Abstract
Cyclic-AMP response element-binding protein (CREB) signaling has a critical role in the formation of memories. CREB signaling is dysfunctional in the brains of mouse models of Alzheimer's disease (AD), and evidence suggests that CREB signaling may be disrupted in human AD brains as well. Here, we show that both CREB and its activated form pCREB-Ser133 (pCREB) are reduced in the prefrontal cortex of AD patients. Similarly, the transcription cofactors CREB-binding protein (CBP) and p300 are reduced in the prefrontal cortex of AD patients, indicating additional dysfunction of CREB signaling in AD. Importantly, we show that pCREB expression is reduced in peripheral blood mononuclear cells (PBMC) of AD subjects. In addition, pCREB levels in PBMC positively correlated with pCREB expression in the postmortem brain of persons with AD. These results suggest that pCREB expression in PBMC may be indicative of its expression in the brain, and thus offers the intriguing possibility of pCREB as a biomarker of cognitive function and disease progression in AD.
Introduction
Cyclic-AMP response element binding protein (CREB) has long been known to be important for the formation of memories.1, 2 It is thought that phosphorylation of CREB at Ser-133 (pCREB), followed by the recruitment of critical transcription factors such as CREB-binding protein (CBP) and p300, allows the transcription of genes such as Egr-1 (zif268) which are required for memory formation.3, 4 We and others have shown that CREB signaling is dysfunctional in mouse models of Alzheimer's disease (AD), a disease characterized by cognitive decline and memory impairments.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 However, relatively little work has been carried out to investigate CREB in humans with AD. Two papers have shown that total and activated CREB are reduced in the postmortem hippocampus of individuals with AD, which supports the idea that CREB signaling is defective in AD.17, 18 However, these observations were based exclusively on postmortem brain tissue, which represents an end state. Thus, it remains unclear whether CREB signaling is impaired during disease progression. Moreover, the analysis was confined to the hippocampus and lacked cellular fractionation, which are important considerations for the interpretation of CREB function.19, 20, 21, 22 Most importantly, whether this impairment is echoed peripherally and can be detected in living persons remains unknown. To examine CREB signaling during disease progression, we chose to look at CREB expression in peripheral blood mononuclear cells (PBMC).23 We examined pCREB, Total CREB and CBP in the PBMC of individuals with AD, mild cognitive impairment (MCI) and age- and education-matched, cognitively intact controls. We then compared the expression level of pCREB and CBP in PBMC with the expression level in the brain to determine whether peripheral pCREB or CBP reflects their expression level in the AD brain. First, we observed that Total CREB and pCREB are decreased in the nuclear fraction of postmortem prefrontal cortex (PFC) in individuals with AD when compared with age-matched, cognitively normal controls. We observed a similar reduction in the expression of the transcription cofactors CREB-binding protein (CBP) and p300, which are critical for CREB signaling.24 In support of the significance of this observation, previous research in mice has indicated that deficits in CBP result in cognitive impairments,25, 26, 27 and we have previously reported deficits in both CBP and p300 in a mouse model of AD.6 However, we believe this is the first evidence of diminished CBP or p300 in human AD PFC. We also observed a significant reduction in pCREB and CBP expression in PBMC isolated from AD patients compared with non-AD individuals, and trending reductions, albeit insignificant, in the level of Total CREB and the ratio of pCREB to Total CREB. Importantly, pCREB expression in PBMC positively correlated with pCREB expression in the postmortem PFC, indicating that pCREB expression in the PBMC may be indicative of pCREB expression in the brain in AD. Finally, in contrast to a previous report, we found no association between pCREB expression in the PFC and the severity of amyloid or tau pathology.18 This observation is important because it suggests that reduced pCREB expression in the PFC is not simply a result of increased brain pathology and degeneration. The results presented here show that pCREB is impaired in AD brain and PBMC and offer the exciting possibility that pCREB may be a useful biomarker for cognitive function in AD.
Materials and methods
Participants
Clinical data and biospecimens came from participants in the, MAR, MAP and Religious Orders Study.28, 29 Participants without dementia are recruited from more than 40 Catholic religious groups across the USA. Individuals undergo clinical evaluation, blood draw and brain donation at death. A subset agreed to annual blood draws. The clinical evaluation includes 21 cognitive performance tests which are used to inform on diagnoses of dementia, AD and MCI.30, 31 The follow-up rate exceeds 95% and the autopsy rate exceeds 90%. At the time of death, a neurologist reviews all clinical data and provides a summary diagnosis without access to neuropathologic data. At the time of these analyses, more than 1200 participants had enrolled and more than 600 autopsies obtained. The study was approved by the Institutional Review Board of Rush University Medical Center. All participants signed an informed consent and an Anatomic Gift Act for organ donations. Only female persons were used in this study. Demographic data are summarized in Supplementary Table 1. See Supplementary Methods for description of PBMC and PFC isolation.
Nuclear protein extraction and western blot
Nuclear protein from PBMC and PFC was extracted and analyzed by western blot as previously described.6
Analysis of protein level
Protein levels were normalized using densiometric measurements from ImageJ software by dividing the densiometric value for Total CREB, pCREB, CBP, p300 or PKA by the densiometric value for Lamin. For most of the PBMC samples, nine samples were run per gel; three AD, three MCI and three Normal. For the PFC and the associated PBMC, either five or four samples per AD or Normal group were run per gel. Z-scores were then calculated for the normalized values.32
Statistical analysis
A Shapiro–Wilk test was used to confirm the normality of distribution (GraphPad Prism, La Jolla, CA, USA). To determine sample number, a power analysis was carried out on a preliminary experiment of PFC samples (G*Power). For the PBMC experiments, the PFC sample size was used as a starting point for sample number, and more samples were added as available. For PFC comparisons, a two-tailed, unpaired t-test was used. For PBMC comparisons between Normal, MCI and AD, a one-way analysis of variance was used, and one-tailed, unpaired t-tests were used for secondary analysis. For PBMC comparisons between Non-AD and AD, one-tailed, unpaired t-tests were used. For PBMC and PFC correlations, linear regression was used. For amyloid and tau pathology comparisons, a two-tailed, unpaired t-test was used. For PFC pCREB and pathology correlations, a Pearson test was used.
Results
CREB signaling components are reduced in the PFC of individuals with AD
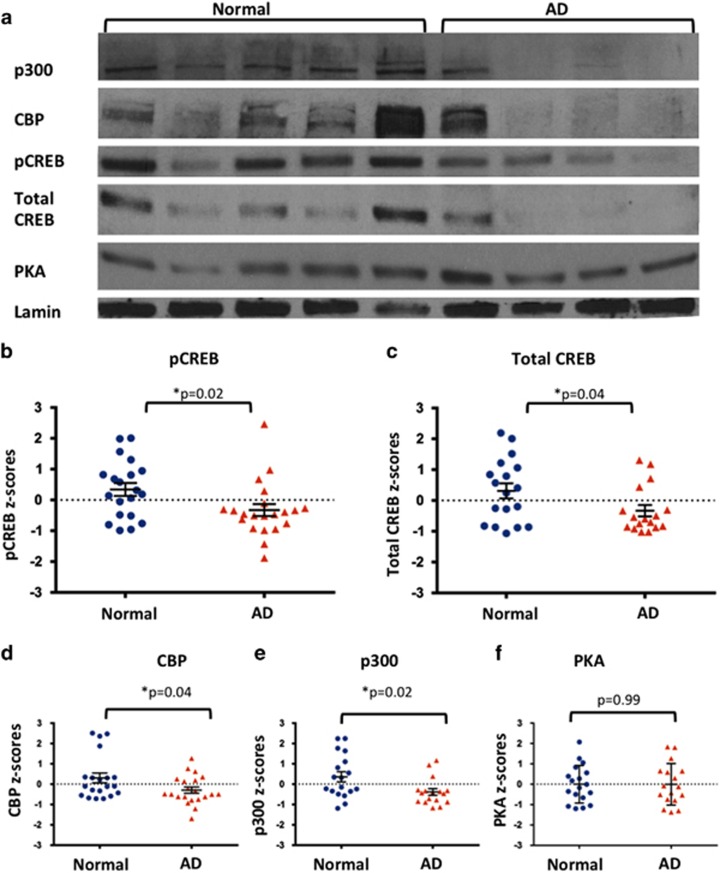
First, we examined the levels of Total CREB, pCREB, CBP, p300 and PKA in the nuclear fraction of postmortem PFC of individuals with a clinical diagnosis of AD and cognitively intact controls matched for age and education. We observed reduced levels of pCREB and Total CREB, in the PFC of AD individuals (Figures 1a and c). These results are in agreement with previously reported observations of Total CREB and pCREB levels in postmortem AD hippocampus.17, 18 However, to our knowledge, this is the first report of reduced Total CREB and pCREB in AD PFC, and suggests that pathology is not confined to the hippocampal formation. In addition to reduced expression of Total CREB and pCREB, we also had the novel observation that CBP and p300, transcription cofactors critical for CREB signaling, are reduced in AD PFC (Figures 1a, d and e). This result suggests that multiple impairments may exist in the CREB signaling components in AD brain as we have previously reported in the APPswe/PS1ΔE9 mouse model of AD.6 These results also suggest that reduced CREB signaling in the AD brain may have a role in cognitive dysfunction in AD. Interestingly, we did not observe reductions in nuclear protein levels of PKA, suggesting that either impaired CREB phosphorylation in AD PFC may not be a sole result of decreased PKA or that PKA expression does not reflect its activity (Figures 1a and f).
Figure 1.
CREB signaling components in AD PFC are lower compared with age- and education-matched, cognitively intact controls (a). Representative western blot image of p300, CBP, pCREB, Total CREB and PKA in human PFC. (b) pCREB expression (normalized to Lamin) in nuclear fractions of PFC of AD individuals and cognitively intact controls (P=0.02). (c) Total CREB expression (normalized to Lamin) in nuclear fractions of PFC of AD individuals and cognitively intact controls (P=0.04) (d). CBP expression (normalized to Lamin) in nuclear fractions of PFC of AD individuals and cognitively intact controls (P=0.04). (e) p300 expression (normalized to Lamin) in nuclear fractions of PFC of AD individuals and cognitively intact controls (P=0.02). (f) PKA expression (normalized to Lamin) in nuclear fractions of PFC of AD individuals and cognitively intact controls (P=0.99). Error bars represent s.e.m. AD, Alzheimer's disease; CBP, CREB-binding protein; CREB, cyclic-AMP response element binding protein; PBMC, peripheral blood mononuclear cells; PFC, prefrontal cortex.
pCREB and CBP are reduced in the PBMC of individuals with AD
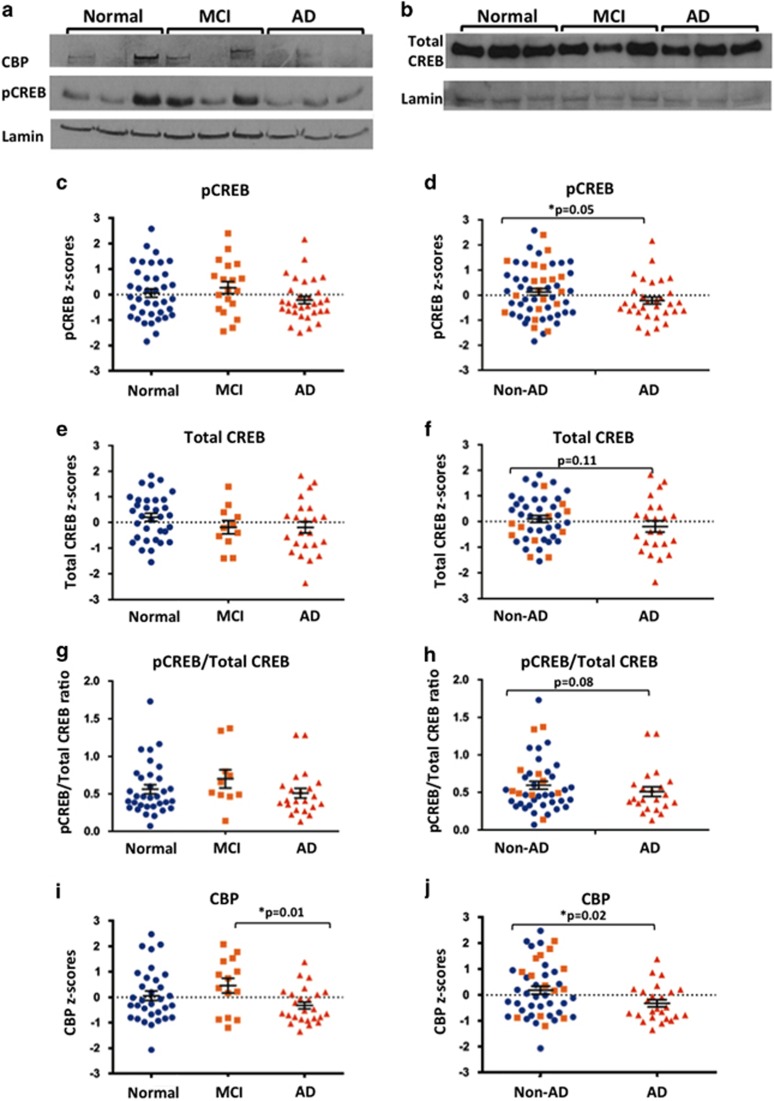
Next, we examined the levels of pCREB, Total CREB and CBP in the PBMC of individuals with clinically diagnosed AD, MCI and age- and education-matched controls to determine whether pCREB, Total CREB and CBP are also reduced in AD PBMC. We observed a nonsignificant reduction in pCREB expression in the PBMC of individuals with AD when compared by a one-way analysis of variance with individuals with MCI or cognitively normal individuals, and observed no difference between PBMC from normal or MCI individuals (Figures 2a and c). To examine whether reduced pCREB is indicative of a definitive AD diagnosis, we examined pCREB expression in PBMC of individuals with AD compared with non-AD. We observed that pCREB level was significantly lower in AD PBMC compared with non-AD PBMC by a one-tailed, unpaired t-test. (Figure 2d). Next, we examined Total CREB in PBMC and observed a trending, but nonsignificant, decrease in Total CREB in AD PBMC when compared with non-AD PBMC (Figures 2e and f). The ratio of pCREB to Total CREB in PBMC also showed a nonsignificant reduction in AD PBMC when compared with non-AD PBMC (Figures 2g and h). These results suggest that reduced pCREB in AD PBMC may be a combination of reduced levels of total protein and impaired phosphorylation. Next, we measured CBP in the PBMC of clinically diagnosed AD patients, MCI or age- and education-matched controls. We observed a significant difference in CBP expression by a one-way analysis of variance, and follow-up analysis revealed that CBP expression was significantly lower in individuals with AD compared with individuals with MCI (Figure 2i). Because we did not observe a difference in CBP expression between normal and MCI, we hypothesized that levels of CBP too are reduced in definitive AD. As with pCREB, we observed that CBP is significantly lower in the PBMC of individuals with AD when compared with individuals without AD (one-tailed, unpaired t-test, Figure 2j). These results suggest for the first time that CREB signaling deficits in the brain may also be apparent systemically, and offers the intriguing possibility that the expression of CREB signaling components in PBMC may be used as a readout for CREB signaling in the brain.
Figure 2.
pCREB and CBP are reduced in AD PBMC. (a) Representative western blot of pCREB and CBP in nuclear fractions of PBMC of AD, MCI and cognitively normal controls. (b) Representative western blot of Total CREB in nuclear fractions of PBMC of AD, MCI and cognitively normal controls. (c) pCREB z-scores of PBMC in Normal, MCI and AD individuals were not different by a one-way analysis of variance (ANOVA) (P=0.20). (d) pCREB is significantly lower in the PBMC of AD individuals compared with non-AD individuals when compared by a one-tailed, unpaired t-test (P=0.05). (e) Total CREB is not significantly different by a one-way ANOVA (P=0.25). (f) Total CREB is not significantly different in AD PBMC when compared with non-AD PBMC by a one-tailed, unpaired t-test (P=0.11). (g) The ratio of pCREB to Total CREB was not significantly different by a one-way ANOVA (P=0.33). (h) The ratio of pCREB to Total CREB was reduced in AD PBMC when compared with non-AD PBMC by a one-tailed, unpaired t-test (P=0.08). (i) CBP z-scores of PBMC in Normal, MCI and AD individuals were significantly different by a one-way ANOVA (P=0.049). Follow-up analysis using a two-tailed, unpaired t-test revealed that CBP is significantly reduced in AD PBMC compared with MCI PBMC (P=0.01). (j) CBP is significantly lower in the PBMC of AD individuals compared with non-AD individuals when compared by a one-tailed, unpaired t-test (P=0.02). Error bars represent s.e.m. AD, Alzheimer's disease; CBP, CREB-binding protein; CREB, cyclic-AMP response element binding protein; MCI, mild cognitive impairment; PBMC, peripheral blood mononuclear cells; PFC, prefrontal cortex.
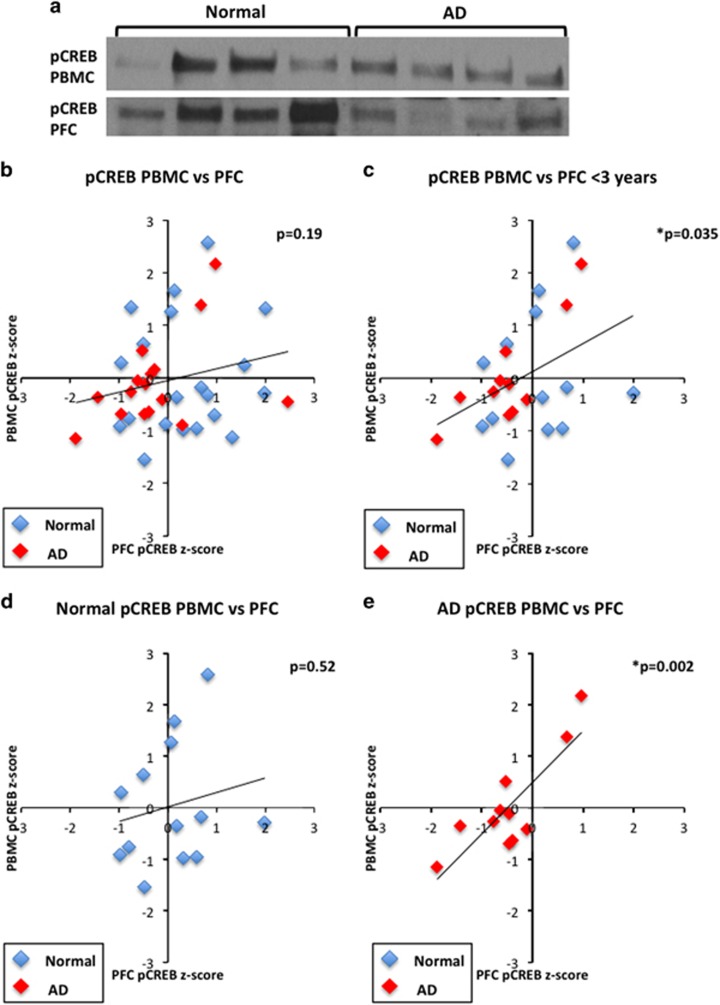
Association of pCREB in PBMC with pCREB in brain PFC
To address the possibility that CREB signaling components in the PBMC might be indicative of CREB signaling in the brain, we compared pCREB and CBP in PBMC of AD or cognitively intact individuals with pCREB and CBP of the corresponding postmortem PFC. For this purpose, we used PBMC and PFC from 20 normal and 21 AD individuals (Figure 3a). We observed a weak positive correlation between pCREB expression in PBMC and expression in the brain by a linear regression analysis (Figure 3b). However, the PBMC in this experiment were isolated as many as 4–5 years prior to death, and thus temporally mismatched with brain readout. We hypothesized that by narrowing the interval between blood sample draw and death, we might observe a stronger relationship between expression in the blood and expression in the brain. Therefore, we performed an additional analysis in which PBMC that were drawn from patients 3 years or less from the time of death (that is, time of postmortem brain collection; 13 normal and 11 AD) were included. We observed a significant positive correlation by a linear regression analysis between pCREB expression in the PBMC and pCREB expression in the PFC for all samples, when the time interval between PBMC sample draw and postmortem brain sample collection was less than 3 years (Figure 3c). Examining the association between pCREB expression in PBMC and brain of cognitively intact individuals revealed weak correlation (Figure 3d). However, a very strong positive correlation was observed in the AD individuals (Figure 3e). These results strongly suggest that pCREB in the PBMC reflects pCREB signaling in the brain, and that this correlation is particularly strong in AD. These results suggest that pCREB in PBMC may serve as a noninvasive marker for pCREB expression in the brain.
Figure 3.
pCREB expression in PBMC correlates with pCREB expression in PFC. (a) Representative blot showing expression of pCREB in PBMC and PFC in the same individuals. (b) pCREB in the PBMC is weakly correlated with pCREB expression in the PFC (P=0.19). (c) Linear regression analysis revealed that pCREB expression in PBMC correlates with pCREB expression in the PFC when the temporal interval between blood and brain sample is <3 years (P=0.035). (d, e) No correlation is observed in cognitively normal individuals between PFC pCREB and PBMC pCREB (d; P=0.52). However, a strong positive correlation exists between PFC pCREB and PBMC pCREB in the AD individuals (e; P=0.002). AD, Alzheimer's disease; CREB, cyclic-AMP response element binding protein; PBMC, peripheral blood mononuclear cells; PFC, prefrontal cortex.
Association of CBP in PBMC with CBP in brain PFC
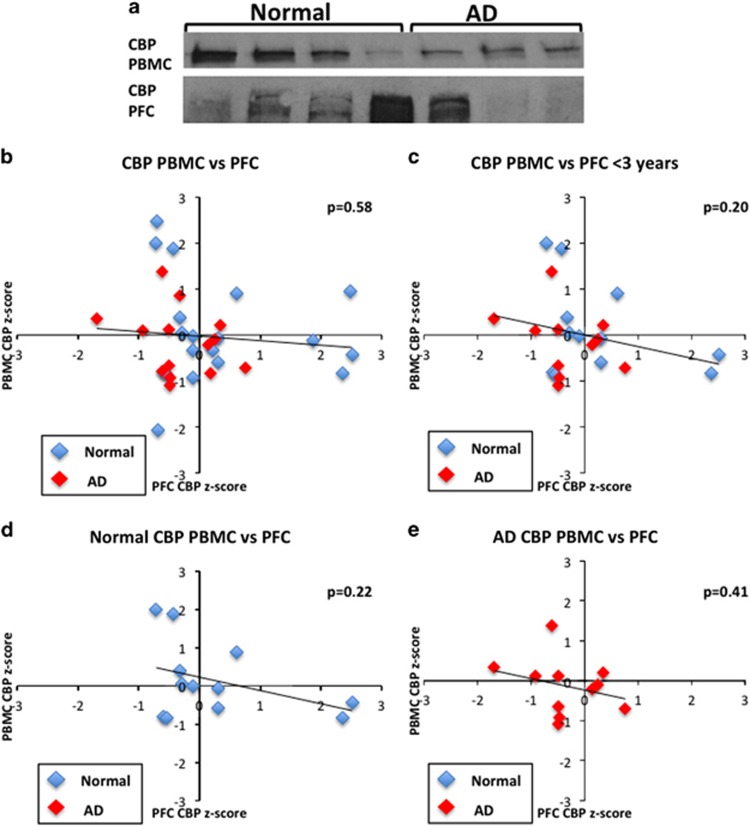
We also compared CBP expression in the PBMC with CBP expression in the PFC (Figure 4a). We observed no correlation between PBMC CBP and PFC CBP (Figure 4b). Analysis of PBMC samples drawn within 3 years prior to death (Figure 4c) as well as analyzing the correlation inside diagnostic group, that is, in normal individuals or in AD patients (Figures 4d and e) revealed no correlation between CBP in PBMC and in PFC. This result suggests that whereas CBP may be independently reduced in both PFC and PBMC in AD, the relationship between PBMC and PFC on an individual level is not correlative at our sample size.
Figure 4.
CBP expression in PBMC is not related to CBP expression in the PFC. (a) Representative blot showing expression of CBP in PBMC and PFC in the same individuals (b). CBP expression in the PBMC is not correlated with expression in the PFC by a Pearson correlation (P=0.58). (c) CBP expression in PBMC drawn less than 3 years prior to death is weakly correlated with CBP expression in the PFC (P=0.20). (d, e) When the data are split into cognitively normal and AD individuals, weak negative correlations are observed between PFC CBP and PBMC CBP in cognitively normal individuals (d; P=0.22) and AD individuals (e; P=0.41). AD, Alzheimer's disease; CBP, cyclic-AMP response element-binding protein-binding protein; PBMC, peripheral blood mononuclear cells; PFC, prefrontal cortex.
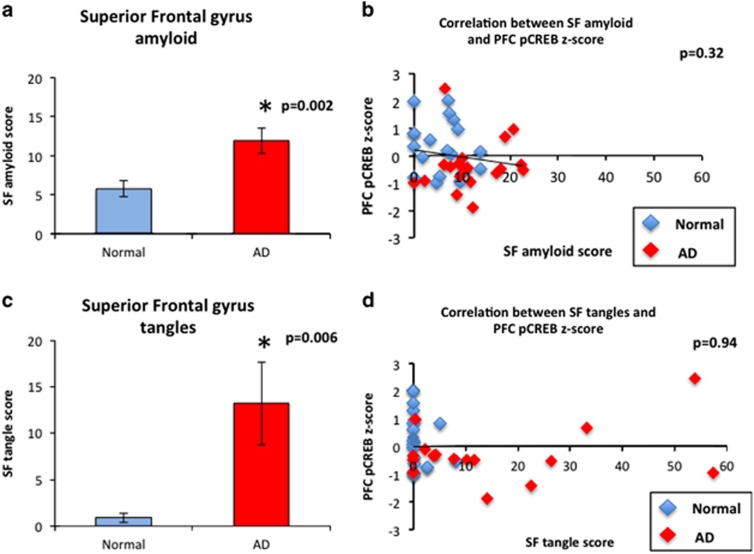
pCREB expression in the PFC does not correlate with pathological hallmarks of AD
We have previously shown that deficits in CREB signaling precede onset of amyloid deposition in a mouse model of AD.6 Thus, we hypothesized that the deficits in CREB signaling are not necessarily the result of advanced AD pathology. To examine this hypothesis in the human disease, we compared pCREB expression in the PFC with amyloid and tau pathology scores for the entire brain and for the superior frontal gyrus. Although we observed increased pathology in the AD group (Figures 5a and c), we did not observe a relationship between either amyloid or tau pathology and PFC pCREB expression by a Pearson correlation analysis (Figures 5b and d, Supplementary Figure 1). These results support the hypothesis that dysfunctional CREB signaling in AD is not simply the result of increased amyloid or tau pathology, in contrast to a previous report,18 and offers the intriguing possibility that CREB signaling components may serve as novel, accessible markers of cognitive function and disease progression.
Figure 5.
PFC pCREB expression is not associated with severity of local amyloid or tau pathology. (a) Amyloid counts are higher in the superior frontal gyrus (SFG) of AD compared with cognitively normal SFG (P=0.002). (b) pCREB in the PFC is not correlated with severity of amyloid pathology in SFG by a Pearson correlation (P=0.32). (c) Tangle counts are higher in the postmortem SFG of AD compared with cognitively normal (P=0.006). (d) pCREB in the PFC is not correlated with severity of tangle pathology in the SFG by a Pearson correlation (P=0.94). AD, Alzheimer's disease; CREB, Cyclic-AMP response element-binding protein; PFC, prefrontal cortex.
Discussion
In this study, we have made several novel observations and suggest that they are mechanistically and diagnostically indicative of AD. First, we confirmed an earlier observation that Total CREB and pCREB are decreased in postmortem AD brain.17, 18 We have also made the novel observation that in addition to previous reports of lower postmortem pCREB and Total CREB in the hippocampus, this deficit is also present in the PFC. The PFC is vulnerable to neurodegeneration in AD,33, 34, 35, 36 and enhancing CREB phosphorylation in the brain through phosphodiesterase inhibitors has been shown to improve performance in PFC-dependent memory tasks in macaques.37 Our data suggest that one mechanism underlying cognitive impairment in AD may be reduced CREB signaling. It should be noted that levels of CREB and pCREB in postmortem PFC samples represent steady state levels of these proteins, rather than activity-dependent expression. This observation supports our previous finding in a mouse model of familial AD, where pCREB levels were reduced at steady state and following learning, compared with wild-type counterparts. These results suggest that CREB impairments in AD are not restricted to active learning, and a reduction in availability of CREB signaling components may be a feature of AD contributing to cognitive dysfunction.6
Furthermore, we are the first to report that the CREB transcription cofactors CBP and p300 are reduced in the postmortem AD brain. CBP recruitment following CREB activation is a critical event in facilitating the CRE-based gene transcription thought to underlie the formation of long-term memory, and enhancing CBP has been previously shown to rescue cognitive deficits in a mouse model of AD.11, 25 Dysregulation of CBP may contribute to the abnormal epigenetic regulation of immediate early genes in the PFC.38 Our observation that CBP is reduced in AD PFC strengthens the evidence that CREB signaling is dysfunctional in AD, and offers another potential therapeutic target for the treatment of AD. Our observation that protein levels of p300 are reduced in AD PFC is intriguing in light of the fact that p300 has been hypothesized to be overactive in its function of acetylating tau in AD.39, 40, 41 We cannot exclude the possibility that protein expression of p300 may not be indicative of its activity level, and future experiments will determine the nature of p300 dysfunction in AD.
Interestingly, we did not observe deficits in PKA expression in AD PFC. This may suggest that either the impairments in CREB phosphorylation cannot be solely attributed to PKA activity or that PKA protein expression does not faithfully reflect its activity. CREB is a substrate for many kinases, including PKC, CaMKII, CaMKIV, MSK and RSK.42 Therefore, the source of impaired CREB phosphorylation in AD PFC remains an open question for further investigation.
Next, we show that pCREB and CBP expression is significantly reduced in PBMC of AD patients. Examination of CREB expression in PBMC offers a noninvasive route for monitoring its signaling in the brain and thus perhaps cognitive functioning. We therefore asked whether Total CREB, pCREB and CBP were also reduced in the PBMC of individuals with AD as they are in the PFC. We observed that levels of pCREB and CBP in the PBMC of individuals with AD were significantly reduced compared with the non-AD samples. These data suggest that the reduction in CREB and CBP expression may be tied to the onset of AD, rather than general cognitive impairments. We did observe high variability in our PBMC analysis. One explanation for this may be that many of the individuals in our PBMC analysis are still alive, and we cannot rule out the possibility that the individuals in the normal or MCI groups may yet develop AD or other neurodegenerative disease. Future experiments should examine a time course of samples drawn from the same individual over time to determine whether pCREB and CBP decline following the onset of AD. In addition, we observed a trending reduction in Total CREB expression in AD PBMC, as well as a trending reduction in the ratio of pCREB to Total CREB. These results suggest that the reduction in pCREB in AD PBMC may be a result of both reduced levels of Total CREB and impairments in phosphorylation. Additional experiments will be necessary to determine the cause of impaired phosphorylation in AD PBMC, and whether this mechanism is autonomous. One possible mechanism for the impairments in CREB phosphorylation is through kinase function. CREB in PBMC responds to many of the same kinases as neuronal CREB (for review, see Kuo and Leiden43), suggesting the possibility of common regulatory pathways. For example, granulocyte-macrophage colony-stimulating factor has been shown to activate CREB in leukocytes via RSK.44 Interestingly, peripheral administration of granulocyte-macrophage colony-stimulating factor to a mouse model of AD has been shown to improve cognitive function.45 Similarly, mice deficient in CaMKIV not only exhibit impairments in memory, but also exhibit impaired CREB phosphorylation in T cells.46, 47 Therefore, impairments in kinase function may be a possible mechanism underlying dysregulation of CREB phosphorylation in both blood and brain. In addition, we cannot exclude the possibility that brain-derived factors may have a role in CREB metabolism in PBMC.
Importantly, we observed a positive correlation between pCREB expression in PFC samples and temporally matched blood samples. This correlation was particularly strong in AD individuals. This analysis provides the first evidence that pCREB expression in PBMC may be correlated with pCREB expression in the brain. Thus, it appears that impairments in pCREB in AD may be a long-lasting phenomenon. More experiments are warranted to determine the predictive power of pCREB as a blood biomarker for cognitive dysfunction in AD.
We also analyzed the relationship of CBP expression in the PBMC and PFC. In these analyses, we did not observe a significant relationship between PBMC and PFC CBP. However, it is clear from our data that a great deal of variability exists in the CBP samples and therefore this phenomenon may be explained by sample size too low to account for the variability in the samples. Indeed, we did not observe a significant reduction in CBP in our primary analysis of normal PBMC compared with AD PBMC, and only observed a significant difference when we combined the normal and MCI individuals for higher power. Therefore, although it appears that a negative correlation exists between PFC CBP and PBMC CBP in the normal and AD groups when analyzed separately, the overall correlation may be too weakly powered to draw definitive correlations when analyzing across groups.
Finally, we did not observe a correlation between amyloid or tau pathology and pCREB expression in the PFC. This observation is important because it suggests that declining pCREB expression is not simply the result of increased AD pathology. Although it has been proposed that amyloid and tau may interact with CREB signaling components,18, 40, 48, 49 our experiments in a mouse model of AD suggest that CREB signaling components may be dysfunctional prior to the onset of amyloid deposition and neurofibrillary tangles, and therefore the cause of CREB dysfunction may be independent of theses lesions.6 Similarly, enhancing CBP in a mouse model of AD is able to rescue cognitive function without affecting pathology.11 Indeed, it is well known that the severity of AD pathology is poorly associated with cognitive function during life.50, 51 Therefore, the fact that we do not observe a correlation between pathology and pCREB might mean that pCREB could be more indicative of cognitive function than severity of pathology. In summary, the results presented here offer an exciting start for further studies examining CREB signaling in AD, as well as offer a novel candidate for a blood biomarker to monitor cognitive functioning in AD.
Acknowledgments
The study was supported by NIH grants R01AG033570 (OL), P30AG10161, RF1AG15819, R01AG17917 (DAB), PECTS Award CCTS Pre-doctoral Education (NB).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
Supplementary Material
References
- Yin JC, Wallach JS, Del Vecchio M, Wilder EL, Zhou H, Quinn WG et al. Induction of a dominant negative CREB transgene specifically blocks long-term memory in Drosophila. Cell 1994; 79: 49–58. [DOI] [PubMed] [Google Scholar]
- Kandel ER. The molecular biology of memory: cAMP, PKA, CRE, CREB-1, CREB-2, and CPEB. Mol Brain 2012; 5: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones MW, Errington ML, French PJ, Fine A, Bliss TV, Garel S et al. A requirement for the immediate early gene Zif268 in the expression of late LTP and long-term memories. Nat Neurosci 2001; 4: 289–296. [DOI] [PubMed] [Google Scholar]
- Lakhina V, Arey RN, Kaletsky R, Kauffman A, Stein G, Keyes W et al. Genome-wide functional analysis of CREB/long-term memory-dependent transcription reveals distinct basal and memory gene expression programs. Neuron 2015; 85: 330–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu YS, Long N, Pigino G, Brady ST, Lazarov O. Molecular mechanisms of environmental enrichment: impairments in Akt/GSK3beta, neurotrophin-3 and CREB signaling. PLoS One 2013; 8: e64460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartolotti N, Segura L, Lazarov O. Diminished CRE-induced plasticity is linked to memory deficits in familial Alzheimer's disease mice. J Alzheimers Dis 2015; 50: 477–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saura CA, Choi SY, Beglopoulos V, Malkani S, Zhang D, Shankaranarayana Rao BS et al. Loss of presenilin function causes impairments of memory and synaptic plasticity followed by age-dependent neurodegeneration. Neuron 2004; 42: 23–36. [DOI] [PubMed] [Google Scholar]
- Marambaud P, Wen PH, Dutt A, Shioi J, Takashima A, Siman R et al. A CBP binding transcriptional repressor produced by the PS1/epsilon-cleavage of N-cadherin is inhibited by PS1 FAD mutations. Cell 2003; 114: 635–645. [DOI] [PubMed] [Google Scholar]
- Francis YI, Stephanou A, Latchman DS. CREB-binding protein activation by presenilin 1 but not by its M146L mutant. Neuroreport 2006; 17: 917–921. [DOI] [PubMed] [Google Scholar]
- Francis YI, Diss JK, Kariti M, Stephanou A, Latchman DS. p300 activation by Presenilin 1 but not by its M146L mutant. Neurosci Lett 2007; 413: 137–140. [DOI] [PubMed] [Google Scholar]
- Caccamo A, Maldonado MA, Bokov AF, Majumder S, Oddo S. CBP gene transfer increases BDNF levels and ameliorates learning and memory deficits in a mouse model of Alzheimer's disease. Proc Natl Acad Sci USA 2010; 107: 22687–22692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YM, Huang XW, Zhang YW, Rockenstein E, Bu GJ, Golde TE et al. Alzheimer's beta-secretase (BACE1) regulates the cAMP/PKA/CREB pathway independently of beta-amyloid. J Neurosci 2012; 32: 11390–11395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimoto I, Okamoto T, Matsuura Y, Takahashi S, Okamoto T, Murayama Y et al. Alzheimer amyloid protein precursor complexes with brain GTP-binding protein G(o). Nature 1993; 362: 75–79. [DOI] [PubMed] [Google Scholar]
- Wang RS, Zhang YW, Sun P, Liu RZ, Zhang X, Zhang X et al. Transcriptional regulation of PEN-2, a key component of the gamma-secretase complex, by CREB. Mol Cell Biol 2006; 26: 1347–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dineley KT, Westerman M, Bui D, Bell K, Ashe KH, Sweatt JD. Beta-amyloid activates the mitogen-activated protein kinase cascade via hippocampal alpha7 nicotinic acetylcholine receptors: In vitro and in vivo mechanisms related to Alzheimer's disease. J Neurosci 2001; 21: 4125–4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller M, Cardenas C, Mei L, Cheung KH, Foskett JK. Constitutive cAMP response element binding protein (CREB) activation by Alzheimer's disease presenilin-driven inositol trisphosphate receptor (InsP3R) Ca2+ signaling. Proc Natl Acad Sci USA 2011; 108: 13293–13298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto-Sasaki M, Ozawa H, Saito T, Rosler M, Riederer P. Impaired phosphorylation of cyclic AMP response element binding protein in the hippocampus of dementia of the Alzheimer type. Brain Res 1999; 824: 300–303. [DOI] [PubMed] [Google Scholar]
- Pugazhenthi S, Wang M, Pham S, Sze CI, Eckman CB. Downregulation of CREB expression in Alzheimer's brain and in Abeta-treated rat hippocampal neurons. Mol Neurodegener 2011; 6: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cammarota M, Paratcha G, Bevilaqua LRM, de Stein ML, Lopez M, de Iraldi AP et al. Cyclic AMP-responsive element binding protein in brain mitochondria. J Neurochem 1999; 72: 2272–2277. [DOI] [PubMed] [Google Scholar]
- Vianna MRM, Izquierdo LA, Barros DM, Ardenghi P, Pereira P, Rodrigues C et al. Differential role of hippocampal cAMP-dependent protein kinase in short- and long-term memory. Neurochem Res 2000; 25: 621–626. [DOI] [PubMed] [Google Scholar]
- Cammarota M, Bevilaqua LRM, Ardenghi P, Paratcha G, de Stein ML, Izquierdo I et al. Learning-associated activation of nuclear MAPK, CREB and Elk-1, along with Fos production, in the rat hippocampus after a one-trial avoidance learning: abolition by NMDA receptor blockade. Mol Brain Res 2000; 76: 36–46. [DOI] [PubMed] [Google Scholar]
- Crino P, Khodakhah K, Becker K, Ginsberg S, Hemby S, Eberwine J. Presence and phosphorylation of transcription factors in developing dendrites. Proc Natl Acad Sci USA 1998; 95: 2313–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch JM, Hinze-Selch D, Stingele K, Huchzermeier C, Goder R, Seeck-Hirschner M et al. Changes in CREB phosphorylation and BDNF plasma levels during psychotherapy of depression. Psychother Psychosom 2009; 78: 187–192. [DOI] [PubMed] [Google Scholar]
- Arias J, Alberts AS, Brindle P, Claret FX, Smeal T, Karin M et al. Activation of cAMP and mitogen responsive genes relies on a common nuclear factor. Nature 1994; 370: 226–229. [DOI] [PubMed] [Google Scholar]
- Lopez-Atalaya JP, Ciccarelli A, Viosca J, Valor LM, Jimenez-Minchan M, Canals S et al. CBP is required for environmental enrichment-induced neurogenesis and cognitive enhancement. EMBO J 2011; 30: 4287–4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett RM, Malvaez M, Kramar E, Matheos DP, Arrizon A, Cabrera SM et al. Hippocampal focal knockout of CBP affects specific histone modifications, long-term potentiation, and long-term memory. Neuropsychopharmacology 2011; 36: 1545–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alarcon JM, Malleret G, Touzani K, Vronskaya S, Ishii S, Kandel ER et al. Chromatin acetylation, memory, and LTP are impaired in CBP+/- mice: A model for the cognitive deficit in Rubinstein-Taybi syndrome and its amelioration. Neuron 2004; 42: 947–959. [DOI] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Arvanitakis Z, Wilson RS. Overview and findings from the religious orders study. Curr Alzheimer Res 2012; 9: 628–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Buchman AS, Barnes LL, Boyle PA, Wilson RS. Overview and findings from the rush Memory and Aging Project. Curr Alzheimer Res 2012; 9: 646–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DA, Wilson RS, Schneider JA, Evans DA, Beckett LA, Aggarwal NT et al. Natural history of mild cognitive impairment in older persons. Neurology 2002; 59: 198–205. [DOI] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Aggarwal NT, Arvanitakis Z, Shah RC, Kelly JF et al. Decision rules guiding the clinical diagnosis of Alzheimer's disease in two community-based cohort studies compared to standard practice in a clinic-based cohort study. Neuroepidemiology 2006; 27: 169–176. [DOI] [PubMed] [Google Scholar]
- Cheadle C, Vawter MP, Freed WJ, Becker KG. Analysis of microarray data using Z score transformation. J Mol Diagn 2003; 5: 73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salat DH, Kaye JA, Janowsky JS. Selective preservation and degeneration within the prefrontal cortex in aging and Alzheimer disease. Arch Neurol-Chicago 2001; 58: 1403–1408. [DOI] [PubMed] [Google Scholar]
- van Veluw SJ, Sawyer EK, Clover L, Cousijn H, De Jager C, Esiri MM et al. Prefrontal cortex cytoarchitecture in normal aging and Alzheimer's disease: a relationship with IQ. Brain Struct Funct 2012; 217: 797–808. [DOI] [PubMed] [Google Scholar]
- DeKosky ST, Scheff SW. Synapse loss in frontal cortex biopsies in Alzheimer's disease: correlation with cognitive severity. Ann Neurol 1990; 27: 457–464. [DOI] [PubMed] [Google Scholar]
- Grady CL, Furey ML, Pietrini P, Horwitz B, Rapoport SI. Altered brain functional connectivity and impaired short-term memory in Alzheimer's disease. Brain 2001; 124(Pt 4): 739–756. [DOI] [PubMed] [Google Scholar]
- Rutten K, Basile JL, Prickaerts J, Blokland A, Vivian JA. Selective PDE inhibitors rolipram and sildenafil improve object retrieval performance in adult cynomolgus macaques. Psychopharmacology 2008; 196: 643–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickx A, Pierrot N, Tasiaux B, Schakman O, Kienlen-Campard P, De Smet C et al. Epigenetic regulations of immediate early genes expression involved in memory formation by the amyloid precursor protein of Alzheimer disease. PLoS One 2014; 9: e99467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min SW, Cho SH, Zhou Y, Schroeder S, Haroutunian V, Seeley WW et al. Acetylation of tau inhibits its degradation and contributes to tauopathy. Neuron 2010; 67: 953–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min SW, Chen X, Tracy TE, Li Y, Zhou Y, Wang C et al. Critical role of acetylation in tau-mediated neurodegeneration and cognitive deficits. Nat Med 2015; 21: 1154–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aubry S, Shin W, Crary JF, Lefort R, Qureshi YH, Lefebvre C et al. Assembly and interrogation of Alzheimer's disease genetic networks reveal novel regulators of progression. PLoS One 2015; 10: e0120352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonze BE, Ginty DD. Function and regulation of CREB family transcription factors in the nervous system. Neuron 2002; 35: 605–623. [DOI] [PubMed] [Google Scholar]
- Kuo CT, Leiden JM. Transcriptional regulation of T lymphocyte development and function. Annu Rev Immunol 1999; 17: 149–187. [DOI] [PubMed] [Google Scholar]
- Kwon EM, Raines MA, Blenis J, Sakamoto KM. Granulocyte-macrophage colony-stimulating factor stimulation results in phosphorylation of cAMP response element-binding protein through activation of pp90RSK. Blood 2000; 95: 2552–2558. [PubMed] [Google Scholar]
- Boyd TD, Bennett SP, Mori T, Governatori N, Runfeldt M, Norden M et al. GM-CSF upregulated in rheumatoid arthritis reverses cognitive impairment and amyloidosis in Alzheimer mice. J Alzheimers Dis 2010; 21: 507–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KA, Means AR. Defective signaling in a subpopulation of CD4(+) T cells in the absence of Ca2+/calmodulin-dependent protein kinase IV. Mol Cell Biol 2002; 22: 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takao K, Tanda K, Nakamura K, Kasahara J, Nakao K, Katsuki M et al. Comprehensive behavioral analysis of calcium/calmodulin-dependent protein kinase IV knockout mice. Plos One 2010; 5: e9460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu HL, Jin XX, Yin XM, Jin NN, Liu F, Qian W. PKA-CREB signaling suppresses Tau transcription. J Alzheimers Dis 2015; 46: 239–248. [DOI] [PubMed] [Google Scholar]
- Zhang ZH, Xi GM, Li WC, Ling HY, Qu P, Fang XB. Cyclic-AMP response element binding protein and tau are involved in the neuroprotective mechanisms of nerve growth factor during focal cerebral ischemia/reperfusion in rats. J Clin Neurosci 2010; 17: 353–356. [DOI] [PubMed] [Google Scholar]
- Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R et al. Physical basis of cognitive alterations in Alzheimer's disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol 1991; 30: 572–580. [DOI] [PubMed] [Google Scholar]
- Mesulam NM. Neuroplasticity failure in Alzheimer's disease: Bridging the gap between plaques and tangles. Neuron 1999; 24: 521–529. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.