Keywords: nerve regeneration, ozone, cerebral infarction, magnetic resonance, diffusion tensor imaging, anisotropy, internal capsule, white matter, corticospinal tract, cerebral peduncle, neural regeneration
Abstract
Major ozonated autohemotherapy has been shown to promote recovery of upper limb motor function in patients with acute cerebral infarction, but whether major ozonated autohemotherapy affects remote injury remains poorly understood. Here, we assumed that major ozonated autohemotherapy contributes to recovery of clinical function, possibly by reducing remote injury after acute cerebral infarction. Sixty acute cerebral infarction patients aged 30–80 years were equally and randomly allocated to ozone treatment and control groups. Patients in the ozone treatment group received medical treatment and major ozonated autohemotherapy (47 mg/L, 100 mL ozone) for 10 ± 2 days. Patients in the control group received medical treatment only. National Institutes of Health Stroke Scale score, modified Rankin scale score, and reduced degree of fractional anisotropy values of brain magnetic resonance diffusion tensor imaging were remarkably decreased, brain function improved, clinical efficiency significantly increased, and no obvious adverse reactions detected in the ozone treatment group compared with the control group. These findings suggest that major ozonated autohemotherapy promotes recovery of neurological function in acute cerebral infarction patients by reducing remote injury, and additionally, exhibits high safety.
Introduction
Ozone is a strong oxidant that has been used for many years in the medical field. The Swiss dentist, Fisch (1899–1966), first applied ozone to clinical practice. In 1968, Wolff first used ozone autohemotherapy, or specifically, major ozonated autohemotherapy (MOAH), which was initially applied to systemic disease and cerebral infarction.
MOAH for the treatment of ischemic disease (including severe limb ischemia and ulceration) has achieved certain effects (Adams et al., 2003; Bocci, 2007; Bocci et al., 2009, 2011; Marfella et al., 2010). Moreover, ozone also has an effect on cerebrovascular disease (Clavo et al., 2004; Liu, 2009; Wu et al., 2013).
Transcranial Doppler sonography showed noticeably improved mean flow velocity in the middle cerebral artery, basilar artery, and vertebral artery after ozone therapy in acute cerebral infarction patients compared with the control group (Yin, 2013). Further, our previous study found that MOAH improved recovery of upper limb motor function in patients with acute cerebral infarction (Wu et al., 2013). Reasons for poor therapeutic effects following cerebral infarction include not only difficult nerve regeneration at the infarct site, but also secondary remote injury (Li et al., 2011; Liu et al., 2012). Magnetic resonance diffusion tensor imaging (DTI) can be used to evaluate remote injury after cerebral infarction (Le Bihan, 2003). Fractional anisotropy (FA), a common DTI index, reflects integrity and damage of nerve fibers and myelin sheaths. Specifically, vascular lesions induce neuronal or axonal loss that leads to damage and a resulting decrease in FA values (Nicoletti et al., 2006). DTI can also be used to detect discrete changes in the cerebral peduncle at early onset of internal capsule infarction. Integrity of the cerebral peduncle pyramidal tract is strongly associated with motor function of the affected upper limb (Wang et al., 2015). However, there have been no studies concerning the effect of ozone therapy on remote injury after acute cerebral infarction.
This study aimed to evaluate the clinical efficiency of MOAH for treating acute cerebral infarction by using the National Institutes of Health Stroke Scale (NIHSS) score, modified Rankin scale (mRS) score, and magnetic resonance DTI. DTI was used to objectively evaluate the effect of ozone on secondary remote injury after acute cerebral infarction.
Subjects and Methods
Subjects
A total of 60 acute cerebral infarction patients were recruited for this study, aged 30–80 years, and including 33 males and 27 females. Subjects were hospitalized in the Department of Neurology, Guangzhou General Hospital of Guangzhou Military Command of China from December 2008 to December 2012.
Diagnostic criteria for cerebral infarction
Cerebral infarction (also known as ischemic stroke) results from the death of hypoxic and ischemic brain tissue due to a disrupted blood supply, and leads to neurological deficits. Cerebral infarction is often confined to a blood supply area. Cerebral infarction can be finally diagnosed by a history of acute onset, physical examination, and brain magnetic resonance imaging (MRI) (Adams et al., 2003).
Inclusion criteria
Patients meeting all of the following criteria were considered for admission to our study: (1) 30–80 years old; (2) NIHSS scores of 6–20 (Wu et al., 2013); (3) onset time > 6 hours, < 72 hours, with no intravenous thrombolysis; (4) acute cerebral infarction confirmed by brain MRI; (5) lesions in the blood supply area of the unilateral middle cerebral artery, and a single lesion involving the internal capsule (Likitjaroen et al., 2012); and (6) first onset.
Exclusion criteria
Patients meeting any of the following criteria were excluded from the study: (1) history of cerebral infarction, cerebral hemorrhage, brain tumor, brain contusion, or other brain lesions; (2) thrombolytic therapy; (3) shock, unstable vital signs, peptic ulcer, gastrointestinal bleeding, severe cardiopulmonary complications, liver or kidney dysfunction, or life expectancy ≤ 1 month; (4) blood coagulation dysfunction or abnormal platelet volume and function, thalassemia, sickle cell anemia, or glucose-6-phosphate dehydrogenase deficiency; (5) hyperthyroidism with uncontrolled symptoms; (6) use of kinase drugs or anti-free radical agents; (7) pregnant or lactating women, and patients with mental illness or high sensitivity; (8) patients with a pacemaker or claustrophobia, who could not undergo MRI; and (9) poor compliance, could not complete the relevant examinations, treatments, or recordings.
This study was approved by the Ethics Committee of Guangzhou General Hospital of Guangzhou Military Command of China. Participants and their family members were informed of the protocol, and provided written informed consent. This study was in accordance with the Declaration of Helsinki (World Medical Association, 2014).
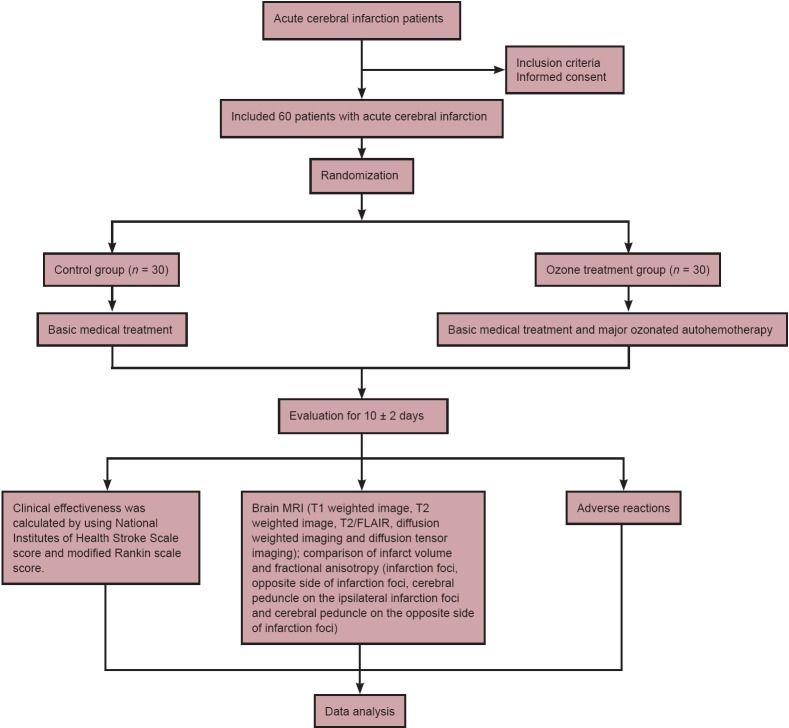
A flow chart of the intervention is shown in Figure 1.
Figure 1.
Intervention flow chart.
Treatment
Sixty acute cerebral infarction patients were equally and randomly assigned to ozone treatment and control groups. Patients in the ozone treatment group underwent medical treatment and MOAH. Patients in the control group only underwent medical treatment.
Medical treatment: (1) aspirin enteric-coated tablets (Bayer HealthCare, Beijing, China), 0.3 g, orally taken, once a night; (2) atorvastatin calcium tablets (Pfizer, New York, NY, USA), 20 mg, orally taken, once a night; (3) Xueshuantong injection, a traditional Chinese patent medicine with the main component being arasaponin (lyophilized, Zhunzi Z20025652, Lot number 11100407) (Guangxi Wuzhou Pharmaceutical Co., Ltd., Wuzhou, Guangxi Province, China), 0.45 g, intravenous drip, once a day; and (4) in accordance with Guidelines for Early Stroke Treatment formulated by the Stroke Council of the American Heart Association in 2003, complications such as hypertension, arrhythmia, and high blood sugar were monitored and treated. Simultaneously, patients received corresponding physical rehabilitation.
A high pressure ozone generator (Humazone Promedic, Humares, Germany) and blood bags were used during MOAH. The procedure was as follows: 100 mL of venous blood was collected from the patient’s elbow and placed in a closed sterile system containing 2.5% sodium citrate 10 mL. Ozone (100 mL, 47 mg/L) was added by a high-pressure method. After mixing for approximately 5 minutes, the mixture was intravenously infused into the patient within 30 minutes. This procedure was performed by a professional nurse in an Ozone Treatment Room, once a day, for 10 ± 2 days as a course.
Therapeutic evaluation
Outcomes were evaluated using NIHSS and mRS (Lai and Duncan, 2001), according to functional defect scores at 10 ± 2 days after treatment. Basic recovery: functional scores decreased by 91–100%; significant improvement: functional scores decreased by 46–90%; improvement: functional scores decreased by 18–45%; ineffectiveness: functional scores decreased by 17%; aggravation: functional scores increased by more than 18%; death. Basic recovery, significant improvement, and improvement were considered effective. Clinical efficiency was calculated by: number of effective individuals/total number × 100%.
MRI measurements
Image acquisition and data processing: MRI was performed using a Sonate 1.5 T MRI scanner (Siemens Medical Solutions, Erlangen, Germany) with a conventional head coil. Subjects lay transversely in the supine position. The scanning parameters were as follows: T1 weighted image: repetition time 107 ms, echo time 9 ms; T2 weighted image: repetition time 3,670 ms, echo time 107 ms; T2/FLAIR: repetition time 8,707 ms, echo time 128 ms; and diffusion weighted imaging: repetition time 3,300 ms, echo time 90 ms, slice thickness 4 mm, field of view: 220 × 220. Infarct volume was calculated according to a previous method (Zhong, 2007): voxel size was sampled to 1 mm × 1 mm × 1 mm using MRIcro version 1.38 software (Siemens). Estimated volume values for the responsible focus (mm3) were obtained by adding the number of voxels. DTI was performed using a single-shot echo-planar imaging pulse sequence: repetition time 10,000 ms, echo time 112 ms, slice thickness 4 mm, interval 0.5 mm, successive scanning of 30 slices, matrix 128 × 128, field of view 240 mm × 240 mm, diffusion sensitive gradient direction (diffusion direction) of 13 and acquisition without diffusion weighting, and diffusion sensitive coefficient b value of 1,000 s/mm2. DTI scanning data were inputted into a Leonard workstation (Siemens, Bonn, Germany) for FA measurement. Selection of oval 34 mm2 regions of interest: infarct focus and distal left-right symmetrical cerebral peduncle regions (Ragin et al., 2006). Regions of inhomogeneous signal, such as calcification, were avoided. Three-dimensional (3D) diffusion tensor images were drawn by diffusion tensor tractography. Based on color FA images, 3D white matter images of the bilateral corticospinal tract were recomposed (minimum FA threshold = 0.20) (Kunimatsu et al., 2004) to observe shift, continuity, and destruction of fiber bundles.
Statistical analysis
Measurement data presented as the mean ± SD were evaluated by SPSS 16.0 software (SPSS, Chicago, IL, USA). The paired t-test was used to compare intragroup data before and after treatment. The two-way analysis of variance or independent samples t-test was used for intergroup comparison. The Wilcoxon rank-sum test was used to detect ranked data. P < 0.05 was considered statistically significant.
Results
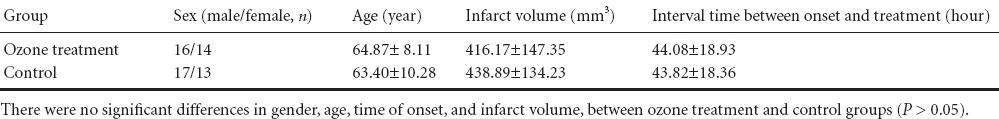
Quantitative analysis of participants and baseline data
Sixty patients were included in the final analysis, and none were excluded. There were no significant differences in gender, age, time of onset, infarct volume, and concomitant diseases between ozone treatment and control groups (P > 0.05). Overall, the above data were comparable (Table 1).
Table 1.
Baseline patient data
Outcome of MOAH for treating acute cerebral infarction
No significant differences in NIHSS or mRS scores were detected between ozone treatment and control groups before treatment (P > 0.05). In contrast, at 10 ± 2 days after treatment, NIHSS scores and mRS scores were significantly decreased in both groups (P < 0.05). NIHSS and mRS scores were both significantly lower in the ozone treatment group compared with the control group (P < 0.05; Table 2). Total efficiency was significantly higher in the ozone treatment group (73.3%) than the control group (70%) (P < 0.05; Table 3).
Table 2.
Changes in NIHSS scores and mRS scores between ozone treatment and control groups before and after treatment
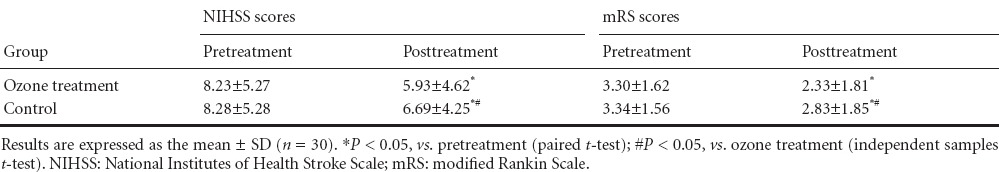
Table 3.
Comparison of total efficiency between both groups
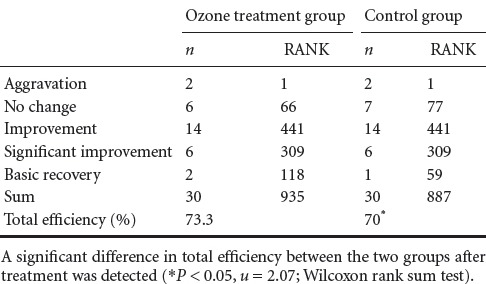
NIHSS scores and mRS scores were significantly different between ozone treatment and control groups at 10 ± 2 days after treatment (P < 0.05; Table 2).
Changes in magnetic resonance DTI after MOAH for treatment of acute cerebral infarction
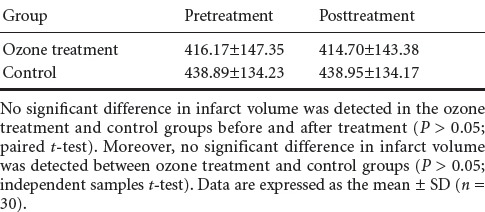
Comparison of infarct volume
Infarct volume was not significantly different in ozone treatment and control groups before or after treatment (P > 0.05). Moreover, no significant difference was detected between ozone treatment and control groups (P > 0.05; Table 4).
Table 4.
Comparison of infarct volume (mm3) between both groups before and after treatment
Comparison of corticospinal tract DTI
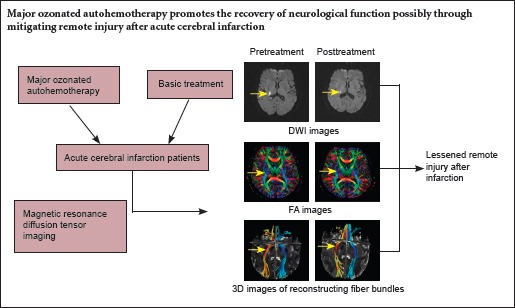
A weak signal was detected in the internal capsule at the site of infarction, and a slightly weak signal in the cerebral peduncle below the infarction site (Figure 2). Therefore, signal was weak in the region where the pyramidal tract forms. With progression, the signal intensity decreased considerably, and was lighter in the ozone treatment group than the control group. DTI revealed no significant change on the infarction side of the corticospinal tract in 13 patients from the ozone treatment group. Additionally, the corticospinal tract was sparse in 17 patients. Further, no significant change was detected on the infarction side of the corticospinal tract in 10 patients from the control group, while the corticospinal tract appeared sparse in 20 patients.
Figure 2.
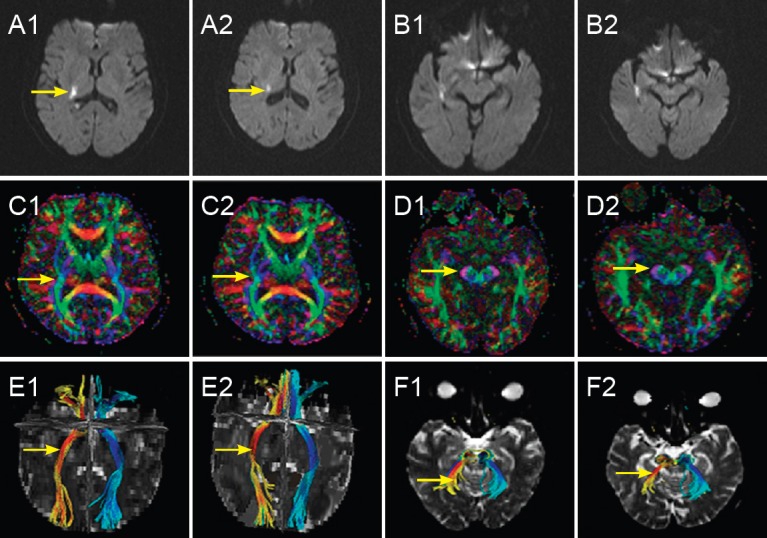
Alterations in a 77-year-old female patient with acute cerebral infarction in the right basal ganglia in the ozone treatment group before and after treatment.
(1, 2) Pretreatment (1) and 9 days posttreatment (2) in the ozone treatment group, respectively. (A, B) Diffusion weighted images of the infarction focus and corresponding cerebral peduncle before and after treatment: signal intensity was lower in the infarction focus after treatment compared with before treatment (arrows), while no obvious abnormal signal was detected in the corresponding cerebral peduncle. (C, D) Fractional anisotropy images of the infarction focus and corresponding cerebral peduncle before and after treatment: signal intensity in the infarction focus and corresponding cerebral peduncle was lower than in contralateral regions before treatment (arrows), but showed a decreased trend after treatment. (E, F) Three-dimensional images of reconstructed fiber bundles in the infarction focus and corresponding cerebral peduncle before and after treatment: corticospinal tracts (arrows) were injured and aggravated after treatment. Yellow represents longitudinal fiber bundles on the infarction side; green represents longitudinal fiber bundles on the normal contralateral side; red represents horizontal fiber bundles on the infarction side; and blue represents horizontal fiber bundles on the normal contralateral side.
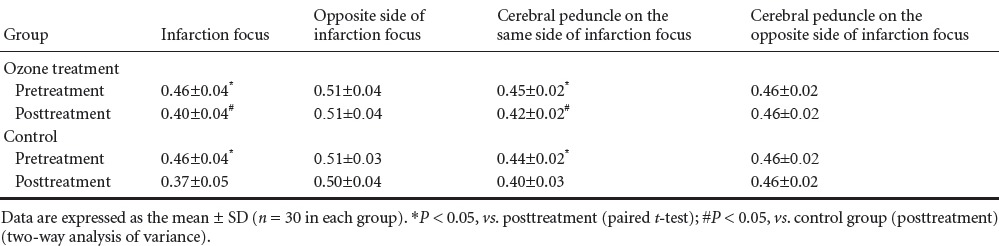
Comparison of FA values
FA values were decreased in infarction foci and ipsilateral cerebral peduncle in both groups (P < 0.05). Likewise, FA values were significantly decreased in infarction foci and ipsilateral cerebral peduncle 10 ± 2 days after treatment. The degree of reduction was less in the ozone treatment group than the control group (P < 0.05; Table 5, Figure 2).
Table 5.
Fractional anisotropy changes in both groups before and after treatment
Adverse reactions
No noticeable adverse reactions were observed in any of the 60 patients who had acute cerebral infarctions in the territory supplied only by the middle cerebral artery. After treatment, brain MRI revealed a small amount of bleeding at the site of infarction in three cases from the ozone treatment group and two cases from the control group, suggesting the capillary bleeding was caused by ischemia and reperfusion. Clinical symptoms did not worsen, so antiplatelet therapy could be continued.
Discussion
We have used NIHSS, mRS, and brain MRI to assess recovery of clinical function after infarction treatment with MOAH. Our results show that MOAH promotes nerve regeneration and recovery of clinical function after acute cerebral infarction.
At present, many basic studies support effects of ozone on recovery of cells and blood vessels after ischemia. (1) Ozone oxidation and oxygen saturation provide sufficient energy for ischemic tissue. Ozone reduces damage to biomacromolecules by reconstructing the redox balance of cells (Mallok et al., 2015). (2) Hoffmann (2001) confirmed that ozone maintains erythrocyte membrane integrity, improves erythrocyte metabolism, activates the pentose phosphate pathway, increases 2,3-diphosphoglycerate content in erythrocytes, and consequently increases oxygen supply. Sycheva et al. (2013) verified that ozone diminishes hypoxia and improves microcirculation after myocardial infarction. (3) MOAH maintains adenosine triphosphate content and energy metabolism under ischemia and hypoxia, and reduces cell apoptosis (Shiratori et al., 1993). (4) Larini et al. (2003) assumed that ozone activates antioxidant enzymes within the body. Ozone pretreatment reduces malondialdehyde and protein carbonyl content, and promotes superoxide dismutase and glutathione peroxidase activity in rat skeletal muscle, suggesting that ozone has important clinical significance in protection from ischemia/reperfusion injury (Koca et al., 2010). Increased O2/O3 concentration and increased expression of Mn-superoxide dismutase, glutathione peroxidase 1, and endothelial nitric oxide synthase in the heart and gastrocnemius (Di Filippo et al., 2015) further indicates that ozone is strongly associated with antioxidant enzymes in the body.
In this study, NIHSS scores and mRS scores were considerably lower in the ozone treatment group than the control group 10 ± 2 days after treatment. Additionally, total efficiency was enhanced in the ozone treatment group compared with the control group. These findings suggest that clinical function is visibly improved in cerebral infarction patients undergoing MOAH. Ozone therapy may improve prognosis in cerebral infarction patients by improving nerve fiber damage and demyelination at the diseased region, and simultaneously, remote pyramidal damage. We detected markedly decreased FA values in the infarction site compared with the contralateral side in both groups before and after treatment. The degree of reduction in FA values was smaller in the ozone treatment group than the control group. Concurrently, decreased degree of FA values in the cerebral peduncle on the infarction side was also significantly smaller in the ozone treatment group than the control group. This may be because ozone rapidly combines with hemoglobin after entering the human body, improving oxygen supply and blood circulation in the brain, and elevating cell viability. Thus, ozone improves hypoxia in the ischemic penumbra, and contributes to collateral circulation and recovery of neurological function (Wu et al., 2013). Ozone therapy activates the antioxidant system, improves blood circulation and oxygen metabolism in cells and local microcirculation, increases adenosine triphosphate in erythrocytes, protects neuronal apoptosis in the ischemic penumbra, reduces fractional edema (Wasser, 2013), mitigates nerve fiber swelling, and reduces anisotropy decreases. Our above results confirm that ozone therapy has a protective and promoting effect on nerves and the remote pyramidal tract in acute cerebral infarction patients. We can infer that ozone therapy may improve nerve fiber damage and demyelination.
Our results demonstrate that 10 ± 2 days after treatment, clinical efficiency is considerably improved in the ozone treatment group. Diffusion weighted imaging did not show significant differences in infarct volume between ozone treatment and control groups, indicating that ozone therapy cannot improve infarct size in a short period, and its effect is not obviously associated with infarct size. Our DTI findings confirmed that after treatment, decreased degree of FA values was significantly less in the infarction focus and cerebral peduncle on the infarction side in the ozone treatment group compared with the control group. This indicates that DTI can more readily detect changes in patients with internal capsule infarction at early onset of the disease. Pyramidal tract integrity in the cerebral peduncle can further assess the degree of recovery after disease, and can reflect outcomes of cerebral infarction. This suggests that ozone therapy may improve prognosis in cerebral infarction possibly by relieving remote pyramidal tract damage.
MOAH is safe and effective for patients with acute internal capsule infarction in the territory supplied only by the middle cerebral artery. During rechecking, no remarkably adverse reactions were found except for a small amount of bleeding around the infarction focus in a few patients. However, Ureyen et al. (2015) suggested that ozone therapy may increase the possibility of thrombotic complications. Because of our limited sample size and the short-term effect, it is not clear whether long-term MOAH can shorten infarction focus and reduce scar tissue formation. Our future studies will use a larger sample size and pay particular attention to the above problems.
Acknowledgments
We thank Dr. Gerd Wasser (German doctor, vice chairman of European Associate of Ozone Therapy) for original ideas and useful theory; and Professor Xiao-feng He (Nanfang Hospital in China, president of Chinese Federation of Ozone Therapy) for valuable guidance and profound knowledge in rich research experience on ozone therapy.
Footnotes
Funding: This research was supported by the Science and Technology Project of Guangdong Province of China, No. 2013B021800164; the Scientific Research Project in Medicine of Guangdong Province of China, No. B200258.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using Cross-Check to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Copyedited by James R, de Souza M, Wang J, Qiu Y, Li CH, Song LP, Zhao M
References
- 1.Adams HP, Jr, Adams RJ, Brott T, del Zoppo GJ, Furlan A, Goldstein LB, Grubb RL, Higashida R, Kidwell C, Kwiatkowski TG, Marler JR, Hademenos GJ. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003;34:1056–1083. doi: 10.1161/01.STR.0000064841.47697.22. [DOI] [PubMed] [Google Scholar]
- 2.Bocci V. The case for oxygen-ozonetherapy. Br J Biomed Sci. 2007;64:44–49. doi: 10.1080/09674845.2007.11732755. [DOI] [PubMed] [Google Scholar]
- 3.Bocci V, Borrelli E, Travagli V, Zanardi I. The ozone paradox: ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29:646–682. doi: 10.1002/med.20150. [DOI] [PubMed] [Google Scholar]
- 4.Bocci V, Zanardi I, Huijberts MS, Travagli V. Diabetes and chronic oxidative stress. A perspective based on the possible usefulness of ozone therapy. Diabetes Metab Syndr. 2011;5:45–49. doi: 10.1016/j.dsx.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Clavo B, Catala L, Perez JL, Rodriguez V, Robaina F. Ozone therapy on cerebral blood flow: a preliminary report. Evid Based Complement Alternat Med. 2004;1:315–319. doi: 10.1093/ecam/neh039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Filippo C, Trotta MC, Maisto R, Siniscalco D, Luongo M, Mascolo L, Alfano R, Accardo M, Rossi C, Ferraraccio F, D’Amico M. Daily oxygen/O3 treatment reduces muscular fatigue and improves cardiac performance in rats subjected to prolonged high intensity physical exercise. Oxid Med Cell Longev 2015. 2015:190640. doi: 10.1155/2015/190640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffmann A VR. The influence of ozone on 2,3-diphosphoglycerate synthesis in red blood cell concentrates. Imperial College London: The 15th ozone world congress; 2001. [Google Scholar]
- 8.Koca K, Yurttas Y, Bilgic S, Cayci T, Topal T, Durusu M, Kaldirim U, Akgul EO, Ozkan H, Yanmis I, Oguz E, Tunay S, Korkmaz A, Basbozkurt M. Effect of preconditioned hyperbaric oxygen and ozone on ischemia-reperfusion induced tourniquet in skeletal bone of rats. J Surg Res. 2010;164:e83–89. doi: 10.1016/j.jss.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 9.Kunimatsu A, Aoki S, Masutani Y, Abe O, Hayashi N, Mori H, Masumoto T, Ohtomo K. The optimal trackability threshold of fractional anisotropy for diffusion tensor tractography of the corticospinal tract. Magn Reson Med Sci. 2004;3:11–17. doi: 10.2463/mrms.3.11. [DOI] [PubMed] [Google Scholar]
- 10.Lai SM, Duncan PW. Stroke recovery profile and the Modified Rankin assessment. Neuroepidemiology. 2001;20:26–30. doi: 10.1159/000054754. [DOI] [PubMed] [Google Scholar]
- 11.Larini A, Bianchi L, Bocci V. The ozone tolerance: I) Enhancement of antioxidant enzymes is ozone dose-dependent in Jurkat cells. Free Radic Res. 2003;37:1163–1168. doi: 10.1080/10715760310001604170. [DOI] [PubMed] [Google Scholar]
- 12.Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nat Rev Neurosci. 2003;4:469–480. doi: 10.1038/nrn1119. [DOI] [PubMed] [Google Scholar]
- 13.Li C, Ling X, Liu S, Xu A, Zhang Y, Xing S, Pei Z, Zeng J. Early detection of secondary damage in ipsilateral thalamus after acute infarction at unilateral corona radiata by diffusion tensor imaging and magnetic resonance spectroscopy. BMC Neurol. 2011;11 doi: 10.1186/1471-2377-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Likitjaroen Y, Suwanwela NC, Mitchell AJ, Lerdlum S, Phanthumchinda K, Teipel SJ. Isolated motor neglect following infarction of the posterior limb of the right internal capsule: a case study with diffusion tensor imaging-based tractography. J Neurol. 2012;259:100–105. doi: 10.1007/s00415-011-6134-6. [DOI] [PubMed] [Google Scholar]
- 15.Liu X, Tian W, Li L, Kolar B, Qiu X, Chen F, Dogra VS. Hyperintensity on diffusion weighted image along ipsilateral cortical spinal tract after cerebral ischemic stroke: a diffusion tensor analysis. Eur J Radiol. 2012;81:292–297. doi: 10.1016/j.ejrad.2010.12.053. [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Cui YG, Jiang L, Rong MG. Evaluation of the efficacy of High-pressure ozone on acute cerebral infarction. Zhongguo Dangdai Yiyao. 2009;16:2. [Google Scholar]
- 17.Mallok A, Vaillant JD, Soto MT, Viebahn-Hansler R, Viart Mde L, Perez AF, Cedeno RI, Fernandez OS. Ozone protective effects against PTZ-induced generalized seizures are mediated by reestablishment of cellular redox balance and A1 adenosine receptors. Neurol Res. 2015;37:204–210. doi: 10.1179/1743132814Y.0000000445. [DOI] [PubMed] [Google Scholar]
- 18.Marfella R, Luongo C, Coppola A, Luongo M, Capodanno P, Ruggiero R, Mascolo L, Ambrosino I, Sardu C, Boccardi V, Lettieri B, Paolisso G. Use of a non-specific immunomodulation therapy as a therapeutic vasculogenesis strategy in no-option critical limb ischemia patients. Atherosclerosis. 2010;208:473–479. doi: 10.1016/j.atherosclerosis.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Nicoletti G, Lodi R, Condino F, Tonon C, Fera F, Malucelli E, Manners D, Zappia M, Morgante L, Barone P, Barbiroli B, Quattrone A. Apparent diffusion coefficient measurements of the middle cerebellar peduncle differentiate the Parkinson variant of MSA from Parkinson’s disease and progressive supranuclear palsy. Brain. 2006;129:2679–2687. doi: 10.1093/brain/awl166. [DOI] [PubMed] [Google Scholar]
- 20.Ragin AB, Wu Y, Storey P, Cohen BA, Edelman RR, Epstein LG. Monocyte chemoattractant protein-1 correlates with subcortical brain injury in HIV infection. Neurology. 2006;66:1255–1257. doi: 10.1212/01.wnl.0000208433.34723.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiratori R, Kaneko Y, Kobayashi Y, Yamamoto Y, Sano H, Ishizu Y, Yamamoto T. Can ozone administration activate the tissue metabolism? A study on brain metabolism during hypoxic hypoxia. Masui. 1993;42:2–6. [PubMed] [Google Scholar]
- 22.Sycheva EI, Khodasevich LS, Solomina OE, Zubareva MI. The influence of ozone therapy on oxygen metabolism kinetics and the microcirculation system during spa and resort treatment of the post-infarction patients. Vopr Kurortol Fizioter Lech Fiz Kult. 2013:9–13. [PubMed] [Google Scholar]
- 23.Ureyen CM, Bas CY, Arslan S. Myocardial infarction after ozone therapy: is ozone therapy Dr. Jekyll or Mr. Hyde? Cardiology. 132:101–104. doi: 10.1159/000431078. [DOI] [PubMed] [Google Scholar]
- 24.Wang RR, Li C, Zhang S, Zhou LJ, He L, Li HD. Diffusion tensor imaging change in crus cerebri in striatocapsular infarction and correlation with upper extremity motor dysfunction. Radiol Med. 2015 doi: 10.1007/s11547-015-0534-0. [DOI] [PubMed] [Google Scholar]
- 25.Wasser G. Ischemic stroke penumbra and extracorporeal ozone treatment. Neuroradiol J. 2013;26:243–251. doi: 10.1177/197140091302600301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Medical Association (2014) Declaration of Helsinki: ethical principles for medical research involving human subjects. General Assembly of the World Medical Association. J Am Coll Dent. 81:14–18. [PubMed] [Google Scholar]
- 27.Wu X, Li Z, Liu X, Peng H, Huang Y, Luo G, Peng K. Major ozonated autohemotherapy promotes the recovery of upper limb motor function in patients with acute cerebral infarction. Neural Regen Res. 2013;8:461–468. doi: 10.3969/j.issn.1673-5374.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yin Y. The effect of ozone therapy on the cerebral blood flow of patients with acute ischemic stroke. Zhongguo Dangdai Yiyao. 2013;20:2. [Google Scholar]
- 29.Zhong HZ. Study on the relationship between the syndromes of Ischemic stroke within 72 hours and the lesion volume under MRI. Beijing: Beijing Chinese Medicine University; 2007. [Google Scholar]