Keywords: nerve regeneration, traditional Chinese medicine, brain injury, cerebral ischemia, reperfusion, transforming growth factor-beta 1, nerve injury, neurological severity score, neurofunctional rehabilitation, inflammatory reaction, neural regeneration
Abstract
Electroacupuncture at the head acupoints Baihui (GV20) and Shuigou (GV26) improves recovery of neurological function following ischemic cerebrovascular events, but its mechanism remains incompletely understood. We hypothesized that the action of electroacupuncture at these acupoints is associated with elevated serum levels of transforming growth factor beta 1 (TGF-β1). To test this, we established a rat model of cerebral ischemia by middle cerebral artery occlusion. Electroacupuncture was performed at Baihui and Shuigou with a “disperse-dense” wave at an alternating frequency of 2 and 150 Hz, and at a constant intensity of 3 mA. Each electroacupuncture session lasted 30 minutes and was performed every 12 hours for 3 days. Neurological severity scores were lower in injured rats after acupuncture than in those not subjected to treatment. Furthermore, serum level of TGF-β1 was greater after electroacupuncture than after no treatment. Our results indicate that electroacupuncture at Baihui and Shuigou increases the serum level of TGF-β1 in rats with acute cerebral ischemia/reperfusion injury, and exerts neuroprotective effects.
Introduction
Acupuncture is an important part of traditional Chinese medicine. Clinical practice and animal experiments show that acupuncture markedly improves functional recovery after ischemic cerebrovascular disease, but research into its mechanism is lacking.
Transforming growth factor beta 1 (TGF-β1) has many biological effects, contributing to physiological and pathological processes such as cell growth, differentiation, inflammation, tissue repair, angiogenesis, tumorigenesis and metastasis (Ferrari et al., 2006; Wang et al., 2010; Han et al., 2011). Accordingly, TGF-β1 is expressed in a variety of tissues and cells. In the central nervous system, TGF-β1 protects the brain against ischemic injury via its antioxidant and anti-apoptotic actions, and its regulation of microglia and astrocyte responses (Ferrari et al., 2006; Wang et al., 2010; Han et al., 2011). TGF-β1 also alleviates cerebral edema, reduces infarct area, and promotes angiogenesis by inhibiting inflammation in the central nervous system in the early stages of cerebral ischemia.
The mechanism of action of electroacupuncture for inflammatory injury after cerebral infarction is attracting increasing attention. Xu et al. (1998) reported that the Baihui (GV20) acupoint was most frequently used in the acute phase of cerebral apoplexy, followed by Shuigou (GV26). Electroacupuncture at Baihui and Shuigou can affect the brain and choroid plexus.
The aim of the present study was to explore the mechanism underlying the effects of electroacupuncture at head acupoints on cerebral ischemia/reperfusion injury, and to provide new insight into acupuncture treatment of ischemic cerebrovascular disease by measuring TGF-β1 content in blood after middle cerebral artery occlusion (MCAO) in rats.
Materials and Methods
Animals
Seventy-two healthy, clean, adult male Sprague-Dawley rats, weighing 220–270 g, were provided by the Experimental Animal Center of Henan University of Traditional Chinese Medicine, China (license No. SCXK (Yu) 2011-0013). The rats were housed in individual cages, in a well-ventilated room with a 12/12-hour light/dark cycle, at 18–26°C and relative humidity of 40–70%. Rats were allowed free access to food and water, except for 12 hours before surgery, when they were fasted but allowed to drink water freely. The investigation conformed to the Guide for the Care and Use of Laboratory Animals (NIH publication No. 85-23, revised 1996), and the protocol was approved by the Institutional Animal Care Committee of the First Affiliated Hospital of Xinxiang Medical College, China.
Establishment of MCAO model
All 72 rats were randomly divided into three groups: sham-operated (n = 8), model (n = 32) and electroacupuncture (n = 32). The model and electroacupuncture groups were each divided into four subgroups according to reperfusion time (12, 24, 48 and 72 hours; n = 8 rats per subgroup). A rat infarction model was induced by MCAO as previously described (Longa et al., 1989). Rats in the model and electroacupuncture groups were anesthetized with 10% chloral hydrate intraperitoneally and fixed in the supine position. A median incision was made in the neck to expose the common carotid artery, and the internal and external carotid arteries were isolated. Common carotid artery flow was blocked using an artery clamp. A small incision (0.2–0.3 mm long) was made in the external carotid artery, and a suture thread (approximately 0.22 mm in diameter, 60 mm in length) was used to plug the artery. The thread was pulled gently, and when resistance was felt, the end of the thread was deemed to have left the internal carotid artery and reached the external carotid artery stump. The suture was removed 2 hours later to initiate reperfusion. The incision was sutured, the rats were placed in warm, clean cages, and recovery was monitored. The model was considered successful when (1) contralateral limb paralysis and contralateral turning were observed; (2) the hanging tail test was positive; (3) the ipsilateral eye was fully or partially closed. Rats not meeting all three criteria would have been excluded from the experiment, but the model was successfully established in all animals. Sham-injured rats underwent identical procedures except the carotid artery was not occluded.
Acupuncture treatment
According to the meridian circulation and nerve segment distribution, the Baihui and Shuigou acupoints were selected using the animal acupoint atlas for experimental acupuncture (Mergenthaler et al., 2004) and the rat acupoint atlas (Hua et al., 1991). In rats, Baihui is at the middle of the vertex, on the line joining the two ear apexes, and Shuigou is located at the tip of the nose. A Hanyi disposable sterile acupuncture needle (0.35 mm × 25.00 mm; Tianjin Huahong Medical Material Co., Ltd., Tianjin, China) was inserted transversely into the Baihui acupoint, keeping the angle between the needle and the skin surface at 15°. At the Shuigou acupoint, the needle was tilted 30°. The depth of insertion was 10–12 mm. G6805-1 electroacupuncture apparatus (Qingdao Xin Sheng Industrial Co., Ltd., Qingdao, Shandong Province, China) was connected to the handle of the needles after they were inserted into the two acupoints. The following parameters were selected: “disperse-dense” wave, alternating frequency of 2 and 150 Hz, constant intensity of 3 mA. Reperfusion started 2 hours after ischemia, and electroacupuncture treatment was initiated immediately. Each session lasted 30 minutes and was performed once every 12 hours, for 3 consecutive days. The model and sham-injured groups received no treatment. Neurological function and TGF-β1 levels were measured after 12, 24, 48 and 72 hours of reperfusion.
Neurological evaluation
Neurological function was evaluated according to the following five-point scale (Longa et al., 1989): 0, no neurological impairment; 1, contralateral forepaw cannot be completely extended; 2, contralateral turning when walking; 3, limping on the hemiplegic side; 4, loss of consciousness and walking ability.
TGF-β1 measurement
Animals were anesthetized with chloral hydrate. Fasting venous blood (2 mL) was collected from all rats in the morning, and centrifuged for 5 minutes at 3,000 r/min. Serum was obtained and stored at −20°C until use. Serum TGF-β1 level was measured using an enzyme-linked immunosorbent assay kit (Bender MedSystems, Vienna, Austria), according to the manufacturer’s instructions.
Statistical analysis
Data are expressed as the mean ± SD, and were analyzed using SPSS 11.0 software (SPSS, Chicago, IL, USA). Groups were compared by two-way repeated-measures analysis of variance. P < 0.05 was considered statistically significant.
Results
Electroacupuncture improved recovery of neurological function in rats with acute cerebral ischemia/reperfusion injury
Neurological severity scores were higher in the model and electroacupuncture groups than in the sham-injured group 12, 24, 48 and 72 hours after cerebral ischemia/reperfusion (P < 0.05). A slight decrease in neurological severity scores was observed over time in the model and electroacupuncture groups, but this did not reach statistical significance (P > 0.05). Neurological severity scores in the electroacupuncture group were lower than those in the model group at each time point (P < 0.05; Table 1).
Table 1.
Neurological function and serum TGF-β1 level at various times after reperfusion in rat models of MCAO
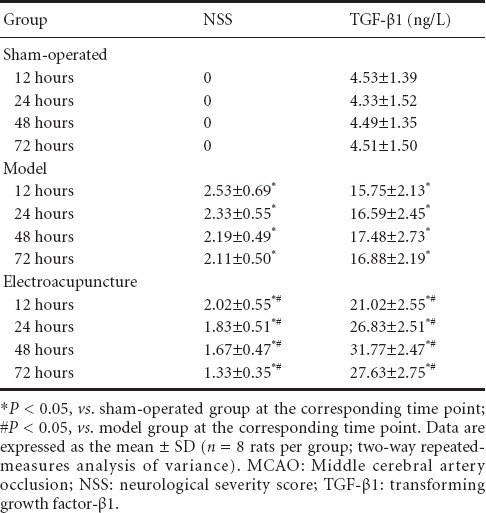
Electroacupuncture increased serum TGF-β1 level in rats with acute cerebral ischemia/reperfusion injury
Serum level of TGF-β1 in the model and electroacupuncture groups was greater than in the sham-operated group 12, 24, 48 and 72 hours after cerebral ischemia/reperfusion (P < 0.05). TGF-β1 level in the model group was significantly elevated after cerebral ischemia/reperfusion at all time points examined, increasing between 12 and 48 hours, and decreasing at 72 hours. In the electroacupuncture group, TGF-β1 level was higher than in the model group at all time points (P < 0.05; Table 1).
Discussion
The present study shows that electroacupuncture at head acupoints can improve recovery of neurological function, promote endogenous TGF-β1 generation, and attenuate cerebral ischemia/reperfusion injury. TGF-β1 expression in neurons is a marker for neuronal survival. The study indicates that electroacupuncture at head acupoints promotes the protection and repair of rat neurons after cerebral ischemia/reperfusion injury, and suggests that electroacupuncture is an effective drug-free treatment for this type of injury.
Studies of acupuncture treatment for ischemic brain injury have made progress in recent years (Zhou et al., 2014). The main functions of acupuncture treatment are improvement of blood circulation, increasing of cerebral blood flow, improvement of hemorheological properties, regulation of metabolism and neurotransmitter balance after ischemia, reduction of oxidative free radical damage, reduction of lipid peroxidation, excitatory amino acid release and toxicity, maintenance of membrane equilibrium, prevention of calcium overload in cells, regulation of gene expression, and inhibition of neuronal apoptosis (Liu et al., 2004; Dong et al., 2009).
These are all important effects in neuroprotection, nerve regeneration, synaptic remodeling and angiogenesis after ischemic cerebrovascular disease. The mechanisms underlying electroacupuncture at head acupoints for the treatment of ischemic cerebrovascular disease are complex, and warrant further research.
Footnotes
Funding: This study was supported by the Key Project Fund of Henan Medical Science and Technology of Henan Province Health Bureau in China, No. 200902009.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using Cross-Check to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Copyedited by Slone-Murphy J, Raye W, Wang J, Qiu Y, Li CH, Song LP, Zhao M
References
- 1.Dong JL, Ni GX. Advances in mechanism of acupuncture treatment of ischemic brain injury. Jiangsu Zhongyiyao. 2009;41:81–82. [Google Scholar]
- 2.Ferrari G, Pintucci G, Seghezzi G. VEGF a prosurvival factor, acts in concert with TGF-beta1 to induce endothelial cell apoptosis. Proc Natl Acad Sci USA. 2006;103:17260–17265. doi: 10.1073/pnas.0605556103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flynn RW, Mac Walter RS, Doney AS. The cost of cerebral ischaemia. Neuropharmacology. 2008;55:250–256. doi: 10.1016/j.neuropharm.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 4.Han MG, Sun JN, Fan AY. Effect of silymarin on the expression of transforming growth factor-β1 mRNA and tissue inhibitor metalloproteinase-1 mRNA in rats with tubulointerstitial fibrosis. Xinxiang Yixueyuan Xuebao. 2011;28:418–421. [Google Scholar]
- 5.Hua XB, Li CR, Zhou HL, Song DL, Hu YL. Research on rat acupoint atlas. Shiyan Dongwu yu Dongwu Shiyan. 1991 [Google Scholar]
- 6.Li ZR. Experimental acupuncture. 2nd edition. Beijing: China press of traditional Chinese Medicine; 2007. [Google Scholar]
- 7.Liu H, Wang Y, Chang LH. Development of neurobiochemical researches on acupuncture treatment of ischemic stroke. Zhen Ci Yan Jiu. 2004;29:72–75. [Google Scholar]
- 8.Longa EZ, Weinstein PR, Carlson S. Reversible middle cerebral Artery occlusion without craniectomy in rats. Stroke. 1989;20:84–91. doi: 10.1161/01.str.20.1.84. [DOI] [PubMed] [Google Scholar]
- 9.Mergenthaler P, Dirnagl U, Meisel A. Pathophysiology of stroke: lessons from animal models. Metab Brain Dis. 2004;19:151–167. doi: 10.1023/b:mebr.0000043966.46964.e6. [DOI] [PubMed] [Google Scholar]
- 10.Wang M, Li B, Zhang GH. Effect of melatonin on transforming growth factor-β and connective tissue growth factor in asthmatic mice. Shiyan Erke Linchuang Zazhi. 2010;25:646–648. [Google Scholar]
- 11.Xu YZ, Bi Z. Study on ancient literature of acupuncture and moxibustion of apoplexy. Shanghai Zhenjiu Zazhi. 1998;17:42–43. [Google Scholar]
- 12.Zhou F, Wang L, Liu PP, Hu WW, Zhu XD, Shen H, Yao YY. Puerarin protects brain tissue against cerebral ischemia/reperfusion injury by inhibiting the inflammatory response. Neural Regen Res. 2014;9:2074–2080. doi: 10.4103/1673-5374.147934. [DOI] [PMC free article] [PubMed] [Google Scholar]


