14.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006. Sep;35 Suppl 2:ii37–41. [DOI] [PubMed] [Google Scholar]
- 15.Mohamed M, Patel D, Zhao S, Ballal MS, Scott S. Increased mortality amongst patients sustaining neck of femur fractures as in-patients in a trauma centre. Open Orthop J. 2015;9:412–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh I, Okeke J, Edwards C. Outcome of in-patient falls in hospitals with 100% single rooms and multi-bedded wards. Age Ageing. 2015;44:1032–35. [DOI] [PubMed] [Google Scholar]
- 17.Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99:137–43. [DOI] [PubMed] [Google Scholar]
- 18.NICE news and features. Older patients at high risk of hospital falls. Available from: https://www.nice.org.uk/news/article/older-patients-at-high-risk-of-hospital-falls [Accessed 16 May 2016]. [Google Scholar]
- 19.Ulrich R, Quan X, Zimring C, Joseph A, Choudhary R. The role of the physical environment in the hospital of the 21st century: a once-in-a-lifetime opportunity. Report to The Center for Health Design, for the designing for the 21st century hospital project, 2004. Available from: http://www.herg.gatech.edu/Files/ulrich_role_physical.pdf (accessed 24 May 2016). [Google Scholar]
- 20.Lawson B, Phiri M. Hospital design: room for improvement. Health Serv J. 2000;110:24–7. [PubMed] [Google Scholar]
- 21.Snow T. Planning the future of ward design. Nurs Stand. 2008;23:12–3. [PubMed] [Google Scholar]
- 22.Pennington H, Isles C. Should hospitals provide all patients with single rooms? BMJ. 2013;347:f5695. [DOI] [PubMed] [Google Scholar]
- 23.Department of Health (2004) The NHS Knowledge and Skills Framework (NHS KSF) and the development review process. Available from: http://www.msg.scot.nhs.uk/wp-content/uploads/KSF-Handbook.pdf (accessed 21 Sep 2015). [Google Scholar]
- 24.Wood J. Exploring staff nurses' views of professional development. Nursing Times. 2006;102, 36–38. [PubMed] [Google Scholar]
- 25.Currid T. Experience of stress in acute mental health nurses. Nurs Times 2008;104: 39–40. [DOI] [PubMed] [Google Scholar]
- 26.Singh I, Morgan K, Belludi G, Verma A, Aithal S. Does nurses' education reduce their work-related stress in the care of older people? Journal of Clinical Gerontology & Geriatrics. 2015;6:34–7. [Google Scholar]
- 27.Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med. 2010; 26:645–92. [DOI] [PubMed] [Google Scholar]
- 28.Cameron ID, Murray GR, Gillespie LD et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010; 20, CD005465. [DOI] [PubMed] [Google Scholar]
- 29.Weinberg J, Proske D, Szerszen A et al. An inpatient fall prevention initiative in a tertiary care hospital. Jt Comm J Qual Patient Saf. 2011; 37:317–25. [DOI] [PubMed] [Google Scholar]
- 30.Dykes PC, Carroll DC, Hurley A et al. Fall prevention in acute care hospitals. A randomized trial. JAMA. 2010;304:1912–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older hospital inpatients. A randomised controlled trial. Age Ageing. 2004;33:390–95. [DOI] [PubMed] [Google Scholar]
- 32.Singh I, Edwards C, Okeke J. Impact of Cognitive Impairment on Inpatient Falls in Single Room Setting and its Adverse Outcomes. J Gerontol Geriatr Res. 2015;S4:S4–001. doi:10.4172/2167-7182.S4-001 [Google Scholar]
- 33.Singh I, Subhan Z, Krishnan M, Edwards C, Okeke J. Loneliness among Older People in Hospitals: A Comparative Study between Single Rooms and Multi-Bedded Wards to Evaluate Current Health Service within the Same Organisation. Gerontol Geriatr Res. 2016; 2: 1015. [Google Scholar]
- 34.Maben J, Griffiths P, Penfold C et al. One size fits all? Mixed methods evaluation of the impact of 100% single-room accommodation on staff and patient experience, safety and costs. BMJ Qual. Safety. 2015;25:241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]