Abstract
Objective
Persons with serious mental illness frequently receive inadequate medical care and are more likely to experience difficulty navigating the health care system compared with the general population. To address this gap in quality, we developed a program of peer co-led collaborative activation training for primary care (CAT-PC) designed to improve “patient activation” and person-centered care in primary care visits for middle-aged and older adults with serious mental illness and cardiovascular risk. This report presents pilot study feasibility and participant outcomes for CAT-PC.
Method
A pre-post pilot evaluation of CAT-PC included N = 17 adults (age ≥ 50) with serious mental illness and cardiovascular health risk conditions, and N = 6 primary care providers. CAT-PC consists of 9 weekly peer co-led patient education and skills training sessions and a 45-min video-based training for primary care providers. Pre-post measures included the Patient Activation Measure (PAM), Perceived Efficacy in Patient-Physician Interactions (PEPPI), Autonomy Preference Index (API) for preferred role in primary care encounters, and Social Skills Performance Assessment (SSPA) role-play test for medical visits.
Results
All 17 participants attended 5 or more sessions. Post-intervention improvement was found for patient activation and simulated performance of medical visit communication skills. Trends were observed for improved self-efficacy in provider interactions and greater preference for a more collaborative role in decision-making.
Conclusions and Implications
CAT-PC is a brief, peer co-led education and skills training intervention potentially improving patient activation in primary care encounters and providing an important missing component in emerging models of “patient-centered behavioral health homes” for this high-risk group.
Keywords: patient activation, medical encounter, skills training, older adult, serious mental illness
People with serious mental illness have a life expectancy 8 to 32 years shorter than the general population (Colton & Manderscheid, 2006; Druss, Zhao, Von Esenwein, Morrato, & Marcus, 2011), a gap that has increased by 15 years since the early 2000s (Viron & Stern, 2010). This health disparity is largely due to the elevated burden of cardiovascular risk factors, such as obesity, diabetes, and metabolic syndrome, experienced within this group at nearly twice the rate of the general population (Scott & Happell, 2011; Sokal et al., 2004), combined with a lack of adequate and appropriate medical care (Wang, Demler, & Kessler, 2002). Although the frequency of medical care provider visits is comparable between individuals with or without mental illness, those with serious mental illness have lower rates of screening for common chronic health conditions and are at greater risk to receive lower quality care (Druss, Rosenheck, Desai, & Perlin, 2002; Frayne et al., 2005; Nasrallah et al., 2006). For example, adults with schizophrenia and diabetes are less likely to receive routine hemoglobin A1c monitoring, blood lipid profiles, or eye exams when compared with persons with diabetes who do not have a mental illness (McIntyre, 2009; Meyer & Stahl, 2009; Morden, Mistler, Weeks, & Bartels, 2009). In a separate study of people over 65 years of age hospitalized for an acute myocardial infarction, those with psychiatric conditions had a 19% greater 1-year mortality rate compared with the general population (Druss, Bradford, Rosenheck, Radford, & Krumholz, 2001). This higher mortality rate was attributable to the failure to receive guideline-based care that is routinely recommended following a heart attack (Druss et al., 2001). The observation that individuals with serious mental illness are less likely to receive standard evidence-based health care, despite seeing physicians at similar rates, suggests that there is a different dynamic that may impede effective collaboration between providers and patients for this high-risk group.
To date, efforts to improve the quality of health care for people with serious mental illness have focused on the implementation of “behavioral health homes” that promote routine health screening, registries of chronic health conditions, and the provision of basic primary care within mental health service delivery settings (Substance Abuse & Mental Health Services Administration, 2012). Improving the process, quality, and standard of health care delivery is a critical factor in mitigating the health disparity experienced by persons with serious mental illness (Rubenstein, Mittman, Yano, & Mulrow, 2000). However, these attempts to improve provider delivery of care are incomplete without also addressing corresponding “patient” factors that may impede active and effective participation in primary care encounters for these individuals. (Note: We use the term “patient,” rather than “consumer” or “client,” as a commonly used and understood term applied to the role of individuals receiving medical treatments in primary health care settings). For example, persons with serious mental illness are more likely than those without a mental illness to experience poor communication skills, inadequate access to health care information, difficulty navigating health care environments, and a lack of familiarity or confidence in taking an active role as patients in health care encounters such as discussing treatment options, shared goal setting, and shared decision making (Bartels, Mueser, & Miles, 1997; Morden et al., 2009).
The quality and nature of interactions between adults with serious mental illness and their primary care providers may be a contributing factor to their receipt of substandard care, however, the unique roles of providers and patients in such interactions are not well understood. In patient populations without mental illness, factors affecting patient engagement and the quality of doctor– patient interactions include perceived health status and needs, health literacy, patient activation, and the degree to which physicians adopt a patient-centered communication style (Chewning et al., 2012; Coulter, 2012; Street, Makoul, Arora, & Epstein, 2009). Greater patient activation has been associated with better illness self-management, more positive medication attitudes, higher overall functioning, and lower rates of substance abuse (Green et al., 2010; Salyers et al., 2009). Prior evidence demonstrates that most individuals with serious mental illness would prefer a more active role in their health care. For example, in a study of 84 individuals with serious mental illness, over 80% expressed a preference to be active participants in shared decision making (Mahone, 2008). However, primary care physicians may not know the preferences for decision making for their patients with serious mental illness or how to communicate clearly and effectively with them (Fiscella, Franks, Srinivasan, Kravitz, & Epstein, 2007; Hamann et al., 2010; Priebe et al., 2007; Van Os et al., 2004).
To address this gap, we developed a skills training intervention consisting of collaborative activation training for persons with serious mental illness and their primary care providers (CAT-PC) with the goal of improving patient activation skills and provider communication in the primary care medical encounter. This intervention focuses on helping patients understand their health concerns, the health care system, and how to play an active collaborative role in the medical encounter. In addition, primary care providers receive brief training in person-centered care and communication skills tailored for improving their interactions with their patients who have serious mental illness to prepare them to be receptive to the new skills acquired by participating in the training program. The aim of CAT-PC is to better prepare persons with serious mental illness and comorbid health conditions for their primary care encounters by identifying specific personal health goals, improving health care communication skills, and engaging them as activated participants in shared goal setting and decision making. This report provides a detailed description of the CAT-PC program and presents findings from a pilot study evaluating its feasibility and potential effectiveness.
Method
We conducted a pre-post pilot study evaluating the feasibility and potential effectiveness of the CAT-PC program through a state-funded community mental health center, a Federally Qualified Health Center, and two primary care practices in Manchester, New Hampshire. Written informed consent was obtained through procedures approved by the Committee for the Protection of Human Subjects at Dartmouth College and by Institutional Review Boards specific to each site.
Participants
Individuals with serious mental illness age 50 and older with cardiovascular risk factors were recruited from the community mental health center that were also being seen for medical care by a primary care provider at either of the two primary care practices or the Federally Qualified Health Center. We selected persons age 50 and older due to the common presence of medical comorbidity in middle-aged and older adults with serious mental illness and the need for integrated health care targeting persons at high risk for early mortality and premature nursing home placement (Aschbrenner, Cai, Grabowski, Bartels, & Mor, 2011; Bartels, 2004; Bartels & Naslund, 2013; Bartels, Pratt, Mueser, Forester, et al., in press). Primary care providers were approached to participate in the pilot program including internists, family physicians, and nurse practitioners. Providers were then asked to identify patients who met the following criteria: (a) age 50 and older; (b) a DSM–IV diagnosis of schizophrenia spectrum disorder, bipolar disorder, or major depression associated with a functional impairment of at least 12 months or longer; and (c) at least one major cardiovascular risk factor, defined as one or more of the following: heart disease, diabetes, impaired fasting glucose, hypertension, hyperlipidemia, current smoker, or overweight/obese (diagnosis or BMI > 25). We also recruited participants from referrals by clinicians at the community mental health center and then recruited their providers who were sent a copy of the provider training materials and an instructional video.
Eligible patients interested in learning more were invited to an information session. Recruitment information materials emphasized the voluntary nature of the program and explained that the decision to participate would have no impact on care received from the provider, clinic, or medical institution. A trained research interviewer conducted assessments at baseline and following the final training session. Out of a pool of approximately 300 potentially eligible participants across all three clinics, 30 patients expressed interest in the program and participated in baseline assessments. Seven patients dropped out before the program began (two were excluded because their primary care provider withdrew consent due to scheduling conflicts; four decided not to proceed due to anticipated conflicts of the classes with care needs or treatment appointments; and one was admitted to an assisted living facility before the intervention began); five did not complete the intervention; and one was admitted to a nursing home and lost to follow-up. The final study group consisted of 17 patients and 6 participating providers. We achieved a completion rate of 74%, which is consistent with a prior study of an intervention similarly targeting older adults with serious mental illness and medical comorbidity (Bartels, Pratt, Mueser, Wolfe, et al., in press).
The CAT-PC Program
Patient activation training
CAT-PC patient training consists of nine group-based 90-min sessions delivered weekly over 2 months. Groups consist of four to eight participants and can be delivered in a primary care clinic or a community-based health center. The CAT-PC program, based on a component of a comprehensive skills training and health care management intervention for older adults with serious mental illness (Bartels et al., 2004; Bartels, Pratt, Mueser, Forester, et al., in press; Mueser et al., 2010; Pratt, Bartels, Mueser, & Forester, 2008), consists of interactive educational and experience-based skills training sessions organized into six modules: (a) Basics of Heart Health, (b) Personal Health Assessment, (c) Setting Achievable Lifestyle Goals, (d) Making the Most of a Health Care Visit, (e) Communicating Effectively with Health Care Providers, and (f) Getting Help with Medical Visits from Family Members. The six modules are delivered over 9 sessions as outlined in Table 1.
Table 1.
Overview of the CAT-PC Program Curriculum
| Session | Class topics |
|---|---|
| Week 1 | Understanding Heart Health
|
| Week 2 | Personal Health Assessment
|
| Week 3 | Setting Achievable Lifestyle Goals
|
| Week 4 | Being Active in Health Care
|
| Week 5 | Preparing for a Medical Visit
|
| Week 6 | Taking an Active Role in the Medical Encounter Part I
|
| Week 7 | Taking an Active Role in the Medical Encounter Part II
|
| Week 8 | Getting Help from Family and Friends in Reaching Goals
|
| Week 9 | Course Review and Following Treatment Recommendations
|
All sessions were co-led by a PhD level social worker and two wellness peer specialists who were individuals with serious mental illness with lived experiences making positive health behavior changes and managing cardiovascular risk factors (e.g., smoking cessation, weight loss, increased physical activity) supporting participant self-efficacy, skill development, and knowledge acquisition. A leader’s manual and participant workbooks were developed for each session with input from primary care providers and individuals with serious mental illness. The two peer specialists helped to model the process of setting goals and making informed choices about healthy lifestyle change, and demonstrated role-play practice sessions for engaging in primary health care encounters. The social worker and peer support specialists also met weekly to coordinate the educational and experience-based skills training components.
The goal of the skills training sessions is to activate participants to better use health care visits by coming prepared with specific health concerns and goals, using improved health communication skills, requesting health information on treatment options, and engaging in shared decision making. Session 1 consists of a discussion of health goals and personal experiences as patients in primary care. First, the peer specialists elicit participants’ past experiences with medical visits, including barriers and facilitators to making medical appointments and their experiences talking with a doctor about health-related issues. Second, the provider–patient relationship is described as a two-way street, and participants are asked to write down a list of things that both they and their provider could do to improve future medical visits. The overall goal is to help participants’ identify successes and challenges that they have experienced in past visits, and to consider ways in which their experiences could be improved.
Sessions 2–5 address three components of patient activation for effective primary care visits: identifying and prioritizing health concerns, identifying a healthy lifestyle goal, and preparing for and actively engaging in a medical encounter. During the second session, each participant completes an online personal health assessment using the How’s Your Health Web-based survey (Wasson, 2005). After answering basic health-related questions, the participant receives a summary of their identified health concerns and health care needs and a list of sources of additional information specific to his or her health situation. Peer co-leaders help participants use the online survey to prioritize the health concerns that they will share with their primary care provider during a future visit. During Session 3, the focus shifts to setting achievable lifestyle goals using material adapted from the National Alliance on Mental Illness (NAMI) Hearts and Minds curriculum (Burland & Nemec, 2007). The curriculum includes information about major preventable health risk factors for persons with mental illness (e.g., obesity, diabetes, high blood pressure), and modifying health behaviors (e.g., healthy eating, exercise, smoking cessation) to decrease these risks. During this session, peer co-leaders share stories about their own successes in achieving healthy lifestyle behaviors, including how they were able to overcome challenges toward meeting their health goals. The session closes with homework instructions for participants to identify a health goal using a goal setting tip sheet designed to help them break down components of effective goal setting (e.g., attainable, specific, time-limited, positive).
Sessions 4 and 5 introduce skill building for the medical encounter in role play sessions and by providing a step-by-step guide to actively engaging in the encounter. During Session 4, participants review effective steps to making and preparing for a medical visit (e.g., organizing medication lists, writing down health concerns, planning transportation), and role play calling the primary care office to make an appointment. During Session 5, each of the patient activation components discussed in prior sessions are combined and illustrated in a 20-min video featuring a simulated primary care encounter with an activated patient with serious mental illness. The video was scripted by the study authors, and narrated by an individual with serious mental illness who shares his lived experiences of feeling underprepared, frustrated, and confused during medical visits. Actors assume the roles of a person with serious mental illness and a primary care physician and demonstrate skills and strategies highlighted in the CAT-PC program aimed at becoming a fully engaged and activated participant in primary health care encounters. The intent of the video is to bring CAT-PC content and concepts to life by illustrating how a primary care visit can be transformed into a shared, collaborative, and person-centered encounter by an activated patient and an informed provider.
Sessions 6 and 7 concentrate on acquiring patient activation skills through group discussions, practice exercises, and role play simulations. By participating in these activities, participants specifically learn to: (a) share health concerns, (b) ask questions, (c) express treatment preferences, and (d) share health goals with a primary care provider during a medical visit. Participants are given the option to use their own personal health concern or goal in the role play scenario or select one from a scripted case scenario. The two peer specialists facilitate role play practice in groups of two to four to maximize opportunities for sharing and to reduce the pressure on each individual.
Session 8 focuses on the use of social support for medical care visits. Strategies are taught for involving family members in goal setting and navigating medical encounters, and participants are encouraged to invite a family member or significant other to attend this session. The interactive session also covers the ways that family members can support each other’s health goals through practical support, shared health goals, and positive communication. Finally, Session 9 includes a review of the overall CAT-PC program and a discussion of strategies for following through with treatment recommendations and health behavior change goals.
Provider training
The provider component consists of a brief training session that prepares primary care providers to be receptive to the new skills that their patients will acquire through the CAT-PC program, and provides guidelines for cardiovascular disease prevention and treatment addressing specific pharmacological, behavioral, and communication challenges associated with serious mental illness. The aim of the training is to improve provider knowledge, patient-centered communication skills, and collaborative goal setting. The training is primarily video-based and includes a handout containing guidelines for evidence-based screening, monitoring, and management of cardiovascular risk. The training video details approaches for facilitating the medical encounter for individuals with serious mental illness. It is narrated by a physician who is board certified in internal medicine and psychiatry, and features a patient with serious mental illness who describes the challenge mental illness symptoms present for the medical encounter and shares his personal experiences of improvement in patient activation as a result of the CAT-PC program. Providers in the first cohort participated in a 45-min in-person training facilitated by a physician researcher. In response to requests to have the physician training easily fit into busy primary care schedules, providers in the second and third cohorts were mailed the training video and handout to view at their convenience.
Study Measures
Feasibility was evaluated using process measures including patient and physician recruitment success rates, participant attendance, and completion rates of assessment measures. Patient activation skills were assessed using self-report measures as well as performance-based assessments.
Self-report measures
The Patient Activation Measure (PAM) short form is a 13-item measure of patient knowledge, skills, and confidence for managing one’s own health care (Hibbard, Stockard, Mahoney, & Tusler, 2004). Each item asks patients to rate their level of agreement or disagreement with such statements as, “I am confident that I can tell a doctor my concerns, even when he or she does not ask” on a 5-point Likert scale, ranging from 1 (disagree strongly) to 5 (agree strongly). This is converted into a 0–100 scale assigned to one of four categories of progressively greater stages of activation: (a) acquiring the belief that an active role is important, (b) acquiring knowledge and confidence needed to assume an active role, (c) engaged in taking action, and (d) maintaining active role over time and under challenging circumstances.
The short-form Perceived Efficacy in Patient-Physician Interactions Scale (PEPPI) is a 5-item measure of patients’ perceived efficacy in communicating questions, concerns, preferences, and values to providers, and obtaining desired health care information (ten Klooster et al., 2012). Each question is answered on a 10-point Likert scale, ranging from 1 (not at all confident) to 10 (extremely confident). The five items are summed for a total score between 10 (lowest perceived efficacy) to 50 (highest possible perceived efficacy).
The Autonomy Preference Index (API) is a 14-item measure of patients’ self-reported preferences for health care decision making and information seeking (Ende, Kazis, Ash, & Moskowitz, 1989). The decision making subscale consists of 6-items assessing patients’ preferences for making medical decisions (e.g., “The important medical decisions should be made by your doctor, not by you;” “You should feel free to make decisions about everyday medical problems”), whereas the 8-item information-seeking component assesses patients’ desire for medical information (e.g., “When there is more than one method to treat a problem, you should be told about each one”). Scores range from 0–100, with higher scores indicating stronger preferences for participation.
Performance-based assessments
We used a version of the Social Skills Performance Assessment (SSPA) role-play test (Patterson, Moscona, McKibbin, Davidson, & Jeste, 2001) adapted to assess communication skills of people with serious mental illness with primary care providers as a standardized measure of communication skills (Pratt et al., 2007). Participants receive instructions about the role-play tasks and then read descriptions of two specific medical care scenarios in which they are asked to demonstrate communication skills such as describing symptoms, requesting clarification, discussing treatment options, and negotiating a shared plan. The role-plays are audiotaped for scoring and rated by an independent researcher on anchored 5-point Likert scales, ranging from 1 (low) to 5 (high), on demonstration of health communication skills (i.e., ability to report symptoms, ask for treatment options, report medication side effects, and negotiate medication decisions); level of motivation and engagement; fluency or flow of conversation; clarity of content and flow of speech; focus; expression of affect; and overall performance. The SSPA for communicating with doctors in medical care encounters has demonstrated good interrater and test–retest reliability (Pratt et al., 2007).
Participant Experiences and Satisfaction Questionnaire
This questionnaire was created to obtain ratings and qualitative reports from participants on their experiences and satisfaction with the CAT-PC program and recommendations for future improvements. The questionnaire consists of nine items, including six questions rated with a 5-point Likert scale assessing patient experiences and satisfaction including perceived usefulness of program materials and skills training activities, program convenience, and overall satisfaction with the program. In addition, four open-ended questions were used to gather information on what participants liked most and least about the program and to obtain specific recommendations for improving the program. The questionnaire was administered by telephone within 1-month post-intervention. Open-ended responses were examined for recurring themes representative of the participant’s viewpoints and recommendations for future improvements.
Fidelity Assessment
The research team monitored program fidelity through weekly supervision and protocol review sessions including the principal investigator, co-investigators, and program facilitators. In addition, the principal investigator observed at least one session during the course of the program and provided feedback to program facilitators. Ongoing review of program sessions throughout the study period revealed both the strengths and weaknesses of protocol design and treatment delivery. This pilot work will form the basis for subsequently modifying the design of the CAT-PC program for a larger clinical trial.
Statistical Analyses
Pre-post outcomes were analyzed using two-tailed t tests. Pre-post effect sizes were computed using Cohen’s d, and the following thresholds, defined by Cohen (1988), were used to determine whether an effect size was small (.20), moderate (.50), or large (.80; Cohen, 1988). A p < .05 was used to define significance. SPSS version 19.0 was used for all statistical analyses.
Results
Participant characteristics are listed in Table 2. There were N = 17 participants enrolled in the study who began the intervention following the introductory session, all of whom attended five or more sessions over the 9-week period. Over half of the participants had schizophrenia-spectrum disorders and the most common co-morbid health conditions were hypertension and diabetes.
Table 2.
Demographic Characteristics of the CAT-PC Program Participants
| Total sample (N = 17) |
||
|---|---|---|
| Characteristics | N | % |
| Age (M ± SD) | 58.5 ± 4.8 | |
| Gender | ||
| Female | 9 | 53 |
| Male | 8 | 47 |
| Ethnicity | ||
| White | 17 | 100 |
| Non-White | 0 | 0 |
| Marital status | ||
| Never married | 3 | 18 |
| Married | 14 | 82 |
| Education | ||
| High school graduate | 15 | 88 |
| Less than high school | 2 | 12 |
| Residential | ||
| Living independently | 14 | 82 |
| Supervised/supported housing | 3 | 18 |
| Medical diagnosis | ||
| Hypertension | 9 | 53 |
| Diabetes | 8 | 47 |
| COPD | 2 | 12 |
| Stroke | 2 | 12 |
| Asthma | 4 | 24 |
| Psychiatric diagnosis | ||
| Schizoaffective | 3 | 18 |
| Schizophrenia | 7 | 41 |
| Depression | 3 | 18 |
| Bipolar | 4 | 24 |
Patient Activation Outcomes
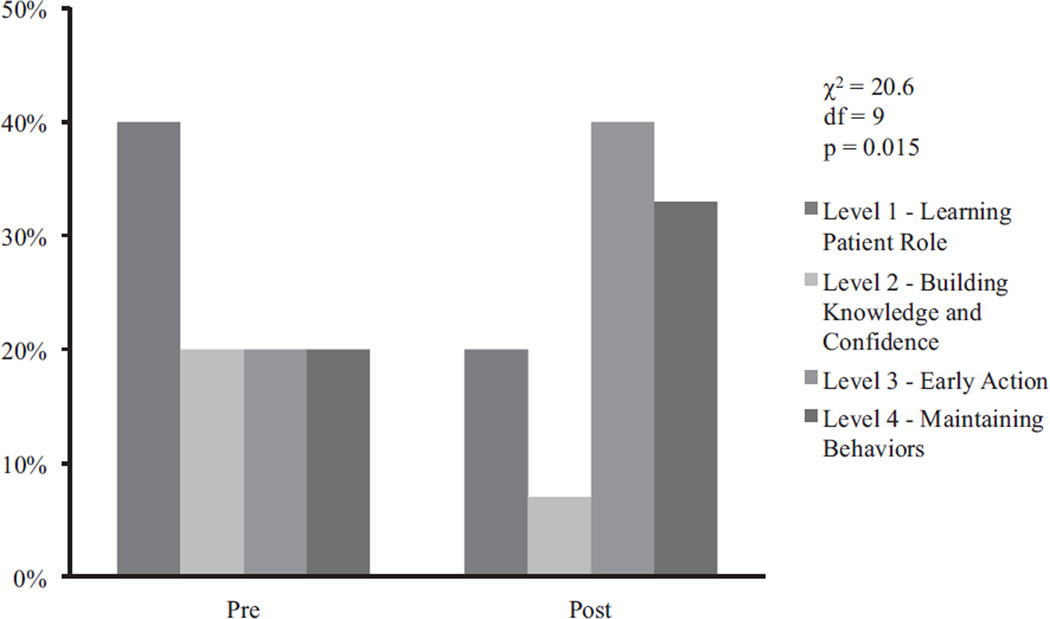
Table 3 summarizes participant outcomes with respect to activation, self-efficacy, and preference for autonomy in health care decision making. Significant pre-post improvement was found for the PAM with a medium effect size. We also evaluated activation with respect to clinically significant categorical levels of patient activation (see Figure 1). The proportion of participants reporting activated behaviors in clinical encounters (early action or maintenance) increased from 35% (N = 6) at baseline to 71% (N = 12) post-intervention. A trend was observed for improved self-efficacy in interacting with primary care physicians as measured by the PEPPI, with similar medium effect sizes.
Table 3.
Pre- and Post-CAT-PC Self-Reported and Performance-Based Outcome Measures
| Pre-intervention |
Post- intervention |
||||||
|---|---|---|---|---|---|---|---|
| Measure | M | SD | M | SD | ES | t | p |
| Perceived skills | |||||||
| Patient activation | 53.5 | 12.9 | 60.2 | 12.8 | 0.54 | 2.3 | 0.03 |
| Patient Activation Measure (PAM)a | |||||||
| Self-efficacy | 37.9 | 11.2 | 42.8 | 6.8 | 0.55 | 1.8 | 0.08 |
| Perceived Efficacy in Patient-Physician Interactions (PEPPI)b | |||||||
| Personal preference | |||||||
| Preference for decision making | 46.9 | 12.2 | 46.4 | 10.2 | 0.05 | −.2 | 0.88 |
| Autonomy preference index decision-making subscalec | |||||||
| Preference for information | 77.0 | 9.0 | 80.1 | 11.5 | 0.15 | 1.1 | 0.28 |
| Autonomy preference index information-seeking subscaled | |||||||
| Performance-based measures | |||||||
| Social Skills Performance Assessment (SSPA)e | |||||||
| Communication tasks | |||||||
| Interest | 3.7 | 1.1 | 4.0 | 1.1 | 0.28 | 1.67 | 0.12 |
| Fluency | 4.4 | 0.6 | 4.6 | 0.7 | 0.17 | 0.59 | 0.57 |
| Clarity | 4.6 | 0.7 | 4.7 | 0.4 | 0.27 | 0.94 | 0.36 |
| Focus | 4.0 | 1.1 | 4.5 | 0.6 | 0.58 | 2.1 | 0.06 |
| Social appropriateness | 4.8 | 0.5 | 5.0 | 0.0 | 0.67 | 1.7 | 0.11 |
| Overall communication performance | 4.3 | 0.4 | 4.5 | 0.4 | 0.66 | 2.8 | 0.02 |
| Medical tasks | |||||||
| Reporting physical symptoms | 2.9 | 1.1 | 3.5 | 1.1 | 0.61 | 1.6 | 0.14 |
| Asking for treatment options | 3.2 | 1.0 | 3.7 | 0.7 | 0.60 | 1.6 | 0.13 |
| Reporting medical side effects | 3.0 | 1.2 | 3.2 | 0.7 | 0.23 | 0.7 | 0.51 |
| Negotiating medical decisions | 3.1 | 1.3 | 3.6 | 1.1 | 0.37 | 1.1 | 0.29 |
| Overall medical performance | 3.1 | 0.9 | 3.5 | 0.7 | 0.56 | 1.5 | 0.15 |
PAM is a measure of patient activation, with scores ranging from 0 to 100, with 100 representing highest possible patient activation.
PEPPI is a measure of perceived efficacy in medical encounters, with scores ranging from 0 to 100, with 100 representing maximum perceived efficacy.
The autonomy preference index (API) decision-making subscale represents preferred role in the medical encounter. Scores range from 0 (maximal passive role) to 100 (dominant role), with 50 representing a patient’s desire for shared control with the physician.
The autonomy preference index (API) information-seeking subscale measures patients’ desire for medical information, with scores ranging from 0 to 100, with 100 representing a patient’s desire for maximal information in all medical situations.
Social Skills Performance Assessment assesses communication skills of people with serious mental illness in primary care encounters. Scores for each communication or medical task ranges from 1 (worst possible performance) to 5 (best possible performance).
Figure 1.
Pre-post categorical activation outcomes of the Patient Activation Measure (PAM).
No pre-post differences were observed with respect to mean preference scores for autonomous decision making or in information seeking as measured by the API. The proportion of participants describing a preference for a more collaborative role with their physicians increased from 53% (N = 9) to 71% (N = 12) following participation in the program, though this change was not statistically significant. We also assessed performance in simulated tests of communication skills with primary care providers. Table 3 shows improvements in overall performance on the SSPA, with a trend observed for improved focus.
Patient Experiences and Satisfaction
The mean scores for satisfaction on the Patient Experiences and Satisfaction Questionnaire were 4.55 (SD = 0.69), indicating a high level of overall program satisfaction. Results for each item are presented in Table 4. Selected quotes and overall descriptive themes from the open-ended questions exploring patient satisfaction and recommendations for future improvements are listed in Table 5. Participants reported that they most liked the patient activation skills training and health education component of the program, and least liked its brief duration and long training sessions. Participants also desired more individual feedback on their patient activation skills to confirm that they were using skills effectively both during role-play sessions and in actual medical visits with a primary care provider. Finally, participants recommended that the program include more peer models of successful weight loss, and additional education and guidance on health behavior change and how to share health goals with a doctor.
Table 4.
Responses to the Participant Experiences and Satisfaction Questionnaire
| Survey questions | M | SD |
|---|---|---|
| How much progress did you make toward your goals?a | 3.64 | 0.92 |
| How useful were the training materials used in the program?b | 3.91 | 1.22 |
| How helpful did you find the role play practice in the program?c | 3.73 | 1.35 |
| How convenient was it for you to participate in this program?d | 4.73 | 0.65 |
| Overall, how satisfied were you with the program?e | 4.55 | 0.69 |
| Would you recommend this program to other people?f | 2.91 | 0.30 |
Scores ranged from 1 (None at all) to 5 (A great deal).
Scores ranged from 1 (Not at all useful) to 5 (Extremely useful).
Scores ranged from 1 (Not at all helpful) to 5 (Extremely helpful).
Scores ranged from 1 (Not at all convenient) to 5 (Extremely convenient).
Scores ranged from 1 (Not at all satisfied) to 5 (Extremely satisfied).
Possible scores were 1 (No), 2 (Maybe), and 3 (Yes).
Table 5.
Selected Quotes and Overall Descriptive Themes Representing Patient Satisfaction and Recommendations for Future Improvements
| Domains | Descriptive themes | Selected quotes |
|---|---|---|
| Favorite aspect | Patient activation skills training | “It gave me the encouragement to talk to my doctor and not just sit there and listen.” “I liked how it taught us how to talk to our doctors and how you can ask your doctor for help. And I got to meet new people. Went at a good pace. I was never bored.” “The role-playing. I found it very interesting and fun.” |
| Health education | “Learning about food journals and health goals. Making an attempt to follow-through for my doctor’s appointments.” “It helped to understand myself and my illness.” |
|
| Least favorite aspect | Brief duration | “Wish it was longer [than nine sessions]. Too much information crammed into sessions. I wanted to talk more on each subject.” “I wish it was a longer program.” |
| Length of training sessions | “The 90 min was a little too long for me. Hard to concentrate with my meds.” “It was hard to remember everything from a 90-min jam-packed session. Can’t retain that much information.” |
|
| Not enough feedback | “The role-plays. I was never sure if I was doing them right.” “I wish there was someone I could talk to after I go to my doctor’s appointment to see how much I’ve improved since the first one.” |
|
| Recommended future improvements | Peer modeling Health behavior change |
“To see videos of or meet more successful people. I found them inspiring.” “More ideas on how to lose weight. Simpler ideas ‘choose this food instead of this food.’” “Give me more ideas to bring to my doctor.” |
Discussion
This pilot study demonstrated that a nine-session, peer co-led, patient activation program for primary care encounters (CAT-PC) was associated with significant improvement in patient activation for persons with serious mental illness. In addition, CAT-PC was associated with significant improvement in patient communication skills in simulated tests of performance in primary medical encounters. These findings, despite the small sample size, provide preliminary evidence that a brief intervention designed to improve patient participation in primary care medical encounters is not only feasible, but holds promise toward potentially achieving greater patient activation and improving communication skills within this high-risk group.
These results also highlight the potential for the CAT-PC program to contribute to efforts aimed at improving the quality of health care for persons with serious mental illness who have high rates of medical comorbidity. To date, interventions aimed at improving primary health care for these individuals have largely concentrated on improving provider behaviors in the delivery of care, including the creation of integrated “medical homes” focused on increasing screening, treatment, and health care coordination for common chronic health conditions (Alakeson, Frank, & Katz, 2010). CAT-PC complements these efforts by focusing on the reciprocal goal of improving patient engagement and activation in the clinical encounter. Engaging “patients” as full participants in health care encounters reflects a growing awareness of the critical role of shared goal setting (Schulman-Green, Naik, Bradley, Mc-Corkle, & Bogardus, 2006), shared decision making (Stiggelbout et al., 2012), and behavioral activation for self-management (Hibbard & Greene, 2013).
A growing literature supports patient activation as a key factor for achieving effective and efficient health care (Hibbard, Mahoney, Stock, & Tusler, 2007). In studies of persons without mental illness, greater patient activation (as measured by the PAM) has been associated with increased engagement in positive health behaviors, improved health outcomes, and lower health care costs (Hibbard & Green, 2013). For example, higher PAM scores (in general population samples) have been associated with greater participation in aerobic exercise and physical activity, increased fruit and vegetable consumption, lower rates of smoking and obesity, and improved subjective health and mental health status (Fowles, Terry, Xi, Hibbard, Bloom, & Harvey, 2009; Hibbard et al., 2007). In health care encounters, increased activation has contributed to a greater likelihood of having breast cancer screening, hemoglobin A1c monitoring, or blood lipid profiles, as well as having important health indicators within the normal range (e.g., blood glucose, HDL “good cholesterol,” triglycerides; Greene & Hibbard, 2012). For psychiatric care visits, greater health knowledge, better illness self-management skills, greater confidence in self-managing illness and greater confidence navigating the health care system have been attributed to fewer emergency department visits and acute hospitalizations (Salyers, Rollins, Clendenning, McGuire, & Kim, 2011). However, improving patient activation in primary care visits has not been addressed for individuals with serious mental illness.
Our finding of a trend for improved perceived self-efficacy in patient–physician interactions may also suggest the potential for better health outcomes for persons with serious mental illness participating in patient activation training. For example, higher self-efficacy among older adults has been associated with greater satisfaction with physician care and communication (Maly, Frank, Marshall, DiMatteo, & Reuben, 1998). High self-efficacy has been identified as a predictor of self-reported health status across a range of chronic health conditions and age groups (Grembowski et al., 1993; Kaplan, Ries, Prewitt, & Eakin, 1994; Riazi, Thompson, & Hobart, 2004).
CAT-PC builds on our earlier work to enhance self-management skills in persons with serious mental illness. We consider information, skills training, and goal setting exercises to be critical elements for a patient activation intervention to successfully augment the patient’s voice within the clinical encounter. The approach illustrated in this pilot study aligns closely with over three decades of research in individuals without mental illness on strategies to improve patient engagement and activation. A review of these interventions found that promising approaches consisted of patient coaching, feedback of patient-reported outcome measures, and communication skills training for providers (Haywood, Marshall, & Fitzpatrick, 2006). Although many interventions described in the review consisted of single sessions delivered just prior to the clinical consultation, we intentionally developed a 9-week training course, given the unique challenges of our target population. Although we demonstrated the potential effectiveness of our intervention, we recognize the practical tension between the more intensive nature of our method and the need for brief and scalable approaches.
Based on results from our satisfaction questionnaire, there was a high level of satisfaction with the program, but there were also recommendations for program improvement. Participants desired a longer program with respect to the number of sessions, though they indicated that individual sessions should be shorter in duration. Future modifications to the program should include brief training sessions incorporating frequent breaks and energizing activities that can help older adults with serious mental illness stay focused and engaged. Participants also recommended that the program include more peer models of successful weight loss, and additional guidance on health behavior change and how to share health goals with a doctor. Participants’ desire to hear additional weight loss success stories from older adults with serious mental illness underscores the potential value of “lived experience” and peer modeling of successful health behavior change.
Despite the promising nature of these results, there are a number of limitations that warrant consideration. First, the study was not powered to detect statistically significant changes due to the small sample size, and the use of a pre-post design prohibits any inference of program effectiveness due to the lack of a comparison group. Consistent with the intent of a pilot study, our goal was to examine feasibility and potential effectiveness. A determination of effectiveness will require a larger and appropriately selected sample, ideally employing a randomized controlled study design. Second, the intervention initially included a brief in-person training of the primary care physicians, potentially limiting the generalizability of CAT-PC due to the practical challenges of busy physician schedules. We subsequently addressed this concern by sending a training video and handout for providers to view at their convenience; however, we are not able to confirm if providers participated in these self-guided trainings and we did not conduct pre-post assessments of provider skills. Finally, participants in our pilot study were recruited using a convenience sample of adults with serious mental illness in New Hampshire. Hence, we are unable to generalize our findings to an ethnically or racially diverse population.
Conclusions
The CAT-PC program is designed to improve the quality and outcomes of primary health care encounters for the high-risk group of middle-aged and older adults with serious mental illness with medical comorbidity by providing training in taking an active participatory role. Our results support the feasibility and potential effectiveness of a nine-session, peer co-led training program in improving engagement and activation in primary care by employing active learning strategies including discussing video demonstrations of skills, identifying personal wellness goals, and engaging in role-plays practicing health care communication skills and shared goal setting. If proven effective in a future empirical trial, CAT-PC may provide the “missing link” between efforts to improve the delivery of primary care for persons with serious mental illness in behavioral health homes and the critical ingredient of achieving a shared partnership toward pursuing better health and health care through the full participation of a prepared, engaged, informed, and activated patient.
Acknowledgments
Grant support received from the National Institute of Mental Health (Grant number: NIMH K24MH066282).
Contributor Information
Stephen J. Bartels, Geisel School of Medicine at Dartmouth and The Dartmouth Institute for Health Policy and Clinical Practice
Kelly A. Aschbrenner, Geisel School of Medicine at Dartmouth and The Dartmouth Institute for Health Policy and Clinical Practice
Stephanie A. Rolin, Geisel School of Medicine at Dartmouth
Delia Cimpean Hendrick, Geisel School of Medicine at Dartmouth.
John A. Naslund, The Dartmouth Institute for Health Policy and Clinical Practice
Marjan J. Faber, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands
References
- Alakeson V, Frank RG, Katz RE. Specialty care medical homes for people with severe, persistent mental disorders. Health Affairs. 2010;29:867–873. doi: 10.1377/hlthaff.2010.0080. [DOI] [PubMed] [Google Scholar]
- Aschbrenner KA, Cai S, Grabowski DC, Bartels SJ, Mor V. Medical comorbidity and functional status among adults with major mental illness newly admitted to nursing homes. Psychiatric Services. 2011;62:1098–1100. doi: 10.1176/appi.ps.62.9.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ. Caring for the whole person: Integrated health care for older adults with severe mental illness and medical comorbidity. Journal of the American Geriatrics Society. 2004;52:S249–S257. doi: 10.1111/j.1532-5415.2004.52601.x. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Forester B, Mueser KT, Miles KM, Dums AR, Pratt SI, White P. Enhanced skills training and health care management for older persons with severe mental illness. Community Mental Health Journal. 2004;40:75–90. doi: 10.1023/b:comh.0000015219.29172.64. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Mueser KT, Miles KM. Functional impairments in elderly patients with schizophrenia and major affective illness in the community: Social skills, living skills, and behavior problems. Behavior Therapy. 1997;28:43–63. [Google Scholar]
- Bartels SJ, Naslund JA. The underside of the silver tsunami—Older adults and mental health care. The New England Journal of Medicine. 2013;368:493–496. doi: 10.1056/NEJMp1211456. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Mueser KT, Forester BP, Wolfe R, Cather C, Feldman J. Long-term outcomes of a randomized trial of integrated skills training and preventive health care for older adults with serious mental illness. American Journal of Geriatric Psychiatry. doi: 10.1016/j.jagp.2013.04.013. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Mueser KT, Wolfe R, Santos M, Naslund JA, Riera E. Integrated psychiatric and medical illness self-management for middle-aged and older adults with serious mental illness. Psychiatric Services. doi: 10.1176/appi.ps.201300023. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burland J, Nemec P. NAMI training programs. Psychiatric Rehabilitation Journal. 2007;31:80–82. [Google Scholar]
- Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: A systematic review. Patient Education and Counseling. 2012;86:9–18. doi: 10.1016/j.pec.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum, Inc; 1988. [Google Scholar]
- Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease. 2006;3:A42. [PMC free article] [PubMed] [Google Scholar]
- Coulter A. Patient engagement-what works? Journal of Ambulatory Care Management. 2012;35:80–89. doi: 10.1097/JAC.0b013e318249e0fd. [DOI] [PubMed] [Google Scholar]
- Druss BG, Bradford WD, Rosenheck RA, Radford MJ, Krumholz HM. Quality of medical care and excess mortality in older patients with mental disorders. Archives of General Psychiatry. 2001;58:565–572. doi: 10.1001/archpsyc.58.6.565. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Medical Care. 2002;40:129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow-up of a nationally representative U.S. survey. Medical Care. 2011;49:599–604. doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients’ desire for autonomy: Decision making and information-seeking preferences among medical patients. Journal of General Internal Medicine. 1989;4:23–30. doi: 10.1007/BF02596485. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Srinivasan M, Kravitz RL, Epstein R. Ratings of physician communication by real and standardized patients. Annals of Family Medicine. 2007;5:151–158. doi: 10.1370/afm.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring self-management of patients’ and employees’ health: Further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Education and Counseling. 2009;77:116–122. doi: 10.1016/j.pec.2009.02.018. [DOI] [PubMed] [Google Scholar]
- Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Berlowitz DR. Disparities in diabetes care: Impact of mental illness. Archives of Internal Medicine. 2005;165:2631–2638. doi: 10.1001/archinte.165.22.2631. [DOI] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Polen MR, Leo MC, Hibbard JH, Tusler M. Development of the Patient Activation Measure for mental health. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37:327–333. doi: 10.1007/s10488-009-0239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. Journal of General Internal Medicine. 2012;27:520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grembowski D, Patrick D, Diehr P, Durham M, Beresford S, Kay E, Hecht J. Self-efficacy and health behavior among older adults. Journal of Health and Social Behavior. 1993;34:89–104. [PubMed] [Google Scholar]
- Hamann J, Mendel R, Schebitz M, Reiter S, Buhner M, Cohen R, Berthele A, Kissling W. Can psychiatrists and neurologists predict their patients’ participation preferences? Journal of Nervous and Mental Disease. 2010;198:309–311. doi: 10.1097/NMD.0b013e3181d6128c. [DOI] [PubMed] [Google Scholar]
- Haywood K, Marshall S, Fitzpatrick R. Patient participation in the consultation process: A structured review of intervention strategies. Patient Education and Counseling. 2006;63:12–23. doi: 10.1016/j.pec.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J. What the evidence shows about patient activation: Better health outcomes and care experiences; fewer data on costs. Health Affairs. 2013;32:207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Services Research. 2007;42:1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research. 2004;39:1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan RM, Ries AL, Prewitt LM, Eakin E. Self-efficacy expectations predict survival for patients with chronic obstructive pulmonary disease. Health Psychology. 1994;13:366–368. doi: 10.1037//0278-6133.13.4.366. [DOI] [PubMed] [Google Scholar]
- Mahone IH. Shared decision making and serious mental illness. Archives of Psychiatric Nursing. 2008;22:334–343. doi: 10.1016/j.apnu.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived Efficacy in Patient-Physician Interactions (PEPPI): validation of an instrument in older persons. Journal of the American Geriatrics Society. 1998;46:889–894. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- McIntyre RS. Introduction: Balancing the equation: Managing comorbidities in patients with severe mental illness. Journal of Clinical Psychiatry. 2009;70:4. doi: 10.4088/JCP.7075su1c.01. [DOI] [PubMed] [Google Scholar]
- Meyer JM, Stahl SM. The metabolic syndrome and schizophrenia. Acta Psychiatrica Scandinavica. 2009;119:4–14. doi: 10.1111/j.1600-0447.2008.01317.x. [DOI] [PubMed] [Google Scholar]
- Morden NE, Mistler LA, Weeks WB, Bartels SJ. Health care for patients with serious mental illness: Family medicine’s role. Journal of the American Board of Family Medicine. 2009;22:187–195. doi: 10.3122/jabfm.2009.02.080059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Pratt SI, Bartels SJ, Swain K, Forester B, Cather C, Feldman J. Randomized trial of social rehabilitation and integrated health care for older people with severe mental illness. Journal of Consulting and Clinical Psychology. 2010;78:561–573. doi: 10.1037/a0019629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, Lieberman JA. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: Data from the CATIE schizophrenia trial sample at baseline. Schizophrenia Research. 2006;86:15–22. doi: 10.1016/j.schres.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Moscona S, McKibbin CL, Davidson K, Jeste DV. Social skills performance assessment among older patients with schizophrenia. Schizophrenia Research. 2001;48:351–360. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- Pratt SI, Bartels SJ, Mueser KT, Forester B. Helping older people experience success: An integrated model of psychosocial rehabilitation and health care management for older adults with serious mental illness. American Journal of Psychiatric Rehabilitation. 2008;11:41–60. [Google Scholar]
- Pratt SI, Kelly SM, Mueser KT, Patterson TL, Goldman S, Bishop-Horton S. Reliability and validity of a performance-based measure of skills for communicating with doctors for older people with serious mental illness. Journal of Mental Health. 2007;16:569–579. [Google Scholar]
- Priebe S, McCabe R, Bullenkamp J, Hansson L, Lauber C, Martinez-Leal R, Wright DJ. Structured patient-clinician communication and 1-year outcome in community mental healthcare: Cluster randomised controlled trial. The British Journal of Psychiatry. 2007;191:420–426. doi: 10.1192/bjp.bp.107.036939. [DOI] [PubMed] [Google Scholar]
- Riazi A, Thompson A, Hobart J. Self-efficacy predicts self-reported health status in multiple sclerosis. Multiple Sclerosis. 2004;10:61–66. doi: 10.1191/1352458504ms986oa. [DOI] [PubMed] [Google Scholar]
- Rubenstein LV, Mittman BS, Yano EM, Mulrow CD. From understanding health care provider behavior to improving health care: The QUERI framework for quality improvement. Medical Care. 2000;38:I129–I141. [PubMed] [Google Scholar]
- Salyers MP, Matthias MS, Spann CL, Lydick JM, Rollins AL, Frankel RM. The role of patient activation in psychiatric visits. Psychiatric Services. 2009;60:1535–1539. doi: 10.1176/appi.ps.60.11.1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salyers MP, Rollins AL, Clendenning MD, McGuire AB, Kim E. Impact of illness management and recovery programs on hospital and emergency room use by Medicaid enrollees. Psychiatric Services. 2011;62:509–515. doi: 10.1176/appi.ps.62.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Education and Counseling. 2006;63:145–151. doi: 10.1016/j.pec.2005.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues in Mental Health Nursing. 2011;32:589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- Sokal J, Messias E, Dickerson FB, Kreyenbuhl J, Brown CH, Goldberg RW, Dixon LB. Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Disease. 2004;192:421–427. doi: 10.1097/01.nmd.0000130135.78017.96. [DOI] [PubMed] [Google Scholar]
- Stiggelbout A, Weijden T, Wit MD, Frosch D, Légaré F, Montori V, Elwyn G. Shared decision making: Really putting patients at the centre of healthcare. British Medical Journal. 2012;344:e256. doi: 10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Education and Counseling. 2009;74:295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- Substance Abuse Mental Health Services Administration. Behavioral health homes for people with mental health and substance use conditions: The core clinical features. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions; 2012. [Google Scholar]
- ten Klooster PM, Oostveen J, Zandbelt LC, Taal E, Drossaert CH, Harmsen EJ, van de Laar MA. Further validation of the 5-item Perceived Efficacy in Patient–Physician Interactions (PEPPI-5) scale in patients with osteoarthritis. Patient Education and Counseling. 2012;87:125–130. doi: 10.1016/j.pec.2011.07.017. [DOI] [PubMed] [Google Scholar]
- Van Os J, Altamura AC, Bobes J, Gerlach J, Hellewell JS, Kasper S, Robert P. Evaluation of the Two-Way Communication Checklist as a clinical intervention. Results of a multinational, randomised controlled trial. The British Journal of Psychiatry. 2004;184:79–83. doi: 10.1192/bjp.184.1.79. [DOI] [PubMed] [Google Scholar]
- Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51:458–465. doi: 10.1176/appi.psy.51.6.458. [DOI] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health. 2002;92:92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasson J. How’s your health? 2005 Retrieved from http://howsyourhealth.org/