Abstract
Developing interventions to reduce sedentary behavior in the workplace is an important public health priority. Furthermore, research is needed to determine whether different approaches to breaking up prolonged sitting during the workday are equally feasible and effective. Thus, the purpose of this study was to determine whether varying the frequency and duration of activity breaks during the workday would differentially impact sedentary behavior and health outcomes. Inactive females (N = 49) working full-time sedentary jobs were recruited for this parallel-group randomized trial. Participants were randomly assigned to take short, frequent breaks from sitting (1–2 min every half hour; SB) or longer, planned breaks from sitting (two 15-minute breaks per workday; LB) during each workday across an 8-week intervention. Sedentary time and health outcomes were assessed at baseline and post-intervention. The study ran from March 2014–June 2015. Results showed sedentary time during the workday decreased significantly in the SB group (− 35.6 min; d = − 0.75; p = 0.03), but did not change in the LB group (+ 4.5 min; d = 0.12). Participants in the SB group also demonstrated small-to-moderate declines in total cholesterol (d = − 0.33; p = 0.10), triglycerides (d = − 0.38; p = 0.06) and fasting blood glucose (d = − 0.29; p = 0.01) from pre to post-intervention. Health outcomes did not change in the LB group. This study demonstrated that taking short, frequent breaks from sitting during the workday is a feasible and effective approach for reducing sedentary time at work. These results have implications for the development of public health messages addressing sedentary behavior, and inform future interventions to reduce sedentary time in the workplace.
Trial registration
This study is registered at www.clinicaltrials.gov: NCT02609438.
Keywords: Sedentary, Sitting, Worksite, Intervention, Biomarkers
Highlights
-
•
Adherence rates were 69% (short breaks) and 61% (long breaks) across 8 weeks.
-
•
Sedentary time declined in participants who took short frequent breaks from sitting.
-
•
Fasting blood glucose improved post-intervention in the short break group only.
-
•
Taking short, frequent breaks from sitting may be a feasible and effective approach.
1. Introduction
Prolonged sitting is a significant public health concern and high levels of chronic sedentary behavior are associated with increased risk of obesity, diabetes, cardiovascular disease, some cancers, and mortality (Dunstan et al., 2005, Healy et al., 2008a, Katzmarzyk et al., 2009, Patel et al., 2010, Wilmot et al., 2012, George et al., 2013). Until recently, sedentary behavior was considered synonymous with a lack of moderate/vigorous physical activity, but accumulating evidence suggests metabolic health is compromised in those who spend the majority of their days engaged in sedentary behaviors, even if they are engaging in moderate/vigorous physical activity (Owen et al., 2010). In other words, sedentary behavior is an independent risk factor for obesity and chronic disease; therefore, interventions designed to target this outcome specifically are warranted (Hamilton et al., 2008, Dunstan et al., 2010).
Long bouts of uninterrupted sedentary behavior are likely to result in moderate to large reductions in glucose tolerance and insulin sensitivity (Dunstan et al., 2012, Saunders et al., 2012, Stephens et al., 2011). However, there is some evidence that breaking up sedentary time may help counteract some of these negative metabolic effects (Owen 2012). Short-term laboratory-based experiments have demonstrated that when sitting is interrupted every 30 min by brief activity breaks (i.e., two minutes of treadmill walking), postprandial glucose and insulin levels are significantly reduced (Dunstan et al., 2012, Peddie et al., 2013). One observational study also demonstrated a significant relationship between health outcomes (i.e., triglycerides, glucose, waist circumference) and the total number of breaks from sitting, independent of total sedentary time (Healy et al., 2008b). A recent meta-analysis, however, cautioned that more research is needed to better understand the relative importance of the frequency, duration, and intensity of activity breaks (Chastin et al., 2015).
Unfortunately, sitting has become increasingly ubiquitous in most workplaces. Since the 1960s, jobs that require moderate physical activity have declined significantly (Church et al., 2011). Up to 80% of adults in the United States now have sedentary occupations, during which 70–80% of the workday is spent sitting, primarily in bouts over 20 min without a break (Clemes et al., 2014, Parry and Straker, 2013, Thorp et al., 2012). As technology advances and labor-saving devices proliferate, these trends are likely to persist unless interventions are implemented.
In 2010, Chau and colleagues published a review highlighting a paucity of workplace interventions to reduce sitting (Chau et al., 2010). Since that time, sedentary behavior has garnered increasing interest and a number of interventions designed to reduce sitting time at work have been developed. In 2014, Neuhaus and colleagues reviewed workplace interventions using activity-permissive workstations and found a mean reduction in sedentary time of 77 min per 8-hour workday across 8 studies (Neuhaus et al., 2014). A recent Cochrane review also supported the potential effectiveness of sit-to-stand desks, but found no evidence to support other approaches (e.g., information and counseling), and concluded overall that much more research is needed to determine whether interventions to decrease occupational sitting are effective, particularly in the long-term (Shrestha et al., 2016). Additionally, to date only a handful of studies have measured cardiometabolic risk factors in the context of a workplace intervention to reduce sitting time, and the results thus far have been inconclusive (Alkhajah et al., 2012, Carr et al., 2013, Carr et al., 2015, Puig-Ribera et al., 2015).
Despite emerging evidence from laboratory studies that breaking up sedentary time confers cardiometabolic benefits, the extent to which such benefits can be observed in the context of a real-world intervention warrants further investigation. Furthermore, no studies to date have examined whether different approaches to breaking up prolonged sitting during the workday are equally feasible and effective. Multiple countries (e.g., Australia, Canada) now provide general sedentary behavior guidelines that recommend reducing time spent in prolonged sitting (Australian Department of Health, 2014, Canadian Society for Exercise Physiology, 2011), but in order to make specific recommendations about how one should go about breaking up sitting time, it is important to determine the relative effectiveness of various approaches. Thus, the purpose of the present study was to compare the effects of short, frequent breaks from sitting versus longer, planned breaks from sitting on sedentary behavior during the workday and cardiometabolic health among inactive female office employees.
2. Methods
2.1. Overview of study design
This parallel-group randomized trial employed an 8-week intervention to compare the two break strategies. All participants were advised to accumulate 30 min of activity/non-sitting time across the course of each workday, but half were randomly assigned to a short break (SB) group, and half were assigned to a long break (LB) group. Specifically, participants in the SB group were instructed to stand/move for 1–2 min every half hour, and participants in the LB group were instructed to take two 15-minute breaks from sitting each workday. All participants were advised to stand at a minimum, and move around or walk if possible during each break. Height-adjustable desks were not provided for this study. Outcomes were assessed at baseline and immediately following the 8-week intervention. All procedures were approved by the Kansas State University institutional review board (protocol 7031). Participant recruitment began in March 2014 and data collection was complete in June 2015.
2.2. Participants
Participants were recruited via university email lists and flyers distributed at local businesses. Interested individuals were directed to an online survey to assess eligibility. In order to be eligible to participate, individuals had to be premenopausal females over 21 years old, work at least 35 h per week, self-report sitting for at least 80% of working hours, and engage in < 60 min per week of moderate/vigorous physical activity (MVPA). To determine MVPA, participants described their exercise habits (frequency, duration, type) during the past month, and research staff followed up to clarify if necessary. Individuals who were pregnant or actively attempting to lose weight were excluded. Participants were primarily university employees in office settings with set hours (8:00 a.m.-5:00 p.m.) but not set break schedules.
2.3. Procedures
Individuals who met inclusion criteria received a packet containing the informed consent document, an Actigraph GT3X accelerometer, and a log sheet for documenting accelerometer wear time. Participants were asked to wear the accelerometer on the left hip during waking hours for 7 consecutive days and to document the exact times they wore the monitor each day, as well as any periods of monitor removal. Following the week of accelerometer wear, participants attended a baseline testing and orientation appointment, during which they submitted the signed the informed consent document, returned the accelerometer, and completed the health assessments. Prior to the appointment, participants were randomized to the SB or LB group, by an investigator not involved with testing, using a random digit generator in Microsoft Excel. Participants were blinded to treatment group assignment until their orientation session. For the post-intervention assessments, participants wore the accelerometer for one week beginning Monday of week 8, and reported to the laboratory during the week immediately following the intervention to repeat the health assessments.
2.4. Intervention
Immediately following the baseline health assessments, each participant attended a 30-minute individual orientation session with a trained research assistant. After an overview of the study objectives and procedures, participants were informed of their group assignment and completed a planning worksheet with the research assistant. Specifically, participants identified 3–4 specific strategies they would use to take daily activity breaks, and devised strategies for overcoming potential barriers. Participants also received a list of computer/mobile applications they could use to prompt daily activity breaks, and 8 weeks of daily activity logs.
Participants began the intervention on the Monday following their orientation session. Every Monday morning, they received an email from the research team containing information or tips related to reducing sitting time at work. During week 4 of the intervention, participants received a brief phone call from a research assistant to discuss any questions or concerns.
All participants were asked to keep daily activity logs across the 8-week duration of the intervention. For the SB group, participants were asked to record (in real time) the start time and duration of every activity break (standing or walking) that was at least one minute in duration. For the LB group, participants were asked to record the time they planned to take their two breaks, then indicate the actual time and duration of the breaks. The LB activity log also included a section to record additional breaks from sitting (time and duration) that were outside of the planned 15-minute breaks. At the end of each week, participants submitted their logs in a pre-addressed envelope or via email.
2.5. Measures
2.5.1. Demographics
At baseline, participants completed a brief demographics survey to indicate age, race, education, income, and hours worked per week.
2.5.2. Adherence
Adherence to the intervention protocols was assessed using the daily activity logs. Each day was coded as: (1) full adherence, (2) partial adherence, (3) no adherence, or (4) did not attend work. For the SB group, full adherence was defined as a minimum of 12 activity breaks (out of 16 recommended) per 8-h workday, and partial adherence was defined as a minimum or 6 activity breaks per 8-h workday. Days when participants took fewer than 6 breaks or did not submit a log were coded as no adherence. For the LB group, full adherence was defined as at least two activity breaks totaling ≥ 25 min, and partial adherence was defined as one activity break ≥ 10 min, or two activity breaks totaling < 25 min. Days when participants did not report an activity break longer than 10 min or did not submit a log were coded as no adherence.
2.5.3. Sedentary behavior and physical activity
Sedentary behavior and light/moderate activity were assessed objectively using Actigraph (Pensacola, FL) GT3X accelerometers. Data were collected over 10-s epochs at a sampling frequency of 30 Hz across 3 axes. Data were downloaded and analyzed using ActiLife 6.0. Log diaries were used to determine wear time, and only periods during which the participant indicated she was wearing the monitor for a minimum of 10 h per day were included in analyses. Sedentary behavior was defined as periods when counts per minute were ≤ 100 (Matthews et al., 2008), and the ranges for light and moderate activity were 100–1951 and 1952–5724, respectively (Freedson et al., 1998). Because the intervention targeted sitting time during the workday, we used a time filter to restrict the data to participants' working hours (i.e., Monday-Friday, 8 a.m.-5 p.m.). Outcomes were averaged across the number of days of wear.
2.5.4. Cardiometabolic health outcomes
Trained research assistants collected all health outcome data. Blood pressure was assessed using an automated blood pressure cuff (Omron model HEM-907XL) after participants had been seated for at least five minutes. Systolic and diastolic measurements were taken twice, one minute apart, with a third measurement if values differed by > 5 mmHg. The two values that were within acceptable agreement were averaged and used in analyses. Weight was measured to the nearest 0.1 kg using a Health-O-Meter 349KLX scale, and height was measured to the nearest 0.1 cm using a portable stadiometer. Waist circumference was measured to the nearest 0.1 cm using a spring-loaded tape measure. Two measurements were taken with a third assessment when the first two were > 0.5 cm different. Fasting blood samples were taken via finger stick, transferred to cassettes using a capillary tube procedure, and inserted in the Cholestech LDX analyzer to calculate total cholesterol, triglycerides, and fasting blood glucose.
2.6. Statistical analysis
A preliminary power analysis (80% power, a = 0.05) estimated a sample size of 28 per group was necessary to detect a medium-size reduction (d = 0.5) in sedentary time at work. Based on previous research, this effect size was considered conservative and feasible. To account for 20% attrition, we aimed to recruit 35 participants per group. This study was not powered to detect changes in the cardiometabolic health outcomes, but they were assessed as secondary outcomes.
Data were analyzed using SPSS version 20 (IBM Corporation, Armonk, NY). We conducted t-tests to examine baseline differences between completers and dropouts, and between participants assigned to the SB and LB conditions. Next, we calculated percent adherence for each participant by dividing the number of full adherence days by the total number of days worked. This procedure was repeated with partial adherence days added to full adherence days and Mann–Whitney U-tests were used to identify differences in adherence between the two conditions.
We conducted a series of 2 (group) × 2 (time) repeated measures analyses of variance (ANOVAs) to examine changes in sedentary behavior and cardiometabolic health outcomes from baseline to post-intervention. Effect sizes (Cohen's d) were calculated within groups for all outcomes.
3. Results
3.1. Participant characteristic and retention
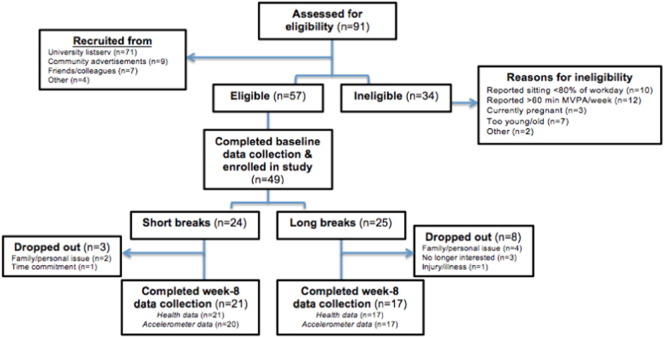
Participant flow through the study is depicted in the CONSORT diagram (Fig. 1).
Fig. 1.
CONSORT diagram.
A total of 91 individuals expressed interest in the study and completed the pre-screening questionnaire. Of these, 57 were eligible to participate and 49 completed all baseline data collection and were randomized to either the SB (n = 24) or LB (n = 25) group. Of participants who were randomized, 11 dropped out [SB (n = 3; 87.5% retention), LB (n = 8; 68.0% retention)]. Participants who dropped out primarily cited family/personal issues unrelated to the study as reasons for discontinuing participation. Participants who completed the study did not differ from those who dropped out on any baseline or demographic variables.
Demographic characteristics of the sample are presented in Table 1.
Table 1.
Demographic characteristics of the sample.
| Variable | Mean (SD)/Freq (%) |
|
|---|---|---|
| Long break group n = 25 |
Short break group n = 24 |
|
| Age | 38.92 (7.88) | 38.50 (8.67) |
| Hours worked per week | 41.52 (4.09) | 41.52 (2.48) |
| Body mass index | ||
| Normal weight (18.5–24.9) | 7 (28%) | 6 (25%) |
| Overweight (25–29.9) | 3 (12%) | 4 (16.7%) |
| Obese (> 30) | 15 (60%) | 14 (58.3%) |
| Race | ||
| White | 22 (88%) | 19 (79.2%) |
| Asian | 1 (4%) | 2 (8.3%) |
| African American | 2 (8%) | 3 (12.5%) |
| Education | ||
| High school graduate | 4 (16%) | 3 (12.5%) |
| College graduate | 8 (32%) | 12 (50%) |
| Advanced degree | 13 (52%) | 9 (37.5%) |
| Annual household income | ||
| <$30,000 | 4 (16%) | 2 (8.3%) |
| $30,000–$59,999 | 4 (16%) | 10 (41.7%) |
| $60,000–$89,999 | 5 (20%) | 8 (33.3%) |
| >$90,000 | 7 (28%) | 3 (12.5%) |
| Not disclosed | 5 (20%) | 1 (4.2%) |
The average age of the sample was 38.71 ± 8.19 years. Most participants were working full-time in office positions at the university. Participants were primarily white and college educated. Nearly 60% of the sample was obese. There were no significant demographic differences between the two study groups at baseline; however, participants assigned to the LB group had higher total cholesterol (p = 0.02) and fewer minutes of sedentary time per workday (p = 0.05) at baseline than participants assigned to the SB group.
3.2. Adherence
Based on the daily logs, participants who completed the study fully adhered to the recommended protocols 69.2% (SB group) and 60.8% (LB group) of working days, and partially adhered an additional 19.9% (SB group) and 20.1% (LB group) of working days. We also calculated adherence rates in the full sample of randomized participants (dropouts included). This more conservative approach yielded adherence rates of 60.5% (SB group) and 49.2% (LB group) for full adherence only, and 79.6% (SB group) and 65.2% (LB group) when days with partial adherence were also included. The difference in adherence between groups was statistically significant (p = 0.04) for the final analysis only.
3.3. Sedentary behavior and physical activity
At baseline, the average percentage time at work spent in sedentary behavior was 83.1%. Table 2 includes the within-group means, standard deviations, and effect sizes for all accelerometer and health outcomes.
Table 2.
Descriptive statistics for sedentary behavior and health outcomes.
| Variable | Group | 1. Baseline M (SD) |
2. Post-interventionM (SD) | d |
p (time) |
|---|---|---|---|---|---|
| Sedentary min per workday | Short | 433.4 (45.5) | 397.8 (49.5) | − 0.75 | 0.03 |
| Long | 415.7 (45.8) | 421.1 (40.3) | 0.12 | 0.68 | |
| Light activity per workday | Short | 70.3 (19.6) | 74.2 (21.6) | 0.19 | 0.36 |
| Long | 62.3 (29.9) | 63.2 (22.5) | 0.04 | 0.87 | |
| Moderate activity per workday | Short | 17.3 (8.0) | 16.9 (9.4) | − 0.04 | 0.80 |
| Long | 12.8 (5.1) | 15.5 (7.8) | 0.42 | 0.07 | |
| Total cholesterol | Short | 170.7 (29.4) | 160.7 (30.8) | − 0.33 | 0.10 |
| Long | 196.2 (27.0) | 191.4 (27.4) | − 0.18 | 0.34 | |
| Triglycerides | Short | 136.2 (52.6) | 115.4 (56.2) | − 0.38 | 0.06 |
| Long | 145.3 (69.6) | 143.3 (76.1) | − 0.03 | 0.81 | |
| Glucose | Short | 98.8 (15.2) | 94.6 (13.8) | − 0.29 | 0.01 |
| Long | 102.2 (37.8) | 102.4 (39.8) | 0.004 | 0.93 | |
| Systolic blood pressure | Short | 113.1 (11.8) | 110.3 (11.8) | − 0.23 | 0.25 |
| Long | 113.4 (14.6) | 112.1 (17.5) | 0.08 | 0.73 | |
| Diastolic blood pressure | Short | 74.2 (8.5) | 72.2 (10.4) | − 0.21 | 0.14 |
| Long | 74.4 (11.3) | 74.8 (11.4) | 0.03 | 0.86 | |
| Waist circumference (cm) | Short | 103.29 (19.0) | 102.21 (18.7) | − 0.06 | 0.14 |
| Long | 103.32 (19.7) | 102.52 (20.2) | − 0.04 | 0.54 | |
| Weight (kg) | Short | 86.38 (30.9) | 86.24 (30.6) | − 0.01 | 0.51 |
| Long | 86.37 (26.9) | 86.14 (27.7) | − 0.01 | 0.68 |
Note: Bold indicates statistical significance (p < .05).
Analyses revealed a significant group by time interaction for average minutes of sedentary time during the workday [F(1,35) = 4.29, p = 0.05, η2 = 0.11]. Sedentary time decreased significantly in the SB group (− 35.57 min; d = − 0.75; p = 0.03), but did not change in the LB group (+ 5.35 min; d = 0.12). There were no significant changes in light or moderate intensity activity during the workday in either group.
We also examined self-reported time in activity breaks based on the activity logs. Among participants who completed the study, participants in the SB group reported standing/moving for an average of 80.3 min per workday, which was significantly greater (p = 0.006) than the 46.3 min of standing/moving per workday reported by participants in the LB group.
3.4. Cardiometabolic health outcomes
Results revealed a main effect approaching significance for total cholesterol [F(1,36) = 3.58, p = 0.07, η2 = 0.09], which declined in both the SB (d = − 0.33) and LB (d = − 0.18) groups. Neither the main effect nor the interaction effect was significant for triglycerides; however, effect sizes revealed a larger decline in the SB group (d = − 0.38, p = 0.06) than the LB group (d = − 0.03, p = 0.81) from baseline to post-intervention. There was a borderline significant interaction effect for fasting blood glucose [F(1,36) = 3.27, p = 0.08, η2 = 0.08], with values decreasing significantly in the SB group (d = − 0.29, p = 0.01) but not the LB group (d = 0.004, p = 0.93). Neither systolic nor diastolic blood pressure changed significantly from baseline to post-intervention, but effect sizes revealed small reductions in the SB group only (d = − 0.23 and d = − 0.21 for systolic and diastolic, respectively). There were no changes in body weight or waist circumference in either group. Overall, effect sizes revealed small positive effects for the assessed health outcomes in the SB group, and no changes in the LB group.
4. Discussion
The purpose of this study was to compare the effects of short, frequent breaks in sitting versus longer, planned breaks in sitting on sedentary behavior and cardiometabolic health among inactive female office employees. In general, results favored the SB group over the LB group. Participants in the SB group demonstrated significant reductions in sedentary time during the workday and small improvements on several of the assessed health outcomes. Further research is needed to understand whether the lack of change in sedentary behavior in the LB group was a function of an impractical goal, an inability of the accelerometer to detect longer bouts of standing, or another issue (e.g., lack of environmental support for longer bouts of standing).
Previous epidemiological (Healy et al., 2008b) and laboratory-based (Dunstan et al., 2012) studies have provided evidence that frequent breaks from prolonged sitting produce favorable changes in cardiometabolic outcomes, but the feasibility of taking frequent breaks during a typical workday in a real-world context has not been examined. In the present study, participants encouraged to stand up and move every 30 min for 1–2 min across an 8-week period significantly reduced their sedentary behavior by approximately 36 min per workday, which was in line with the instruction to reduce daily occupational sitting time by 30 min. Although the changes in cardiometabolic outcomes were modest, participants in the SB group did exhibit improvements in fasting blood glucose, which is encouraging considering the small change in sedentary behavior. Previous intervention studies that have measured cardiometabolic outcomes have largely showed null results, with the exception of isolated improvements in individual variables (i.e., HDL cholesterol (Alkhajah et al., 2012) and waist circumference (Carr et al., 2013)). The current study provides preliminary evidence that a recommendation to take frequent breaks from sitting may lead to favorable changes in health outcomes associated with chronic disease risk.
These results have potential implications for the development of public health messages addressing sedentary behavior. Individuals need to know that taking short, frequent breaks from sitting may be a feasible and effective approach to reducing sedentary time and improving health. Although physical activity recommendations have undergone a gradual shift to include the message that “everything counts,” the dominant discourse still emphasizes MVPA accumulated in bouts of 10 min of greater (Office of Disease Prevention and Health Promotion, 2008). The results of this study do not discount the importance of MVPA; rather, they suggest that sedentary behavior may be a “low hanging fruit” that can be targeted to elicit changes in health with minimal effort. Given the evidence that the greatest improvements in health occur when individuals move from doing no activity to doing some activity (Physical Activity Guidelines Advisory Committee, 2008), messages about the importance of reducing sedentary behavior may be especially relevant to adults who are completely sedentary, both at home and at work.
The fact that a substantial percentage of participants adhered to the recommended protocols is encouraging because the intervention strategies in the current study exclusively targeted individual/motivational variables, which have previously been deemed insufficient on their own for producing significant changes in sedentary behavior (Owen et al., 2011). In other words, a large proportion of participants were able to take consistent activity breaks even without any institutional support or standing desks in place, perhaps due to the accountability fostered by the daily activity logs. Ideally, workplace interventions should augment individual strategies with organizational and environmental changes that modify the social and physical environment to maximize their public health impact (Carnethon et al., 2009, Gardner et al., 2015, Plotnikoff and Karunamuni, 2012). In particular, providing employees height-adjustable desks that facilitate changes in posture throughout the workday has received substantial support (Neuhaus et al., 2014, Tew et al., 2015).
4.1. Limitations
There are a number of limitations to be acknowledged. The informed consent document disclosed the objective of the study; thus, participants were aware that there were two conditions and were not blinded to their treatment group assignment. However, we predicted participants would be more motivated to adhere to their assigned protocol if they understood the purpose of the study. Additionally, there was no true control group with which to compare the two intervention conditions, and we did not reach the target sample size due to recruitment difficulties. The sample was relatively homogenous, so the extent to which these findings would extend to males, active individuals, employees working outside the office setting, employees with rigid daily schedules, or less educated individuals is uncertain. While objective, accelerometers are not an ideal tool for assessing sedentary time because they have difficulty distinguishing between sitting and standing. Future studies should consider using an ActivPAL inclinometer or other device that can recognize differences in posture (Lyden et al., 2012).
Delivering the intervention in a real-world setting did raise questions about how, exactly, participants altered their behavior during the workday. Self-reported adherence to the protocols was similar between groups, but objectively measured sedentary behavior differed significantly. Furthermore, objectively measured light and moderate intensity activity did not change, so it is unclear what replaced sedentary behavior during the workday for the SB group. To minimize burden, participants did not report whether they were standing or walking during their breaks, nor did they report on the strategies used to adhere to the protocols. Future studies should collect this information to better understand the factors driving intervention effects, and should assess sedentary behavior and physical activity outside of work to identify possible compensation effects.
5. Conclusion
In conclusion, results of this study showed that taking short, frequent breaks from sitting during the workday was a feasible and effective approach for reducing sedentary time at work among participating employees. Future studies should complement the individual-level strategies delivered in this intervention with organizational and environmental changes at the worksite level to determine whether greater improvements in sedentary behavior and health outcomes can be achieved.
Abbreviations
- SB
short breaks
- LB
long breaks
- MVPA
moderate-to-vigorous physical activity
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Transparency document
Transparency document.
Acknowledgments
This study was funded by a University Small Research Grant from Kansas State University (USRG-3046). All testing was conducted at the Physical Activity and Nutrition Clinical Research Consortium (PAN-CRC).
Footnotes
The Transparency document associated with this article can be found, in online version.
References
- Alkhajah T.A., Reeves M.M., Eakin E.G., Winkler E.A.H., Owen N., Healy G.N. Sit-stand workstations: a pilot intervention to reduce office sitting time. Am. J. Prev. Med. 2012;43(3):298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- Australian Department of Health Australia's physical activity and sedentary behaviour guidelines. 2014. http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines (Accessed November 2, 2015)
- Canadian Society for Exercise Physiology Canadian physical activity and Canadian sedentary behaviour guidelines. 2011. http://www.csep.ca/en/guidelines/get-the-guidelines (Accessed November 2, 2015)
- Carnethon M., Whitsel L.P., Franklin B.A. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120(17):25–41. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- Carr L.J., Karvinen K., Peavler M., Smith R., Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr L.J., Leonhard C., Tucker S., Fethke N., Benzo R., Gerr F. Total worker health intervention increases activity of sedentary workers. Am. J. Prev. Med. 2015 doi: 10.1016/j.amepre.2015.06.022. [DOI] [PubMed] [Google Scholar]
- Chastin S.F.M., Egerton T., Leask C., Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity. 2015;23:1800–1810. doi: 10.1002/oby.21180. [DOI] [PubMed] [Google Scholar]
- Chau J.Y., van der Pleog H.P., van Uffelen J.G. Are workplace interventions to reduce sitting effective? A systematic review. Am. J. Prev. Med. 2010;51:352–356. doi: 10.1016/j.ypmed.2010.08.012. [DOI] [PubMed] [Google Scholar]
- Church T.S., Thomas D.M., Tudor-Locke C. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemes S.A., OʼConnell S.E., Edwardson C.L. Office workers' objectively measured sedentary behavior and physical activity during and outside working hours. J. Occup. Environ. Med. 2014;56(3):298–303. doi: 10.1097/JOM.0000000000000101. [DOI] [PubMed] [Google Scholar]
- Dunstan D.W., Salmon J., Owen N. Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia. 2005;48:2254–2261. doi: 10.1007/s00125-005-1963-4. [DOI] [PubMed] [Google Scholar]
- Dunstan D.W., Healy G.N., Sugiyama T., Owen N. ‘Too much sitting’ and metabolic risk – has modern technology caught up with us? Eur. Endocrinol. 2010;6:19–23. [Google Scholar]
- Dunstan D.W., Kingwell B.A., Larsen R. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson P.S., Melanson E., Sirard J. Calibration of the computer science and applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Gardner B., Smith L., Lorencatto F., Hamer M., Biddle S.J.H. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2015 doi: 10.1080/17437199.2015.1082146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George E.S., Rosenkranz R.R., Kolt G.S. Chronic disease and sitting time in middle-aged Australian males: findings from the 45 and up study. Int. J. Behav. Nutr. Phys. Act. 2013;10:20. doi: 10.1186/1479-5868-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M.T., Healy G.N., Dunstan D.W., Zderic T.W., Owen N. Too little exercise and too much sitting: inactivity physiology and the need for new recommendations for sedentary behavior. Curr. Cardiol. Risk Rep. 2008;2:292–298. doi: 10.1007/s12170-008-0054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy G.N., Wijndaele K., Dunstan D.W. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- Healy G.N., Dunstan D.W., Salmon J. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk P.T., Church T.S., Craig C.L., Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med. Sci. Sports Exerc. 2009;41:998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- Lyden K., Kozey Keadle S.L., Staudenmayer J.W., Freedson P.S. Validity of two wearable monitors to estimate breaks from sedentary time. Med. Sci. Sports Exerc. 2012;44(11):2243–2252. doi: 10.1249/MSS.0b013e318260c477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews C.E., Chen K.Y., Freedson P.S. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhaus M., Eakin E.G., Straker L. Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obes. Rev. 2014 doi: 10.1111/obr.12201. [DOI] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion Physical activity guidelines for Americans. 2008. http://health.gov/paguidelines/guidelines/ (Accessed November 2, 2015)
- Owen N. Sedentary behavior: understanding and influencing adults' prolonged sitting time. Prev. Med. 2012;55(6):535–539. doi: 10.1016/j.ypmed.2012.08.024. [DOI] [PubMed] [Google Scholar]
- Owen N., Healy G.N., Matthews C.E., Dunstan D.W. Too much sitting: the population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010;38(3):105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen N., Sugiyama T., Eakin E.E., Gardiner P.A., Tremblay M.S., Sallis J.F. Adults' sedentary behavior: determinants and interventions. Am. J. Prev. Med. 2011;41(2):189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- Parry S., Straker L. The contribution of office work to sedentary behavior associated risk. BMC Public Health. 2013;13(1):296. doi: 10.1186/1471-2458-13-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A.V., Bernstein L., Deka A. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am. J. Epidemiol. 2010;172:419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peddie M.C., Bone J.L., Rehrer N.J., Skeaff C.M., Gray A.R., Perry T.L. Breaking up prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am. J. Clin. Nutr. 2013;98:358–366. doi: 10.3945/ajcn.112.051763. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee Physical activity guidelines advisory committee report. 2008. http://health.gov/paguidelines/report/pdf/CommitteeReport.pdf (Accessed November 2, 2015)
- Plotnikoff R., Karunamuni N. Reducing sitting time: the new workplace health priority. Arch. Env. Occup. Health. 2012;67(3):125–127. doi: 10.1080/19338244.2012.697407. [DOI] [PubMed] [Google Scholar]
- Puig-Ribera A., Bort-Roig J., Gonzalez-Suarez A.M. Patterns of impact resulting from a ‘sit less, move more’ web-based program in sedentary office employees. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0122474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders T.J., Larouche R., Colley R.C., Tremblay M.S. Acute sedentary behaviour and markers of cardiometabolic risk: a systematic review of intervention studies. J. Nutr. Metab. 2012;712435 doi: 10.1155/2012/712435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha N., Kukkonen-Harjula K.T., Verbeek J.H., Ijaz S., Hermans V., Bhaumik S. Workplace interventions for reducing sitting at work. Cochrane Database Syst. Rev. 2016;3 doi: 10.1002/14651858.CD010912.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens B.R., Granados K., Zderic T.W., Hamilton M.T., Braun B. Effects of 1 day of inactivity on insulin action in health men and women: interaction with energy intake. Metabolism. 2011;60:941–949. doi: 10.1016/j.metabol.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Tew G.A., Posso M.C., Arundel C.E., McDaid C.M. Systematic review: Height-adjustable workstations to reduce sedentary behaviour in office-based workers. Occup. Med. 2015;65(5):357–366. doi: 10.1093/occmed/kqv044. [DOI] [PubMed] [Google Scholar]
- Thorp A.A., Healy G.N., Winkler E. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int. J. Behav. Nutr. Phys. Act. 2012;9:128. doi: 10.1186/1479-5868-9-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmot E.G., Edwardson C.L., Achana F.A. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.