Abstract
Background
Symptoms of anxiety and depression are prevalent in older adults.
Aims
To compare clinician-guided and self-guided versions of a transdiagnostic internet-delivered cognitive–behavioural therapy (iCBT) intervention for adults aged 60 years and above.
Method
Adults (n=433) with symptoms of anxiety and depression were randomly allocated to: (1) clinician-guided treatment (n=153); (2) initial clinician interview followed by self-guided treatment (n=140); or (3) self-guided treatment without interview (n=140).
Results
Large reductions (d ≥1.00) in symptoms of depression and anxiety were observed across groups, and sustained at follow-up. No differences were observed in clinical outcomes or satisfaction ratings. Age did not affect outcomes.
Conclusions
Carefully developed iCBT interventions may significantly reduce symptoms of anxiety and depression in older adults when delivered in either clinician-guided or self-guided formats.
Declaration of interest
N.T. and B.F.D. developed the Wellbeing Plus Course but derive no financial benefit from it.
Copyright and usage
© 2016 The Royal College of Psychiatrists. This is an open access article distributed under the terms of the Creative Commons Non-Commercial, No Derivatives (CC BY-NC-ND) licence.
Clinical and subclinical levels of depression and anxiety are common in older adults,1–3 and are associated with reduced quality of life, increased disability and increased risk of suicide.4 Treatments such as cognitive–behavioural therapy (CBT) are known to be effective,5,6 but only a small proportion of older people with depression and anxiety seek or receive evidence-based treatment.7,8 Barriers to care include stigma, costs of treatment, mobility limitations and the limited number of trained therapists, which can all be reduced using internet-delivered CBT (iCBT).9 iCBT can be supported by a clinician, provided as a self-guided treatment with an initial interview followed by monitoring of outcomes, or provided in a fully automated manner without contact or monitoring. In studies conducted to date, clinician-guided iCBT has been associated with superior outcomes relative to self-guided and fully automated iCBT.10 However, recently developed self-guided iCBT, which include automated prompts and other strategies designed to increase completion rates, has shown levels of clinical improvement equivalent to clinician-guided treatment.11–15 Whereas several studies have demonstrated the efficacy of iCBT in treating anxiety and depression in older adults,16–22 there have been no trials directly comparing guided and self-guided iCBT with this population. The comparison is warranted because we do not know whether older adults require additional support to benefit from self-guided iCBT, which can in turn affect the cost of making this treatment widely available.
The present study compared the efficacy and acceptability of an iCBT intervention delivered with varying levels of clinician guidance. The Wellbeing Plus Course is a transdiagnostic intervention designed for adults aged 60 years and above with anxiety or depression. Participants were randomised to clinician-guided or self-guided iCBT groups, with the latter receiving either an orientation interview or no interview. It was hypothesised that all groups would report significant improvements on measures of anxiety and depression but that the clinician-guided group would obtain superior outcomes, and that the outcomes of the self-guided group which received an orientation interview would be superior to the other self-guided group. It was also hypothesised that outcomes would be maintained from post-treatment to 3-month follow-up.
Method
Participants
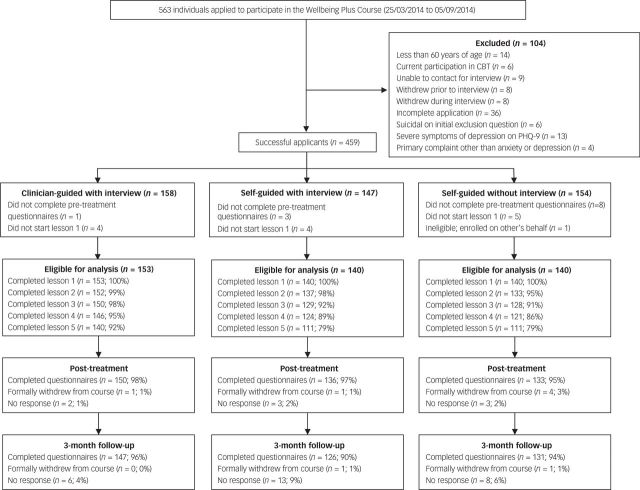
The study was promoted in newspapers and online, and participants were recruited via a specialist research unit (www.ecentreclinic.org) that provides information about common mental and chronic health conditions and offers free psychological treatment via participation in clinical trials. The CONSORT flowchart for the trial is displayed in Fig. 1. A total of 563 individuals applied to participate in the study and 459 met the criteria for inclusion. The inclusion criteria were: (a) resident of Australia, (b) at least 60 years of age and (c) a principal complaint of symptoms of anxiety or depression. The exclusion criteria were: (a) current participation in CBT and (b) very severe symptoms of depression (defined as a total score ≥24 or responding >2 to Question 9 on the 9-item Patient Health Questionnaire (PHQ-9).23 Questions pertaining to the inclusion and exclusion criteria were assessed via an online application form.
Fig. 1. Participant flow from application to 3-month follow-up. CBT, cognitive–behavioural therapy; PHQ-9, 9-item Patient Health Questionnaire.
Applicants meeting inclusion criteria were randomly allocated at the point of application to one of three treatment groups, using a permuted block randomisation sequence generated by B.F.D.: (a) interview plus clinician-guided group (iCG; n=158); (b) interview plus self-guided group (iSG; n=147); or (c) self-guided group (SG; n=154). The randomisation sequence was created by B.F.D. using an online randomiser (www.random.org) and participant randomisation occurred at the point of application, via the eCentreClinic software system, before participants had any contact with the researchers or the researchers had the opportunity to review the details of participants’ applications. Thus, the researchers were masked to group allocation until the participant was deemed to have made a successful or unsuccessful application. The study was approved by the Human Research Ethics Committee (HREC) of Macquarie University, Sydney, Australia, and the trial was registered on the Australian and New Zealand Clinical Trials Registry (ANCZTR) as ACTRN12613000958785.
Design and measures
The study employed a three-arm CONSORT-revised compliant randomised controlled trial (RCT) comparing an internet-delivered treatment for older adults provided with three levels of support. The researchers sought to recruit at least 450 participants, which, with alpha set at 0.05 and a power of 0.80, would enable the detection of small effect size differences (i.e. Cohen’s d>0.35) between groups. All outcome measures were collected via online questionnaires. The primary measures of anxiety and depression were administered weekly to monitor participants’ progress and safety throughout treatment. The secondary and tertiary measures were administered at pre-treatment, post-treatment and 3-month follow-up, and the acceptability and satisfaction questions were administered post-treatment.
Primary measures
Two primary measures were used to assess the presence and severity of depression and anxiety: the PHQ-9, a 9-item measure of the presence and severity of symptoms of depression, based on the DSM-IV diagnostic criteria for major depressive disorder;23 and the 7-item Generalised Anxiety Disorder scale (GAD-7), a 7-item measure of the presence and severity of symptoms of general anxiety, which is based on the DSM-IV diagnostic criteria for GAD.24
Secondary measures
Two secondary measures were used: the Geriatric Depression Scale (GDS), a 15-item short-form screening measure for the assessment and detection of depression among older adults. The GDS employs a simple ‘Yes’ or ‘No’ response, and places less emphasis on the somatic symptoms of depression, which are often confounded in older adults by other physical conditions.25 The 10-item Kessler Psychological Distress Scale (K-10) was used to measure general psychological distress, with total scores ≥22 associated with a diagnosis of anxiety and depressive disorders.26
Tertiary measures
Two tertiary measures were used: the Sheehan Disability Scale (SDS), a 3-item measure of disability and functional impairment in work, study, social life and family life and household responsibilities,27 and the Satisfaction with Life Scale (SWLS), a 5-item measure of judgements of subjective well-being.28
Acceptability and satisfaction
Treatment satisfaction and acceptability were assessed at post-treatment using two questions taken from other studies: (1) ‘Would you feel confident in recommending this course?’ and (2) ‘Was it worth your time doing the course?’ Participants responded with a ‘Yes’ or ‘No’ response.16,17,20
Treatment intervention
The Wellbeing Plus Course is an 8-week intervention that teaches core transdiagnostic psychological principles and skills such as cognitive challenging, exposure and behavioural activation that have been found to be effective at reducing symptoms of depression and anxiety in older adults.16,17,20 The Wellbeing Plus Course consists of five online lessons, homework assignments and case-enhanced stories, which detail the experiences of older adults recovering from symptoms of depression and anxiety (Table 2). Each lesson is presented in a slide show format that combines didactic material (i.e. text-based instructions and information) with case-enhanced stories. Participants are instructed to read the lessons over 8 weeks according to a timetable. Participants also receive regular automatic emails which notify them of new course materials, reinforce completion of materials and practice of skills. Participants are encouraged to complete one lesson every 7–10 days and to attempt to regularly practice the skills covered within the lesson summaries.
Table 2. Content of the Wellbeing Plus Course and recommended timetable.
| Lesson | Time before next lesson | Lesson content | Primary skill taught in lesson and homework | Additional resources |
|---|---|---|---|---|
| Lesson 1 | 1 week | Education about the general prevalence and symptoms of anxiety and low mood without mention of specific disorders. Introduction of a cognitive–behavioural therapy model and explanation of the functional relationship between physical, thought and behavioural symptoms in psychological distress. Instructions for identifying their own symptoms and how their symptoms interact. Transdiagnostic vignettes and examples of anxiety and low mood symptoms provided. | Symptom identification Symptom formulation |
Sleep management What to do in a mental health emergency Managing chronic health conditions Transdiagnostic case stories |
| Lesson 2 | 2 weeks | Introduction to the basic principles of cognitive therapy and importance of managing thoughts to manage anxiety and low mood. Instructions for monitoring and challenging thoughts related to anxiety and low mood. Transdiagnostic vignettes and examples of thoughts provided. | Thought monitoring Thought challenging |
Structured problem-solving Worry time Challenging beliefs Transdiagnostic case stories |
| Lesson 3 | 1 week | Introduction to the physical symptoms of hyper-arousal and hypo-arousal and their relationship to anxiety and low mood. Instructions about managing physical symptoms using de-arousal strategies such as controlled breathing and scheduling pleasant activities. Transdiagnostic vignettes and examples of physical symptoms provided. | Controlled breathing Activity scheduling |
Communication skills A list of 100 pleasant things to do Transdiagnostic case stories |
| Lesson 4 | 2 weeks | Introduction to the behavioural symptoms of anxiety and low mood. Explanation of avoidance and safety behaviours and their relationship with ongoing distress. Instructions for graded exposure for safely confronting fears and increasing activity levels. Transdiagnostic vignettes and examples of graded exposure provided. | Graded exposure | Assertive communication Transdiagnostic case stories |
| Lesson 5 | 2 weeks | Information about the occurrence of lapses and the process of recovery from anxiety and low mood. Information about the signs of relapse and managing lapses. Instructions for creating a relapse | Relapse prevention | Transdiagnostic case stories |
Clinician contact
Participants in the iCG and iSG groups received a brief telephone interview from one of the clinicians. This call was scripted and aimed to: (a) discuss the aims of treatment; (b) convey hope by describing the results of previous participants; (c) emphasise the importance of consistent practice of the skills over time; and (d) answer questions about the treatment. The interview calls were designed to take between 10 and 20 min.
Participants in the iCG group also received weekly contact from clinicians during treatment. Two registered and experienced psychologists (V.F. and L.J.) provided all clinical contact with participants, via telephone or a secure email system. In accordance with previous research,29 clinicians were instructed to: (a) answer participants’ questions; (b) summarise content; (c) encourage skills practice; (d) resolve difficulties applying skills; and (e) reinforce progress. Clinicians were instructed not to introduce therapeutic skills not covered within the course and, unless clinically indicated, to limit the time spent in contact or contacting participants to approximately 10–15 min per week.
Participants in the iSG and SG groups were informed via the online application system that they would not receive clinical contact throughout treatment unless their symptoms became more severe. The symptom questionnaire responses of participants in these groups were monitored weekly by the clinicians, but contact was only initiated if a deterioration in their mental health (i.e. defined as an increase in PHQ-9 total score of ≥5 with a total score ≥15 or a PHQ-9 question 9 score of 3) was observed. This contact involved the administration of a risk assessment and, if needed, referral to appropriate crisis services.
Statistical analysis
All analyses were conducted using SPSS version 21. Group differences in demographic variables and diagnostic variables were analysed using binomial and multinomial logistic regression and general linear models analyses. The alpha significance level for the preliminary analyses was adjusted from 0.05 to 0.01 as a partial control for the number of analyses conducted. Participants who did not start the interventions were not included in any analyses.
A generalised estimation equation (GEE) modelling technique was employed to examine changes in the measures over time. An unstructured working correlation structure was selected, coupled with a robust error estimation, for GEE analyses. GEE models specified a gamma distribution with a log-link response scale to address skewness in the dependent variable distributions. Symptom scores at the time of completing the online application were employed as baseline for the primary measures. However, for the secondary and tertiary outcomes, which were not assessed at initial application, pre-treatment was used as baseline. SPSS pairwise comparisons were used to examine significant main and interaction effects. To determine whether the age of older adults affected clinical outcomes, GEE analyses were repeated on the primary outcomes using participant age as a model covariate.
In addition, three different statistics were calculated for comparison and benchmarking purposes. First, the average percentage change across time was calculated from the GEE analyses for each of the outcome variables with 95% confidence intervals. Second, Cohen’s d effect sizes and 95% confidence intervals were calculated for the between-groups effects based on the estimated marginal means derived from the GEE models. To provide data about negative outcomes,30 the numbers of participants reporting symptom deteriorations ≥30% and symptoms in the clinical ranges at post-treatment (i.e. above recognised clinical cut-offs on the GAD-7 and PHQ-9) on the primary outcome measures were also calculated.
Results
Baseline data, adherence and attrition
The demographic characteristics of the sample are shown in Table 1. Participant flow, treatment attrition, lesson completion and questionnaire response are shown in Fig. 1. As shown in Table 1, participants reported having had symptoms for several decades and the majority had not sought professional help in the past 12 months. No differences were found between the groups on the demographic variables. A minimum of 95% of participants in each group completed questionnaires at post-treatment compared with a minimum of 90% at 3-month follow-up. No differences were found between participants who completed and did not complete post-treatment questionnaires (Ps>0.01). The means, percentage reductions and effect sizes for the groups are shown in Table 3.
Table 1. Demographic characteristics and treatment and symptom histories of the treatment groups.
| Variable | Clinician-guided with interview (n=153) | Self-guided with interview (n=140) | Self-guided without interview (n=140) | Overall (n=433) | Statistical comparison between groups | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Gender | |||||||||
| Male | 53 | 35 | 50 | 36 | 52 | 37 | 155 | 36 | Wald’s χ2=0.20, P=0.905 |
| Female | 100 | 65 | 90 | 64 | 88 | 63 | 278 | 64 | |
| Age, years | |||||||||
| Mean | 65 (3.8) | 66 (4.6) | 67 (5.6) | 66 (4.7) | F2,430=4.73, P=0.009 | ||||
| Range | 60–78 | 60–80 | 60–93 | 60–93 | |||||
| Age frequency | |||||||||
| 60–64 years | 78 | 51 | 69 | 49 | 63 | 45 | 210 | 49 | Wald’s χ2=1.10, P=0.578 |
| 65–74 years | 74 | 48 | 64 | 46 | 63 | 45 | 201 | 46 | Wald’s χ2=0.37, P=0.829 |
| 75 years and above | 1 | 1 | 7 | 5 | 14 | 10 | 22 | 5 | Wald’s χ2=8.66, P=0.013 |
| Marital status | |||||||||
| Single/never married | 8 | 5 | 8 | 6 | 3 | 2 | 19 | 4 | Wald’s χ2=2.35, P=0.309 |
| Married/de facto | 96 | 63 | 98 | 70 | 99 | 71 | 293 | 68 | Wald’s χ2=2.63, P=0.269 |
| Separated/divorced/widowed/other | 49 | 32 | 34 | 24 | 38 | 27 | 121 | 28 | Wald’s χ2=2.23, P=0.328 |
| Education | |||||||||
| High school or less | 32 | 21 | 27 | 19 | 26 | 19 | 85 | 20 | Wald’s χ2=0.27, P=0.874 |
| Certificate/diploma/other | 43 | 28 | 37 | 27 | 47 | 33 | 127 | 29 | Wald’s χ2=1.89, P=0.389 |
| University | 78 | 51 | 76 | 54 | 67 | 48 | 221 | 51 | Wald’s χ2=1.16, P=0.561 |
| Vocational statusa | |||||||||
| Full-time/part-time employment | 84 | 55 | 76 | 54 | 65 | 46 | 225 | 52 | Wald’s χ23.57, P=0.168 |
| Full-time/part-time student | 1 | 1 | 4 | 3 | 2 | 1 | 7 | 2 | Wald’s χ2=2.00, P=0.367 |
| Unemployed/seeking employment | 9 | 6 | 8 | 6 | 9 | 6 | 26 | 6 | Wald’s χ2=0.07, P=0.966 |
| Registered disability | 4 | 3 | 5 | 4 | 4 | 3 | 13 | 3 | Wald’s χ2=0.24, P=0.885 |
| Retired | 83 | 54 | 86 | 61 | 87 | 62 | 256 | 59 | Wald’s χ2=2.34, P=0.311 |
| Age at symptom onset, years: mean (s.d.) | 33 (19) | 33 (18) | 35 (20) | 33 (19) | F2,423=0.50, P=0.609 | ||||
| Treatment in previous 12 months | |||||||||
| Yes | 53 | 35 | 45 | 32 | 51 | 36 | 149 | 34 | Wald’s χ2=0.57, P=0.750 |
| No | 100 | 65 | 95 | 68 | 89 | 63 | 284 | 66 | |
| Health professionals seen for treatment | |||||||||
| General practitioner | 87 | 57 | 81 | 58 | 82 | 59 | 250 | 58 | Wald’s χ2=0.09, P=0.957 |
| Psychiatrist | 9 | 6 | 7 | 5 | 7 | 5 | 108 | 25 | Wald’s χ2=0.21, P=0.901 |
| Psychologist/counsellor | 39 | 26 | 36 | 26 | 33 | 24 | 23 | 5 | Wald’s χ2=0.15, P=0.926 |
| Other | 14 | 9 | 10 | 7 | 10 | 7 | 34 | 8 | Wald’s χ2=0.54, P=0.760 |
| Taking prescription medication | |||||||||
| No | 101 | 66 | 89 | 65 | 98 | 70 | 288 | 67 | Wald’s χ2=1.32, P=0.516 |
| Anxiety | 12 | 8 | 16 | 11 | 12 | 9 | 40 | 9 | Wald’s χ2=1.21, P=0.544 |
| Depression | 19 | 12 | 19 | 14 | 15 | 11 | 53 | 12 | Wald’s χ2=0.53, P=0.764 |
| Both anxiety and depression | 21 | 14 | 16 | 11 | 15 | 11 | 52 | 12 | Wald’s χ2=0.69, P=0.708 |
| Distribution of symptoms at assessment | |||||||||
| Anxiety symptoms (GAD-7) | |||||||||
| Minimal anxiety | 18 | 12 | 8 | 6 | 10 | 7 | 36 | 8 | Wald’s χ2=3.77, P=0.152 |
| Mild anxiety | 57 | 37 | 51 | 36 | 53 | 38 | 161 | 37 | Wald’s χ2=0.62, P=0.970 |
| Moderate anxiety | 50 | 33 | 54 | 39 | 51 | 36 | 155 | 36 | Wald’s χ2=1.14, P=0.565 |
| Severe anxiety | 28 | 18 | 27 | 19 | 26 | 19 | 81 | 19 | Wald’s χ2=0.49, P=0.976 |
| Depression symptoms (PHQ-9) | |||||||||
| No depression | 13 | 9 | 15 | 11 | 11 | 8 | 39 | 9 | Wald’s χ2=0.76, P=0.683 |
| Mild depression | 56 | 37 | 50 | 36 | 53 | 38 | 159 | 37 | Wald’s χ2=0.14, P=0.933 |
| Moderate depression | 47 | 31 | 48 | 34 | 51 | 36 | 146 | 34 | Wald’s χ2=1.09, P=0.578 |
| Moderately severe depression | 29 | 19 | 24 | 17 | 17 | 12 | 70 | 16 | Wald’s χ2=2.68, P=0.261 |
| Severe depression | 8 | 5 | 3 | 2 | 8 | 6 | 19 | 4 | Wald’s χ2=2.55, P=0.279 |
GAD-7, 7-item Generalised Anxiety Disorder Scale; PHQ-9, 9-item Patient Health Questionnaire.
Categories of vocational status were not mutually exclusive; participants could indicate more than one to best describe their situation.
All data were self-reported. Numbers and percentages are rounded to nearest whole number.
Table 3. Means, s.d.s, percentage change and effect sizes (Cohen’s d) for the primary and secondary outcome measures.
| Estimated marginal means (s.d.) | Percentage change from assessment (95% CI)a | Within group effect size from assessment (95% CI) | Between group effect size at post-treatment (95% CI) | Between group effect size at 3-month follow-up (95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Assessment | Post-treatment | 3-month follow-up | Post-treatment | 3-month follow-up | Post-treatment | 3-month follow-up | Clinician-guided | Self-guided with assessment | Purely self-guided | Clinician guided | Self-guided with assessment | Pure Self-guided | |
| Primary outcomes | ||||||||||||||
| Depression (PHQ-9) | ||||||||||||||
| iCG | 153 | 10.74 (4.88) |
4.39 (3.81) |
4.30 (3.37) |
59 (53 to 64) |
60 (55 to 65) |
1.45 (1.20–1.70) |
1.54 (1.28–1.79) |
– | −0.01 (−0.24 to 0.22) |
−0.10 (−0.33 to 0.13) |
– | −0.11 (−0.34 to 0.12) |
−0.13 (−0.35 to 0.10) |
| iSG | 140 | 10.43 (4.61) |
4.44 (3.67) |
4.71 (3.79) |
57 (51 to 63) |
55 (48 to 60) |
1.44 (1.17–1.70) |
1.36 (1.09–1.61) |
– | – | −0.09 (−0.32 to 0.14) |
– | – | −0.01 (−0.24 to 0.22) |
| SG | 140 | 10.43 (4.73) |
4.78 (3.90) |
4.75 (3.79) |
54 (48 to 60) |
54 (48 to 60) |
1.30 (1.04–1.56) |
1.33 (1.06–1.58) |
– | – | – | – | – | – |
| Anxiety (GAD-7) | ||||||||||||||
| iCG | 153 | 9.86 (4.58) |
4.17 (3.96) |
3.73 (3.09) |
58 (51 to 64) |
62 (57 to 67) |
1.33 (1.08–1.57) |
1.57 (1.31–1.82) |
– | −0.14 (−0.37 to 0.09) |
−0.26 (−0.49 to −0.02) |
– | −0.41 (−0.41 to 0.05) |
−0.22 (−0.45 to −0.01) |
| iSG | 140 | 10.45 (4.38) |
4.74 (4.02) |
4.36 (3.90) |
55 (48 to 61) |
58 (52 to 64) |
1.36 (1.09–1.61) |
1.47 (1.20–1.73) |
– | – | −0.11 (−0.35 to 0.12) |
– | – | −0.04 (−0.27 to 0.20) |
| SG | 140 | 10.44 (4.14) |
5.19 (4.02) |
4.50 (3.79) |
50 (43 to 56) |
57 (51 to 62) |
1.29 (1.03–1.54) |
1.50 (1.23–1.76) |
– | – | – | – | – | – |
| Secondary outcomes | ||||||||||||||
| Geriatric depression (GDS) | ||||||||||||||
| iCG | 153 | 8.07 (3.46) |
4.83 (3.71) |
4.41 (3.59) |
40 (32 to 47) |
45 (38 to 52) |
0.90 (0.67–1.14) |
1.04 (0.80–1.28) |
– | 0.03 (−0.20 to 0.26) |
−0.15 (−0.38 to 0.08) |
– | 0.02 (−0.21 to 0.25) |
−0.02 (−0.25 to 0.20) |
| iSG | 140 | 7.82 (3.79) |
4.73 (3.43) |
4.35 (3.55) |
40 (32 to 46) |
44 (36 to 51) |
0.85 (0.61–1.10) |
0.94 (0.70–1.19) |
– | – | −0.18 (−0.42 to 0.05) |
– | – | −0.04 (−0.28 to 0.19) |
| SG | 140 | 7.72 (3.59) |
5.36 (3.43) |
4.50 (3.67) |
31 (23 to 38) |
42 (33 to 49) |
0.67 (0.43–0.91) |
0.89 (0.64–1.13) |
– | – | – | – | – | – |
| Psychological distress (K-10) | ||||||||||||||
| iCG | 153 | 24.92 (6.68) |
17.01 (6.31) |
16.05 (5.57) |
32 (28 to 36) |
36 (32 to 39) |
1.22 (0.97–1.46) |
1.44 (1.19–1.69) |
– | −0.11 (−0.34 to 0.12) |
−0.23 (−0.46 to 0.00) |
– | −0.12 (−0.35 to 0.11) |
−0.19 (−0.42 to 0.04) |
| iSG | 140 | 24.97 (6.51) |
17.69 (5.92) |
16.76 (5.92) |
29 (25 to 33) |
33 (29 to 37) |
1.17 (0.91–1.42) |
1.32 (1.06–1.57) |
– | – | −0.13 (−0.37 to 0.10) |
– | – | −0.07 (−0.31 to 0.16) |
| SG | 140 | 25.09 (6.15) |
18.50 (6.39) |
17.21 (6.39) |
26 (22 to 30) |
31 (27 to 36) |
1.05 (0.80–1.30) |
1.26 (1.00–1.51) |
– | – | – | – | – | – |
| Tertiary outcomes | ||||||||||||||
| Disability (SDS) | ||||||||||||||
| iCG | 153 | 11.51 (7.79) |
6.17 (6.06) |
5.53 (6.56) |
46 (37 to 54) |
52 (42 to 60) |
0.77 (0.53–1.00) |
0.83 (0.59–1.06) |
– | −0.02 (−0.25 to 0.21) |
−0.06 (−0.29 to 0.17) |
– | −0.03 (−0.26 to 0.19) |
−0.00 (−0.23 to 0.23) |
| iSG | 140 | 11.47 (7.22) |
6.31 (6.63) |
5.76 (6.74) |
45 (35 to 54) |
50 (39 to 59) |
0.74 (0.50–0.98) |
0.82 (0.57–1.06) |
– | – | −0.04 (−0.27 to 0.20) |
– | – | −0.03 (−0.20 to 0.27) |
| SG | 140 | 10.94 (6.98) |
6.54 (6.15) |
5.54 (6.27) |
40 (30 to 49) |
49 (39 to 58) |
0.67 (0.43–0.91) |
0.81 (0.57–1.06) |
– | – | – | – | – | – |
| Life satisfaction (SWLS) | ||||||||||||||
| iCG | 153 | 16.38 (6.93) |
19.63 (7.92) |
20.89 (7.79) |
−20 (−28 to −12) |
−28 (−35 to −20) |
0.44 (0.21–0.66) |
0.61 (0.38–0.84) |
– | −0.11 (−0.34 to 0.12) |
−0.03 (−0.26 to 0.20) |
– | −0.00 (−0.23 to 0.23) |
−0.05 (−0.28 to 0.17) |
| iSG | 140 | 16.52 (6.98) |
20.46 (7.22) |
20.92 (7.69) |
−24 (−31 to −17) |
−27 (−35 to −19) |
0.55 (0.31–0.79) |
0.60 (0.36–0.84) |
– | – | 0.08 (−0.16 to 0.31) |
– | – | −0.05 (−0.29 to 0.18) |
| SG | 140 | 17.94 (7.22) |
19.88 (7.57) |
21.32 (7.93) |
−11 (−18 to −4) |
−19 (−26 to −12) |
0.26 (0.03–0.50) |
0.45 (0.21–0.68) |
– | – | – | – | – | – |
iCG, interview plus clinician-guided internet-delivered cognitive–behavioural therapy (iCBT); iSG, interview plus self-guided iCBT; SG, self-guided iCBT; GAD-7, Generalised Anxiety Disorder 7-item scale; PHQ-9, 9-item Patient Health Questionnaire; GDS-15, 15-item Geriatric Depression Scale; K-10, 10-item Kessler Psychological Distress Scale; SDS, Sheehan Disability Scale; SWLS, Satisfaction with Life Scale.
The percentage change from baseline statistics are estimates of relative change derived from the GEE models conducted separately for each outcome.
Primary outcomes
The primary outcomes were depression and anxiety symptom levels, which were assessed with the PHQ-9 and GAD-7 respectively. The GEE analyses indicated a significant effect for time (PHQ-9: Wald’s χ2=738.80, P<0.001; GAD-7: Wald’s χ2=682.88, P<0.001) but no significant time × group interactions (PHQ-9: Wald’s χ2=4.34, P=0.362; GAD-7: Wald’s χ2=4.43, P=0.351). Pairwise comparisons indicated that on the PHQ-9, all groups reduced their symptoms from assessment to post-treatment (P<0.001) but not from post-treatment to 3-month follow-up (P=0.761). On the GAD-7, all groups reduced in their symptoms from assessment to post-treatment (P<0.001) and from post-treatment to 3-month follow-up (P=0.002).
Secondary outcomes
The secondary outcomes were geriatric-specific depression symptoms and general psychological distress, as measured by the GDS and K-10 respectively. The GEE analyses indicated a significant effect for time (GDS: Wald’s χ2=371.43, P<0.001; K-10: Wald’s χ2=793.60, P<0.001) but no significant time × group interactions (GDS: Wald’s χ2=6.52, P=0.164; K-10: Wald’s χ2=5.58, P=0.233). Pairwise comparisons indicated that on both measures, all groups showed significant symptom reduction from assessment to post-treatment (P<0.001) and from post-treatment to 3-month follow-up (P<0.001).
Tertiary outcomes
The tertiary outcomes were disability and satisfaction with life, assessed with the SDS and SWLS respectively. Analyses indicated a significant effect for time (SDS: Wald’s χ2=282.31, P<0.001; SWLS: Wald’s χ2=241.25, P<0.001). All groups showed symptom reduction from assessment to post-treatment (P<0.001) and from post-treatment to 3-month follow-up in both disability and satisfaction (P<0.009).
There was no significant time × group interaction for disability (SDS: Wald’s χ2=1.71, P=0.790) but there was evidence of an interaction for satisfaction with life (SWLS: Wald’s χ2=12.34, P=0.015). Pairwise comparisons indicated that the iSG group did not improve in satisfaction with life from post-treatment to 3-month follow-up (P=0.363), whereas the iCG and SG groups did improve (Ps<0.003). However, there were no overall differences in satisfaction with life between the three groups at either post-treatment (P range: 0.334–0.780) or at 3-month follow-up (P range: 0.642–0.981).
Age and clinical outcomes
The GEE analyses revealed no significant effect for age (GAD-7: Wald’s χ2=0.57, P=0.449; PHQ-9: Wald’s χ2=0.28, P=0.591) or significant interactions on the primary outcomes (GAD-7: Wald’s χ2=3.24, P=0.518; PHQ-9: Wald’s χ2=0.33, P=0.988) when age was entered into the analyses as a covariate.
Clinician time
There were significant differences in clinician contact time between groups (F=415.50, P<0.001). The iCG group received more clinician time than the iSG and SG groups (Ps<0.001), but there were no differences between the iSG and SG groups (P=0.483). The mean total clinician time per participant in the iCG group was 68.47 min (s.d.=34.35), which was comprised of answering and making calls (total=1320; M=8.63 min; s.d.=2.80; range 0–20) as well as reading, sending and responding to secure emails (total=750; M=4.90; s.d.=2.78; range 0–12). Because of technical difficulties and deterioration, 52% (73/140) of the iSG group and 56% (79/140) of the SG group received one or more contacts via email or telephone during treatment. The mean total clinician time per participant in the iSG group was 4.61 min (s.d.=8.08) and the mean total clinician time per participant in the SG group was 6.43 min (s.d.=10.24).
Negative outcomes
Less than 1% (1/150), 3% (3/136) and 2% (2/133) in the iCG, iSG and SG groups respectively had increases in depression scores ≥30% and also scored above clinical cut-off at post-treatment. None of the iCG group, 3% (4/136) of the iSG and 2% (2/133) of the SG groups respectively had increases in anxiety scores ≥30% and scored above the clinical cut-off at post-treatment. No participants reported symptom deteriorations or changes in personal safety requiring referral to crisis services.
Treatment completion and satisfaction rates
There was no difference between groups in the number of lessons completed at post-treatment (F=1.12, P=0.326) or follow-up (F=2.18, P=0.114). Of the participants who completed the evaluation questions at post-treatment, 95% (132/139), 94% (117/124) and 91% (112/123) of participants in the iCG, iSG and SG groups respectively, responded that they ‘would recommend the course’ to others. Similarly, 94% (131/139), 92% (115/124) and 95% (117/123) of participants in the iCG, iSG, and SG groups respectively responded that the course was ‘worth their time’. There were no differences between groups in the proportions reporting they would recommend the course (F=0.92, P=0.398) or that it was worth their time (F=0.41, P=0.668).
Discussion
The present study compared the efficacy and acceptability of three support levels for a new transdiagnostic internet-delivered intervention, the Wellbeing Plus Course, for adults aged 60 years and above with symptoms of depression and anxiety. No differences were found between the groups. High completion and acceptability rates were achieved in all three groups. All groups were associated with significant reductions in symptoms and very low rates (i.e. <4%) of symptom deterioration.
Similarly, large reductions in symptoms of depression (Cohen’s d ≥1.30; average reduction ≥54%) and anxiety (Cohen’s d ≥1.29; average reductions ≥50%) were observed across the three treatment groups and were maintained or improved at follow-up. The magnitude of the observed reductions are comparable with other studies that have evaluated the efficacy of psychological treatments for older adults when administered face to face31,32 and via the internet.16–20 Significant improvements were also observed on secondary and tertiary outcome measures, which included satisfaction with life, improvements in psychological distress and disability.
The present findings extend the literature in several ways. First, the results from this large RCT augment existing studies indicating that transdiagnostic treatments for symptoms of anxiety or depression are not only effective for younger adults31,32 but also older adults.14,17 Second, the results of this study indicate that clinician guidance or a pre-treatment telephone interview with a clinician may not be necessary to achieve strong clinical outcomes among older adults. This finding contributes to a growing body of evidence indicating that carefully designed self-guided treatments, which include automated prompts and other features that improve engagement are able to produce high rates of engagement and large clinical benefits.11–15 It is important to note that the results of the present trial have been partially replicated in an online national mental health service in Australia which used the clinician-guided iCBT model described here.33 High rates of course completion, satisfaction and strong clinical outcomes were observed in that sample of patients in routine clinical care, indicating the intervention can be successfully translated from a research setting into a routine clinical environment. This is consistent with recent results from other clinics indicating that both younger and older adults can benefit from iCBT when administered as part of routine clinical care.34–36 It is also notable that participants in the present study reported having had symptoms for several decades (M onset=33 years; s.d.=19) and many (≥66%) had not sought professional help in the past 12 months, which highlight the public health potential of internet-delivered psychological treatments to the large number of older adults with untreated anxiety and depression.
This study has a number of limitations. First, the absence of a control group means it is not possible to control for the effects of spontaneous remission. However, controlled trials using similar methods have found very little change in control groups (e.g. Cohen’s ds<0.15) without active intervention,16,20 which may reflect the chronicity of symptoms. Second, the present trial was designed as a superiority trial and consequently caution is needed in concluding any statistical findings as supporting clinical equivalence, which requires the use of specific equivalence trial analyses. Third, the results are based on self-reported symptom scores. The absence of a formal diagnostic interview means that some care is needed in generalising the results of the current study to older adults meeting diagnostic criteria for anxiety and depressive disorders. Fourth, it is unclear whether the current results would be maintained beyond the 3-month follow-up period, although the improvements in similar studies were still evident at 12-month follow-up.16,20 A further limitation of the current study is that it used a sample of older adults who were both seeking psychological treatment and were comfortable enough with the use of computers to participate in the study. Some caution is therefore needed in generalising the results to older adults presenting to other settings and who may not be interested in psychological treatment or are not sufficiently confident with computers.
Two further considerations are the nature of the intervention and the nature of support that was available to patients if needed. The Wellbeing Plus Course has been carefully developed over several phases of research, with each version evaluated in clinical trials and modified with the help of feedback from large numbers of participants. Moreover, the self-reported symptoms of all participants were carefully monitored during treatment and half of those in the self-guided groups were contacted, even if only briefly, by a clinician to check their safety or assist with technical difficulties during treatment. Hence, this model of self-guided treatment differs from fully automated interventions in facilitating the safety and engagement of participants, whereas still representing a cost-effective method of administration.
In conclusion, these results extend evidence indicating that CBT can help older adults recover from symptoms of anxiety and depression. The results also indicate that carefully developed clinician-guided and self-guided iCBT interventions, delivered either with and without a clinical interview, can result in similarly high treatment completion rates, levels of satisfaction and large clinical outcomes. The findings of the current trial further highlight the considerable potential of iCBT and interventions like the Wellbeing Plus Course to improve access to treatment for older adults with anxiety and depression who might otherwise never receive treatment.
Acknowledgements
The authors gratefully acknowledge the participants for their involvement and helpful comments. This research was enabled by a National Priority Driven Research Program Grant from beyondblue. The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript; or decision to submit the manuscript for publication. B.F.D. is supported by a National Health and Medical Research Council (NHMRC) Australian Public Health Fellowship. M.G. is supported by a Macquarie University Research Fellowship.
References
- 1.Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry 2010; 67: 489–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety 2010; 27: 351–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pirkis J, Pfaff J, Williamson M, Tyson O, Stocks N, Goldney R, et al. The community prevalence of depression in older Australians. J Affect Disord 2009; 115: 54–61. [DOI] [PubMed] [Google Scholar]
- 4.Unützer J, Bruce ML. The elderly. Ment Health Serv Res 2002; 4: 245–7. [DOI] [PubMed] [Google Scholar]
- 5.Hendriks GJ, Oude Voshaar RC, Keijsers GPJ, Hoogduin CAL, Van Balkom AJLM. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand 2008; 117: 403–11. [DOI] [PubMed] [Google Scholar]
- 6.Peng X-D, Huang C-Q, Chen L-J, Lu Z-C. Cognitive behavioural therapy and reminiscence techniques for the treatment of depression in the elderly: a systematic review. J Int Med Res 2009; 37: 975–82. [DOI] [PubMed] [Google Scholar]
- 7.Mackenzie CS, Reynolds K, Cairney J, Streiner DL, Sareen J. Disorder-specific mental health service use for mood and anxiety disorders: associations with age, sex, and psychiatric comorbidity. Depress Anxiety 2012; 29: 234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trollor JN, Anderson TM, Sachdev PS, Brodaty H, Andrews G. Prevalence of mental disorders in the elderly: the Australian National Mental Health and Well-Being Survey. Am J Geriatr Psychiatry 2007; 15: 455–66. [DOI] [PubMed] [Google Scholar]
- 9.Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2012; 12: 745–64. [DOI] [PubMed] [Google Scholar]
- 10.Andersson G, Titov N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014; 13: 4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berger T, Caspar F, Richardson R, Kneubuhler B, Sutter D, Andersson G. Internet-based treatment of social phobia: a randomised controlled trial comparing unguided with two types of guided self-help. Behav Res Ther 2011; 49: 158–69. [DOI] [PubMed] [Google Scholar]
- 12.Berger T, Hämmerli K, Gubser N, Caspar F. Internet-based treatment of depression: a randomised controlled trial comparing guided with unguided self-help. Behav Res Ther 2011; 40: 251–66. [DOI] [PubMed] [Google Scholar]
- 13.Titov N, Dear BF, Johnston L, Lorian C, Zou J, Wootton B, et al. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: randomised controlled trial. PloS One 2013; 8: e62873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dear B, Gandy M, Karin E, Staples LG, Johnston L, Fogliati VJ, et al. The Pain Course: a randomised controlled trial examining an internet delivered pain management program when provided with different levels of clinician support. Pain 2015; 156: 1920–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer B, Bierbrodt J, Schröder J, Berger T, Beevers CG, Weiss M, et al. Effects of an Internet intervention (Deprexis) on severe depression symptoms: randomized controlled trial. Internet Interv 2015; 2: 48–59. [Google Scholar]
- 16.Dear BF, Zou JB, Ali S, Lorian CN, Johnston L, Sheehan J, et al. Clinical and cost-effectiveness of therapist-guided internet-delivered cognitive behavior therapy for older adults with symptoms of anxiety: a randomized controlled trial. Behav Ther 2015; 46: 206–17. [DOI] [PubMed] [Google Scholar]
- 17.Dear BF, Zou JB, Ali S, Lorian CN, Johnston L, Terides MD, et al. Examining self-guided internet-delivered cognitive behavior therapy for older adults with symptoms of anxiety and depression: two feasibility open trials. Internet Interv 2015; 2: 17–23. [Google Scholar]
- 18.Dear BF, Zou J, Titov N, Lorian C, Johnston L, Spence J, et al. Internet-delivered cognitive behavioural therapy for depression: a feasibility open trial for older adults. Aust NZ J Psychiatry 2013; 47: 169–76. [DOI] [PubMed] [Google Scholar]
- 19.Zou JB, Dear BF, Titov N, Lorian CN, Johnston L, Spence J, et al. Brief internet-delivered cognitive behavioral therapy for anxiety in older adults: a feasibility trial. J Anxiety Disord 2012; 26: 650–5. [DOI] [PubMed] [Google Scholar]
- 20.Titov N, Dear BF, Ali S, Zou JB, Lorian CN, Johnston L, et al. Clinical and cost-effectiveness of therapist-guided internet-delivered cognitive behavior therapy for older adults with symptoms of depression: a randomized controlled trial. Behav Ther 2015; 46: 193–205. [DOI] [PubMed] [Google Scholar]
- 21.Spek V, Cuijpers P, Nyklícek I, Smits N, Riper H, Keyzer J, et al. One-year follow-up results of a randomized controlled clinical trial on internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years. Psychol Med 2008; 38: 635–9. [DOI] [PubMed] [Google Scholar]
- 22.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med 2007; 37: 319–28. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–7. [DOI] [PubMed] [Google Scholar]
- 25.Sheikh J, Yesavage J. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986; 5: 165–73. [Google Scholar]
- 26.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-L, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32: 959–76. [DOI] [PubMed] [Google Scholar]
- 27.Sheehan DV. The Anxiety Disease. Scribner, 1983. [Google Scholar]
- 28.Diener E, Emmons R, Larsen R, Griffin S. The satisfaction with life scale. J Pers Assess 1985; 49: 71–5. [DOI] [PubMed] [Google Scholar]
- 29.Johnston L, Titov N, Andrews G, Spence J, Dear BF. A RCT of a transdiagnostic internet-delivered treatment for three anxiety disorders: examination of support roles and disorder-specific outcomes. PloS One 2011; 6: e28079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rozental A, Andersson G, Boettcher J, Ebert D, Cuijpers P, Knaevelsrud C, et al. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv 2014; 1: 12–9. [Google Scholar]
- 31.Gould RL, Coulson MC, Howard RJ. Efficacy of cognitive behavioral therapy for anxiety disorders in older people: a meta-analysis and meta-regression of randomized controlled trials. J Am Geriatr Soc 2012; 60: 218–29. [DOI] [PubMed] [Google Scholar]
- 32.Wetherell JL, Petkus AJ, Thorp SR, Stein MB, Chavira DA, Campbell-Sills L, et al. Age differences in treatment response to a collaborative care intervention for anxiety disorders. Br J Psychiatry 2013; 203: 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Titov N, Dear B, Staples LG, Bennett-Levy J, Klein B, Rapee R, et al. MindSpot Clinic: an accessible, efficient and effective online treatment service for anxiety and depression. Psychiatr Serv 2015; 66: 1043–50. [DOI] [PubMed] [Google Scholar]
- 34.Andersson G, Hedman E. Effectiveness of guided internet-based cognitive behavior therapy in regular clinical settings. Verhaltenstherapie 2013; 23: 140–8. [Google Scholar]
- 35.Mewton L, Sachdev P, Andrews G. A naturalistic study of the acceptability and effectiveness of internet-delivered cognitive behavioural therapy for psychiatric disorders in older Australians. PloS One 2013; 8: e71825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ruwaard J, Lange A, Schrieken B, Dolan CV, Emmelkamp P. The effectiveness of online cognitive behavioral treatment in routine clinical practice. PloS One 2012; 7: e40089. [DOI] [PMC free article] [PubMed] [Google Scholar]