Abstract
Background:
Surveys suggest most people would prefer to die in their own home.
Aim:
To examine predictors of place of death over an 11-year period between 2000 and 2010 in Dumfries and Galloway, south west Scotland.
Design:
Retrospective cohort study.
Setting/Participants:
19,697 Dumfries and Galloway residents who died in the region or elsewhere in Scotland. We explored the relation between age, gender, cause of death (cancer, respiratory, ischaemic heart disease, stroke and dementia) and place of death (acute hospital, cottage hospital, residential care and home) using regression models to show differences and trends. The main acute hospital in the region had a specialist palliative care unit.
Results:
Fewer people died in their own homes (23.2% vs 29.6%) in 2010 than in 2000. Between 2007 and 2010, men were more likely to die at home than women (p < 0.001), while both sexes were less likely to die at home as they became older (p < 0.001) and in successive calendar years (p < 0.003). Older people with dementia as the cause of death were particularly unlikely to die in an acute hospital and very likely to die in a residential home (p < 0.001). Between 2007 and 2010, an increasing proportion of acute hospital deaths occurred in the specialist palliative care unit (6% vs 11% of all deaths in the study).
Conclusion:
The proportion of people dying at home fell during our survey. Place of death was strongly associated with age, calendar year and cause of death. A mismatch remains between stated preference for place of death and where death occurs.
Keywords: Place of death, cause of death, home, acute hospital, residential care, cottage hospital, death, palliative care, dementia, advance care planning, hospice, hospice care, patient preference
What is already known about the topic?
The provision of appropriate end-of-life care is increasingly seen as a health priority in the United Kingdom and other developed countries.
Surveys suggest that most people would prefer to die in their own homes.
Most UK deaths still occur in National Health Service (NHS) hospitals.
What this paper adds?
In a predominantly rural area of Scotland between 2000 and 2010, there was a decline in deaths at home and on the general wards of the acute hospital and an increase in deaths in the specialist palliative care unit (SPCU) and residential care.
Men and women were less likely to die at home as they became older.
Older people with dementia as the cause of death were particularly unlikely to die in an acute hospital and very likely to die in a residential home.
Implications for practice, theory or policy
There remains a mismatch between stated preference for place of death and where death occurs.
We should continue to monitor trends in place of death
Health and social services should consider how best to meet the future needs and preferences of an increasingly old and frail UK population.
Introduction
The provision of appropriate end-of-life care is increasingly seen as a health priority in the United Kingdom and other developed countries.1 Most people still die in hospital despite many expressing a preference to die at home.2 Figures from National Records of Scotland and the British Office for National Statistics show that in 2010, 58% of all deaths in Scotland3 and 54% of all deaths in England and Wales4 occurred in hospital. The proportion who die in hospital varies internationally, from 11% in Albania to 78% in Japan5 with different health care systems likely contributing to these variations. Similar international variations are seen when cancer and non-cancer deaths6 and other deaths that require palliative care are considered separately.7
Hospice care is a common preference when offered as an end-of-life treatment option. In a study of patients attending general practices, 64% identified home as the preferred place for end-of-life care with 16% favouring a hospice as the second most popular option.8 In those having close personal experience of dying, the proportion preferring hospice care was higher at 35%. Another UK study of patients admitted to a hospice found both patient and relative preferences for a home death decreased as death approached (for patients 90%–50% and relatives 92–40%), whereas preference for a hospice death increased (for patients 10%–40% and relatives 8%–40%).9
Against this background, and the recent observation that at any one time 29% of hospital inpatients in Scotland have entered the last year of their lives,10 the purpose of our study was to examine the determinants of place of death in Dumfries and Galloway, a largely rural region in south west Scotland, over an 11-year period between 2000 and 2010. Our primary aim was to determine whether death at home was becoming more or less common. Second, we wanted to explore the relation between age, gender, cause and place of death and the extent to which our hospital’s specialist palliative care unit (SPCU) impacted acute hospital deaths.
Methods
The main data sources for our retrospective cohort study were death registration records from National Records of Scotland3 and the Scottish Morbidity Records (SMR01) dataset, which records all inpatient and day case discharges from non-obstetric and non-psychiatric specialties in Scottish National Health Service (NHS) hospitals.11 We included all 19,697 deaths of Dumfries and Galloway residents that occurred in the region or elsewhere in Scotland, but not if they occurred outside Scotland as we did not always have information on place of death. We excluded 461 deaths of visitors from other areas who died in Dumfries and Galloway as their end-of-life care planning was unlikely to be within local influence; and 162 people who died in transport accidents as their deaths were clearly unplanned.
The first part of our analysis was of the relation between age, gender, calendar year and place of death. We selected an 11-year period between 2000 and 2010 in order to examine time trends and considered four places of death: acute hospital, cottage hospital, residential care and home. Acute hospitals included the local district general hospital, a smaller community hospital that also provides acute care, and any other acute hospital in Scotland (usually tertiary care centres). We were able to document admission to the SPCU using SMR01 records from 2007, enabling us to distinguish SPCU deaths from those that occurred elsewhere in the acute hospital between 2007 and 2010. The SPCU is an eight-bedded facility within the acute hospital run by a palliative care consultant and multidisciplinary team, accessed by general practitioners (GPs) and acute hospital inpatients.
Cottage hospitals were eight 12–24 bed hospitals and one nursing home in which cottage hospital beds are commissioned. These are run by GPs, accessed by GPs and hospital consultants and offer adult assessment, rehabilitation and palliative care. Residential care covered all cases where the institutional code on the death certificate was a care home, nursing home or a mental health facility (primarily long-term patients in the community). The home setting comprised deaths occurring in the person’s own home together with all non-institutional locations including 21 deaths in ambulances, 2 in prisons, 2 in clinics and 1 in a GP surgery. We felt it was logical to consider these non-institutional locations as ‘home’ because most of those dying at one of these locations will have been living at home. The time period used was calendar year of death registration rather than actual date of death, in line with the reporting of national death statistics.3
We examined the relation between age band, gender, year and place of death by fitting a binary logistic regression model with ‘died at home’ or ‘did not die at home’ as the outcome variable. Age, gender and year of death were the explanatory variables. In the model, the categorised age variable was considered as continuous for simplicity as the relationship with the outcome variable turned out to be linear (in the logit scale). The baseline for the outcome variable was dying at home, while the baselines for the explanatory variables were age group 75 years, female gender and year of death 2007. We also tested for possible interactions including that between age and year of death.
The second part of our analysis was of the relation between age, gender, cause and place of death between 2007 and 2010. We considered six disease categories: cancer, ischaemic heart disease (IHD), stroke, respiratory disease, dementia and other causes. The first four are the main causes of death in Dumfries and Galloway, and dementia was included as it is a major cause of cognitive frailty. The cause of death was taken as the underlying cause of death from the death record using International Classification of Diseases–Revision 10 (ICD-10) codes: C00-C97 for cancer, I21-I25 for IHD, I60-I69 for stroke and J00-J99 for respiratory disease. We used the dementia code groups F01, F03, G30 and R54 from the End of Life Care Local Authority Profiles to define dementia deaths.12 We also investigated the proportion of deaths in the SPCU that were for diseases other than cancer. All causes of death in our study were mutually exclusive. Patients with dementia and cancer were considered to have died from cancer, as per the World Health Organization (WHO) ICD-10 coding algorithm.
In order to examine these relationships in more detail, we fitted a multinomial logistic regression model with four possible places of death (acute hospital, cottage hospital, residential care and home) as outcome variables. Age, gender, year of death and the six causes of death were the explanatory variables. The baseline category for the cause of death was other causes (i.e. not cancer, IHD, stroke, respiratory disease or dementia). Marginal probabilities from the final model were used to explore the effect of these on the outcome variables. We used R statistical software.
Results
A total of 19,697 deaths of Dumfries and Galloway residents over the period 2000–2010 met our inclusion criteria. Table 1 shows the population characteristics and underlying causes of death in each of the four settings. Of all deaths during the 11 years of our study, 9333 (47.4%) were in an acute hospital, 5229 (26.5%) at home, 3073 (15.6%) in residential care and 2062 (10.5%) in cottage hospitals. People were more likely to die at home when they were younger and more likely to die in residential care and cottage hospitals as they became older. Table 1 also suggests that people were less likely to die at home in 2010 than in 2000. These changes occurred against a background of an ageing population and a progressive reduction in acute hospital, cottage hospital and residential care beds during the period of study: the number of people aged 75 years and over rose by 21.1% from 12,260 to 14,850 between 2000 and 2010, while acute hospital beds fell from 350 to 330, cottage hospital beds from 185 to 170 and residential care beds from 1244 to 1202.
Table 1.
Place of death by age, gender and year of registration.
| Cottage hospital, n (%) | Home, n (%) | Residential care, n (%) | Acute hospital, n (%) | |
|---|---|---|---|---|
| Age | ||||
| <65 | 118 (3.7) | 1388 (43.5) | 33 (1.0) | 1649 (51.7) |
| 65–74 | 296 (7.6) | 1314 (33.7) | 182 (4.7) | 2110 (54.1) |
| 75–84 | 840 (12.5) | 1617 (24.1) | 918 (13.7) | 3337 (49.7) |
| 85+ | 808 (13.7) | 910 (15.4) | 1940 (32.9) | 2237 (37.9) |
| All ages | 2062 (10.5) | 5229 (26.5) | 3073 (15.6) | 9333 (47.4) |
| Gender | ||||
| Male | 971 (10.3) | 2949 (31.3) | 918 (9.7) | 4585 (48.7) |
| Female | 1091 (10.6) | 2280 (22.2) | 2155 (21.0) | 4748 (46.2) |
| Year of registration | ||||
| 2000 | 185 (10.6) | 516 (29.6) | 253 (14.5) | 792 (45.4) |
| 2001 | 180 (10.4) | 520 (30.0) | 259 (14.9) | 775 (44.7) |
| 2002 | 177 (10.2) | 466 (26.9) | 291 (16.8) | 796 (46.0) |
| 2003 | 202 (10.8) | 534 (28.6) | 285 (15.2) | 849 (45.4) |
| 2004 | 211 (11.5) | 482 (26.3) | 266 (14.5) | 876 (47.7) |
| 2005 | 191 (10.5) | 450 (24.8) | 258 (14.2) | 914 (50.4) |
| 2006 | 171 (9.6) | 462 (25.9) | 267 (14.9) | 886 (49.6) |
| 2007 | 159 (8.6) | 501 (27.2) | 296 (16.1) | 887 (48.1) |
| 2008 | 167 (9.5) | 442 (25.2) | 290 (16.6) | 852 (48.7) |
| 2009 | 215 (12.2) | 431 (24.5) | 276 (15.7) | 835 (47.5) |
| 2010 | 204 (11.1) | 425 (23.2) | 332 (18.1) | 871 (47.5) |
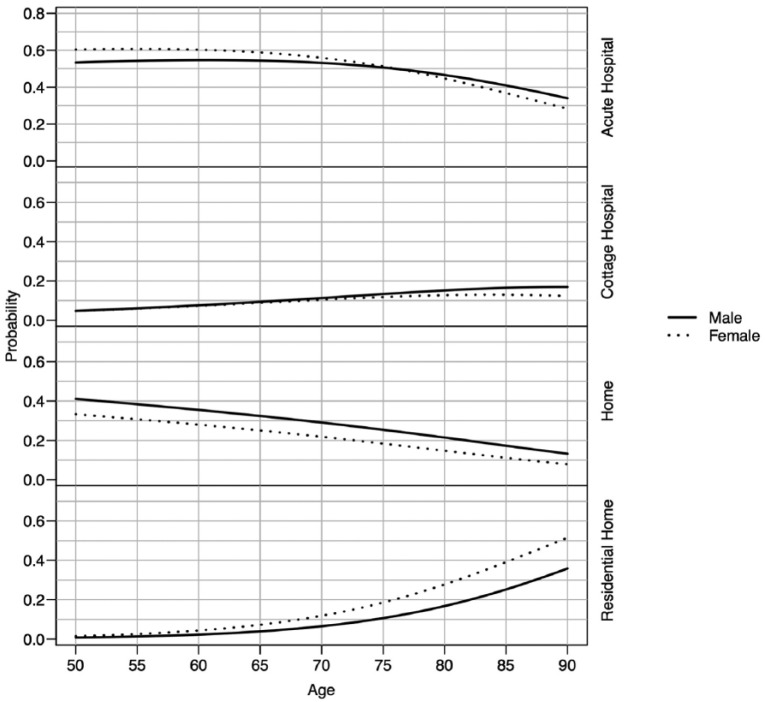
The results of our binary logistic regression model, in which the outcome variable was dying at home, confirm that people were less likely to die at home than not at home (p < 0.001), that men were more likely to die at home than women (p < 0.001) and that both sexes were less likely to die at home with age (p = 0.001) (Figure 1). We also show significant trends with time. Figure 2 shows the relationship predicted by this model for the effect of age and year of death registration on the probability of dying at home between 2007 and 2010. Men and women were more likely to die at home if under 60 years of age and progressively less likely to die at home if over 60 years during this time period (p = 0.003). We show parameter estimates and confidence intervals for the binary logistic regression model in Appendix 1 (available online).
Figure 1.
Likelihood of dying in each of four locations of death by age and gender between 2000 and 2010, as fitted in binary regression model. Men and women were progressively less likely to die at home or in an acute hospital and more likely to die in a cottage hospital or residential care as they became older.
Figure 2.
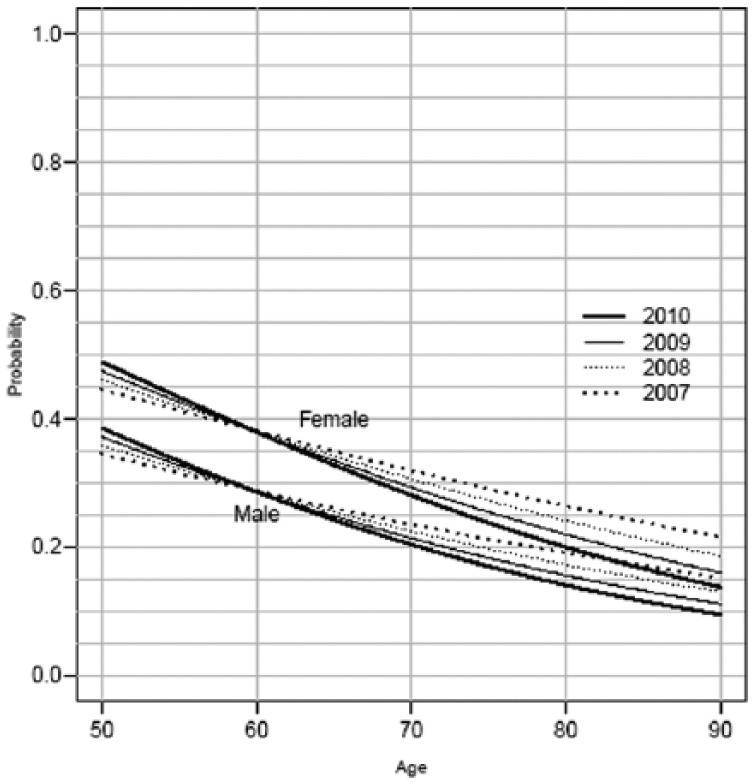
Likelihood of dying at home by age, gender and year of death registration between 2007 and 2010, as fitted in binary regression model. In 2010, the effect of age was ‘steeper’ than in 2007, that is, the probability of dying at home decreased progressively as people became older than in 2007.
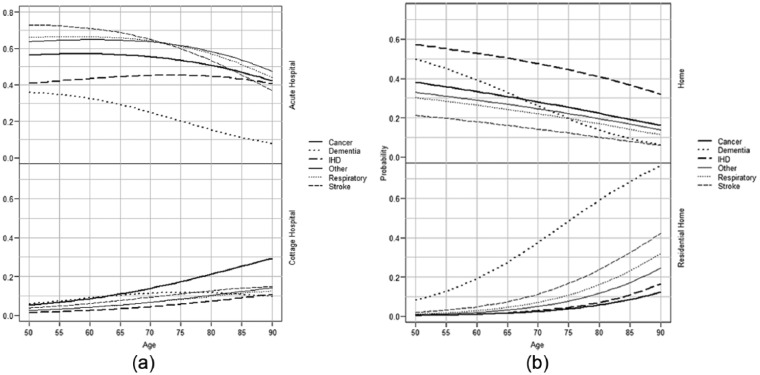
We report the relation between six causes of death and place of death between 2007 and 2010 in Table 2. The six causes of death were cancer, IHD, stroke, respiratory disease, dementia and all other causes. Those with cancer were most likely to die in acute hospitals (51.8%) and moderately likely to die at home (27.8%). Home was the most common place of death for people with IHD (43.7% of all IHD deaths) but not for those whose cause of death was stroke (10%) or respiratory disease (17.6%). Patients with dementia were most likely to die in residential care (71.7%). Figure 3 shows the additional effect of age: people were less likely to die at home as they aged irrespective of cause of death, whereas older people with dementia as cause of death were particularly unlikely to die in an acute hospital and very likely to die in a residential home. Parameter estimates and confidence intervals for the multinomial logistic regression model are given in Appendix 2 (available online)
Table 2.
Place of death by cause of death 2007–2010.
| Cottage hospital, n (%) | Home, n (%) | Residential care, n (%) | Acute hospital, n (%) | SPCU, n (%) | Not SPCU, n (%) | |
|---|---|---|---|---|---|---|
| Malignant neoplasm | 321 (15.7) | 569 (27.8) | 97 (4.7) | 1059 (51.8) | 549 (26.8) | 510 (24.9) |
| Ischaemic heart disease | 75 (6.3) | 519 (43.7) | 102 (8.6) | 493 (41.5) | 8 (0.7) | 485 (40.8) |
| Stroke | 76 (11.0) | 69 (10.0) | 214 (31.1) | 330 (47.9) | 8 (1.2) | 322 (46.7) |
| Respiratory | 76 (8.7) | 153 (17.6) | 181 (20.8) | 460 (52.9) | 6 (0.7) | 454 (52.2) |
| Dementia | 42 (8.5) | 47 (9.5) | 354 (71.7) | 51 (10.3) | 3 (0.6) | 48 (9.7) |
| Other causes | 155 (8.2) | 442 (23.3) | 246 (13.0) | 1052 (55.5) | 86 (8.2) | 966 (91.8) |
| All causes | 745 (10.4) | 1799 (25.0) | 1194 (16.6) | 3445 (48.0) | 660 (9.2) | 2785 (38.8) |
SPCU: specialist palliative care unit.
Figure 3.
(a) Likelihood of dying in an acute or cottage hospital by age and cause of death between 2007 and 2010, as fitted in multinomial regression model. Those with dementia as cause of death were particularly unlikely to die in an acute hospital as they aged. (b) Likelihood of dying at home or in residential care by age and cause of death between 2007 and 2010, as fitted in multinomial regression model. People were less likely to die at home as they aged. Those with dementia very likely to die in a residential home as they aged.
Between 2007 and 2010, 660 out of 3445 (19.2%) of all acute hospital deaths occurred in the SPCU. The proportion of deaths that occurred in the SPCU increased from 6.4% in 2007 to 10.7% of all deaths in 2010. When we considered SPCU deaths separately, then the proportion of deaths occurring in the rest of the acute hospital fell from 41.7% in 2007 to 36.8% in 2010. Most SPCU deaths (83.2%) were due to cancer, while 549 out of 1059 (51.8%) of the patients who died in an acute hospital of cancer between 2007 and 2010 did so in the SPCU (Table 2).
Discussion
The main findings of our study are that fewer people died in their own homes in 2010 compared to 2000 (23.2% vs 29.6%). Men were more likely to die at home than women, while both sexes were less likely to die at home as they became older and in successive calendar years irrespective of the cause of death. Older people with dementia as the cause of death were particularly unlikely to die in an acute hospital and very likely to die in a residential home. Between 2007 and 2010, an increasing proportion of acute hospital deaths occurred in the SPCU (6% vs 11% of all deaths in the study).
Place of death and diagnosis
Place of death was strongly related to diagnosis. Deaths from cancer primarily occurred in acute hospitals or at home. Most acute hospital cancer deaths occurred in the SPCU with home and SPCU accounting for over 50% of all cancer deaths. This supports the view that patient preferences are being met in the majority of deaths from cancer. The acute hospital, but not the SPCU, was a common place of death for patients with IHD, stroke and respiratory disease. We observed that as many deaths from IHD occurred at home as in hospital, presumably reflecting the high incidence of sudden death in these patients.
Residential care was the commonest place of death for patients whose cause of death was dementia and the second most common place of death for patients with stroke and respiratory disease (Table 2; Figure 3). Very few patients whose primary cause of death was dementia died at home, as observed by others.13 These findings may be in keeping with patient choice if we accept that residential care becomes ‘home’ for many elderly patients. If we combine all home and residential care deaths to take account of this view, then this becomes the most common place of death over acute hospital excluding SPCU (41.6% vs 38.8% as per Table 2). Although home death may have been the majority preference in the early stages of dementia, this is unlikely to be practical without a significant increase in resource as disease progresses.
Factors predicting home death
Higginson identified four factors predicting home death in the United Kingdom: age, socioeconomic status, degree of urbanisation and ethnicity.14 Home death is less likely in the elderly, metropolitan areas, non-Caucasians and lower socioeconomic groups.14 Our study supports increasing age as a strong negative predictor for home death (Figure 3), and this together with the ageing population of Dumfries and Galloway15 may well explain the decline in home deaths. We cannot comment on the influence of urbanisation, ethnicity and socioeconomic status given that Dumfries and Galloway is rural, predominately Caucasian and the fact that area deprivation codes are poor at identifying rural deprivation.16
Home versus hospital?
Although we know that people who die spend over 90% of the last 6 months of their lives in the community,17 it is still not clear whether dying at home is better than dying in hospital for patients and their families.14,18 If it was agreed that death in an acute hospital general ward is the least desirable option for patients in whom death can be anticipated and planned, then a shift in place of death from acute hospital to home, hospice, residential care or cottage hospital is required. Our view is not necessarily that home is the most desirable of these options but that acute hospital may be the least desirable. There are, nevertheless, several reasons why an acute hospital might remain the commonest place of death in 2010 despite a majority of patients expressing a wish to die at home. Health professionals do not find it easy to discuss end-of-life issues19 and may therefore be unaware of preferences for place of death.20 The patient may change their mind as death approaches9 and relatives may insist on active treatment when a palliative approach might be more appropriate. Acute hospital admission may become necessary in those whose last illness is not anticipated and when development of an inter-current illness means the patient is unable to be supported at home.21 It is perhaps inevitable, therefore, that acute hospital with or without SPCU remains the most common place of death in this and other studies
National and international comparisons
A study from England and Wales between 2004 and 2010 reported a decrease in NHS hospital deaths (58% to 54%) and rise in home deaths (18% to 21%).4 This is in contrast to the decline in home deaths we observed, although home deaths were still more common in south west Scotland in 2010 (23.3%) than in England and Wales (20.8%) in the same year. In Belgium, a shift from hospital to care homes has recently been reported, as in our study.22 International comparisons are difficult to interpret given the differences in health care systems that exist in different countries though trends suggest that home deaths are slowly increasing in some, but not all, developed economies. The challenge for the United States23 and Canada24 is to continue this trend, and for Italy25 and Greece26 to reverse theirs, despite an ageing population and higher expectations of a good death at the end of life. The inclusion of specialist home palliative care services in national health policies is likely to be crucial for success here.27
Strengths and limitations
Our study has strengths and limitations. We believe we are one of the first UK studies to investigate place of death for five major diseases, and by doing so identify the challenges in enabling people to have choice over their place of death. This crucial part of end-of-life care is relevant to those with major organ failure and frailty as well as cancer. We acknowledge three important limitations. First, we recorded place of death rather than place of care. It is possible that an individual was cared for at home up to the last hours of life but recorded as an acute hospital death. Second, many who died in our acute hospital received specialist palliative care input although they were not admitted to the SPCU. Third, our cause of death analysis did not account for comorbidity or frailty, both of which may make a home death less likely.
Conclusion
In conclusion, our data suggest evolving trends in place of death with fewer deaths at home and in the general wards of acute hospital but more deaths in SPCU and residential care. Very few patients over 85 years and even fewer of those whose primary cause of death was dementia died in their own home. We should continue to monitor trends in place of death, while health and social services consider how best to meet the future needs and preferences of an increasingly old and frail UK population.
Supplementary Material
Acknowledgments
C.I., D.C., H.B., A.C. and A.A. had the idea for the paper, created the research questions, shaped the design and analysis and wrote the first draft. A.A., C.W. and R.M.-A. were responsible for the statistical analyses. All authors contributed to the final draft. The authors would like to acknowledge Richard Hunter, ISD Scotland, who provided additional statistical support, and Drs Peter Hutchison and Lindsay Martin for their input to the design of this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Because this study was a survey and did not involve identifiable patient data, we did not seek ethical approval in keeping with our Health Board policy.
Exclusive licence: The corresponding author (C.I.) has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence on a worldwide basis to the Sage Publishing Group Ltd and its Licensees.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Dixon J, King D, Matosevic T, et al. Equity in the provision of palliative care in the UK: review of evidence. Personal Social Services Research Unit, London School of Economics, April 2015, www.pssru.ac.uk/publication-details.php?id=4962 (accessed 12 September 2015). [Google Scholar]
- 2. Gomes B, Higginson I, Calanzani N, et al. ; on behalf of PRISMA. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 2012; 23: 2006–2015. [DOI] [PubMed] [Google Scholar]
- 3. National Records Scotland Annual Vital Events Statistics. http://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/general-publications/births-deaths-and-other-vital-events-preliminary-annual-figures
- 4. Gomes B, Calanzani N, Higginson IJ. Reversal of the British trends in place of death: time series analysis 2004–2010. Palliat Med 2011; 26: 102–107. [DOI] [PubMed] [Google Scholar]
- 5. Broad JB, Gott M, Kim H, et al. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 population, using published and available statistics. Int J Public Health 2013; 58: 257–267. [DOI] [PubMed] [Google Scholar]
- 6. Cohen J, Houttekier D, Onwuteaka-Philipsen B, et al. Which patients with cancer die at home? A study of six European countries using death certificate data. J Clin Oncol 2010; 28: 2267–2273. [DOI] [PubMed] [Google Scholar]
- 7. Pivodic L, Pardon K, Morin L, et al. ; on behalf of EURO-IMPACT. Place of death in the population dying from diseases indicative of palliative care need: a cross-national population-level study in 14 countries. J Epidemiol Community Health 2016; 70: 17–24. [DOI] [PubMed] [Google Scholar]
- 8. Charlton RC. Attitude towards care of the dying: a questionnaire survey of general practice attenders. Fam Pract 1991; 8: 356–359. [DOI] [PubMed] [Google Scholar]
- 9. Hinton J. Which patients with terminal cancer are admitted from home care? Palliat Med 1994; 8: 197–210. [DOI] [PubMed] [Google Scholar]
- 10. Clark D, Armstrong M, Allan A, et al. Imminence of death among hospital inpatients: prevalent cohort study. Palliat Med 2014; 28: 474–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. ISD Scotland Data Dictionary A-Z. SMR01-General/Acute Inpatient and Day Case. http://www.ndc.scot.nhs.uk/Dictionary-A-Z/Definitions/index.asp?Search=S&ID=460&Title=SMR01%20-%20General/Acute%20Inpatient%20and%20Day%20Case
- 12. National End of Life Care Intelligence Network. End of life care local authority profiles – indicators metadata guide, http://www.endoflifecare-intelligence.org.uk/view?rid=511
- 13. Sleeman K, Ho Y, Verne J, et al. ; on behalf of the GUIDE_Careproject. Reversal of English trend towards hospital death in dementia: a population-based study of place of death and associated individual and regional factors, 2001–2010. BMC Neurol 2014; 14: 59, http://www.biomedcentral.com/1471-2377/14/59 (accessed 4 April 2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higginson I, Sarmento V, Calanzani N, et al. Dying at home – is it better: a narrative appraisal of the state of the science. Palliat Med 2013; 27: 918–924. [DOI] [PubMed] [Google Scholar]
- 15.Baseline Study and Regional Economic Profile for Dumfries and Galloway Regional Economic Strategy 2014–2020. http://crichtonobservatory.org.uk/index.php/component/content/article/98-data-themes/995-baseline-study-and-regional-economic-profile-for-dumfries-and-galloway-regional-economic-strategy-2014-2020
- 16. Scottish index of multiple deprivation 2009: general report, www.scotland.gov.uk/publications/2009/10/28104046/0 (accessed February 2012).
- 17. Percentage of end of life spent at home or in a community setting, http://www.isdscotland.org/Health-Topics/Health-and-Social-Community-Care/Publications/data-tables.asp?id=1462#1462
- 18. Harding R. Response to place of death in the population dying from diseases indicative of palliative care need: a cross-national population-level study in 14 countries. J Epidemiol Community Health 2016; 70: 9. [DOI] [PubMed] [Google Scholar]
- 19. Munday D, Petrova M, Dale J. Exploring preferences for place of death with terminally ill patients: qualitative study of experiences of general practitioners and community nurses in England. BMJ 2009; 338: b2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Meussen K, Van den Block L, Bossuyt N, et al. GPs’ awareness of patients’ preference for place of death. Br J Gen Pract 2009; 59: 665–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCall K, Rice AM. What influences decisions around the place of care for terminally ill cancer patients? Int J Palliat Nurs 2005; 11: 541–547. [DOI] [PubMed] [Google Scholar]
- 22. Houttekier D, Cohen J, Surkyn J, et al. Study of recent and future trends in place of death in Belgium using death certificate data: a shift from hospitals to care homes. BMC Public Health 2011; 11: 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Flory J, Yinong YX, Gurol I, et al. Place of death: U.S. trends since 1980. Health Aff 2004; 23: 194–200. [DOI] [PubMed] [Google Scholar]
- 24. Wilson DM, Truman CD, Thomas R, et al. The rapidly changing location of death in Canada, 1994–2004. Soc Sci Med 2009; 68: 1752–1758. [DOI] [PubMed] [Google Scholar]
- 25. Costantini M, Balzib D, Garronecc E, et al. Geographical variations of place of death among Italian communities suggest an inappropriate hospital use in the terminal phase of cancer disease. Public Health 2000; 114: 15–20. [DOI] [PubMed] [Google Scholar]
- 26. Yang L, Sakamoto N, Marui E. A study of home deaths from 1951 to 2002. BMC Palliat Care 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gomes B, Calanzani N, Curiale V, et al. Effectiveness and cost effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013; 6: CD 007760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.