Abstract
Background:
The transport of critically ill patients for procedures or tests outside the Intensive Care Unit (ICU) is potentially hazardous; hence, the transport process must be organized and efficient. Plenty of data is available on pre- and inter-hospital transport of patients; the data on intrahospital transport of patients are limited. We audited the complications and benefits of intrahospital transport of critically ill patients in our tertiary care center over 6 months.
Materials and Methods:
One hundred and twenty adult critically ill cancer patients transported from the ICU for either diagnostic or therapeutic procedure over 6 months were included. The data collected include the destination, the accompanying person, total time spent outside the ICU, and any adverse events and adverse change in vitals.
Results:
Among the 120 adult patients, 5 (4.1%) required endotracheal intubation, 5 (4.1%) required intercostal drain placement, and 20 (16.7%) required cardiopulmonary resuscitation (CPR). Dislodgement of central venous catheter occurred in 2 (1.6%) patients, drain came out in 3 (2.5%) patients, orogastric tube came out in 1 (0.8%) patient, 2 (1.6%) patients self-extubated, and in one patient, tracheostomy tube was dislodged. The adverse events were more in patients who spent more than 60 min outside the ICU, particularly requirement of CPR (18 [25%] vs. 2 [4.2%], ≤60 min vs. >60 min, respectively) with P < 0.05. Transport led to change in therapy in 32 (26.7%) patients.
Conclusion:
Transport in critically ill cancer patients is more hazardous and needs adequate pretransport preparations. Transport in spite being hazardous may lead to a beneficial change in therapy in a significant number of patients.
Key words: Complications, critically ill, intrahospital transport
Introduction
The decision to transport a critically ill patient, either within a hospital or to another facility, is based on an assessment of the potential benefits of transport weighed against the potential risks. It may be pre-, inter-, and intrahospital. In intrahospital transport, critically ill patients are transported to various locations to obtain diagnostic tests or therapeutic procedures.[1] This usually involves moving the patient from an area of the hospital such as the Intensive Care Unit (ICU), the emergency department, the operating theater, areas where treatment with the same intensity is not available.
Even the shortest transport may cause life-threatening complications.[1] The risks include cardiovascular and respiratory instability, missed doses of medication, poor monitoring, and numerous mechanical difficulties.[2,3] Reported complication rates range from 16% to 84%,[4,5] with life-threatening disturbances as high as 8%.[2] Plenty of data is available on pre- and inter-hospital transport, the data available on intrahospital transport are limited.[3,6] The transport of critically ill patients outside the ICU is potentially hazardous; hence, the transport process must be organized and efficient. We audited the intrahospital transport data of adult critically ill patients in our tertiary care center over 6 months.
Materials and Methods
This was a prospective audit undertaken between June 2014 and November 2014 in the ICU of a tertiary care referral center. We obtained a waiver of informed consent from the Institutional Review Board.
One hundred and twenty critically ill adult cancer patients transported from the ICU for either diagnostic or therapeutic procedure over 6 months from June to November 2014 were included.
The data collected included the destination of the patient (computed tomography [CT] scan, intervention radiology, magnetic resonance imaging scan, operation theater, and radiotherapy), the accompanying person (junior or senior resident [JR or SR]), total time spent outside the ICU, and any adverse events such as accidental disconnection or removal of vascular catheters, other tubes, and drains. We also noted the incidence of equipment failure, development of complications such as pneumothorax, need for additional therapy such as need for cardiopulmonary resuscitation (CPR), and increase in the need for vasopressors.
Vitals (heart rate [HR], blood pressure [BP], respiratory rate, oxygen saturation [SpO2]), mode of ventilation (spontaneous or invasive or noninvasive), dose of vasoactive agents, and volume status were noted before initiating transport and after transport. Similarly, Glasgow coma scale and any focal neurological deficits before and after were also noted. Severity score was calculated using the Acute Physiology and Chronic Health Evaluation II (APACHE II) on the day of admission and sequential organ failure assessment (SOFA) score system on the day of transport.
Need for any procedures during the transport such as endotracheal intubation, tracheostomy, ICD insertion, and new venous access was documented.
We also documented whether transport led to any change in therapy such as escalation or de-escalation of antibiotics, insertion of drains or pigtail catheter, or surgical exploration. ICU outcomes of patients were recorded.
Results
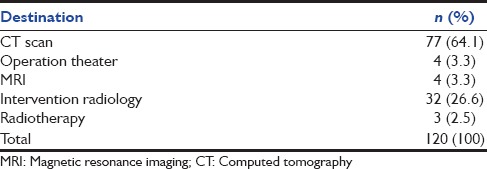
One hundred and twenty critically ill adult cancer patients underwent intrahospital transport. Table 1 shows the destination of the patients. Median HR, median mean BP, and median PaO2 /FiO2 ratio before shifting were 119 bpm, 76 mmHg, and 215, respectively, and afterward, they were 126 bpm, 75 mmHg, and 248, respectively (P > 0.05).
Table 1.
Destination of patients
Among the 120 patients, 51 (42.5%) were transported in an emergency, while it was elective in 69 (57.5%) patients. Thirty two (26.7%) patients were transported by second-year JR, 27 (22.5%) by third-year JR, 47 (39.2%) by first-year SR, and 14 (11.7%) patients by second-year SR.
Complications that occurred during transport are classified as either related to nursing/medical errors or those related to worsening of patients’ physiological condition (major complications plus cardiac arrest). The complications related to nursing/medical error were accidental dislodgement of peripheral intravenous lines, central venous catheters, surgical drains, orogastric tubes, and endotracheal and tracheostomy tubes [Table 2].
Table 2.
Incidence of complications
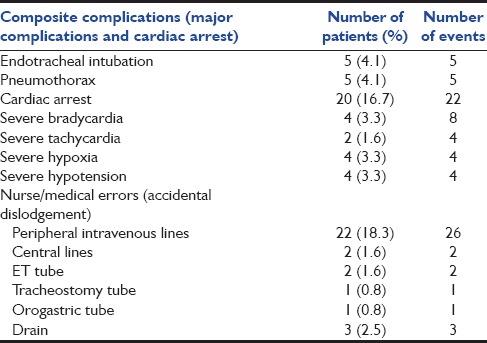
Thirty-four (28.3%) patients had composite complications, which included cardiac arrest and other major complications (spontaneous pneumothorax, sudden cardiac arrest, severe bradycardia [HR <50/min], severe tachycardia [HR >180/min], severe hypoxia [SpO2 <60%], and severe hypotension [mean BP <50 mmHg]) because of worsening of patients’ physiological condition. The total number of major complication events were 52 among 34 (28.3%) patients, 10 patients had more than one complication.
Twenty (16.7%) patients required CPR, i.e. either chest compressions or a bolus dose of adrenaline, among these, 17 (85%) patients were shifted on an emergency basis and 3 (15%) were on an elective basis, 16 (80%) patients were unstable, and 4 (20%) patients were stable.
The incidence of the adverse events (composite complications) was significantly higher (P < 0.05) in patients who spent more than 60 min outside the ICU, particularly the need for CPR (18 [25%] vs. 2 [4.2%]).
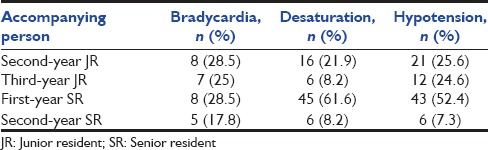
The unfavorable changes in vital parameters and untoward adverse events were more in patients who were accompanied by first-year SR (post-MD) and second-year JR (postgraduate trainees) than the patients who were accompanied by other residents [Table 3]. However, overall, the complications were more in patients transported by SRs as compared to JRs.
Table 3.
Relationship between seniority of accompanying person and adverse events
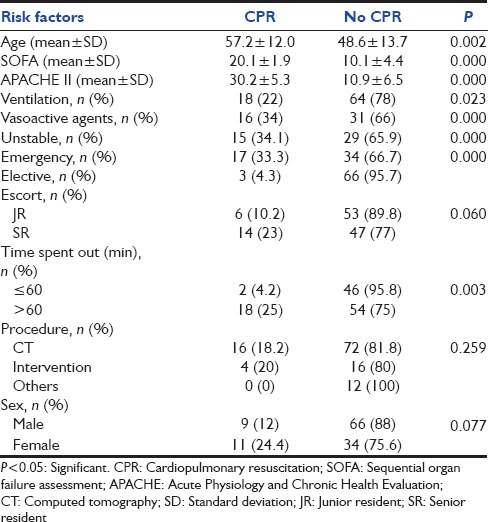
On univariate analysis, patients who were clinically unstable, requiring vasoactive agents, with high severity scores (APACHE II and SOFA), transported on emergency basis, and those who spent more than 60 min outside the ICU showed a significant association (P < 0.05) with the high incidence of composite complications (major complications plus cardiac arrest) and cardiac arrest with a need for CPCR [Tables 4 and 5].
Table 4.
Association between risk factors and composite complications (major complications plus cardiac arrest)
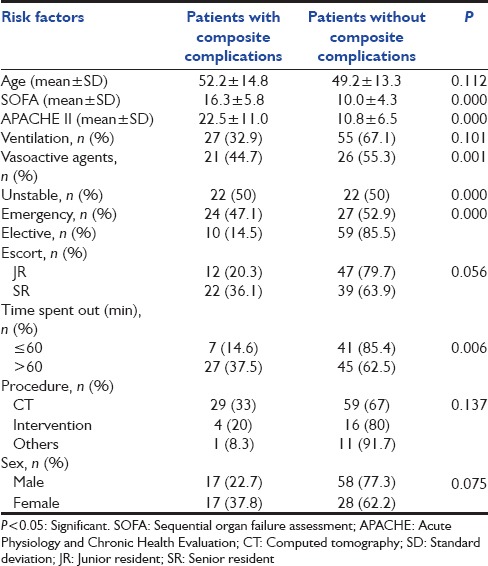
Table 5.
Association between risk factors and cardiac arrest
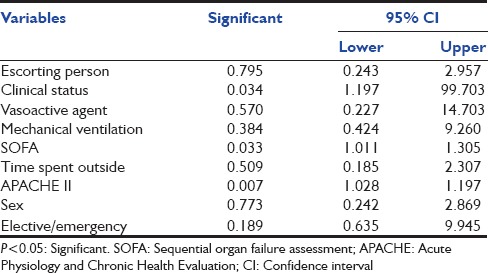
On multivariate analysis of the various risk factors, only severity of illness indices such as SOFA and APACHE II of the patients showed a significant correlation with combined complications (major complications and CPCR) [Table 6].
Table 6.
Multivariate analysis of variables and association with composite complications (major complications and cardiopulmonary resuscitation)
Transport directly led to a change in antibiotic therapy in 43 (35.8%) patients, and other interventions such as insertion of a pigtail catheter for drainage of collections, surgical re-exploration, and angioembolization in 32 (26.7%) patients. Thirty-five percent of the patients died in the ICU, none of the deaths was directly related to transport.
Discussion
Transport should occur when the benefits to the patients exceed the risks; diagnostic tests or procedures are expected to alter the management and they do not compromise the patients’ outcome directly.
In our audit, the incidence of severe adverse events such as cardiac arrest (16.7%) was greater than that reported by Szem et al.[4] (5.9%) and Waydhas (up to 8%).[2] However, on adjusting the incidence of cardiac arrest for age, sex, severity of illness, procedures for which they transported, nature of transport (emergency/nonemergency), duration of transport, accompanying person, and clinical status of the patients before transport, only severity of illness indices (APACHE II and SOFA) showed a significant correlation with the need for CPCR.
In addition, there was a higher incidence of respiratory system-related complications (14.2%) such as desaturation, spontaneous pneumothorax, and accidental extubation, when compared with the data published by Silmara et al. (9.4%).[7] The incidence of accidental dislodgement of lines and drains in our patients was higher (35.8%) than that reported in the literature (25.8%).[8] Our incidence of severe hypotension (3.3%) was modest as compared with other reports (0–21%).[1,2] In addition, the incidence of severe desaturation (3.3%) was consistent with that reported in other studies (2–17%).[1,9,10]
In our study, on univariate analysis, the adverse rates were inversely related to physician seniority which is similar to that of a study done by Papson et al.[8] Overall, more number of major complications occurred in patients transported by SRs, but on logistic regression, there was no significant difference in the complications among JR or SR, this may be because SRs transported sicker patients than those transported by JRs.
We found that the incidence of complications, in particular need for CPR, was inversely related to the time spent outside in ICU. Another important finding was transport led to a change of therapy in nearly one-fourth of the patients transported. Similarly, Hurst et al. reported that diagnostic testing produced a change in therapy in 39% of the patients transported, while abdominal CT and angiography led to a change in treatment in more than 50% of the patients.[10] Our audit shows that intrahospital transport and imaging led to change in therapy, though the transport often led to hazardous changes in vital parameters.
The limitation of our study is that it is a single-center study. Transport can be made safe by stabilizing patients before transport, preparing them adequately, and having trained personnel accompanying the patients.
Conclusion
Transport in critically ill cancer patients is more hazardous and needs adequate pretransport preparations. Transport in spite being hazardous may lead to a beneficial change in therapy in a significant number of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wright I, Rogers PN, Ridley S. Risks in intrahospital transport. Ann Intern Med. 1988;108:638. doi: 10.7326/0003-4819-108-4-638_1. [DOI] [PubMed] [Google Scholar]
- 2.Waydhas C. Intrahospital transport of critically ill patients. Crit Care. 1999;3:R83–9. doi: 10.1186/cc362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovell MA, Mudaliar MY, Klineberg PL. Intrahospital transport of critically ill patients: Complications and difficulties. Anaesth Intensive Care. 2001;29:400–5. doi: 10.1177/0310057X0102900412. [DOI] [PubMed] [Google Scholar]
- 4.Szem JW, Hydo LJ, Fischer E, Kapur S, Klemperer J, Barie PS. High-risk intrahospital transport of critically ill patients: Safety and outcome of the necessary “road trip”. Crit Care Med. 1995;23:1660–6. doi: 10.1097/00003246-199510000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Andrews PJ, Piper IR, Dearden NM, Miller JD. Secondary insults during intrahospital transport of head-injured patients. Lancet. 1990;335:327–30. doi: 10.1016/0140-6736(90)90614-b. [DOI] [PubMed] [Google Scholar]
- 6.Gillman L, Leslie G, Williams T, Fawcett K, Bell R, McGibbon V. Adverse events experienced while transferring the critically ill patient from the emergency department to the intensive care unit. Emerg Med J. 2006;23:858–61. doi: 10.1136/emj.2006.037697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silmara M, Helena Corrêa AP, Helena Bronzatto LC. Characterization of the intrahospital transport of critically ill patients. Acta Paul Enferm. 2014;27:115–9. [Google Scholar]
- 8.Papson JP, Russell KL, Taylor DM. Unexpected events during the intrahospital transport of critically ill patients. Acad Emerg Med. 2007;14:574–7. doi: 10.1197/j.aem.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 9.Wallen E, Venkataraman ST, Grosso MJ, Kiene K, Orr RA. Intrahospital transport of critically ill pediatric patients. Crit Care Med. 1995;23:1588–95. doi: 10.1097/00003246-199509000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Hurst JM, Davis K, Jr, Johnson DJ, Branson RD, Campbell RS, Branson PS. Cost and complications during in-hospital transport of critically ill patients: A prospective cohort study. J Trauma. 1992;33:582–5. doi: 10.1097/00005373-199210000-00015. [DOI] [PubMed] [Google Scholar]


