Abstract
Objectives
To compare the surgical and pathologic outcomes utilizing two surgical approaches for fertility-sparing radical trachelectomy in patients with stage IB1 cervical cancer.
Methods
A prospectively maintained database of vaginal radical trachelectomy (VRT) and abdominal radical trachelectomy (ART) procedures was analyzed. All procedures were performed in a standardized manner by the same surgical group. Parametrial measurements were recorded from the final pathology report. Standard statistical tests were used.
Results
Between 12/2001 and 7/2007, 43 adult patients with FIGO stage IB1 cervical cancer underwent surgery with the intent to perform a fertility-sparing radical trachelectomy. VRT was attempted in 28 patients (65%) and ART in 15 patients (35%). The median measured parametrial length in the VRT group was 1.45 cm compared to 3.97 cm in the ART group, P<0.0001. None of the parametrial specimens in the VRT group contained parametrial nodes. Parametrial nodes were detected in 8 (57.3%) of the ART specimens (P=0.0002). There was no difference in histologic subtypes, lymph vascular space invasion, or median total regional lymph nodes removed in the two groups. Median blood loss was greater but not clinically significant in the ART group, and median operating time was less in the ART group. The overall complication rate was not significantly different in the two groups.
Conclusions
Using standardized techniques, radical abdominal trachelectomy provides similar surgical and pathologic outcomes with possibly a wider parametrial resection, including contiguous parametrial nodes, as compared to the radical vaginal approach.
Introduction
Cervical cancer affects women of all ages, including those in their prime childbearing years. The Centers for Disease Control and Prevention recently reported that 28% of cervical cancers diagnosed from 1988–2004 in the United States were in women between the ages of 20 and 39 (1). Meanwhile, the proportion of births to women over the age of 35 has doubled since 1980 (2). Traditionally IB1 cervical cancer has been treated with radical hysterectomy, where the uterus is removed en bloc with the parametria. While the parametria are a possible site of spread due to direct extension or lymphatic spread, cervical cancer rarely involves the fundus (3). In women with cervical cancer who have delayed childbearing, there is a strong demand for fertility-sparing surgery.
Radical trachelectomy, the removal of the uterine cervix and adjacent tissues, was originally introduced in 1987 by Dr. Daniel Dargent [4]. Radical trachelectomy has been shown to be an effective treatment for early cervical cancer associated with an acceptable live birth rate (4, 5). Radical trachelectomy can be performed abdominally or vaginally, and is coupled with an open or laparoscopic pelvic lymph node dissection.
At our institution, depending on the clinical indication, radical trachelectomy is being performed by either a vaginal or abdominal approach. We initially began performing vaginal trachelectomy with laparoscopic lymph node dissection in 2001; in 2004 we started performing abdominal trachelectomy in select patients. To our knowledge, the two techniques have not been directly compared. The goal of this study was to compare pathologic and surgical outcomes utilizing vaginal versus abdominal trachelectomy for fertility-sparing surgery in stage IB1 cervical cancer.
Materials and Methods
A prospectively maintained database of patients who were scheduled to undergo fertility-sparing radical trachelectomy was analyzed. The inclusion criteria for the study were patients 18 or older with IB1 cervical cancer undergoing fertility-sparing surgery. Seventeen patients were excluded: 15 had tumors other than stage IB1, and two patients had IB1 tumors but were under the age of 18. These two patients were 6 and 8 years old, and had undergone abdominal trachelectomy. It was felt that the measurement of their parametria, which would be expected to be less than that of their adult counterparts, might skew the results. Records were retrospectively reviewed for basic demographic information, cancer history, details of surgery and pathologic findings. Patients who underwent trachelectomy and then had hysterectomy due to positive endocervical margins on frozen-section were included in this analysis. Patients with adenosquamous histology were grouped with the adenocarcinomas.
To eliminate surgeon bias in parametrial measurements, we recorded the pathologist’s measurement of the unfixed specimen’s gross parametrial length in the final pathology report. The longest dimension in centimeters was recorded. If both right and left parametria were measurable, we recorded the measurement as the average of both sides in centimeters. If the length of the parametria was not recorded in the report, the patient’s data were not included in the calculation of median gross parametrial length.
To account for the limits of a retrospective approach, in which a number of the specimens did not have gross parametrial measurements, an expert gynecologic pathologist (KJP) reviewed all available slides from the formalin fixed paraffin embedded sections of cervical and parametrial tissue. The histologic length was measured on each slide (See Figure 1) and the median length for each patient was calculated. Two patients were excluded from this analysis because their slides were unavailable. The histologic length does not correlate to an exact size comparable to the gross measurement but rather can be used to show the relative size discrepancy between the two groups. Surgical approach, vaginal or abdominal, was at the surgeon’s discretion. In general, we elected the vaginal approach for stage IA1–IB1 lesions where the estimated tumor diameter was <2cm, the patient had adequate vaginal anatomy and was a candidate for laparoscopic lymphadenectomy. During the laparoscopic lymphadenectomy, parametrial lymph nodes may have been removed as part of the total pelvic lymphadenectomy. Abdominal trachelectomy was usually offered to patients with stage IB1 lesions with severe vaginal distortion post conization that might limit the vaginal approach or to patients with a lesion 2–4cm in diameter. The techniques for radical vaginal trachelectomy (VRT) and radical abdominal trachelectomy (ART) have been detailed in prior reports (6–8).
Figure 1.
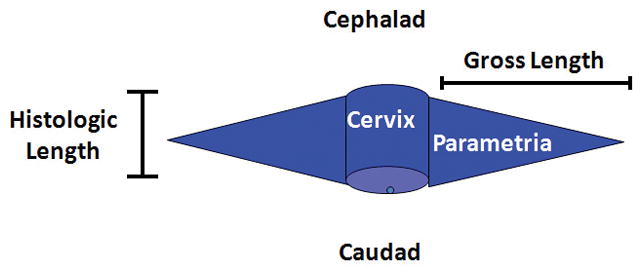
The histologic length was measured on each slide.
The pooled t test was performed for normally distributed variables and the Wilcoxan Rank sum was performed for nonparametric data. Fischer’s Exact Chi Square was used for categorical data. Statistical significance was set at P<0.05 and all tests were two–tailed.
Results
Between 12/2001 and 7/2007, 60 patients underwent an attempt at a fertility-sparing radical trachelectomy; 43 patients- those with stage IB1 disease - met the inclusion criteria for this report. VRT was attempted in 28 patients (65%) and ART in 15 patients (35%) (Table 1). The median age of VRT patients was 30 years (range, 20–40) versus 34 years (range, 30–43) in the ART group (P=0.0003). Immediate completion radical hysterectomy due to intraoperative findings was necessary in 2/28 (7%) VRT patients compared with 2/15 (13%) ART patients (P=0.6). The mean follow up interval was longer in the VRT group (24.9 v 11.6 months, P=0.0062) which was expected, as we began doing ART three years after VRT.
Table 1.
Patient Characteristics and Surgical Outcomes
| VRT (n=28) | ART (n=15) | P value | |
|---|---|---|---|
| Median Age (years) | 30 (27–32) | 34 (32–36) | 0.0003 |
| Histology: | 0.53 | ||
| Adenocarcinoma | 13 (46.6%) | 9 (60%) | |
| Squamous cell carcinoma | 15 (53.6%) | 6 (40%) | |
| Residual Disease in Specimen | 14 (50%) | 9 (60%) | 0.74 |
| Lymph vascular space invasion | 10 (35.7%) | 7 (46.7%) | 0.53 |
| Median lymph nodes obtained | 31 (21–42) | 24 (18–30) | 0.14 |
| Conversion to hysterectomy | 2 (7.1%) | 2 (13.3%) | 0.6 |
| Median estimated blood loss (mL) | 100 (56–200) | 300 (100–350) | 0.001 |
| Median operating time (minutes) | 363 (310–398) | 319 (298–338) | 0.01 |
| Complications (# patients) | 12 | 2 | 0.09 |
| Median hospital stay (days) | 3 (3–5) | 4 (3–5) | 0.35 |
| Median follow up interval (months) | 24.9 (12.7–31.2) | 11.6 (2.7–18.2) | 0.006 |
| Radiation or chemoradiation | 5 (17.9%) | 7 (46.7%) | 0.07 |
Results reported as n (%) or n (25%ile – 75%ile). VRT, vaginal radical trachelectomy; ART, abdominal radical trachelectomy.
In those patients with measurable parametria, the median gross length in the VRT group was 1.45 cm (Figure 2) compared with 3.97 cm in the ART group (Figure 3), P<0.0001 (Table 2). The median histologic length was 1.07 cm (0.89–1.25) in the VRT group, as compared to 1.51 cm (1.36–1.77) in the ART group (P ≤ 0.0001). None of the parametrial specimens in the VRT group included parametrial nodes, whereas 8 (57.3%) of the ART specimens had at least one parametrial node detected (P=0.0002), and in one case it was the only positive node. There was no difference in histologic subtypes, lymph vascular space invasion, or median total regional lymph nodes removed in the VRT versus the ART group (Table 1).
Figure 2.

Unfixed specimen of vaginal radical trachelectomy demonstrating the endocervical margin and 1–2 cm of parametrial tissue continuos with the cervix.
Figure 3.

Unfixed specimen of abdominal radical trachelectomy demonstrating vaginal margin and at least 4cm of parametrial tissue continuous with the cervix.
Table 2.
Pathologic Results of the unfixed trachelectomy specimens with bilateral parametrial measurements by the pathologist
| VRT (n=28) | ART (n=15) | P value | |
|---|---|---|---|
| Median Gross Length (cm) | 1.45 (0.73–1.63) | 3.97 (2.7–5.36) | 0.01 |
| Median Histologic Length (cm) | 1.07 (0.89–1.25) | 1.51 (1.36–1.77) | ≤ 0.0001 |
| Patients with parametrial lymph nodes detected | 0 (0%) | 8 (57.3%) | 0.0002 |
Results reported as n (%) or n (25%ile – 75%ile). VRT, vaginal radical trachelectomy; ART, abdominal radical trachelectomy. 27 VRT & 11 ART patients had slides available. 5 VRT & 12 ART patients had gross parametrial measurements recorded in the pathology report.
Median operating time was greater in the VRT group, 369 min v 319 min (P=0.01). (Table 1.). On average patients stayed in the hospital until post-op day 2 in the VRT group and 3 in the ART group (P=0.34). The number of patients who had complications was not significantly different in the two groups (VRT 12 [42.9%], ART 2 [13.3%], P=0.09). Some patients had more than one complication. In the VRT group there were 3 patients with lower extremity or vulvar edema, 2 with urinary tract infections, 2 with creatinine elevations which resolved, and one with mild transient hydronephrosis. There were 4 VRT patients with bleeding complications: 2 had vaginal bleeding, 1 had an abdominal wall hematoma requiring a transfusion, and 1 had delayed hemorrhage requiring a hysterectomy. Lymphocysts or abscesses requiring drainage were seen in 2 VRT patients and 1 ART patient, and there was one ART patient readmitted for nausea which resolved with observation.”
Radiation or chemoradiation was given to 5 patients in the VRT group and 7 in the ART group (P=0.07). The therapy was adjuvant in all patients except one woman in the VRT group who did not initially receive adjuvant therapy, and was eventually administered chemoradiation for a central recurrence. In the ART group, adjuvant therapy was prompted by a positive endocervical margin (1 patient), a close margin on the trachelectomy specimen (1 patient), and positive lymph node(s) in five patients, including one with a positive parametrial node. In the VRT group, adjuvant therapy was given for a close margin on the trachelectomy specimen in 2 patients and for parametrial spread in 2 patients. All patients who did not undergo completion hysterectomy or receive adjuvant postoperative radiation resumed normal menstruation within 8 weeks from trachelectomy. Some patients did develop cervical stenosis, which was a late complication remedied usually by office outpatient dilation under local anesthesia.
Discussion
We have demonstrated that with the use of standard radical techniques, the size of the parametrial specimen obtained with ART is more than 50% greater than that obtained with VRT when either is performed for Stage IB1 cervical cancer. In ART the uterine arteries are ligated at their point of origin, which correlates to a Class III radical hysterectomy (9). The VRT we perform is analogous to the Schauta-Stoeckel radical vaginal hysterectomy (10), where only the cervicovaginal branch of the uterine artery is ligated, and clamps are placed approximately 2 cm lateral to the vaginal cuff. In our experience, the VRT cervical specimen correlates to a Class II radical abdominal hysterectomy as described by Piver, Rutledge and Smith (9). Studies thus far of trachelectomy have been in patients who have undergone VRT, which has been shown to be a safe and effective treatment in patients with lesions <2cm in diameter (4, 5, 11). The larger parametrial specimen yielded by the ART could have important clinical implications.
Parametrial removal in early cervical cancer has been debated but remains important for several reasons including: 1) to rule out parametrial spread, which would be an indication for further therapy, 2) to prevent local recurrence and 3) to obtain a clear margin on the cervical primary. In our study, 9% of all patients had parametrial involvement, including 2 patients with positive parametrial lymph nodes. These findings are consistent with the literature, where parametrial involvement in IB1 tumors ranges from 6–31% (12–15). Factors which potentially correlate with parametrial tumor spread at the time of radical hysterectomy include lymph node status, size of tumor, deep stromal invasion (12, 13), stage, lymph vascular space invasion, grade (12) (14), histology, and presence of residual tumor in the surgical specimen (14). Patients with cervical cancer that has spread to the parametria require adjuvant chemoradiation, and therefore lose the benefit of the “fertility-sparing” aspect of the surgery.
In our population 12 patients (28%) required radiation or chemoradiation therapy (Table 1). Unfortunately, most of the characteristics that increase the risk of spread (deep stromal invasion and vascular invasion) may not be determined reliably pre-operatively. Other characteristics are subjective, like tumor size. Estimation of lesion size is further complicated at referral centers where a patient has often undergone conization prior to presentation for definitive treatment, which was why we were unable to account for lesion size in this study.
ART could possibly provide a fertility-sparing option for patients with larger tumors, as long as patients were counseled as to the risks and benefits. In patients who require chemoradiation after surgery, there may be an increased risk of complications as compared to either modality alone (16, 17). ART is potentially beneficial for patients with larger tumors (2–4cm) and no spread to the parametria or lymph nodes at the time of trachelectomy. In those patients, removing a larger parametrial specimen would provide more comprehensive pathologic evaluation and could potentially prevent recurrences in the parametria. Previous studies have demonstrated that lymph nodes are scattered throughout the parametria, (15, 18). In our study, parametrial nodes continuous with the trachelectomy specimen were only obtained in patients who underwent ART, and in one patient, the parametrial node was the only positive node. The risk of lymph node metastases is higher in patients with larger tumors, and ART may allow for a more complete lymph node dissection in those patients (19).
The strength of this study is that it is the first to our knowledge that compares the pathologist’s measurement of the specimen obtained at VRT and ART. Also, both procedures were performed at the same institution, by the same surgeons. More information could have been gathered if the parametria were measured prospectively for comparison. The larger percentage of grossly measurable specimens in the ART group (80% versus 17.9%) indicates that the parametria were more easily identified in that group, likely due to their size (Figures 2–3). As surgeons tended to do ART for larger tumors, it is possible that the findings of this study are reflective of the surgeon’s decision to do a more radical excision for larger tumors rather than an indication that ART yields a larger specimen than VRT. However, it is more likely that ART were done for larger tumors due to anecdotal observations by the surgeon that the procedure yielded a larger specimen—the same observations which prompted our decision to formally study this topic. The study results could be biased by the number of patients without grossly parametrial measurements, which is why we conducted an additional analysis to confirm our results—histologic review by an expert gynecologic pathologist. There was a clear difference in the size of the parametrial specimen obtained with ART versus VRT, on both the gross and histologic analyses.
We have demonstrated a significant difference between the sizes of parametrial specimens obtained via ART vs. VRT. Further study is necessary to determine if this pathologic difference will translate into a clinical difference, specifically if ART will afford women with tumors larger than 2 cm the opportunity to benefit from fertility sparing surgery.
References
- 1.Saraiya M, Ahmed F, Krishnan S, Richards TB, Unger ER, Lawson HW. Cervical cancer incidence in a prevaccine era in the United States, 1998–2002. Obstet Gynecol. 2007 Feb;109(2 Pt 1):360–70. doi: 10.1097/01.AOG.0000254165.92653.e8. [DOI] [PubMed] [Google Scholar]
- 2.Martin JA, Kochanek KD, Strobino DM, Guyer B, MacDorman MF. Annual summary of vital statistics--2003. Pediatrics. 2005 Mar;115(3):619–34. doi: 10.1542/peds.2004-2695. [DOI] [PubMed] [Google Scholar]
- 3.Noguchi H, Shiozawa I, Kitahara T, Yamazaki T, Fukuta T. Uterine body invasion of carcinoma of the uterine cervix as seen from surgical specimens. Gynecol Oncol. 1988 Jun;30(2):173–82. doi: 10.1016/0090-8258(88)90021-2. [DOI] [PubMed] [Google Scholar]
- 4.Plante M, Renaud MC, Hoskins IA, Roy M. Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature. Gynecol Oncol. 2005 Jul;98(1):3–10. doi: 10.1016/j.ygyno.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Roman LD. Pregnancy after radical vaginal trachelectomy: maybe not such a risky undertaking after all. Gynecol Oncol. 2005 Jul;98(1):1–2. doi: 10.1016/j.ygyno.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Sonoda Y, Abu-Rustum NR. Radical vaginal trachelectomy and laparoscopic pelvic lymphadenectomy for early-stage cervical cancer in patients who desire to preserve fertility. Gynecol Oncol. 2007;104(Suppl):S50–S5. doi: 10.1016/j.ygyno.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Rustum NR, Sonoda Y, Black D, Levine DA, Chi DS, Barakat RR. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma: technique and review of the literature. Gynecol Oncol. 2006 Dec;103(3):807–13. doi: 10.1016/j.ygyno.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 8.Abu-Rustum NR, Sonoda Y. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma. Gynecol Oncol. 2007;104(Suppl):S56–S9. doi: 10.1016/j.ygyno.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 9.Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974 Aug;44(2):265–72. [PubMed] [Google Scholar]
- 10.Sonoda Y, Abu-Rustum NR. Schauta radical vaginal hysterectomy. Gynecol Oncol. 2007 Feb;104(2 Suppl 1):20–4. doi: 10.1016/j.ygyno.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 11.Dargent D, Martin X, Sacchetoni A, Mathevet P. Laparoscopic vaginal radical trachelectomy: a treatment to preserve the fertility of cervical carcinoma patients. Cancer. 2000 Apr 15;88(8):1877–82. [PubMed] [Google Scholar]
- 12.Covens A, Rosen B, Murphy J, Laframboise S, DePetrillo AD, Lickrish G, et al. How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol. 2002 Jan;84(1):145–9. doi: 10.1006/gyno.2001.6493. [DOI] [PubMed] [Google Scholar]
- 13.Steed H, Capstick V, Schepansky A, Honore L, Hiltz M, Faught W. Early cervical cancer and parametrial involvement: is it significant? Gynecol Oncol. 2006 Oct;103(1):53–7. doi: 10.1016/j.ygyno.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 14.Wright JD, Grigsby PW, Brooks R, Powell MA, Gibb RK, Gao F, et al. Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer. 2007 Sep 15;110(6):1281–6. doi: 10.1002/cncr.22899. [DOI] [PubMed] [Google Scholar]
- 15.Benedetti-Panici P, Maneschi F, D’Andrea G, Cutillo G, Rabitti C, Congiu M, et al. Early cervical carcinoma: the natural history of lymph node involvement redefined on the basis of thorough parametrectomy and giant section study. Cancer. 2000 May 15;88(10):2267–74. [PubMed] [Google Scholar]
- 16.Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib–IIa cervical cancer. Lancet. 1997 Aug 23;350(9077):535–40. doi: 10.1016/S0140-6736(97)02250-2. [DOI] [PubMed] [Google Scholar]
- 17.Bloss JD, Berman ML, Mukhererjee J, Manetta A, Emma D, Ramsanghani NS, et al. Bulky stage IB cervical carcinoma managed by primary radical hysterectomy followed by tailored radiotherapy. Gynecol Oncol. 1992 Oct;47(1):21–7. doi: 10.1016/0090-8258(92)90069-u. [DOI] [PubMed] [Google Scholar]
- 18.Girardi F, Lichtenegger W, Tamussino K, Haas J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecol Oncol. 1989 Aug;34(2):206–11. doi: 10.1016/0090-8258(89)90143-1. [DOI] [PubMed] [Google Scholar]
- 19.Marchiole P, Benchaib M, Buenerd A, Lazlo E, Dargent D, Mathevet P. Oncological safety of laparoscopic-assisted vaginal radical trachelectomy (LARVT or Dargent’s operation): a comparative study with laparoscopic-assisted vaginal radical hysterectomy (LARVH) Gynecol Oncol. 2007 Jul;106(1):132–41. doi: 10.1016/j.ygyno.2007.03.009. [DOI] [PubMed] [Google Scholar]


