Abstract
Background
Spotted fever is a tick-borne rickettsial disease. In Brazil, its notification to the Ministry of Health is compulsory. Since 2007, cases of spotted fever have been integrated to the Notifiable Diseases Information System, and epidemiological analyzes are part of the routines on surveillance programs.
Methods
This descriptive study updates epidemiological information on cases of spotted fever registered in Brazil between 2007 and 2015.
Results
In Brazil, 17,117 suspected cases of the disease were reported and 1,245 were confirmed in 12 states, mainly in São Paulo (550, 44.2 %) and Santa Catarina (276, 22.2 %). No geographic information was registered for 132 cases (10.6 %). Most of the infected people were men (70.9 %), mainly in rural areas (539, 43.3 %), who had contact with ticks (72.7 %). A higher number of suspected cases were registered between 2011 and 2015, but the number of confirmed cases and the incidence were relatively low. Moreover, 411 deaths were registered between 2007 and 2015, mainly in the southeastern region of the country, where the case-fatality rate was 55 %. Lack of proper filling of important fields of notification forms was also observed.
Conclusions
The results showed expansion of suspected cases of spotted fever and high case-fatality rates, which could be related to diagnostic difficulties and lack of prompt treatment. These factors may comprise limitations to the epidemiological surveillance system in Brazil, hence improvement of notification and investigation are crucial to reduce morbidity and mortality due to spotted fever in Brazil.
Keywords: Rickettsial diseases, Epidemiology, Information system, Tick-borne disease
Background
Spotted fever (SF) is an infection caused by gram-negative, obligate intracellular bacteria of the genus Rickettsia. The main agent of SF in Brazil is Rickettsia rickettsii. Nevertheless, other species of Rickettsia associated or not to SF clinical cases have been registered in several regions of the country [1–3]. Amblyomma ticks – such as A. sculptum, A. aureolatum and A. ovale – are the main vectors and their hosts (usually horses, capybaras and canines) are nonspecific, therefore, they may also parasitize humans [4, 5]. Rickettsia rickettsii SF is considered the most lethal rickettsial disease, and the maculopapular rash, its characteristic clinical sign, typically appears on the fifth day of infection [6]. However, it is not present in all cases. Rash absence interferes with the differential diagnosis, and R. rickettsii SF may be confused with other diseases including leptospirosis, dengue fever, ehrlichiosis, viral rash diseases, other rickettsial related diseases from typhus group, etc. [6–8]. Moreover, Rickettsia parkeri strain Atlantic rainforest is present in several regions of Brazil, causing a milder spotted fever with characteristic signs (inoculation eschar and lymphadenopathy) [1, 2].
SF has been observed in Brazil since 1929, but only in 2001 it was included in the list of diseases of compulsory notification (DCN) from the Ministry of Health (MH) [9, 10]. Since 2014, it has become a disease of compulsory and immediate notification. Consequently, health professionals are held responsible for reporting suspected and/or confirmed cases to the municipality, state and the Brazilian Ministry of Health within 24 h. Cases of SF are registered into the Notifiable Diseases Information System (SINAN), which aims to collect, gather and disseminate data on this disease [11]. Currently, SF is considered an emerging disease in Brazil due to the increase in diagnosed cases and expansion of occurrence areas. However, it is still little known by health professionals and the general public [12].
Clinical, epidemiological and laboratory aspects must be considered to confirm cases of SF. Epidemiological history of suspected cases helps and may lead to a timely diagnosis supported by laboratory tests [13, 14]. Epidemiological studies are necessary to evaluate the disease behavior over space and time and may help surveillance programs in Brazil [15]. Thus, this study updates epidemiological information on cases of SF registered in Brazil between 2007 and 2015.
Methods
A descriptive epidemiological study was performed based on cases of spotted fever notified by investigation forms (IF) available in SINAN between 2007 and 2015. The database was accessed on March 14th, 2016. Duplicate or inconsistent information (out of the case definition proposed by the MH) were excluded from the analysis.
Cases were considered suspected whenever the individual presented fever, headache, myalgia and history of tick bites, and/or contact with domestic and/or wild animals, and/or had been to SF known transmission areas in the last 15 days, and/or presented maculopapular rash or hemorrhagic manifestations [13, 14]. Cases were confirmed when signs, symptoms and epidemiological history matched the suspect case definition and when infection with Rickettsia from the spotted fever group (SFG) was established [13, 14].
The laboratory testing recommended for SF by the MH consists of serological evidence of a fourfold change in immunoglobulin G (IgG)-specific antibody titers reactive to Rickettsia rickettsia SF group antigens by indirect immunofluorescence assay (IFA) between paired serum samples (one taken in the first week of illness and a second 2–4 weeks later). Moreover, it is also recommended the detection of R. rickettsia or other SF group DNA in a clinical sample via amplification of a specific target by PCR assay, or demonstration of SF group antigens in a biopsy or autopsy sample by immunohistochemistry, as well as isolation of R. rickettsia or other SF group Rickettsia from a clinical sample in cell culture.
Variables associated with confirmed cases were analyzed according to the following classification [16]:
General data of patients about their origin – region of Brazil, federative unit (FU) of notification and municipality of infection.
Individual data – age, gender and ethnic group.
Clinical data – main signs and symptoms.
Epidemiological data – related specifically to exposure risk.
Treatment – if there was hospitalization, dates of admission and discharge.
Specific laboratory data – if there were laboratory tests.
Conclusion data – evolution of cases, confirmation or disposal criterion, location and characteristics of the probable place of infection.
The annual incidence rates were calculated employing the total population per studied year obtained from the Brazilian Institute of Geography and Statistics (IBGE) [17]. The absolute number of deaths and confirmed cases of SF were used to calculate the annual case-fatality rate. Average coefficients of incidence of SF were calculated for municipalities and states (cases/100,000 inhabitants per year) [17].
A proportion between missing/blank records and total filled fields was carried out for the observed variables to assess the completeness of forms. It was based on the inclusion criteria of the confirmed cases, involving mandatory (dates of notification, investigation start, first symptoms and case closing), essential (dates of hospitalization and development of the case) and conditioned variables (dates of hospitalization, discharge and death).
SINAN parameters were used to evaluate the completeness of data: excellent > 90 %, regular = 70–89 % and bad < 70 % of the filled fields. Timeliness was calculated using the difference in days between the intervals between the following dates: notification and investigation, notification and closing, the first symptoms and hospitalization, the first symptoms and discharge, the first symptoms and death.
The software TabWin 32 version 3.6 [18] was used for data tabulation, Microsoft Office Excel 2010 for charts and graphs, and TerraView version 3.2.0.1 for maps [19]. Secondary data was used in accordance with the National Health Council Resolution 466/2012 and does not cover information that could identify individuals registered in the information system [20].
Results
Between 2007 and 2015, 17,117 suspected cases of spotted fever were reported and 1,245 were confirmed in 12 states: São Paulo (n = 550, 44.2 %), Santa Catarina (n = 276, 22.2 %), Minas Gerais (n = 104, 8.5 %), Rio de Janeiro (n = 90, 7.2 %), Espírito Santo (n = 32, 2.5 %), Paraná (n = 25, 2.0 %), Ceará (n = 11, 0.9 %), Rio Grande do Sul (n = 9, 0.7 %), Goiás (n = 7, 0.5 %), Bahia (n = 4, 0.3 %), Mato Grosso do Sul (n = 4, 0.3 %) and Rondônia (n = 1, 0.1 %). No geographic information was registered for 132 cases of SF (10.6 %). Between 2007 and 2009, the number of reported cases decreased, but in the following years, there was an increase in the number of notifications (Fig. 1).
Fig. 1.

Absolute number of reported cases, confirmed ones and deaths due to spotted fever and annual case-fatality rate between 2007 and 2015 in Brazil
The highest incidence rates were observed in Santa Catarina (0.48/100,000 inhabitants) and São Paulo (0.14/100,000 inhabitants) states. Higher incidences were also observed in the municipalities of Rodeio, Corupá and Luiz Alves (14.3, 13.9, and 13.8 respectively) (Fig. 2). Most infected people were white males between 20 and 64 years of age, from rural areas and who had contact with ticks (Table 1). Deaths were more frequent in males (79.1 %) than females (Table 1). Females had home as the primary site of infection acquisition (210/321, 65.4 %) while males probably acquired infection during leisure activities (239/779, 30.6 %).
Fig. 2.
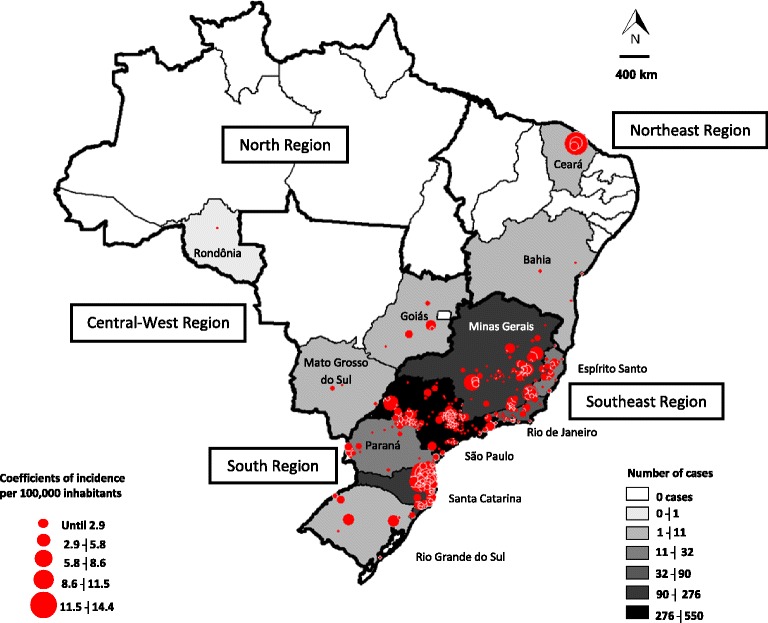
Geographical distribution of confirmed cases of spotted fever by federative unit (FU) and average incidence rate in affected municipalities between 2007 and 2015
Table 1.
Absolute number and percentage of confirmed spotted fever cases and deaths regarding probable area of infection, relation to work, exposure to risk environments and hospitalization, between 2007 and 2015 in Brazil
| Cases | Deaths | |||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Male | ||||
| <1 year | 4 | 0.45 | 2 | 0.61 |
| 1–4 years | 20 | 2.26 | 8 | 2.46 |
| 5–9 years | 49 | 5.54 | 15 | 4.61 |
| 10–14 years | 46 | 5.20 | 18 | 5.53 |
| 15–19 years | 56 | 6.34 | 22 | 6.76 |
| 20–49 years | 445 | 50.39 | 151 | 46.46 |
| 50–64 years | 209 | 23.66 | 82 | 25.23 |
| 65–79 years | 53 | 6 | 27 | 8.30 |
| >80 years | 1 | 0.11 | 0 | 0 |
| Female | ||||
| <1 year | 5 | 1.38 | 1 | 1.16 |
| 1–4 years | 27 | 7.45 | 6 | 6.97 |
| 5–9 years | 27 | 7.45 | 10 | 11.62 |
| 10–14 years | 31 | 8.56 | 12 | 13.95 |
| 15–19 years | 20 | 5.52 | 5 | 5.81 |
| 20–49 years | 183 | 50.55 | 37 | 43.02 |
| 50–64 years | 53 | 14.64 | 12 | 13.95 |
| 65–79 years | 15 | 4.14 | 3 | 3.48 |
| >80 years | 1 | 0.27 | 0 | 0 |
| Ethnic Group | ||||
| White | 816 | 65.54 | 220 | 53.53 |
| Black | 56 | 4.5 | 32 | 7.79 |
| Asian | 7 | 0.56 | 0 | 0 |
| Multiracial | 215 | 17.27 | 90 | 21.9 |
| Indigenous | 4 | 0.32 | 1 | 0.24 |
| Missing/blank | 147 | 11.81 | 68 | 16.55 |
| Probable area of infection | ||||
| Rural | 539 | 43.29 | 146 | 35.52 |
| Urban | 407 | 32.69 | 139 | 33.82 |
| Periurban | 173 | 13.90 | 70 | 17.03 |
| Missing/Blank | 126 | 10.12 | 56 | 13.63 |
| Work-related transmission | ||||
| Yes | 213 | 17.11 | 63 | 15.33 |
| No | 860 | 69.08 | 264 | 64.23 |
| Missing/blank | 182 | 14.62 | 84 | 20.44 |
| Exposure to risk environments | ||||
| Yes | 831 | 66.75 | 254 | 61.80 |
| No | 255 | 20.48 | 64 | 15.57 |
| Missing/blank | 159 | 12.77 | 93 | 22.63 |
| Hospitalization | ||||
| North | 9 | 0.72 | 1 | 0.24 |
| Northeast | 1 | 0.08 | 0 | 0 |
| Southeast | 615 | 49.39 | 336 | 81.75 |
| South | 37 | 2.97 | 4 | 0.97 |
| Central-West | 6 | 0.48 | 1 | 0.24 |
| Missing/blank | 92 | 7.38 | 49 | 11.92 |
The majority of SF patients had visited environments such as forests, rivers and waterfalls (66.7 %) and were exposed to ticks (72.7 %). Other animals such as capybaras (15.6 %), dogs and cats (42.4 %), cattle (17.2 %) and horses (17.4 %) were also reported in the investigation forms of confirmed cases. A higher incidence rate was observed between September and November (41 %). A total of 207 cases of SF (16.6 %) were registered in October.
A total of 411 deaths were registered resulting in an overall case-fatality rate of 33 %. The southeastern region showed the highest case-fatality rate (55 %). An increase of 57.9 % of deaths was observed in the last years (Fig. 1). Among confirmed cases, 760 (61 %) were hospitalized, of which 391 died, representing a case-fatality rate of 51.4 % (Table 1).
Laboratory criteria was the most used in the study period (n = 1,223, 90.2 %) then clinical and epidemiological 103 (8.2 %). The main SF signs and symptoms reported were fever, headache, myalgia, prostration and nausea/vomiting that had a different distribution among Brazilian regions (Fig. 3).
Fig. 3.

Main spotted fever signs and symptoms reported to the Notifiable Diseases Information System, by Brazilian region, between 2007 and 2015. *In the North region only one case was reported that presented the following symptoms: nausea/vomiting, prostration, myalgia, fever and headache
Although most information was available in the notification forms, the discharge date and date of death were the questions less answered (Table 2). Hospitalization date and progression of cases received more responses and were rated as excellent.
Table 2.
Completeness of notification forms for spotted fever in Brazil (2007–2015) concerning dates of notification of the main variables, timeliness of notification and reporting of the first symptoms
| Field | Field completeness | |
|---|---|---|
| N | (%) | |
| Date of notification | 1245 | 100 |
| First symptoms | 1245 | 100 |
| Investigation start | 1245 | 100 |
| Hospitalization | 1238 | 99.43 |
| Admission | 750 | 60.24 |
| Discharge | 368 | 29.55 |
| Course of the case | 1197 | 96.14 |
| Deatha | 424 | 34.05 |
| Closing | 1245 | 100 |
| Timeliness – notification | Media (days) | Median (days) |
| Investigation date | 16.57 | 6 |
| Closing date | 53.36 | 40 |
| Timeliness – reporting of first symptoms | Media (days) | Median (days) |
| Admission date | 7.02 | 4 |
| Discharge date | 16.38 | 8 |
| Deatha | 12.02 | 6 |
aDeath due to spotted fever
Discussion
An increase in the number of suspected cases of SF was observed between 2007 and 2015; however, the number of confirmed cases presented low variation. High case-fatality rates were registered in southeastern Brazil. South and Southeast regions had the highest incidence rates, with most cases being reported in São Paulo and Santa Catarina, a finding corroborated by Barros-Silva et al. [21]. Moreover, the present study shows the first cases of SF in the states of Mato Grosso do Sul and Rondônia, where Rickettsia species were already found in ticks [22, 23]. These results show an expansion of SF in Brazil.
The incorporation of molecular diagnostic techniques by the MH in 2011 increased the number of deaths attributable to SF in Brazil, which could explain the high case-fatality rates registered in the present study [13, 14]. Such techniques allowed the identification of suspected cases that progressed to death without diagnosis using a unique sample. The present work also included records of deaths in southern Brazil, in transition areas within the state of São Paulo, which indicates the possible occurrence of Rickettsia rickettsia. This situation comprises a threat to public health and highlights the need for research on the strains occurring in these regions. Increase in the number of notifications is a result of efforts promoted by the MH, which is developing continuous training processes and educational activities aimed at structuring a network for surveillance of spotted fever and other rickettsial diseases in the country [24].
In the United States of America, a public health system (TickNET) promotes surveillance, research, education and prevention of tick-borne diseases. Nevertheless, notification of cases is not mandatory. In that country, cases are reported under a category called spotted fever rickettsiosis [25–27]. Since the 1930s, countries in the Americas, such as Colombia and Mexico, began to register focal cases of rickettsial diseases as fiebre de tobia and fiebre manchada, respectively. However, these records are collected by research centers and public information is not provided.
The present findings show that most of the confirmed victims were males, which is in agreement with international reports of the Centers for Disease Control and Prevention and the European Center for Disease Prevention and Control [26, 28]. In Brazil, men were infected in leisure activities whereas women become infected in household chores [29]. The most affected ethnic group in Brazil was white people, especially in the Southeast and South. However, rash is not easily seen in black complexion and this could be hindering the diagnosis of SF cases in this ethnic group [30].
The highest incidence was observed in rural areas in individuals who visit forest areas, rivers and waterfalls. Souza et al. [31] reported a high SF incidence in urban areas in São Paulo. The same study also suggested that SF transmission is related to the existence of a dirty pasture environment where A. sculptum ticks and capybaras are present. Although the findings by Souza et al. [31] indicated no relationship between SF and work activities, there is an outbreak record mentioning cases of SF in an animal shelter, which suggests a risk of occupational exposure [32]. Such situation draws attention to the need of preventive practices for professionals engaged in activities that may pose risks for rickettsial infections [33].
Contact with ticks was registered in 72 % of investigation forms. Amblyomma cajennense tick complex has a wide distribution in Brazil [5]. Szabó et al. [4] emphasizes that although Rhipicephalus sanguineus tick is present throughout Brazil, its participation in epidemic cycles has not been definitively proven. Most cases of SF were registered in October, when a higher density of vectors (tick nymphs) is recorded, which may be associated with transmission to humans [34]. However, climate variations should be examined promptly within municipalities and Brazilian ecoregions.
The majority of the confirmed cases required hospitalization. Southeast was the region that had more records of cases and deaths. R. rickettsii have potential for the development of serious forms of the disease, with systemic disorders such as respiratory failure, oliguria, hemorrhagic manifestations, neurological changes and shock. High case-fatality rates may be associated with [29]:
A low index of suspicion per health care professionals.
Lack of knowledge on the clinical features of the disease, which is often confused with other infections that have similar symptoms such as dengue and leptospirosis.
Eco-epidemiological aspects associated with the risk of infection.
Risk factors for exposure to the vector in transmission areas of the disease.
In southern Brazil, the disease is milder and most cases do not require hospitalization. This fact may be associated with infections caused by R. parkeri – an Atlantic rainforest strain that leads to a benign evolution [35]. However, in the north of Paraná, fatal cases of the disease provoked by R. rickettsii were observed [16].
Laboratory tests were used for confirmation of the majority of the cases. The most commonly used is the serologic one that verifies IgM and IgG titers without specifically checking the species of the etiologic agent, which is one of the current limitations of laboratory diagnosis in Brazil. According to Labruna et al. [3], there are different species of Rickettsia of the spotted fever group in Brazil (Rickettsia rickettsii, R. parkeri, R. felis, R. rhipicephali, R. bellii, R. typhi, R. amblyommii, R. andeane and R. monteiroi), many of those with unknown pathogenicity.
The most frequent clinical signs were fever, headache and myalgia. The presence of rash, an important sign of the disease, was recorded in less than 40 % of the confirmed cases. It is necessary to assess the current procedures and to consider regional particularities, thus seeking to identify signs, symptoms and epidemiological characteristics that may be related to the Rickettsia species. SF caused by R. rickettsii evolves rapidly and without the correct and timely medical interventions, clinical cases can develop to severe clinical forms, such as icterus, seizures, hemorrhagic suffusion and extremity necrosis. Further studies should evaluate the burden of SF, considering the impact of deaths of children, young people and adults in working age, as well as amputations resulting from necrotic processes and other sequels. All these injuries generate loss of life years, disability, economic costs to the health system and social security, sick leaves and pensions.
In 2013, the treatment protocol for cases of spotted fever was revised in Brazil, adding new recommendations, with emphasis on use of doxycycline as the first choice medication, regardless of age. The Ministry of Health of Brazil started to provide these drugs in strategic places in endemic areas [36]. Future evaluations of the effectiveness of these new treatment guidelines on case-fatality rates will be required.
The main limitation of this study is the underreporting of cases to epidemiological surveillance systems. The addition of other databases of the Brazilian health system in future analysis – such as those from hospitals, laboratories and mortality information system – would certainly quantify new cases of SF. Low completeness may also interfere with results of studies based on SINAN databases. Regarding confirmed cases, there was complete filling of the notification dates, early symptoms, early research and closing date of the cases. These fields are crucial for understanding the quality of health care in cases of SF. Timeliness – which was analyzed between admission, discharge and death – demonstrated a rapid clinical course and the need to rapidly identify cases and take the appropriate treatment in order to reduce case-fatality rate.
Conclusions
The results showed expansion of suspected cases of spotted fever and high case-fatality rates, which could be related to diagnostic difficulties and lack of prompt treatment. These factors may be limitations of the SF Epidemiological Surveillance System in Brazil, hence improvement of notification and investigation are crucial for to reduce morbidity and mortality due to SF in Brazil.
Acknowledgements
We would like to thank the team from the Zoonosis Surveillance Technical Unit and the technical group for rodent-related diseases from the Ministry of Health of Brazil.
Funding
SVO received financial support from the Coordination for the Improvement of Higher Education Personnel (CAPES). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authors’ contributions
RGG, GSG and SVO conceived and designed the experiments. SVO and JNG performed the experiments. SVO, JNG, GCR, BMCN, KMAV, LXF, FVP, SVCP, EPC, GSG and RGG analyzed the data. SVO contributed materials/analysis tools. RGG, GSG and SVO wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Stefan Vilges de Oliveira, Email: stefanbio@yahoo.com.br.
Jessica Noronha Guimarães, Email: jess.noronha.vet@gmail.com.
Guilherme Carneiro Reckziegel, Email: guilherme.reckziegel@saude.gov.br.
Bidiah Mariano da Costa Neves, Email: bidiah@hotmail.com.
Keline Medeiros de Araújo-Vilges, Email: kelinemed@gmail.com.
Lidsy Ximenes Fonseca, Email: lidsy.fonseca@saude.gov.br.
Fernanda Voietta Pinna, Email: fernanda.voietta@saude.gov.br.
Simone Valéria Costa Pereira, Email: simone.pereira@saude.gov.br.
Eduardo Pacheco de Caldas, Email: eduardo.caldas@saude.gov.br.
Gilberto Salles Gazeta, Email: gsgazeta@gmail.com.
Rodrigo Gurgel-Gonçalves, Email: gurgelrg@hotmail.com.
References
- 1.Spolidorio MG, Labruna MB, Mantovani E, Brandão PE, Richtzenhain LJ, Yoshinari NH. Novel spotted fever group rickettsiosis, Brazil. Emerg Infect Dis. 2010;16(3):521–3. [DOI] [PMC free article] [PubMed]
- 2.Silva N, Eremeeva ME, Rozental T, Ribeiro GS, Paddock CD, Ramos EAG, et al. Eschar-associated spotted fever rickettsiosis, Bahia, Brazil. Emerg Infect Dis. 2011;17(2):275–8. [DOI] [PMC free article] [PubMed]
- 3.Labruna MB, Mattar S, Nava S, Bermudez S, Venzal JM, Dolz G, et al. Rickettsioses in Latin America, Caribbean, Spain and Portugal. Rev MVZ Córdoba. 2011;16(2):2435–57. [Google Scholar]
- 4.Szabó MPJ, Pinter A, Labruna MB. Ecology, biology and distribution of spotted- fever tick vectors in Brazil. Front Cell Infect Microbiol. 2013;3:27. doi: 10.3389/fcimb.2013.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nava S, Beati L, Labruna MB, Cáceres AG, Mangold AJ, Guglielmone AA. Reassessment of the taxonomic status of Amblyomma cajennense with the description of three new species, Amblyomma tonelliae n. sp., Amblyomma interandinum n. sp. and Amblyomma patinoi n. sp., and reinstatement of Amblyomma mixtum, and Amblyomma sculptum (Ixodida: Ixodidae) Ticks Tick Borne Dis. 2014;5(3):252–76. doi: 10.1016/j.ttbdis.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Angerami RN, Câmara M, Pacola MR, Rezende RCM, Duarte RMR, Nascimento EMM, et al. Features of Brazilian spotted fever in two different endemic areas in Brazil. Ticks Tick Borne Dis. 2012;3(5–6):346–8. doi: 10.1016/j.ttbdis.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Del Fiol FS, Junqueira FM, Rocha MC, Toledo MI, Filho SB. Rocky Mountain spotted fever in Brazil. Rev Panam Salud Publica. 2010;27(6):461–6. doi: 10.1590/S1020-49892010000600008. [DOI] [PubMed] [Google Scholar]
- 8.Walker DH, Raoult D. Rickettsia ricketsii and other spotted fever group rickettsiae (Rocky Mountain spotted fever and other spotted fever). In: Mendel GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett´s Principles and practices of infectious diseases. Churchill Livingstone, Philadelphia, 2005
- 9.Piza JT, Meyer JR, Gomes LS. Considerações epidemiológicas e clínicas sobre o tifo exanthematico de São Paulo. São Paulo: Soc Impres Paulista; 1932. [Google Scholar]
- 10.Portaria n° 1.943, de 18 de outubro de 2001, sobre doenças de notificação compulsória. Inf Epidemiol SUS. 2001;10(1):57–8
- 11.Portaria n° 204, de 17 de fevereiro de 2016. Gabinete do Ministro/Ministério da Saúde. Define a Lista Nacional de Notificação Compulsória de doenças, agravos e eventos de saúde pública nos serviços de saúde públicos e privados em todo o território nacional, nos termos do anexo, e dá outras providências. Available in: http://cosemsrs.org.br/imagens/portarias/por_t6h5.pdf.
- 12.Parola P, Paddock CD, Socolovschi C, Labruna MB, Mediannikov O, Kernif T, et al. Update on tick-borne rickettsioses around the world: a geographic approach. Clin Microbiol Rev. 2013;26(4):657–702. doi: 10.1128/CMR.00032-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministério da Saúde do Brasil. Secretaria de Vigilância em Saúde. Doenças de “A” a “Z”. Febre maculosa brasileira e outras riquetsioses. Available in: http://portalsaude.saude.gov.br/index.php?option=com_content&view=article&id=10978&Itemid=657.
- 14.Ministério da Saúde do Brasil. Secretaria de Vigilância em Saúde. Guia de Vigilância em Saúde. Febre maculosa brasileira e outras riquetsioses. Available in: http://portalsaude.saude.gov.br/images/pdf/2015/fevereiro/06/guia-vigilancia-saude-atualizado-05-02-15.pdf.
- 15.Labruna MB. Ecology of rickettsia in South America. Ann N Y Acad Sci. 2009;1166:156–66. doi: 10.1111/j.1749-6632.2009.04516.x. [DOI] [PubMed] [Google Scholar]
- 16.Ministério da Saúde do Brasil. Secretaria de Vigilância em Saúde. Sistema de Informação de Agravos de Notificação - Sinan. Available in: http://portalsinan.saude.gov.br/febre-maculosa.
- 17.Instituto Brasileiro de Geografia e Estatística. Estimativas de População. Available in: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2015/.
- 18.Departamento de Informática do SUS. DATASUS. Download do TabWin. Available in: http://datasus.saude.gov.br/download-do-tabwin.
- 19.TerraView. Projeto TerraView. São José dos Campos, SP: INPE, 2010. Available in: http://www.dpi.inpe.br/terraview/index.php.
- 20.Ministério da Saúde do Brasil, Conselho Nacional de Saúde, Resolução N° 466, de 12 de dezembro de 2012. Aprovar as seguintes diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Available in: http://www.dpi.inpe.br/terraview/index.php.
- 21.Barros-Silva PMR, Pereira SC, Fonseca LX, Maniglia FVP, Oliveira SV, Caldas EP. Febre maculosa: uma análise epidemiológica dos registros do sistema de vigilância do Brasil. Sci Plena. 2014;10(4):047501. [Google Scholar]
- 22.Labruna MB, Camargo LM, Camargo EP, Walker DH. Detection of a spotted fever group Rickettsia in the tick Haemaphysalis juxtakochi in Rondônia, Brazil. Vet Parasitol. 2005;127(2):169–74. doi: 10.1016/j.vetpar.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 23.de Almeida RF, Garcia MV, Cunha RC, Matias J, Araujo e Silva E, de Fatima Cepa Matos M, et al. Ixodid fauna and zoonotic agents in ticks from dogs: first report of Rickettsia rickettsii in Rhipicephalus sanguineus in the state of Mato Grosso do Sul, mid-western Brazil. Exp Appl Acarol. 2013;60(1):63–72. doi: 10.1007/s10493-012-9641-y. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira SV, Pereira SVC, Silva PMRB, Pereira JM, Gomes V, Amorim M, et al. Vigilância de ambientes da febre maculosa brasileira e outras riquetsioses: a etapa inicial de uma proposta para a formação de rede. Rev Pan-Amaz Saude. 2015;6(3):67–71. doi: 10.5123/S2176-62232015000300009. [DOI] [Google Scholar]
- 25.Mead P, Hinckley A, Hook S, Beard CB. TickNET - A Collaborative Public Health Approach to Tickborne Disease Surveillance and Research. Emerg Infect Dis. 2015;21(9):1574. doi: 10.3201/eid2109.150301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Rocky Mountain Spotted Fever. National Center for Emerging and Zoonotic Infectious Diseases, 2015. Available in: http://www.cdc.gov/rmsf/.
- 27.Díaz JS, Cataño JC. Fiebre manchada de lãs montañas rocosas: ni tan manchada ni tan montañosa como pensábamos. Infectio. 2010;14(4):264–76. doi: 10.1016/S0123-9392(10)70120-X. [DOI] [Google Scholar]
- 28.European Centre for Disease Prevention and Control. Epidemiological situation of rickettsioses in EU/EFTA countries. Technical Report, 2013. Available in: http://ecdc.europa.eu/en/publications/Publications/Rickettsioses_2010_final.pdf.
- 29.Angerami RN, Resende MR, Feltrin AFC, Katz G, Nascimento EM, Stucchl RSB, et al. Brazilian spotted fever: a case series from an endemic area in Southeastern Brazil epidemiological aspects. Ann N Y Acad Sci. 2006;1078(1):170–2. doi: 10.1196/annals.1374.030. [DOI] [PubMed] [Google Scholar]
- 30.Favacho ARM, Rozental T, Calic SB, Scofield MAM, Lemos ERS. Fatal Brazilian spotless fever caused by Rickettsia rickettsii in a dark-skinned patient. Rev Soc Bras Med Trop. 2011;44(3):395–6. doi: 10.1590/s0037-86822011000300028. [DOI] [PubMed] [Google Scholar]
- 31.Souza CE, Pinter A, Donalisio MR. Risk factors associated with the transmission of Brazilian spotted fever in the Piracicaba river basin, State São Paulo, Brazil. Rev Soc Bras Med Trop. 2015;48(1):11–7. doi: 10.1590/0037-8682-0281-2014. [DOI] [PubMed] [Google Scholar]
- 32.Rozental T, Ferreira MS, Gomes R, Costa CM, Barbosa PRA, Bezerra IO, et al. A cluster of Rickettsia rickettsii infection at an animal shelter in an urban area of Brazil. Epid infect. 2015;143(11):2446–50. doi: 10.1017/S0950268814003161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barros-Silva PMR, Fonseca LX, Carneiro ME, Araújo-Vilges KM, Oliveira SV, Gurgel-Gonçalves R. Occupational risk of spotted fever: an evaluation of knowledge, attitudes and prevention practices among veterinary medicine students. Rev Patol Trop. 2014;43(4):389–97. [Google Scholar]
- 34.Lemos ERS, Machado RD, Coura JR, Guimarães MA, Freire NMS, Amorim M, et al. Epidemiological aspects of the Brazilian spotted fever: seasonal activity of ticks collected in an endemic area in São Paulo, Brazil. Rev Soc Bras Med Trop. 1997;30(3):181–5. doi: 10.1590/s0037-86821997000300002. [DOI] [PubMed] [Google Scholar]
- 35.Angerami RN, da Silva AM, Nascimento EM, Colombo S, Wada MY, dos Santos FC, et al. Brazilian spotted fever: two faces of a same disease? A comparative study of clinical aspects between an old and a new endemic area in Brazil. Clin Microbiol Infect. 2009;15(s2):207–8. doi: 10.1111/j.1469-0691.2008.02160.x. [DOI] [PubMed] [Google Scholar]
- 36.Ministério da Saúde, Departamento de Gestão e Incorporação de Tecnologias em Saúde da Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Portaria n° 16, de 15 de maio de 2014. Torna pública a decisão de incorporar a doxicilina injetável e o cloranfenicol suspensão para terapêutica da febre maculosa brasileira e outras riquetsioses no Sistema Único de Saúde - SUS. Available in: http://conitec.gov.br/images/Incorporados/Doxiciclina-e-Clorafenicol-FINAL.pdf.


