PRESENTATION
In certain circumstances, new T-wave inversions are not pathological. A 72-year-old woman with hypertension, paroxysmal atrial fibrillation, atrial flutter, and tachycardia-bradycardia syndrome developed frequent symptomatic conversion pauses and underwent uneventful implantation of a dual chamber pacemaker. Her electrocardiogram (ECG) prior to pacemaker implantation is shown in Figure 1. One week after pacemaker implantation, the patient returned for a routine medical appointment. A repeat ECG demonstrated new, diffuse T-wave inversions (Figure 2). The patient had no chest discomfort, dyspnea, or other specific symptoms.
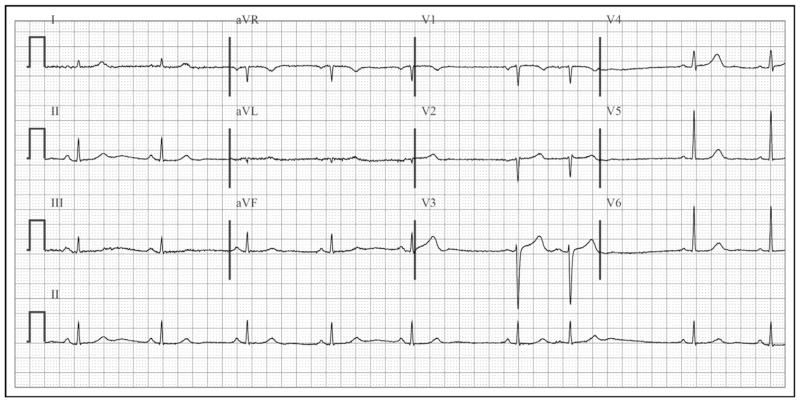
Figure 1.
Prior to pacemaker implantation, the patient’s baseline electrocardiogram (ECG) disclosed sinus rhythm with premature atrial contractions, narrow QRS complexes, and normal T-wave orientation.
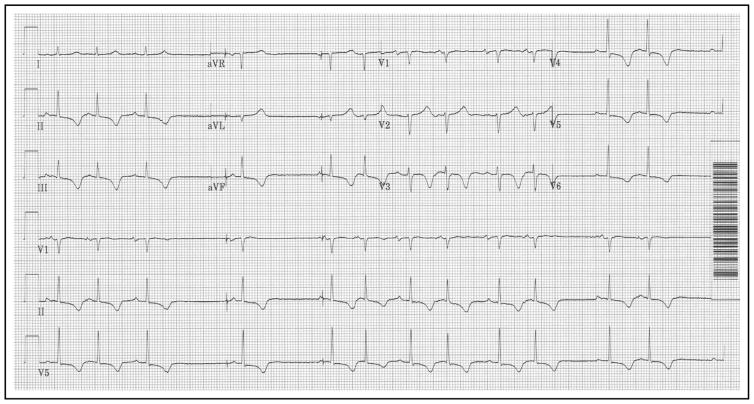
Figure 2.
The ECG obtained 1 week after pacemaker implantation showed new T-wave inversions in leads II, III, aVF, and V3–V6.
ASSESSMENT
Compared with the baseline tracing (Figure 1), the patient’s repeat ECG (Figure 2) demonstrated sinus rhythm with intermittent sinus arrest and atrial pacing, premature atrial contractions, and new T-wave inversions in the inferior leads (II, III, and aVF) and leads V3–V6. Her vital signs and physical examination were normal. Results from laboratory testing, including electrolyte levels, were also normal. A transthoracic echocardiogram demonstrated normal biventricular and valvular function, along with a trivial pericardial effusion. Interrogation of the patient’s pacemaker revealed stable lead parameters. The pacemaker was pacing 23% of the time in the atrium and 54% of the time in the ventricle. An ECG obtained during ventricular pacing is shown in Figure 3.
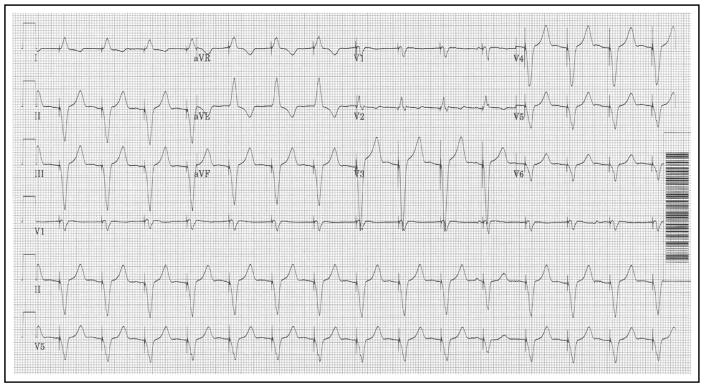
Figure 3.
An ECG obtained during right ventricular pacing via the patient’s pacemaker demonstrated that the paced QRS complexes were negative in leads that had new T-wave inversions (II, III, aVF, and V3–V6).
DIAGNOSIS
The patient’s new T-wave inversions (Figure 2) were present in leads in which the QRS complex was negative during ventricular pacing (leads II, III, aVF, and V3–V6), while T waves remained upright in leads with upright QRS complexes during ventricular pacing (leads I, aVL, aVR, and V2) (Figure 3). Together, the distribution of T-wave inversions, lack of cardiovascular symptoms, normal echocardiogram and laboratory values, and recent ventricular pacing, were consistent with cardiac—or T-wave—memory.
Cardiac memory refers to persistent T-wave changes that develop after a period of abnormal ventricular activation (wide QRS complexes) once normal ventricular activation (with narrow QRS complexes) is restored.1,2 After normal ventricular activation is restored, the T wave “remembers” and mirrors the direction of the wide QRS complexes. Therefore, cardiac memory results in positive T waves in leads that had positive wide QRS complexes and negative T waves in leads that had negative wide QRS complexes. These T-wave changes can follow resolution of any condition that triggers transient QRS widening, including transient left bundle branch block, ventricular tachycardia, intermittent ventricular pre-excitation, and ventricular pacing.3–6 Cardiac memory can persist up to weeks after normal ventricular conduction is restored.1
Recognition of cardiac memory as a potential cause of T-wave inversions is critical to avoid unnecessary hospital admission, cardiac testing, and cardiac catheterization. Fortunately, analysis of T-wave morphology can help differentiate T-wave inversions due to ischemia from those induced by cardiac memory after right-ventricular pacing. One study showed that the combination of a positive T wave in aVL, a positive or isoelectric T wave in lead I, and a maximum T-wave inversion in the pre-cordial leads that was greater than the T-wave inversion in lead III was 92% sensitive and 100% specific for T-wave inversions induced by cardiac memory from right-ventricular pacing.7
MANAGEMENT
Although certain morphologic characteristics of T-wave inversion favor a diagnosis of cardiac memory due to right-ventricular pacing, these criteria do not apply to cardiac memory from other causes. For this reason, having access to an ECG during the wide QRS rhythm can facilitate the diagnosis of cardiac memory.
Once other causes have been ruled out, T-wave inversions secondary to cardiac memory do not, by themselves, require any specific therapy. In patients without pacemakers, cardiac memory may reflect intermittent left bundle branch block, paroxysmal ventricular tachycardia, or intermittent ventricular preexcitation, and ambulatory cardiac rhythm monitoring may be appropriate to establish a diagnosis. Our patient’s cardiac memory was secondary to ventricular pacing, so no further evaluation or treatment was required.
Acknowledgments
Funding: Kramer is supported by a Paul B. Beeson Career Development Award in Aging Research (K23AG045963).
Footnotes
Conflict of Interest: None of the authors have any conflicts of interest to report in association with this topic.
Authorship: All authors had access to the data and a role in writing the manuscript.
References
- 1.Shvilkin A, Huang HD, Josephson ME. Cardiac memory: diagnostic tool in the making. Circ Arrhythm Electrophysiol. 2015;8:475–482. doi: 10.1161/CIRCEP.115.002778. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum MB, Blanco HH, Elizari MV, Lázzari JO, Davidenko JM. Electrotonic modulation of the T wave and cardiac memory. Am J Cardiol. 1982;50:213–222. doi: 10.1016/0002-9149(82)90169-2. [DOI] [PubMed] [Google Scholar]
- 3.Engel TR, Shah R, DePodesta LA, Frankl WS, Krause RL. T-wave abnormalities of intermittent left bundle-branch block. Ann Intern Med. 1978;89:204–206. doi: 10.7326/0003-4819-89-2-204. [DOI] [PubMed] [Google Scholar]
- 4.Sorgente A, Josephson ME. Contribution of the T wave vector in localizing the site of origin of a monomorphic idiopathic ventricular tachycardia. J Cardiol Cases. 2012;5:e28–e31. doi: 10.1016/j.jccase.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicolai P, Medvedowsky JL, Delaage M, Barnay C, Blache E, Pisapia A. Wolff-Parkinson-White syndrome: T wave abnormalities during normal pathway conduction. J Electrocardiol. 1981;14:295–300. doi: 10.1016/s0022-0736(81)80012-x. [DOI] [PubMed] [Google Scholar]
- 6.Chatterjee K, Harris A, Davies G, Leatham A. Electrocardiographic changes subsequent to artificial ventricular depolarization. Br Heart J. 1969;31:770–779. doi: 10.1136/hrt.31.6.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shvilkin A, Ho KK, Rosen MR, Josephson ME. T-vector direction differentiates postpacing from ischemic T-wave inversion in precordial leads. Circulation. 2005;111:969–974. doi: 10.1161/01.CIR.0000156463.51021.07. [DOI] [PubMed] [Google Scholar]