Abstract
We studied dietary patterns, physical activity (PA), and monthly goal setting in a weight reduction intervention in long-distance professional drivers. The study was conducted in Finland in 2009–2012. Male drivers with waist circumference > 100 cm were randomized to a lifestyle counseling (LIFE, N = 55) and a reference (REF, N = 58) group. During 12 months, LIFE participated in 6 face-to-face and 7 telephone counseling sessions on diet and PA. Dietary patterns were assessed using an index combining food diary and counselor interview, and PA with the number of daily steps using a pedometer. Monthly lifestyle goals, perceived facilitators and barriers, and adverse effects of PA in the LIFE participants were monitored using counselors' log books. Forty-seven (85%) LIFE participants completed the 12-month program. After 12 months, the mean dietary index score improved by 12% (p = 0.002, N = 24), and the number of daily steps increased by 1811 steps (median; p = 0.01, N = 22). The most frequent dietary goals dealt with meal frequency, plate model, and intake of vegetables, fruits, and berries. The most common PA mode was walking. Typical facilitators to reach monthly lifestyle goals were support from family and friends and ailment prevention; typical barriers were working schedules and ailments. Adverse effects, most commonly musculoskeletal pain, occurred among 83% of the LIFE participants. Positive changes in lifestyle habits were observed during counseling. Monthly lifestyle counseling combining face-to-face and phone contacts seemed appropriate to long-distance drivers. Barriers for reaching lifestyle changes, and adverse effects of PA were common and need to be addressed when planning counseling.
Trial registration: Clinical Trials NCT00893646
Abbreviations: BMI, body mass index; LIFE, lifestyle counseling group; PA, physical activity; REF, reference group (control)
Keywords: Automobile driving; Male, life style; Counseling; Walking; Diet
Highlights
-
•
Our study is one of the few lifestyle counseling RCTs in truck and bus drivers.
-
•
Dietary habits improved during 12-month program.
-
•
Habitual walking and daily step count increased during 12-month program.
-
•
Improved dietary habits were associated with weight reduction.
-
•
Perceived barriers related to working schedules and ailments were common.
1. Introduction
Obesity and cardiometabolic risk factors are common health concerns in professional truck and bus drivers (Sieber et al., 2014, Dahl et al., 2009, Apostolopoulos et al., 2013). Factors related to work environment and personal behavior affect drivers' lifestyle, which often consists of long sitting periods at work, unhealthy dietary patterns, and low leisure-time physical activity (PA) (Birdsey et al., 2015, Tse et al., 2006, van der Beek, 2012, Varela-Mato et al., 2016, Wong et al., 2014). Professional drivers tend to snack; they also consume fewer fruits and vegetables and more salt and saturated fat than recommended (Jack et al., 1998, McDonough et al., 2014, Nagler et al., 2013). Irregular driving hours and working at night often characterize drivers' schedules (Tse et al., 2006, van der Beek, 2012, Marqueze et al., 2012), which may result in sleep disturbances and obesity (Marqueze et al., 2013, Hemio et al., 2015).
Despite problems in professional drivers' health and lifestyle, few intervention studies have been conducted to improve their health (Gilson et al., 2016, Ng et al., 2015, Tse et al., 2006); the results have been inconclusive. A randomized controlled trial (RCT) among 1061 overweight transit workers, mostly metropolitan bus drivers, resulted in some dietary improvements, but no changes in PA or weight (French et al., 2010). A 4-month smoking cessation and weight management intervention in 227 truck drivers and dock workers, of whom 89% were overweight, showed small improvements in diet but no changes in weight (Sorensen et al., 2010). In general, men are less likely than women to adhere to lifestyle interventions (Pagoto et al., 2012); but when they start, men succeed equally with women (Young et al., 2012).
We conducted a RCT to reduce weight in overweight long-distance truck and bus drivers, using structured, individual counseling on diet and PA. Results on body weight and cardiometabolic risk have been published (Puhkala et al., 2015). In this report, we studied the effects of the structured counseling program on dietary patterns and habitual PA, assessed monthly lifestyle goals, and identified facilitators and barriers to achieving those goals.
2. Methods
2.1. Study design and participants
Our RCT was conducted in Finland in 2009–2012. A more detailed description of the study design has been reported (Puhkala et al., 2015). The main inclusion criteria were being a male truck or bus driver in long-distance service, waist circumference ≥ 100 cm, and being physically inactive (less than twice weekly, moderate-intensity leisure PA for 30 min). Drivers were mainly recruited by fliers in service stations, workplaces, and through labor unions.
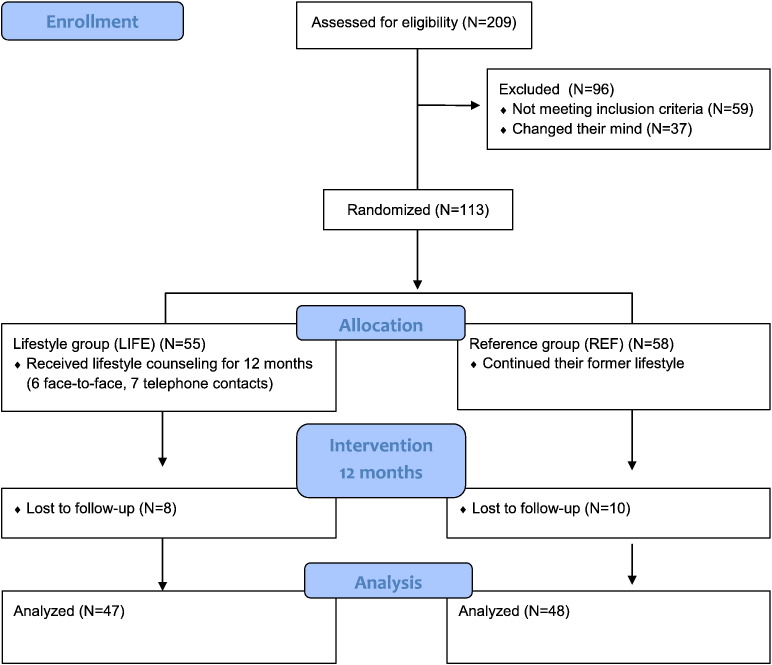
After recruitment for 18 months, 113 eligible drivers were randomized to lifestyle counseling (LIFE, N = 55) and reference (REF, N = 58) groups (Fig. 1). LIFE participated monthly in counseling for 12 months aiming at a 10% body-weight-reduction. Waiting-list REF participants were instructed to follow their former lifestyle during the 12-month period. Assessments for all participants took place at baseline and 12 months, including questionnaires, biochemical blood samples, and body weight measurement.
Fig. 1.
Flow diagram of the study. The lifestyle counseling group (LIFE) participated in 12-month lifestyle counseling program starting from baseline. Assessments took place at baseline and at 12 months. Data from weight reduction study in Finnish professional drivers in 2009–2012. The figure is adapted from Puhkala et al. (2015).
The study was reviewed by Pirkanmaa University Hospital District Ethics (Ref. number R09025). The participants completed a written informed consent. The research was conducted in accordance with the Declaration of Helsinki (2000).
2.2. Counseling program in LIFE
Three trained counselors conducted the program. Topics included diet and PA. The program consisted of 13 individual sessions: 6 face-to-face sessions (baseline and months 1, 3, 6, 9 and 12) with 7 telephone sessions in between. Face-to-face sessions were planned to last for 60 min, telephone sessions for 30 min. All sessions took place during participants' leisure or work breaks. The counselors traveled to meet participants for face-to-face sessions.
We used the Health Action Process Approach (Lippke et al., 2004, Schwarzer et al., 2008, Schwarzer, 2008) as the theory base for developing the program and content of the counseling. The first three sessions focused on intention building, the fourth through twelfth sessions on putting the intentions into action via planning, and the thirteenth session on maintaining the recommended actions. During each counseling session, the participant and the counselor together established dietary and PA goals for the following month. The content of the sessions is described in Table 1.
Table 1.
Contents of the monthly counseling sessions in the lifestyle counseling group (LIFE). Material delivered to the participants is in italics.
| Session: number, timing and type | Contents |
|---|---|
| 1st, month 0 Face-to-face |
Baseline assessments Diet: check-list for dietary patterns; meal frequency (establishing goals for next 4 weeks); diet leaflet PA: instructions to measure daily step count with a pedometer |
| 2nd, month 1 Face-to-face |
Diet: meal frequency (compliance, revision of goals); plate model (establishing goals) PA: BL + 2000 steps on 2 d/wk; PA leaflet |
| 3rd, month 2 Phone |
Diet: meal frequency and plate model (compliance, revision of goals); food quality (establishing goals) PA: adverse effects, compliance; BL + 2000 steps on 2 d/wk, stretching exercises |
| 4th, month 3 Face-to-face |
Diet: meal frequency, plate model and food quality (compliance and revision of goals) PA: adverse effects, compliance; BL + 2000 steps on 3 d/wk |
| 5th, month 4 Phone |
Diet: as 4th session PA: as 4th session |
| 6th, month 5 Phone |
Diet: as 4th session PA: adverse effects, compliance; BL + 2000 steps on 4 d/wk |
| 7th, month 6 Face-to-face |
Diet: as 4th session PA: adverse effects, compliance; BL + 2000 steps on 5 d/wk |
| 8th, month 7 Phone |
Diet: as 4th session PA: adverse effects, compliance; BL + 2000 steps on 3 d/wk and BL + 4000 steps on 2 d/wk |
| 9th, month 8 Phone |
Diet: as 4th session PA: adverse effects, compliance; BL + 2000 steps on 2 d/wk and BL + 4000 steps on 3 d/wk |
| 10th, month 9 Face-to-face |
Diet: as 4th session PA: adverse effects, compliance; BL + 2000 steps on 1 d/wk and BL + 4000 steps on 4 d/wk |
| 11th, month 10 Phone |
Diet: as 4th session PA: adverse effects, compliance; BL + 4000 steps on 5 d/wk |
| 12th, month 11 Phone |
Diet: as 4th session PA: as 11th session |
| 13th, month 12 Face-to-face |
12-month assessments Diet: compliance, check-list for dietary patterns PA: adverse effects, compliance Maintenance of dietary patterns and PA |
PA = physical activity, BL = baseline, d = day(s), wk = week(s).
Data from weight reduction study in Finnish professional drivers in 2009–2012. Adapted and modified from Puhkala et al. (2015).
The counselors used a participant-specific notebook to follow the intended procedures and topics of the counseling sessions. The following items were assessed monthly and recorded in the notebook: weight and waist circumference; setting and reaching the dietary and PA goals; perceived facilitators and barriers to lifestyle changes; and adverse effects of PA. The participants were provided with printed material on lifestyle habits. The participants had log books to assess lifestyle habits, to plan monthly goals, and to monitor daily accomplishment of the goals.
2.3. Lifestyle
2.3.1. Dietary patterns
The LIFE participants completed a 3-day food diary on two working days and one non-working day at baseline and 12 months. They were instructed to report what they ate and drank, as well as timing, amount, and brand names. Based on the food diary and a subsequent interview, the counselors graded 14 dietary items to form a healthy diet index during baseline and 12-month counseling sessions. The items were meal frequency; plate model use; vegetables, fruit, and berries; grain products; milk and milk products; meat and meat products; fish; bread spread; cooking fat; salad dressing; fast food; sweets; energy-containing drinks; and alcohol. The grading criteria (scale 1–3, number 3 being the best) were based on the Finnish Nutrition Recommendations (National Nutrition Council, 2005). Both the amount and quality of each item were taken into account in grading. The dietary index score was the sum of the grades for the 14 items (score range 14–42).
2.3.2. Physical activity
The LIFE participants used log books to record daily steps during the 12-month program. The information on mean daily step count at baseline and 12 months were used in the analyses. Weekly minutes of walking and daily hours of sitting were asked of LIFE and REF participants at baseline and 12 months, using a questionnaire based on the short version of International Physical Activity Questionnaire (Craig et al., 2003, The IPAQ group, 2005).
2.4. Dietary and PA goals
Dietary goals were based on Finnish nutrition recommendations by the National Nutrition Council (2005). The main goals were to decrease energy intake by balancing meal frequency and increasing the intake of vegetables, fruits, and berries. The plate model was used for meals: half of the plate consists of vegetables; one fourth of potatoes, rice, or pasta; and one fourth of meat, fish, or legumes. The other goals were to use vegetable oils and spreads, consume low fat milk and meat products, and reduce the use of low-fiber, rapidly-absorbed carbohydrates (e.g. refined grain-products, sweets, and sugary drinks).
Increasing habitual walking was the major PA goal. The emphasis was on taking walks in leisure time and during work breaks. A pedometer (Omron Walking Style II, HJ-113-E, Omron Healthcare, Kyoto, Japan) was used for setting daily step goals and monitoring their achievement. The ultimate goal at 12 months was to add 4000 steps on five self-selected days of the week. As 4000 steps corresponds to approximately 30 min of brisk walking, the additional steps equate to a total of 150 min a week, meeting the aerobic exercise recommendation of the 2008 United States PA guidelines (U.S. Department of Health and Human Services, 2008). At the first counseling session, the participants were instructed to wear the pedometer on five ordinary working and two non-working days and to calculate the mean number of daily steps. The ultimate step goal was approached progressively with smaller goals of adding increments of 2000 steps to an increasing number of days each week (Table 1). Such an approach has been shown to be achievable in worksite interventions (Wyatt et al., 2004, Aittasalo et al., 2012, Tudor-Locke et al., 2011).
2.5. Factors related to accomplishment of lifestyle goals
Monthly dietary and PA goals, as well as perceived facilitators and barriers to achieve the goals were assessed as total number of times (mentions) the goal was established, and number of times (mentions) the facilitator or barrier was reported by the LIFE participants during 12 months. The first facilitator and barrier mentioned in each session were included in the analyses.
Adverse effects due to PA, or those which prevented participants from performing PA were listed in the counselors' notebooks. They were discussed with the participant during each session. The adverse effects included muscle pain; back pain; hip, knee, or ankle pain; chest pain; cardiac arrhythmia; dyspnea; fatigue; sprains or distorsions; and falls or other accidents leading to symptoms. Adverse effects were reported both by the total number of mentions and by the number of days adverse effects kept participants from reaching PA goals.
2.6. Statistical analyses
Descriptive data are presented as frequencies and percentages, means or medians and standard deviations (SD), or percentiles (Q1, Q3, i.e. interquartile range). Changes in dietary patterns and daily steps in LIFE were analyzed with the Wilcoxon ranks test, and change in dietary index with paired t-test. Differences in changes between LIFE and REF in weekly duration of habitual walking and daily sitting were analyzed with linear logistic regression adjusted by baseline values and age. Spearman correlation analysis was used to analyze associations between changes in dietary items, step count, and body weight (non-parametric data); and Pearson correlation analysis between changes in dietary index and body weight (parametric data). All results were considered to be statistically significant if p < 0.05 or if 95% confidence intervals (CI) did not cross point zero. The analyses were performed with SPSS software (version 22.0).
3. Results and discussion
At baseline, the mean age of the participants (N = 113) was 47 years, and the mean BMI 33 kg/m2. Eighty-three (73%) participants were truck drivers and the rest were bus drivers. Seventy-four (65%) participants had irregular working hours, 17 (18%) shift work, and 12 (13%) regular day shifts. There were no differences between LIFE and REF in background characteristics.
After 12 months, the mean body weight change was − 3.4 in the LIFE (N = 47). When compared to the REF (N = 48), the net change was − 4.0 kg (95% CI − 6.2 to − 1.9) (Puhkala et al., 2015).
3.1. Adherence to the counseling program
Forty-seven (85%) participants in LIFE completed the 12-month program. Compared to other lifestyle counseling studies on males, the proportion of dropouts (15%) was low (Robertson et al., 2014). Reasons for discontinuation were lack of motivation, schedule conflicts, and changes in life circumstances. Thirty-six (76%) of the 47 LIFE completers participated in all 13 offered counseling sessions, and 46 (98%) participated in at least seven sessions.
Good attendance suggested that the program involving both face-to-face and telephone contacts is appropriate to this target group. Participation in counseling meetings was made as easy as possible for the participants, as the counselors traveled to them. It also indicated the participants' interest in health issues and their appreciation of the free counseling offered by health professionals. It is obvious that the most health-conscious drivers were enrolled in the study (Lassen et al., 2007, Sabinsky et al., 2007).
3.2. Lifestyle
3.2.1. Dietary patterns
Table 2 shows dietary patterns and their changes during the 12-month counseling program in the LIFE group. Meal frequency and plate model use improved. Intake of vegetables, fruits, and berries; grain products; milk and milk products; meat and meat products; sweets; fast food; and energy-containing drinks changed to a healthier direction. The mean dietary index score improved significantly by 12% (N = 24). Improved dietary index score was associated with decreased body weight at 12 months (Pearson correlation, r = 0.70, p < 0.001). Meal frequency; plate model use; and healthier intake of vegetables, fruits, and berries; milk and milk products; and bread spread were associated with decreased body weight (Spearman correlation, r = 0.37–0.49). These results are similar to other adult weight reduction studies in which associations of healthier choices with weight reduction have been observed (Bellisle, 2014, Fogelholm et al., 2012).
Table 2.
Dietary patterns at baseline and their changes after 12-month counseling in the lifestyle counseling group (LIFE). Means (SD). Each item was scaled as 1–3, the best value being 3. Items were summed to a dietary index score (range 14–42 points). Within-group differences of the changes (p value) for dietary items were analyzed by Wilcoxon ranks, and for the dietary index score by paired t-test.
| Items of dietary index | N | Baseline | Change after 12 months | p Value of the change |
|---|---|---|---|---|
| Meal frequency | 36 | 2.2 (0.4) | 0.5 (0.5) | < 0.001 |
| Plate model use | 38 | 1.9 (0.7) | 0.6 (0.9) | 0.001 |
| Vegetables, fruits and berries | 40 | 2.0 (0.6) | 0.6 (0.8) | < 0.001 |
| Grain products | 40 | 2.5 (0.5) | 0.4 (0.6) | < 0.001 |
| Milk and milk products | 38 | 2.1 (0.6) | 0.7 (0.7) | < 0.001 |
| Meat and meat products | 40 | 2.4 (0.6) | 0.3 (0.6) | 0.007 |
| Fish | 39 | 2.1 (0.8) | 0.3 (0.9) | 0.09 |
| Bread spread | 40 | 2.5 (0.7) | 0.1 (0.7) | 0.71 |
| Cooking fat | 36 | 2.6 (0.7) | 0.2 (0.7) | 0.12 |
| Oil-based salad dressing | 37 | 2.0 (0.7) | 0.2 (0.8) | 0.09 |
| Fast food | 38 | 2.5 (0.6) | 0.3 (0.7) | 0.02 |
| Sweets | 38 | 2.2 (0.8) | 0.4 (0.9) | 0.008 |
| Energy-containing drinks | 38 | 2.5 (0.6) | 0.4 (0.6) | 0.001 |
| Alcohol | 32 | 2.4 (0.7) | 0.1 (0.6) | 0.41 |
| Dietary index score | 24 | 32.7 (3.7) | 4.0 (5.3) | 0.001 |
SD = standard deviation.
Data from weight reduction study in Finnish professional drivers in 2009–2012.
Previous interventions on drivers' eating patterns are few and inconclusive. French et al. (2010) reported decreased energy intake and improvements in fruit and vegetable consumption, but no changes in consumption of sugary drinks, snacks, and sweets in motor freight workers. Sorensen et al. (2010) found decreases in consumption of sugary drinks, but no change in consumption of sugary snacks, fruits, and vegetables in truck drivers. In small interventions on overweight truck drivers (N = 12–29), some improvements in diet, such as decreased intake of saturated fat, and sugary snacks and drinks, have been observed (Thiese et al., 2015, Wipfli et al., 2013).
3.2.2. Physical activity
Daily number of steps was monitored at baseline and 12 months by 22 participants (47%) in LIFE. At baseline, the median number of daily steps was 6286 (Q1; Q3 5332; 7376). At 12 months, the participants took 1811 (median, Q1; Q3 − 832; 3564) daily steps more than at baseline (p = 0.01). The goal of adding 4000 steps daily on five days a week was reached by three of the 22 participants. Eleven participants managed to increase 2000 steps daily on five days. No association with changes in steps and body weight was observed at 12 months (Spearman correlation; r = − 0.21, p = 0.35).
At baseline, the mean duration of self-reported habitual walking was 82 (SD 99) minutes a week (N = 89). At 12 months, the duration had increased 60 (SD 160) minutes in LIFE and 9 (SD 81) minutes in REF, resulting in a between-group difference in change of 62 min (95% CI 9 to 115) in favor of LIFE (Table 3). In a subgroup of LIFE that completed the pedometer-based monitoring (N = 22), mean self-reported walking increased a little more (70, SD 139 min).
Table 3.
Habitual walking and sitting in the lifestyle counseling (LIFE) and the reference (REF) group at baseline and after 12 months, and net difference between the groups. Linear regression adjusted by baseline value and age. Means (SD).
| LIFE (N = 41–44) |
REF (N = 41–46) |
Net difference (95% CI) | |||
|---|---|---|---|---|---|
| Baseline | 12 months | Baseline | 12 months | ||
| Habitual walking (minutes per week) | 101 (110) | 161 (145) | 64 (85) | 73 (134) | 62 (9 to 115) |
| Sitting during a working day (hours per day) | 10.0 (2.9) | 9.4 (3.1) | 10.1 (3.3) | 10.3 (3.1) | − 0.9 (− 1.9 to 0.1) |
| Sitting during a non-working day (hours per day) | 5.3 (2.4) | 4.7 (2.1) | 5.1 (2.3) | 6.0 (2.7) | − 1.3 (− 2.3 to 0.4) |
SD = standard deviation; 95% CI = 95% confidence interval.
Data from weight reduction study in Finnish professional drivers in 2009–2012.
At baseline, the mean duration of sitting was 10.0 (SD 3.1) hours on a working day and 5.2 (SD 2.3) hours on a non-working day (N = 89). After 12 months, the duration of sitting did not change on a working day. During a non-working day, the mean duration of sitting decreased 0.6 h in LIFE and increased 0.8 h in REF, leading to a net decrease of 1.3 h (95% CI − 2.3 to − 0.4) in favor of LIFE. Reduction of sitting was not one of the major goals of counseling but was often discussed during the counseling sessions. Sedentary time on non-working days may have decreased as participants increased habitual walking.
Even though the number of steps and minutes of habitual walking increased and hours of sitting during a non-working day decreased at the group level, most of the LIFE participants did not achieve the step goal. Therefore, our LIFE participants' dietary improvements may have contributed more to the achieved weight loss than their moderate increases in PA. PA may not be as effective as dietary modification to affect energy balance and decrease overweight (Schwingshackl et al., 2014).
Perceived barriers to increase PA, such as working schedules, ailments, adverse effects of PA, and lack of company, were common, and may have hampered adoption of walking and other PA. In French et al.'s RCT (2010), no changes in PA were observed among motor freight workers. In general, men tend to choose increasing PA for losing weight over changing dietary habits (Kiefer et al., 2005, Robertson et al., 2014). However, male professional drivers seem to differ from other male populations: drivers find it difficult to increase PA, most likely due to environmental barriers (Turner and Reed, 2011).
3.3. Goal setting
The two most frequently mentioned dietary goals dealt with meal frequency (195 mentions) and plate model use (134). Meal frequency goals included balancing frequency of main meals and avoiding snacking. Other frequently mentioned goals dealt with the intake of vegetables, fruits, and berries (65); milk and milk products (24); candies and pastries (10); and alcohol (10). These goals were in line with the ultimate dietary counseling goals. Repeated mention of these goals also reflected participants' challenges in improving certain habits.
The most popular PA mode was walking (208 mentions). Biking was the second most popular (33), followed by gym exercises, swimming, jogging, cross-country skiing, and ball games. Many participants preferred leisure-time housekeeping and repair jobs instead of structured exercises.
3.3.1. Facilitators and barriers
The most mentioned factors that facilitated reaching dietary goals were good quality roadside resting places (8 mentions), support from family and friends (7), and their own preferences (7). The most common barriers were working schedules (15), their own attitudes and habits (13), and family habits (6). The most common facilitators for reaching PA goals were ailment prevention (10 mentions), good opportunities to perform PA (5), improved perceived alertness and well-being (4), spending time with family and friends (3), and social support from family and friends (3). The most common barriers were working schedules (29), ailments and old injuries (21), bad weather conditions or darkness (6), lack of company (3), and fatigue (3).
Facilitators and barriers for reaching dietary and PA goals were very similar to previous findings on professional drivers. Perceived facilitators to healthy lifestyle have been support from family and friends, PA support from management, and health reasons (Hedberg et al., 1998, Wong et al., 2014). Most studies on long-distance drivers suggest that factors related to working schedules and timetable pressures are major environmental barriers (Hedberg et al., 1998, McDonough et al., 2014, Nagler et al., 2013, Turner and Reed, 2011). In many countries, hours-of-service rules are set for professional heavy vehicle drivers; but because of tight competition, unrealistic schedules often cause rule violations (McCartt et al., 2008). Other barriers are poor availability of healthy food; poor or lack of exercise environment; and attitudes and preferences of family, friends, and colleagues (Jack et al., 1998, McDonough et al., 2014, Nagler et al., 2013, Turner and Reed, 2011, Wong et al., 2014). These barriers need to be addressed when providing lifestyle counseling to professional drivers. Roadside resting places should enable healthier food choices and possibilities for PA.
3.3.2. Adverse effects of PA
Thirty-nine (83%) LIFE participants reported one or more adverse effects of PA during the 12-month program. Overall, they reported 50 adverse effects, of which 42 (84%) during the first six months. Most adverse effects were minor. The two most common ones were hip, knee, or ankle pain (17 mentions), and muscle pain (17), mostly due to shin splints. Falls and other such accidents (either during leisure time or at work) leading to injuries such as sprains and distorsions, were reported 12 times. Thirty participants reported that adverse effects interfered with the achievement of step goals on 37 days (median).
Frequent adverse effects imply that musculoskeletal problems are common in overweight men not used to regular exercise, and who begin to increase PA. PA-related adverse effects during lifestyle interventions among professional drivers have not been reported earlier; only injuries related to physically demanding work tasks have been reported (Krueger et al., 2007).
3.4. Strengths and limitations of the study
The study has several strengths. It was the first RCT aimed at decreasing overweight in professional drivers through individual lifestyle counseling. We succeeded at changing dietary patterns and increasing PA in male drivers, resulting in weight loss and improved cardiometabolic risk factors (Puhkala et al., 2015). Participants' preferences, abilities, and experiences were discussed and taken into account when establishing and revising the monthly goals.
Some limitations must also be stated. Dietary patterns and daily steps were not monitored in REF during the 12-month intervention. Data on dietary patterns in LIFE were obtained from counselors' subjective assessments based on participants' food diary and subsequent interview. Misreporting eating is common (Ferrari et al., 2002). In addition, some of the lifestyle habits – for example, PA opportunities – were related to work schedules, which we could not control. Daily step counts were monitored by fewer than half of the LIFE group, probably only those participants who were interested in PA. These findings in dietary and PA patterns need to be replicated in a larger sample in a randomized design.
4. Conclusions
Positive changes in dietary patterns and PA were found in overweight professional drivers during 12-month counseling program, and dietary changes were associated with weight reduction. The monthly counseling program using both face-to-face and telephone contacts seemed appropriate to long-distance drivers. The drivers mentioned support from family and friends, and prevention of ailments as the most frequent facilitators for reaching dietary and PA goals. Frequently mentioned barriers, such as working schedules and ailments, as well as adverse effects of PA hampered adoption of the goals. Such barriers need to be addressed when planning counseling.
Competing interests
The authors declare no conflict of interest.
Transparency document
Transparency document
Acknowledgements
This study was supported by the Academy of Finland, the Ministry of Education and Culture, and the Juho Vainio Foundation. The funders had no role in study design and conduct, and in analyzing and interpreting the results. The authors are thankful to Matti Pasanen, M.Sc., for statistical advice. Research secretary Taru Helenius took care of appointment schedules. Research secretary Tiina Inkovaara participated in recruitment. Biomedical laboratory scientists Ulla Hakala, Ulla Honkanen, Sirke Rasinperä and Leena Aura, and exercise scientist Katriina Ojala, M.Sc., performed clinical assessments.
Footnotes
The Transparency document associated with this article can be found in an online version.
References
- Aittasalo M., Rinne M., Pasanen M., Kukkonen-Harjula K., Vasankari T. Promoting walking among office employees — evaluation of a randomized controlled intervention with pedometers and e-mail messages. BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-403. (403-2458-12-403) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolopoulos Y., Sonmez S., Shattell M.M., Gonzales C., Fehrenbacher C. Health survey of U.S. long-haul truck drivers: work environment, physical health, and healthcare access. Work. 2013;46:113–123. doi: 10.3233/WOR-121553. [DOI] [PubMed] [Google Scholar]
- Bellisle F. Meals and snacking, diet quality and energy balance. Physiol. Behav. 2014;134:38–43. doi: 10.1016/j.physbeh.2014.03.010. [DOI] [PubMed] [Google Scholar]
- Birdsey J., Sieber W.K., Chen G.X. National survey of US long-haul truck driver health and injury: health behaviors. J. Occup. Environ. Med. 2015;57:210–216. doi: 10.1097/JOM.0000000000000338. [DOI] [PubMed] [Google Scholar]
- Craig C.L., Marshall A.L., Sjostrom M. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Dahl S., Kaerlev L., Jensen A. Hospitalization for lifestyle related diseases in long haul drivers compared with other truck drivers and the working population at large. Work. 2009;33:345–353. doi: 10.3233/WOR-2009-0882. [DOI] [PubMed] [Google Scholar]
- Declaration of Helsinki World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2000;284(23):3043–3045. [PubMed] [Google Scholar]
- Ferrari P., Slimani N., Ciampi A. Evaluation of under- and overreporting of energy intake in the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC) Public Health Nutr. 2002;5:1329–1345. doi: 10.1079/PHN2002409. [DOI] [PubMed] [Google Scholar]
- Fogelholm M., Anderssen S., Gunnarsdottir I., Lahti-Koski M. Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review. Food Nutr. Res. 2012;56 doi: 10.3402/fnr.v56i0.19103. Epub 2012 Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French S.A., Harnack L.J., Hannan P.J., Mitchell N.R., Gerlach A.F., Toomey T.L. Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev. Med. 2010;50:180–185. doi: 10.1016/j.ypmed.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson N.D., Pavey T.G., Vandelanotte C. Chronic disease risks and use of a smartphone application during a physical activity and dietary intervention in Australian truck drivers. Aust. N. Z. J. Public Health. 2016;40:91–93. doi: 10.1111/1753-6405.12501. [DOI] [PubMed] [Google Scholar]
- Hedberg G.E., Wikstrom-Frisen L., Janlert U. Comparison between two programmes for reducing the levels of risk indicators of heart diseases among male professional drivers. Occup. Environ. Med. 1998;55:554–561. doi: 10.1136/oem.55.8.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemio K., Puttonen S., Viitasalo K., Harma M., Peltonen M., Lindstrom J. Food and nutrient intake among workers with different shift systems. Occup. Environ. Med. 2015;72:513–520. doi: 10.1136/oemed-2014-102624. [DOI] [PubMed] [Google Scholar]
- Jack F.R., Piacentini M.G., Schroder M.J. Perception and role of fruit in the workday diets of Scottish lorry drivers. Appetite. 1998;30:139–149. doi: 10.1006/appe.1997.0115. [DOI] [PubMed] [Google Scholar]
- Kiefer I., Rathmanner T., Kunze M. Eating and dieting differences in men and women. J. Mens Health Gend. 2005;2:194–201. [Google Scholar]
- Krueger G., Brewster R., Dick V., Inderbitzen R., Staplin L. Transportation Research Board of the National Academies; Washington D.C.: 2007. Commercial Truck and Bus Safety Synthesis Program (CTBSSP) synthesis 15: health and wellness programs for commercial drivers.http://onlinepubs.trb.org/onlinepubs/ctbssp/ctbssp_syn_15.pdf (Web page (visited May 31, 2016)) [Google Scholar]
- Lassen A., Bruselius-Jensen M., Sommer H.M., Thorsen A.V., Trolle E. Factors influencing participation rates and employees' attitudes toward promoting healthy eating at blue-collar worksites. Health Educ. Res. 2007;22:727–736. doi: 10.1093/her/cyl153. [DOI] [PubMed] [Google Scholar]
- Lippke S., Ziegelmann J., Schwarzer R. Initiation and maintenance of physical exercise: stage-specific effects of a planning intervention. Res. Sports Med. 2004;12:221–240. [Google Scholar]
- Marqueze E.C., Ulhoa M.A., Moreno C.R. Irregular working times and metabolic disorders among truck drivers: a review. Work. 2012;41(Suppl. 1):3718–3725. doi: 10.3233/WOR-2012-0085-3718. [DOI] [PubMed] [Google Scholar]
- Marqueze E.C., Ulhoa M.A., Moreno C.R. Effects of irregular-shift work and physical activity on cardiovascular risk factors in truck drivers. Rev. Saude Publica. 2013;47:497–505. doi: 10.1590/s0034-8910.2013047004510. [DOI] [PubMed] [Google Scholar]
- McCartt A.T., Hellinga L.A., Solomon M.G. Work schedules of long-distance truck drivers before and after 2004 hours-of-service rule change. Traffic Inj. Prev. 2008;9:201–210. doi: 10.1080/15389580802040287. [DOI] [PubMed] [Google Scholar]
- McDonough B., Howard M., Angeles R. Lone workers attitudes towards their health: views of Ontario truck drivers and their managers. BMC Res. Notes. 2014;7 doi: 10.1186/1756-0500-7-297. (297-0500-7-297) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler E.M., Viswanath K., Ebbeling C.B., Stoddard A.M., Sorensen G. Correlates of fruit and vegetable consumption among construction laborers and motor freight workers. Cancer Causes Control. 2013;24:637–647. doi: 10.1007/s10552-012-9998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Nutrition Council . Edita Prima Oy; Helsinki: 2005. Suomalaiset ravitsemussuositukset — ravinto ja liikunta tasapainoon (Finnish Nutrition Recommendations)http://www.ravitsemusneuvottelukunta.fi/attachments/vrn/ravitsemussuositus2005.fin.pdf In Finnish. Web page (visited May 31, 2016) [Google Scholar]
- Ng M.K., Yousuf B., Bigelow P.L., Van Eerd D. Effectiveness of health promotion programmes for truck drivers: a systematic review. Health Educ. J. 2015;74:270–286. [Google Scholar]
- Pagoto S.L., Schneider K.L., Oleski J.L., Luciani J.M., Bodenlos J.S., Whited M.C. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring) 2012;20:1234–1239. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- Puhkala J., Kukkonen-Harjula K., Mansikkamaki K. Lifestyle counseling to reduce body weight and cardiometabolic risk factors among truck and bus drivers—a randomized controlled trial. Scand. J. Work Environ. Health. 2015;41:54–64. doi: 10.5271/sjweh.3463. [DOI] [PubMed] [Google Scholar]
- Robertson C., Archibald D., Avenell A. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol. Assess. 2014;18 doi: 10.3310/hta18350. (v–vi, xxiii–xxix, 1–424) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabinsky M.S., Toft U., Raben A., Holm L. Overweight men's motivations and perceived barriers towards weight loss. Eur. J. Clin. Nutr. 2007;61:526–531. doi: 10.1038/sj.ejcn.1602537. [DOI] [PubMed] [Google Scholar]
- Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl. Psychol. 2008;57:1–29. [Google Scholar]
- Schwarzer R., Lippke S., Ziegelmann J. Health action process approach. A research agenda at Freie Universität Berlin to examine and promote health behavior change. Z. Gesundh. 2008;16:157–160. [Google Scholar]
- Schwingshackl L., Dias S., Hoffmann G. Impact of long-term lifestyle programmes on weight loss and cardiovascular risk factors in overweight/obese participants: a systematic review and network meta-analysis. Syst. Rev. 2014;3:130. doi: 10.1186/2046-4053-3-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieber W.K., Robinson C.F., Birdsey J. Obesity and other risk factors: the national survey of U.S. long-haul truck driver health and injury. Am. J. Ind. Med. 2014;57:615–626. doi: 10.1002/ajim.22293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G., Stoddard A., Quintiliani L. Tobacco use cessation and weight management among motor freight workers: results of the gear up for health study. Cancer Causes Control. 2010;21:2113–2122. doi: 10.1007/s10552-010-9630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The IPAQ group International Physical Activity Questionnaires (IPAQ) 2015. 2005. https://sites.google.com/site/theipaq/home Web page (visited May 31, 2016)
- Thiese M.S., Effiong A.C., Ott U. A clinical trial on weight loss among truck drivers. Int. J. Occup. Environ. Med. 2015;6:104–112. doi: 10.15171/ijoem.2015.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse J.L.M., Flin R., Mearns K. Bus driver well-being review: 50 years of research. Transp. Res. F. 2006;9:89–114. [Google Scholar]
- Tudor-Locke C., Craig C.L., Brown W.J. How many steps/day are enough? For adults. Int. J. Behav. Nutr. Phys. Act. 2011;8 (79-5868-8-79) [Google Scholar]
- Turner L.M., Reed D.B. Exercise among commercial truck drivers. AAOHN J. 2011;59:429–436. doi: 10.3928/08910162-20110916-01. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . U.S. Department of Health and Human Services 2015. 2008. 2008 Physical activity guidelines for Americans.http://health.gov/paguidelines/guidelines/ (Web page (visited May 31, 2016)) [Google Scholar]
- van der Beek A.J. World at work: truck drivers. Occup. Environ. Med. 2012;69:291–295. doi: 10.1136/oemed-2011-100342. [DOI] [PubMed] [Google Scholar]
- Varela-Mato V., Yates T., Stensel D.J., Biddle S.J.H., Clemes S.A. Time spent sitting during and outside working hours in bus drivers: a pilot study. Prev. Med. Rep. 2016;3:36–39. doi: 10.1016/j.pmedr.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wipfli B., Olson R., Koren M. Weight-loss maintenance among SHIFT pilot study participants 30-months after intervention. J. Occup. Environ. Med. 2013;55:1–3. doi: 10.1097/JOM.0b013e31827db848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J.Y., Gilson N.D., Bush R.A., Brown W.J. Patterns and perceptions of physical activity and sedentary time in male transport drivers working in regional Australia. Aust. N. Z. J. Public Health. 2014;38:314–320. doi: 10.1111/1753-6405.12214. [DOI] [PubMed] [Google Scholar]
- Wyatt H., Peters J., Reed G. Using electronic step counters to increase lifestyle physical activity: Colorado on the Move. J. Phys. Act. Health. 2004;1:181–190. [Google Scholar]
- Young M.D., Morgan P.J., Plotnikoff R.C., Callister R., Collins C.E. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes. Rev. 2012;13:393–408. doi: 10.1111/j.1467-789X.2011.00967.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document