Abstract
Background
The original homeostasis model assessment (HOMA1) and the updated HOMA model (HOMA2) have been used to evaluate insulin resistance (IR) and β-cell function, but little is known about the usefulness of HOMA2 for the prediction of diabetes in Koreans. The aim of this study was to demonstrate the usefulness of HOMA2 as a predictor of type 2 diabetes mellitus in Koreans without diabetes.
Methods
The study population consisted of 104,694 Koreans enrolled at a health checkup program and followed up from 2001 to 2012. Participants were divided into a normal glucose tolerance (NGT) group and a pre-diabetes group according to fasting glucose and glycosylated hemoglobin levels. Anthropometric and laboratory data were measured at the baseline checkup, and HOMA values were calculated at the baseline and follow-up checkups. The hazard ratios (HRs) of the HOMA1 and HOMA2 values and the prevalence of diabetes at follow-up were evaluated using a multivariable Cox proportional hazards model and Kaplan-Meier analysis.
Results
After adjusting for several diabetes risk factors, all of the HOMA values except 1/HOMA1-β and 1/HOMA2-β in the NGT group were significant predictors of the progression to diabetes. In the NGT group, there was no significant difference in HOMA1-IR (HR, 1.09; 95% confidence interval [CI], 1.04 to 1.14) and HOMA2-IR (HR, 1.11; 95% CI, 1.04 to 1.19). However, in the pre-diabetes group, 1/HOMA2-β was a more powerful marker (HR, 1.29; 95% CI, 1.26 to 1.31) than HOMA1-IR (HR, 1.23; 95% CI, 1.19 to 1.28) or 1/HOMA1-β (HR, 1.14; 95% CI, 1.12 to 1.16). In the non-diabetic group (NGT+pre-diabetes), 1/HOMA2-β was also a stronger predictor of diabetes (HR, 1.27; 95% CI, 1.25 to 1.29) than HOMA1-IR (HR, 1.14; 95% CI, 1.12 to 1.15) or 1/HOMA1-β (HR, 1.13; 95% CI, 1.11 to 1.14).
Conclusion
HOMA2 is more predictive than HOMA1 for the progression to diabetes in pre-diabetes or non-diabetic Koreans.
Keywords: Homeostasis model assessment 1, Homeostasis model assessment 2, Insulin resistance, Insulin secretion
INTRODUCTION
The pathophysiology of type 2 diabetes mellitus (T2DM) involves insulin resistance (IR) and β-cell dysfunction [1,2,3,4]. Accordingly, estimating IR and β-cell function is essential for screening high-risk subjects for T2DM and making a treatment plan. There are several methods for estimating IR and β-cell function, including the hyperinsulinemic euglycemic clamp, frequently sampled intravenous glucose tolerance, C-peptide to glucose ratio, and homeostasis model assessment (HOMA) model [5,6,7].
Among these, the original HOMA (HOMA1) has been broadly used due to its simplicity and cost effectiveness. Previous studies show that an increase of HOMA1-IR and a decrease of HOMA1-β are associated with an increased incidence of diabetes and future cardiovascular events in patients with T2DM [8,9]. The relationship between the HOMA value and future risk of diabetes in Korean male subjects has been examined [10]. However, the HOMA1 model is not always reliable because it does not consider the variations in the glucose resistance of the peripheral tissue and liver, increases in the insulin secretion curve for blood glucose concentrations above 180 mg/dL, and contribution of circulating pro-insulin [11,12].
An updated HOMA (HOMA2), the correctly solved computer model that considers such variations, was announced in 1998. HOMA2 was recalibrated to give steady-state β-cell function (% B) and insulin sensitivity (% S) of 100% in normal young adults when using currently available assays for insulin, specific insulin, or C-peptide [11]. HOMA2 was better than HOMA1 in predicting oral glucose tolerance test (OGTT)-based indexes of β-cell function and glucose resistance in Italians [13,14]. In addition, HOMA2 has been used to study IR and metabolic syndrome in Brazilians [15]. A study targeting people in Iraq observed a correlation between glycosylated hemoglobin (HbA1c) and HOMA2-IR [16].
Despite the diverse ethnic groups included in HOMA research, a study of the correlation between HOMA2 and HO MA1 and the development of overt diabetes has not yet been conducted in Koreans. Therefore, the aim of this study was to compare the usefulness of HOMA1 and HOMA2 for predicting progression to diabetes in Koreans.
METHODS
Study population and design
We designed a retrospective observational study of participants in a medical health checkup program at the Health Promotion Center at Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, from January 2001 to December 2012. The purpose of this medical health check-up program is to promote the health of the employees through regular health checkups and the early detection of existing disease. Most examinees are employees of Korean industrial companies and their family members.
Among the 136,158 subjects, we excluded subjects who had a history of diabetes or were taking oral hypoglycemic agents, as well as those with a fasting blood glucose ≥126 mg/dL or HbA1c ≥6.5% at the baseline checkup. In addition, subjects with missing data and pregnant subjects were excluded from the final analysis. These exclusions (n=31,464) resulted in a final study population of 104,694 subjects.
At the baseline checkup, the subjects were divided by fasting blood glucose and HbA1c levels into the normal glucose tolerance (NGT, fasting blood glucose <100 mg/dL and HbA1c <5.7%) group and the pre-diabetes (100 mg/dL≤fasting blood glucose<126 mg/dL or 5.7%≤HbA1c<6.5%) group. Collectively, all of the subjects constituted the non-diabetic group. In subsequent medical checkups, those subjects with a fasting blood glucose ≥126 mg/dL or HbA1c ≥6.5% were defined as having diabetes. The primary purpose of this study was to compare the predictive ability of HOMA1 and HOMA2 for diabetes, so we calculated the hazard ratios (HRs) of the HOMA values (i.e., HOMA1-IR, 1/HOMA1-β, HOMA2-IR, and 1/HOMA2-β). We monitored changes of the HbA1c, blood glucose, and HOMA values in each group over time. In addition, the subjects were divided into four groups based on each quartile of HOMA values, and we calculated the cumulative prevalence of diabetes in each group.
No specific informed consent was obtained. The requirement for written or verbal consent was waived by the Institutional Review Board during the planning phase of this study. Researchers were only allowed to assess the database for analysis purposes, and the database did not contain any personal identifying information.
Anthropometric and laboratory measurements
Height, weight, waist circumference, and systolic blood pressure were measured in duplicate, and the results were averaged. Systolic blood pressure was taken with a standardized sphygmomanometer after at least 5 minutes of rest, according to the hypertension detection and follow-up protocol [17]. Body mass index (BMI) was calculated by dividing the weight in kilogram by the square of the height in meters. A family history of diabetes was defined as having at least one parent or sibling with diabetes. A current smoker was defined as smoking occasionally or on a daily basis.
After 12 hours of fasting, the fasting blood glucose, total cholesterol, triglyceride, high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), and HbA1c levels were checked. The hexokinase method (Advia 1650 Autoanalyzer; Bayer Diagnostics, Leverkusen, Germany) was used to measure blood glucose levels, and an enzymatic colorimetric test was used to measure total cholesterol and triglyceride levels. The selective inhibition method was used to measure the level of HDL-C, and the homogeneous enzymatic calorimetric test was used to measure the level of LDL-C. Serum insulin concentration was measured with an immunoradiometric assay (INS-IRMA; Biosource, Nivelles, Belgium). Estimated glomerular filtration rate (eGFR) was calculated by the Modification of Diet in Renal Disease Study equation.
HOMA1-IR was defined as [fasting insulin (µU/mL)× fasting glucose (mmol/L)]/22.5. HOMA1-β was calculated using (20×fasting insulin)/(fasting glucose–3.5) [9]. HOMA2-IR and HOMA2-β data were calculated with a HOMA2 calculator released by the Diabetes Trials Unit, University of Oxford: HOMA Calculator. This calculator is available at: http://www.dtu.ox.ac.uk/homacalculator/index.php (updated January 8, 2013). HOMA1-β and HOMA2-β have a negative correlation with diabetes risk, so we took the inverse value to compare them with HOMA-IR or HOMA2-IR.
Statistical analysis
Continuous variables are presented as mean±standard deviation, and the categorical variables are presented as frequency and proportion. HOMA1 and HOMA2 were compared for independent incident diabetes development by use of HRs from multivariable Cox proportional hazards models. The Kaplan-Meier method was used to compare the cumulative prevalence of diabetes for each HOMA value quartile. All of the data were analyzed using R version 3.1.1 (http://www.R-project.org). Statistical significance was defined as P<0.05.
RESULTS
Baseline characteristics of study subjects are shown in Table 1. The median follow-up duration was 6.2 years (range, 1.5 to 15.1), and the mean subject age was 38.9±7.4 years. Our study population included 72,915 NGT subjects (69.6%) and 31,779 pre-diabetes subjects (30.4%). After follow-up, 1,939 subjects (1.9%) were newly diagnosed with T2DM. The subjects in the pre-diabetes group tended to be older, were more often male, and had higher systolic blood pressure, BMI, HbA1c, HDL-C, non-HDL-C, aspartate aminotransferase, alanine transaminase, HOMA-IR, and HOMA2-IR and lower eGFR, HO MA1-β, and HOMA2-β than the NGT group. There were statistically significant differences for all of the variables in the baseline characteristics.
Table 1. Baseline characteristics of the study participants.
| Characteristic | NGT groupa (n=72,915) | Pre-diabetes groupb (n=31,779) | Non-diabetic groupc (n=104,694) | P valued |
|---|---|---|---|---|
| Age at first visit, yr | 37.9±6.8 | 41.2±8.3 | 38.9±7.4 | <0.001 |
| BMI, kg/m2 | 23±2.9 | 24.2±3.1 | 23.4±3.0 | <0.001 |
| Waist circumference, cm | 78.6±9.4 | 82.4±9.3 | 79.8±9.5 | <0.001 |
| Female sex, % | 29,676 (40.7) | 10,996 (34.6) | 40,672 (38.8) | <0.001 |
| Family history of DM, % | 9,625 (13.2) | 5,402 (17.0) | 15,027 (14.4) | <0.001 |
| Current smoker, % | 18,885 (25.9) | 8,517 (26.8) | 27,402 (26.2) | 0.002 |
| Progression to DM, % | 313 (0.4) | 1,626 (5.1) | 1,939 (1.9) | <0.001 |
| AST, IU/L | 23.7±7.0 | 24.9±8.0 | 23.8±7.3 | <0.001 |
| ALT, IU/L | 23.8±13.2 | 27.6±15.7 | 25.0±14.1 | <0.001 |
| Serum creatinine, mg/dL | 1.01±0.15 | 1.04±0.15 | 1.02±0.15 | <0.001 |
| eGFR, mL/min | 79.4±9.1 | 77.3±9.1 | 78.8±9.2 | <0.001 |
| SBP, mm Hg | 111.5±13.0 | 116.2±14.7 | 112.9±13.7 | <0.001 |
| HbA1c, % | 5.26±0.23 | 5.61±0.32 | 5.37±0.30 | <0.001 |
| Total cholesterol, mg/dL | 186.6±31.7 | 196.3±33.4 | 189.6±32.5 | <0.001 |
| Triglyceride, mg/dL | 115.3±73.3 | 140.7±92.3 | 123.0±80.4 | <0.001 |
| LDL-C, mg/dL | 106.6±27.1 | 114.1±28.5 | 108.9±27.7 | <0.001 |
| HDL-C, mg/dL | 54.5±12.3 | 52.4±11.7 | 53.9±12.2 | <0.001 |
| Non-HDL-C, mg/dL | 132.1±32.1 | 143.9±33.4 | 135.7±32.9 | <0.001 |
| HOMA1-IR | 1.91±0.72 | 2.39±0.97 | 2.06±0.84 | <0.001 |
| HOMA1-β | 120.42±70.08 | 93.80±39.82 | 112.34±63.65 | <0.001 |
| HOMA2-IR | 1.27±0.45 | 1.46±0.55 | 1.33±0.49 | <0.001 |
| HOMA2-β | 100.09±35.51 | 93.14±31.67 | 97.98±34.54 | <0.001 |
Values are presented as mean±standard deviation or number (%).
NGT, normal glucose tolerance; BMI, body mass index; DM, diabetes mellitus; AST, aspartate aminotransferase; ALT, alanine transaminase; eGFR, estimated glomerular filtration rate; SBP, systolic blood pressure; HbA1c, glycosylated hemoglobin; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; HOMA1, original homeostasis model assessment; IR, insulin resistance; HOMA2, updated HOMA model.
aThe NGT group is with a plasma glucose <100 mg/dL at the baseline checkup, bThe pre-diabetes group is with a plasma glucose ≥100 and <126 mg/dL at the baseline checkup, cNon-diabetic group: NGT+pre-diabetes group, dNGT group vs. pre-diabetes group.
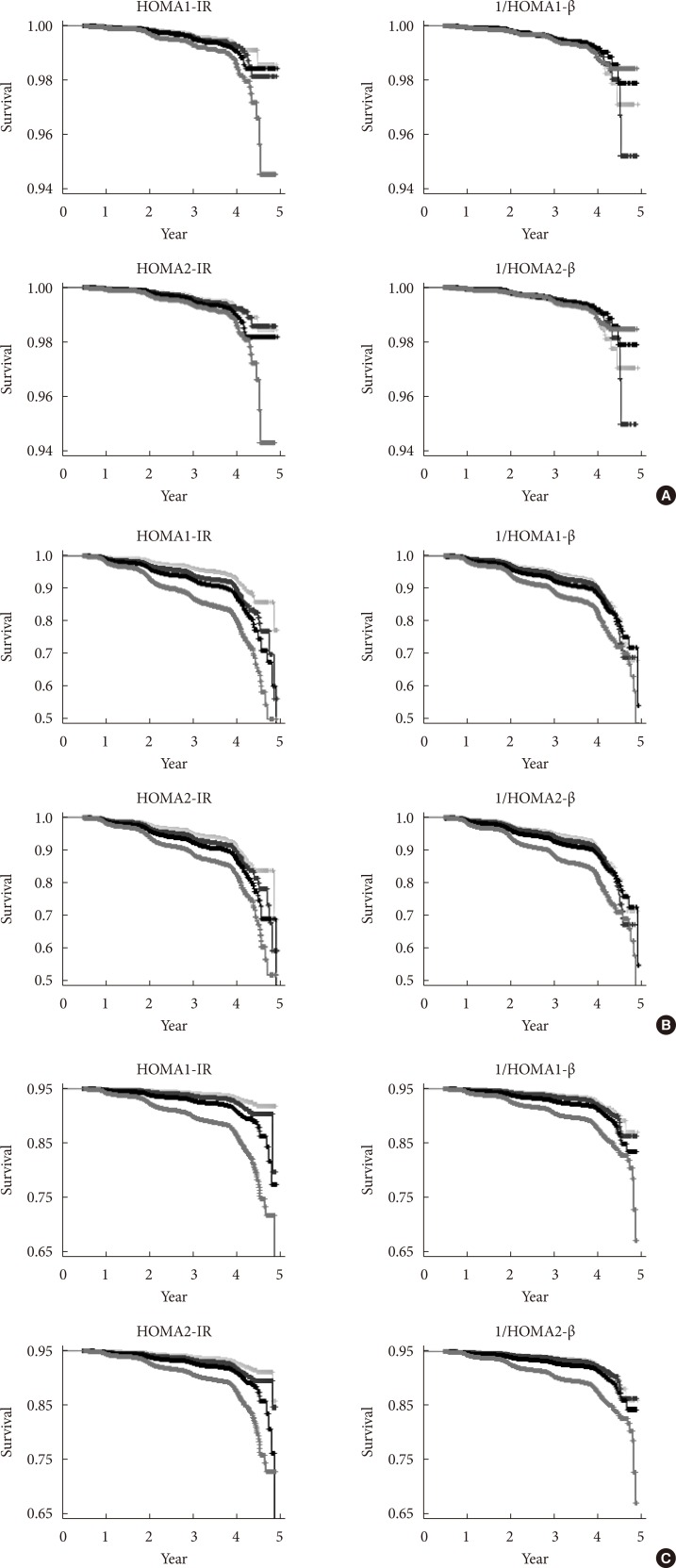
The cumulative incidence of diabetes by quartile for each HOMA value in the NGT group is shown in Fig. 1A, the pre-diabetes group is shown in Fig. 1B, and all subjects together are shown in Fig. 1C. The cumulative prevalence of diabetes tends to increase significantly along with the quartile of HOMA1 and HOMA2 except for 1/HOMA1-β and 1/HO MA2-β in the NGT group. Generally, the high HOMA-IR quartile group had a higher cumulative prevalence of diabetes at follow-up and vice versa in the HOMA-β quartile.
Fig. 1. Kaplan-Meier curves for the cumulative prevalence of type 2 diabetes mellitus for the quartile of homeostasis model assessment (HOMA) values. (A) In the normal glucose tolerance group. (B) In the pre-diabetic group. (C) In the non-diabetic group. In each figure, the 1Q group is displayed in gray, the 2Q group is displayed in blue, the 3Q group in black, and the highest quartile in red. IR, insulin resistance.
Table 2 compares the HRs for the development of diabetes based on the HOMA1 and HOMA2 estimations as the value increased by the standard deviation. In the NGT subjects, HOMA2-IR (HR, 1.18; 95% confidence interval [CI], 1.13 to 1.23; P<0.001) was more predictive than HOMA1-IR (HR, 1.13; 95% CI, 1.1 to 1.17; P<0.001), but there was no significant difference between HOMA2-IR and HOMA1-IR (P> 0.05). HOMA1-β and HOMA2-β did predict progression to diabetes. In the pre-diabetes group, HOMA1-IR (HR, 1.42; 95% CI, 1.38 to 1.46; P<0.001) was a more powerful marker than HOMA2-IR (HR, 1.33; 95% CI, 1.29 to 1.38; P<0.001) or HOMA2-β (HR, 1.26; 95% CI, 1.23 to 1.29; P<0.001). In the non-diabetic group, HOMA2-IR (HR, 1.25; 95% CI, 1.23 to 1.26; P<0.001) and HOMA2-β (HR, 1.26; 95% CI, 1.25 to 1.28; P<0.001) had stronger predictive power than the HOMA1 values.
Table 2. Univariate Cox proportional hazards analysis model of HOMA values for developing type 2 diabetes mellitus.
| Variable | NGT group | Pre-diabetes group | All participants (non-diabetic group) | |||
|---|---|---|---|---|---|---|
| HR (95% CI)a | P value | HR (95% CI)a | P value | HR (95% CI)a | P value | |
| HOMA1-IR | 1.13 (1.1–1.17) | <0.001 | 1.42 (1.38–1.46) | <0.001 | 1.21 (1.20–1.22) | <0.001 |
| 1/HOMA1-β | 0.99 (0.87–1.14) | 0.922 | 1.13 (1.11–1.15) | <0.001 | 1.12 (1.11–1.13) | <0.001 |
| HOMA2-IR | 1.18 (1.13–1.23) | <0.001 | 1.33 (1.29–1.38) | <0.001 | 1.25 (1.23–1.26) | <0.001 |
| 1/HOMA2-β | 0.95 (0.83–1.08) | 0.418 | 1.26 (1.23–1.29) | <0.001 | 1.26 (1.25–1.28) | <0.001 |
HOMA, homeostasis model assessment; NGT, normal glucose tolerance; HR, hazard ratio; CI, confidence interval; HOMA1, original HOMA; IR, insulin resistance; HOMA2, updated HOMA model.
aWhen increased by the standard deviation from the mean value of each HOMA value. Reference is the mean value of each HOMA model.
HOMA-IR values were associated with the development of T2DM independent of age, sex, BMI, family history of diabetes, smoking history, systolic blood pressure, lipid profile, and HbA1c, but there were no differences between HOMA1-IR (HR, 1.09; 95% CI, 1.04 to 1.14; P<0.001) and HOMA2-IR (HR, 1.11; 95% CI, 1.04 to 1.19; P<0.001) in the NGT group. HOMA2-β was the most significant predictive marker in both the pre-diabetic group (HR, 1.29; 95% CI, 1.26 to 1.31; P< 0.001) and the non-diabetic group (HR, 1.27; 95% CI, 1.25 to 1.29; P<0.001) (Table 3).
Table 3. Multivariatea Cox proportional hazards analysis model of HOMA values for developing type 2 diabetes mellitus.
| Variable | NGT group | Pre-diabetes group | All participants (non-diabetic group) | |||
|---|---|---|---|---|---|---|
| HR (95% CI)b | P value | HR (95% CI)b | P value | HR (95% CI)b | P value | |
| HOMA1-IR | 1.09 (1.04–1.14) | <0.001 | 1.23 (1.19–1.28) | <0.001 | 1.14 (1.12–1.15) | <0.001 |
| 1/HOMA1-β | 1.07 (0.97–1.17) | 0.177 | 1.14 (1.12–1.16) | <0.001 | 1.13 (1.11–1.14) | <0.001 |
| HOMA2-IR | 1.11 (1.04–1.19) | 0.001 | 1.13 (1.08–1.18) | <0.001 | 1.12 (1.09–1.15) | <0.001 |
| 1/HOMA2-β | 1.05 (0.93–1.20) | 0.428 | 1.29 (1.26–1.31) | <0.001 | 1.27 (1.25–1.29) | <0.001 |
HOMA, homeostasis model assessment; NGT, normal glucose tolerance; HR, hazard ratio; CI, confidence interval; HOMA1, original HOMA; IR, insulin resistance; HOMA2, updated HOMA model.
aAll estimates reflect adjustment for age, sex, body mass index, family history of diabetes, history of smoking, systolic blood pressure, glycosylated hemoglobin, triglyceride, and high density lipoprotein cholesterol, bWhen increased by the standard deviation from the mean value of each HOMA value. Reference is the mean value of each HOMA model.
DISCUSSION
In this study, after adjusting for diabetes-related variables, both HOMA1-IR and HOMA2-IR were statistically significant markers for predicting the development of diabetes in the NGT group. All HOMA values were predictive in the pre-diabetes and non-diabetic groups. In particular, HOMA2-β was the potential marker for predicting the future development of T2DM in the pre-diabetes and non-diabetic groups.
A previous study compared the performance of HOMA2 with HOMA1 in pre-diabetic and diabetic patients using the OGTT and found that HOMA2 reflected IR and β-cell function more accurately than HOMA1 [13]. In another study, HOMA2 more significantly affected the identification of IR and the detection of metabolic syndrome and polycystic ovarian disease than HOMA1 [18]. In this study, HOMA1-IR and HOMA2-IR were not significantly different in their ability to predict the progression to T2DM in the NGT group, but HOMA2, especially HOMA2-β, was more predictive in pre-diabetic and non-diabetic Koreans than HOMA1. In particular, HOMA2-β was the most predictive marker for the pre-diabetic group, probably due to differences in age, race, and BMI. The β-cell function of Asians is usually lower than in Western ethnic groups [19,20] based on a multiethnic cohort study of diet and cancer [21]. Further, the low HOMA-β group had a higher risk of progression to diabetes than the high HOMA-IR group in a prospective study of Korean men [10]. These outcomes point to the need for a standard model appropriate for Koreans because the factors that affect the development of diabetes vary depending on ethnicity. At a minimum, if we use the established HOMA model, we need to select the best model according to glycemic status.
We also observed that HOMA1-β and HOMA2-β were not significantly predictive in the NGT group. The normoglycemic state results from the homeostasis of glucose production, and consumption is mediated by the liver, skeletal muscle, and pancreas β-cells [22]. Accordingly, both IR and impaired insulin secretion are thought to be critical to the pathophysiology of pre-diabetes although controversy remains about the leading factor for diabetes. Both IR and impaired insulin secretion are independent determinants of the progression from NGT to pre-diabetes and from pre-diabetes to diabetes [23,24,25]. In the NGT group, the level of insulin secretion was low to normal in a person with good insulin sensitivity, so it is difficult to think that HOMA-β alone can predict the progression to diabetes in a healthy person.
The strength of this study is that it was a longitudinal observational study, not a cross-sectional study, and it investigated the usefulness of HOMA2 in a large number of Koreans. Our large sample size gave us the ability to divide the subjects into the NGT and pre-diabetic groups, allowing us to compare the performance of HOMA1 and HOMA2 in the NGT and prediabetes groups.
Even so, this study had several limitations. First, all of the study subjects were enrolled in the health screening center of our hospital, and the study was conducted at a single center. Therefore, the results may not be representative of the entire Korean population. In addition, except for oral hypoglycemic agents, we did not confirm previous medication history, which could affect IR or β-cell function. Finally, we defined pre-diabetes using fasting plasma glucose, so there were no data about the progression to diabetes according to impaired glucose tolerance.
In conclusion, HOMA2, especially HOMA2-β, was more predictive for the progression to diabetes in pre-diabetes or non-diabetic Koreans. HOMA2 may offer a meaningful predictor of diabetes in Koreans if appropriate values are selected depending on individual glycemic status.
ACKNOWLEDGMENTS
This study was supported by Health Promotion Funds from the Korean Ministry for Health, Welfare, and Family Affairs and by the Welfare Bureau of the Seoul Metropolitan Government and SBRI (Samsung Biomedical Research Institute) Grant to CYP.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia. 2003;46:3–19. doi: 10.1007/s00125-002-1009-0. [DOI] [PubMed] [Google Scholar]
- 2.Meier JJ, Bonadonna RC. Role of reduced beta-cell mass versus impaired beta-cell function in the pathogenesis of type 2 diabetes. Diabetes Care. 2013;36(Suppl 2):S113–S119. doi: 10.2337/dcS13-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matthews DR. Insulin resistance and beta-cell function: a clinical perspective. Diabetes Obes Metab. 2001;3(Suppl 1):S28–S33. [PubMed] [Google Scholar]
- 4.Li CL, Tsai ST, Chou P. Relative role of insulin resistance and beta-cell dysfunction in the progression to type 2 diabetes: the Kinmen Study. Diabetes Res Clin Pract. 2003;59:225–232. doi: 10.1016/s0168-8227(02)00249-8. [DOI] [PubMed] [Google Scholar]
- 5.Borai A, Livingstone C, Kaddam I, Ferns G. Selection of the appropriate method for the assessment of insulin resistance. BMC Med Res Methodol. 2011;11:158. doi: 10.1186/1471-2288-11-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meier JJ, Menge BA, Breuer TG, Muller CA, Tannapfel A, Uhl W, Schmidt WE, Schrader H. Functional assessment of pancreatic beta-cell area in humans. Diabetes. 2009;58:1595–1603. doi: 10.2337/db08-1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 8.Sung KC, Reaven GM, Kim SH. Utility of homeostasis model assessment of beta-cell function in predicting diabetes in 12,924 healthy Koreans. Diabetes Care. 2010;33:200–202. doi: 10.2337/dc09-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Saggiani F, Poli M, Perbellini S, Raffaelli A, Cacciatori V, Santi L, Targher G, Bonadonna R, Muggeo M. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care. 2002;25:1135–1141. doi: 10.2337/diacare.25.7.1135. [DOI] [PubMed] [Google Scholar]
- 10.Choi ES, Rhee EJ, Kim JH, Won JC, Park CY, Lee WY, Oh KW, Park SW, Kim SW. Insulin sensitivity and insulin secretion determined by homeostasis model assessment and future risk of diabetes mellitus in Korean men. Korean Diabetes J. 2008;32:498–505. [Google Scholar]
- 11.Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2192. doi: 10.2337/diacare.21.12.2191. [DOI] [PubMed] [Google Scholar]
- 12.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 13.Caumo A, Perseghin G, Lattuada G, Ragogna F, Brunani A, Luzi L. Comparing the original (HOMA1) and the updated (HOMA2) method: evidence that HOMA2 is more reliable than HOMA1. Diabetes. 2007;56(Suppl 1):A406. [Google Scholar]
- 14.Caumo A, Perseghin G, Brunani A, Luzi L. New insights on the simultaneous assessment of insulin sensitivity and beta-cell function with the HOMA2 method. Diabetes Care. 2006;29:2733–2734. doi: 10.2337/dc06-0070. [DOI] [PubMed] [Google Scholar]
- 15.Geloneze B, Vasques AC, Stabe CF, Pareja JC, Rosado LE, Queiroz EC, Tambascia MA BRAMS Investigators. HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS) Arq Bras Endocrinol Metabol. 2009;53:281–287. doi: 10.1590/s0004-27302009000200020. [DOI] [PubMed] [Google Scholar]
- 16.Al-Hakeim HK, Abdulzahra MS. Correlation between glycated hemoglobin and HOMA indices in type 2 diabetes mellitus: prediction of beta-cell function from glycated hemoglobin. J Med Biochem. 2015;34:191–199. doi: 10.2478/jomb-2014-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242:2562–2571. [PubMed] [Google Scholar]
- 18.Safar FH, Mojiminiyi OA, Al-Rumaih HM, Diejomaoh MF. Computational methods are significant determinants of the associations and definitions of insulin resistance using the homeostasis model assessment in women of reproductive age. Clin Chem. 2011;57:279–285. doi: 10.1373/clinchem.2010.152025. [DOI] [PubMed] [Google Scholar]
- 19.Møller JB, Dalla Man C, Overgaard RV, Ingwersen SH, Tornoe CW, Pedersen M, Tanaka H, Ohsugi M, Ueki K, Lynge J, Vasconcelos NM, Pedersen BK, Kadowaki T, Cobelli C. Ethnic differences in insulin sensitivity, beta-cell function, and hepatic extraction between Japanese and Caucasians: a minimal model analysis. J Clin Endocrinol Metab. 2014;99:4273–4280. doi: 10.1210/jc.2014-1724. [DOI] [PubMed] [Google Scholar]
- 20.Torréns JI, Skurnick J, Davidow AL, Korenman SG, Santoro N, Soto-Greene M, Lasser N, Weiss G; Study of Women's Health Across the Nation (SWAN) Ethnic differences in insulin sensitivity and beta-cell function in premenopausal or early perimenopausal women without diabetes: the Study of Women's Health Across the Nation (SWAN) Diabetes Care. 2004;27:354–361. doi: 10.2337/diacare.27.2.354. [DOI] [PubMed] [Google Scholar]
- 21.Maskarinec G, Grandinetti A, Matsuura G, Sharma S, Mau M, Henderson BE, Kolonel LN. Diabetes prevalence and body mass index differ by ethnicity: the Multiethnic Cohort. Ethn Dis. 2009;19:49–55. [PMC free article] [PubMed] [Google Scholar]
- 22.DeFronzo RA. Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes. 1988;37:667–687. doi: 10.2337/diab.37.6.667. [DOI] [PubMed] [Google Scholar]
- 23.Haffner SM, Miettinen H, Gaskill SP, Stern MP. Decreased insulin action and insulin secretion predict the development of impaired glucose tolerance. Diabetologia. 1996;39:1201–1207. doi: 10.1007/BF02658507. [DOI] [PubMed] [Google Scholar]
- 24.Haffner SM, Miettinen H, Gaskill SP, Stern MP. Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes. 1995;44:1386–1391. doi: 10.2337/diab.44.12.1386. [DOI] [PubMed] [Google Scholar]
- 25.Weyer C, Tataranni PA, Bogardus C, Pratley RE. Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care. 2001;24:89–94. doi: 10.2337/diacare.24.1.89. [DOI] [PubMed] [Google Scholar]