Abstract
Background
The relation between central obesity and survival in community-dwelling adults with a normal body mass index (BMI) is not well known.
Objectives
To examine the risk of total and cardiovascular mortality associated with central obesity but normal BMI
Design
Stratified multistage probability design
Setting
Third National Health and Nutrition Examination Survey
Participants
We analyzed data on 15,184 people (52.3% women) aged 18 to 90 years..
Measurements
We used multivariable Cox proportional hazards model to evaluate the relation of obesity patterns defined by BMI and WHR and total and cardiovascular mortality risk after adjustment for confounding factors.
Results
Persons with normal-weight central obesity had the worst long-term survival: a man with a normal BMI (22 kg/m2) and central obesity had greater total mortality risk than one with similar BMI but no central obesity (hazard ratio [HR], 1.87 [95% CI, 1.53–2.29]) and twice the mortality risk of participants who were overweight or obese by BMI only (HR, 2.24 [95% CI,1.52–3.32] and HR, 2.42 [95% CI, 1.30–4.53], respectively). Similarly, women with normal weight and central obesity had higher mortality risk than both women with similar BMI but no central obesity (HR, 1.48 [95% CI, 1.35–1.62]) and women who were obese by BMI only (HR, 1.32 [95% CI, 1.15–1.51]). Expected survival estimates were consistently lower for those with central obesity when controlled for age and BMI.
Limitations
Body fat distribution was assessed based on anthropometric indicators alone. Information on comorbidities was collected by self-report.
Conclusion
Normal-weight central obesity defined by WHR is associated with higher mortality than BMI–defined obesity, particularly in the absence of central fat distribution.
Keywords: normal-weight obesity, fat distribution, mortality, cardiovascular mortality, body mass index
Introduction
Obesity defined by body mass index (BMI) or measures of central obesity, such as waist-to-hip ratio (WHR) and waist circumference, is associated with increased total and cardiovascular mortality.(1–3) However, a recent meta-analysis showed that being overweight by BMI was actually associated with lower total mortality,(4) challenging the paradigm linking BMI to increased mortality. Furthermore, it has been a source of major controversy as to whether measures of fat distribution provide any incremental risk information beyond BMI alone.(2, 3, 5–8) Indeed, the 2013 American Heart Association/American College of Cardiology/The Obesity Society Guidelines for the management of obesity do not recommend measuring WHR, and assume that people with normal BMI are not exposed to any obesity-related cardiovascular risk, in view of the limited available data proving otherwise.(9)
A recent large study demonstrated that incorporating waist circumference information in prediction models did not increase the prognostic value already provided by BMI.(6) However, the study also showed that for a given BMI category, subgroups of waist circumference or WHR were associated with increased mortality risk. Other studies demonstrated that measures of central obesity such as waist-to-hip ratio, waist-to-height ratio (10, 11) or waist circumference alone may provide additional information beyond BMI on mortality risk among middle-aged adults, provided there is no adjustment for obesity-related cardiovascular risk factors.(2, 3, 7) Moreover, a study has also shown that measures of central obesity are more strongly associated with total and cardiovascular disease death than BMI.(12) It has also been demonstrated that persons with normal body weight measured with BMI but with increased body fat measured with bioimpedance have higher total and cardiovascular mortality rates, and a higher prevalence of metabolic syndrome and its components than people with normal BMI and normal body fat content.(13) In addition, a recent meta-analysis of individual patient data in patients with coronary artery disease has shown that persons with normal BMI but in the top tertile of central obesity measures had the highest total mortality rate.(12)
These results have been attributed to several factors. First, the diagnostic accuracy of BMI for obesity is not optimal, especially in persons with greater body fat percentages but normal and intermediate BMI values.(14) Second, persons with normal body weight but increased amounts of body fat have less muscle mass, a factor associated with higher mortality risk and metabolic dysregulation.(15, 16) Third, animal and human studies have recently shown that adipose tissue in the legs and buttocks may have a favorable effect on glucose metabolism, and persons with central distribution of fat, particularly when measured with WHR, have less adipose tissue in the lower extremities.(17)
To our knowledge, no studies in the general US population have specifically focused to assess the mortality risk in persons with normal BMI but central obesity in comparison with people who are overweight or obese by BMI. Thus, we hypothesized that persons with normal BMI but central obesity would have increased mortality risk compared with persons who have any other combination of BMI and central obesity. In the present study, we investigated the total and cardiovascular mortality risks associated with different patterns of body adiposity in a large cohort of participants in the Third National Health and Nutrition Examination Survey (NHANES III). Because hip circumference was not measured in the most contemporary NHANES (1999–2010) and WHR data to define central obesity were crucial to our primary hypothesis, we resolved to test the hypothesis in NHANES III instead.
Methods
Study Design and Subjects
The NHANES III is a cross-sectional survey that produces generalizable health estimates for the US population using stratified multistage probability sampling design. The survey was conducted from 1988 to 1994. From a sample of 39,695 persons, 33,994 were interviewed and 30,818 examined at mobile examination centers. The examination consisted of extensive anthropometric, physiological, and laboratory testing. Waist and hip circumference were measured by a trained examiner with a measuring tape positioned at the high point of the iliac crest for the waist and at the greatest circumference of the buttocks. The design and methods for the survey are available at http://www.cdc.gov/nchs/nhanes.htm.
In the present study, 16,124 adults aged 18 years had WHRs available. Since extremely thin persons and people with history of non-skin cancers are already known to have higher mortality risks, we further restricted our analysis to persons with a BMI > 18.5 kg/m2 and those without history of non-skin cancer, resulting in a sample of 15,184 participants (7,249 men and 7,935 women).
Total and Cardiovascular Mortality Assessment
Identifier data were matched to the National Death Index to determine mortality status with mortality follow-up from the date of NHANES survey through December 31, 2006. A complete description of the methodology to link baseline NHANES III data to the National Death Index can be found elsewhere.(18) International Classification of Diseases, Ninth Revision (ICD-9), codes from 1986 to 1998 and International Classification of Diseases, Tenth Revision (ICD-10), codes from 1999 to 2000 were used to ascertain the underlying cause of death. Cardiovascular deaths were defined as those with ICD-9 codes 390 to 398, 402, and 404 to 429 and ICD-10 codes I00 to I09, I11, I13, and I20 to I51 (NHANES III codes 53–75).
Statistical Analysis
The overarching analytical goal was to estimate the influence of various magnitudes of central obesity and body mass index on all-cause mortality. In order to do this, we conducted weighted survival modeling that enabled the estimation of the relative risk for mortality, as quantified by the hazard ratio, and the expected survival for NHANES III participants. The NHANES III survey design and sampling weights were incorporated into the statistical analysis in order to calculate weighted means, standard errors for continuous variables, and weighted percentages for categorical variables. To determine the risk of all-cause mortality associated with the different patterns of adiposity, we created multivariable Cox proportional hazards models while adjusting for potential confounders that have been shown to be associated with obesity and mortality.(4) These variables were age at time of examination, sex, education level and prior smoking history. Although we considered the adjustment for obesity-related cardiovascular risk factors in the models, our final estimates were not adjusted for these factors. Epidemiologic obesity research has shown that it might be inappropriate for controlling for factors in the causal pathway between obesity and death, such as diabetes, atherogenic dyslipidemia and hypertension.
In testing for differences in mortality risk for combinations of central obesity, as quantified by waist to hip ratio (WHR), and BMI, higher-order interactions of WHR with BMI and other covariates were considered. The association pattern of WHR and BMI was found to be different for male participants vs female participants (i.e., statistically significant higher-order interaction terms), so the final modeling was conducted using sex-stratified data to more clearly present the findings. The interaction terms allowed the potential quadratic risks (U-shaped risks) of values for these variables. The estimated model contains polynomial functions of BMI and WHR (eg, BMI2, BMI2 WHR2). These terms allow for relationships that are more sensitive to change in risk for mortality based on unique combinations (profiles) of WHR and BMI. The estimated risk function, when controlling for other covariates in the model, will resemble a saddle with high-risk areas and low-risk areas. When possible, covariates were grand mean centered to lessen the collinearity induced from quadratic effects. Likelihood ratio tests were used to determine whether these higher-order model terms could be removed. The proportional hazards assumption for all variables was assessed and was satisfied for the final models.
After the final models were established, hazard ratios were estimated with estimated model parameters for different combinations of WHR and BMI, by sex. For these comparisons, we chose a BMI of 22 to represent normal BMI, 27.5 to represent overweight BMI, and 33 to represent obese BMI. For WHR, we chose 0.89 and 1.00 for men and 0.80 and 0.92 for women as a measure of central obesity. Each of these sets of values were chosen to reflect either the approximate midpoint of standard clinical interpretations, to avoid issues with values directly at common threshold values (e.g., BMI values at 30) or to be clinical targets we sought to better understand. Wald-based (or large–sample-based) hazard ratio estimates and their standard errors were assessed to provide significance tests among these representative patient profiles. (19)
Once the fitted Cox model was deemed satisfactory, we sought to estimate measures of absolute risk by means adjusted 5- and 10-year survival estimates.(20) In this analysis, we created replicated observations to standardize (reweight) observations to ensure balance across sex, age, WHR and BMI categories. The expected survival was computed as a weighted (based on the sampling weights) estimate of the per-participants estimated survival. A 95% bootstrap confidence interval based on the 2.5 and 97.5th percentiles of 500 replicates was calculated.
For a sensitivity analysis of the primary study, we repeated the analyses, excluding deaths that occurred within 6 months of enrollment, to account for undetected underlying conditions that could have caused these deaths and were unrelated to the BMI or central obesity status. In addition, we repeated the models adding physical activity, a candidate explanatory variable, to determine whether any association between adiposity and mortality was modified by physical activity.
Statistical significance was defined as P<0.05. Standard descriptive statistics and population estimates were calculated using the SURVEYMEANS and SURVEYFREQ procedures (SAS Institute Inc). This analysis accounted for the complex survey design, using pseudostrata, pseudoprimary sampling units, and sampling weights provided by the National Institute for Health Statistics.(21) The Taylor series linearization approach was used for variance estimation because it was recommended by NHANES.(21) The Cox models used for hazard ratio estimates were weighted similarly and calculated with SURVEYPHREG procedure in the SAS System version 9.3 (SAS Institute Inc). These models were confirmed with the estimates obtained from the r package survival (version 2.38-1 running on base r version 3.2.0), which was used to estimate the expected 5-year survival.
Results
Mean age of the 15,184 survey participants in this study was 45 years, and 7,935 (52.3%) were women. Of the 15,1. 84 people, 6,062 (39.9%) had normal BMI (18.5–24.9 kg/m2) and 5,249 (34.6%) and 3,873 (25.1%) were overweight (25–29.9 kg/m2) and obese (>=30.0 kg/m2) by BMI, respectively. In addition, 10,655 persons (70.2%) would be categorized as centrally obese using WHR World Health Organization criteria for central obesity (WHR>=0.85 in women and WHR>=0.90 in men). Meanwhile, only 4,381 persons (28.9%) met criteria for central obesity when we used waist circumference sex-specific criteria defined by the World Health Organization (>88 cm in women and >102 cm in men). Of persons with normal BMI, 322 (11.0%) of men and 105 (3.3%) of women had a large WHR (>1.0). Of persons with overweight BMI, 1064 (37.0%) of men and 289 (12.0%) of women had a large WHR. Of persons with obese BMI, 928 (63.0%) of men, and 336 (14.0%) of women had a large WHR (>1.0). The analysis of the association between the factors showed that while waist circumference was highly correlated with BMI (correlation coefficient, 0.87) and WHR was also related to BMI (correlation coefficient, 0.34), but to a less extent. The other baseline characteristics of participants stratified by sex are outlined in the Table 1.
Table 1.
Baseline Characteristics of Study Participants
| Characteristica | Participantsb
|
|
|---|---|---|
| Men (n=7,249) | Women (n=7,935) | |
| Age, y | 40.71(18.00;90.00) | 42.04(18.00;90.00) |
| Height, cm | 175.50 (139.40; 206.50) | 161.71(126.9;189.00) |
| Weight, kg | 79.81(40.70;241.80) | 66.04(32.50;213.50) |
| Body mass index, kg/m2 | 26.74(18.50;70.20) | 25.15(18.50;79.60) |
| Waist circumference, cm | 93.89 (62.80;174.10) | 86.52(59.4;170.4) |
| Hip circumference, cm | 98.55(69.10;179.20) | 100.15(69.90;174.70) |
| WHR | 0.94(0.51;1.56) | 0.85(0.55;2.09) |
| Education, No. (%) | ||
| <12 y completed | 3,152 (27.22) | 3,050 (24.30) |
| 12 y completed | 2,008 (30.72) | 2,693 (37.62) |
| ≥13 y completed | 2,044 (42.06) | 2,156 (38.10) |
| Race, No. (%) | ||
| White | 4,952 (84.93) | 5,279 (83.95) |
| African American | 2,029 (10.54) | 2,408 (12.26) |
| Other | 266 (4.53) | 246 (3.79) |
| Below Poverty level, No. (%) | 1,415 (10.96) | 1,896 (14.42) |
| Smoking history, No. (%) | ||
| Nonsmoker | 2,826 (38.50) | 4,977 (56.10) |
| Former smoker | 2,240 (29.98) | 1,286 (19.38) |
| Current smoker | 2,182 (31.52) | 1,672 (24.55) |
| History of myocardial infarction, No. (%) | 388 (4.21) | 206 (2.17) |
| History of hypertension, No. (%) | 2,487 (29.49) | 2,737 (29.17) |
| Systolic blood pressure, mm Hg | 121.06(80.00;244.00) | 114.10(69.00;237.00) |
| Diastolic blood pressure, mm Hg | 75.44(23.00;134.00) | 70.78(20.00;126.00) |
| History of diabetes mellitus, No. (%) | 769 (7.20) | 919 (7.54) |
| Fasting Serum insulin, pmol/L | 58.9(12.20;16438.00) | 56.60(12.20;6046.90) |
| Fasting Plasma glucose, mmol/L | 5.26(1.96;35.67) | 5.04(2.35;32.98) |
| Glycated hemoglobin, % | 5.20(3.0;16.2) | 5.10(3.30;16.10) |
| History of hyper-cholesterolemiac, No. (%) | 1,042 (34.59) | 1,443 (33.92) |
| Total cholesterol, mmol/L | 5.12(1.53;18.16) | 5.14(2.09;17.48) |
| Serum LDL cholesterol, mgd/L | 3.27(0.52;9.83) | 3.12(0.52;9.34) |
| Serum HDL cholesterol, mg/dL | 1.11(0.21;4.16) | 1.36(0.30;5.07) |
| Serum triglycerides, mgld/L | 1.36(0.25;40.84) | 1.17(0.26;25.58) |
| Disease history, No. (%) | ||
| Heart failure | 256 (1.97) | 218 (1.70) |
| Stroke | 172 (1.60) | 166 (1.61) |
| Asthma | 469 (7.55) | 584 (7.89) |
| Chronic bronchitis | 284 (4.05) | 522 (7.80) |
| Emphysema | 165 (2.22) | 84 (1.04) |
| Physical Activity, No. (%) | ||
| Inactive | 1,063 (9.7) | 2,008 (17.3) |
| Insufficiently active | 2,315 (31.9) | 2,787 (35.1) |
| Active | 3,871 (58.4) | 3,140 (47.6) |
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein; WHR, waist-to-hip ratio.
Values are expressed as mean±SD unless specified otherwise.
Denominator may not always total to 15,184 for all participants, 7,249 for men, and 7,935 for women because of missing values.
Total Cholesterol Value higher than 200 mg/dL
There were 3,222 deaths (1413 in women) over a mean follow-up of 14.3 years, of which 1,404 were cardiovascular deaths. The results of the multivariable Cox proportional hazards analysis showed that WHR, but not BMI, was associated with high mortality risk after including both variables in the model (Supplemental Tables 1 and 2). On the basis of the results from this model, we estimated hazard ratios for total and cardiovascular death attributed to normal-weight central obesity in comparison with other groups.
Individual comparison results for different combinations of BMI, central adiposity, and total death are presented in Figure 1. Men (Figure 1a) with normal-weight central obesity (profile 2) would have a higher total mortality risk than participants with any other combinations of BMI and WHR. Specifically, a person with normal-weight central obesity had an 87% higher mortality risk than a person with similar BMI but no central obesity (profile 1; HR=1.87 for profile 2 vs. 1) and had over a 2-fold higher mortality risk compared with a person who was overweight (profile 3) or obese (profile 5) by BMI without central adiposity. A woman with normal-weight central obesity (profile 2, Figure 1b) had a 48% higher total mortality risk than a person with similar BMI but no central obesity (profile 1) and had 40% and 32% higher risk than a person who was overweight and obese by BMI but without central obesity, profiles 3 and 5 respectively. In the sensitivity analyses, exclusion of early deaths in follow-up assessment (first 6 months) from analysis did not change the results. Cardiovascular mortality showed the same relationship: a man with normal-weight central obesity had a higher cardiovascular mortality risk than a person with similar BMI but not central obesity (HR 1.78; 95%CI-1.23–2.57). A woman with normal-weight central obesity had over a 2-fold higher cardiovascular mortality risk compared with a person with similar BMI but without central obesity (HR 2.25; 95%CI 1.66 – 3.05).
Figure 1.
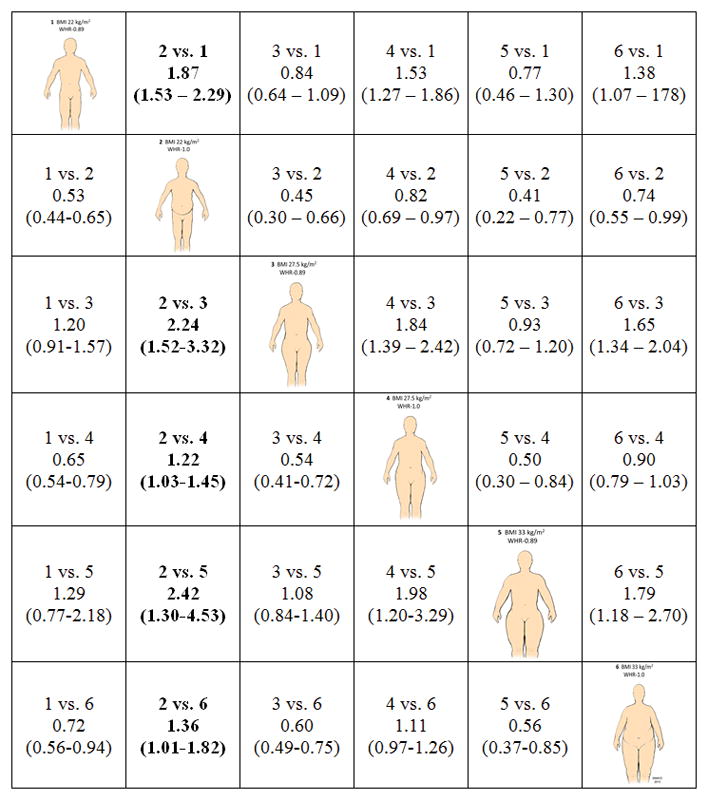
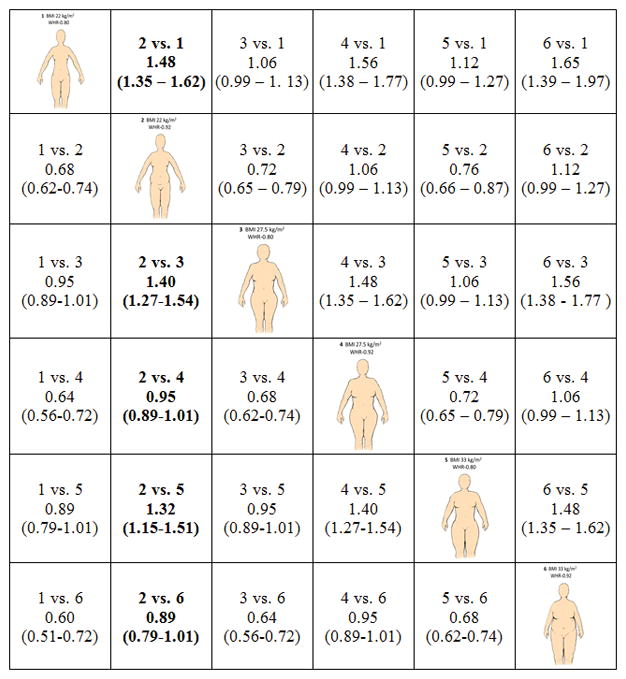
Hazard ratios and 95% CIs for all-cause mortality for men (Figure 1a) and women (Figure 1b) as estimated by statistical models presented in Supplemental Tables 1 and 2. To interpret the hazard ratios, select an intersection of two anthropometric profiles of interest. The group of interest (i) relative to the referent (j) is indicated as entries “i vs. j” in the table cells. For example, to compare a normal weight but centrally obese male (profile 2; BMI = 22, WHR = 1.0) relative to an overweight but not centrally obese person (profile 4; BMI =27.5, WHR = 1.0), the cell in row 4, column 2 would be referenced (Denoted 2 vs. 4 with HR = 1.22 and 95% CI: 1.03 to 1.45).
Tables 2 and 3 presents the standardized expected mortality estimates for males and females, respectively. These results have been normalized to reflect a similar composition of the risk factors adjusted in the models. For men, the effect of central obesity has a pronounced impact on five- and 10-year survival across all age groups. The pattern of rank ordering of expected survival within age group or overall consistently favors those people with less central obesity. The same general pattern is observed in women.
Table 2.
Expected mortality and 95% bootstrap confidence intervals for males
| Age | BMI | WHR | 5-year mortality
|
10-year mortality
|
||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | |||
| 40 | 22 | 0.89 | 1.1 | (0.8, 1.4) | 2.8 | (2.1, 3.4) |
| 1.00 | 2.1 | (1.6, 2.7) | 5.1 | (4.1, 6.6) | ||
|
| ||||||
| 27.5 | 0.89 | 0.9 | (0.7, 1.2) | 2.3 | (1.7, 2.9) | |
| 1.00 | 1.7 | (1.4, 2.1) | 4.2 | (3.4, 4.9) | ||
|
| ||||||
| 33 | 0.89 | 0.9 | (0.5, 1.3) | 2.2 | (1.3, 3.2) | |
| 1.00 | 1.6 | (1.2, 1.9) | 3.8 | (3.0, 4.6) | ||
|
| ||||||
| 37 | 0.89 | 0.9 | (0.5, 1.5) | 2.2 | (1.2, 3.6) | |
| 1.00 | 1.5 | (1.2, 2.0) | 3.8 | (2.9, 4.9) | ||
|
| ||||||
| 50 | 22 | 0.89 | 2.3 | (1.8, 2.9) | 5.7 | (4.5, 6.7) |
| 1.00 | 4.3 | (3.5, 5.3) | 10.3 | (8.7, 12.5) | ||
|
| ||||||
| 27.5 | 0.89 | 1.9 | (1.4, 2.5) | 4.8 | (3.6, 5.9) | |
| 1.00 | 3.5 | (3.0, 4.1) | 8.5 | (7.4, 9.5) | ||
|
| ||||||
| 33 | 0.89 | 1.8 | (1.2, 2.6) | 4.4 | (2.7, 6.3) | |
| 1.00 | 3.2 | (2.6, 3.8) | 7.7 | (6.4, 9.1) | ||
|
| ||||||
| 37 | 0.89 | 1.8 | (1.0, 3.0) | 4.4 | (2.4, 7.2) | |
| 1.00 | 3.1 | (2.5, 4.0) | 7.6 | (6.0, 9.6) | ||
|
| ||||||
| 60 | 22 | 0.89 | 4.7 | (3.8, 5.8) | 11.3 | (9.3, 13.2) |
| 1.00 | 8.7 | (7.2, 10.2) | 20.1 | (17.7, 23.6) | ||
|
| ||||||
| 27.5 | 0.89 | 4.0 | (2.9, 5.0) | 9.6 | (7.3, 11.8) | |
| 1.00 | 7.2 | (6.2, 8.0) | 16.8 | (15.0, 18.3) | ||
|
| ||||||
| 33 | 0.89 | 3.7 | (2.4, 5.4) | 8.9 | (5.7, 12.7) | |
| 1.00 | 6.5 | (5.4, 7.7) | 15.3 | (12.9, 17.5) | ||
|
| ||||||
| 37 | 0.89 | 3.7 | (2.1, 6.2) | 9.0 | (4.9, 14.3) | |
| 1.00 | 6.4 | (5.1, 8.3) | 15.0 | (12.2, 18.3) | ||
|
| ||||||
| 70 | 22 | 0.89 | 9.6 | (7.7, 11.7) | 21.9 | (18.2, 25.7) |
| 1.00 | 17.1 | (14.4, 20.0) | 36.6 | (32.8, 41.3) | ||
|
| ||||||
| 27.5 | 0.89 | 8.1 | (5.9, 10.2) | 18.7 | (14.3, 22.9) | |
| 1.00 | 14.2 | (12.4, 16.0) | 31.3 | (28.4, 33.9) | ||
|
| ||||||
| 33 | 0.89 | 7.5 | (4.9, 10.8) | 17.5 | (11.4, 24.9) | |
| 1.00 | 12.9 | (10.7, 15.4) | 28.7 | (24.6, 32.7) | ||
|
| ||||||
| 37 | 0.89 | 7.5 | (4.4, 12.5) | 17.6 | (9.8, 27.5) | |
| 1.00 | 12.7 | (10.2, 16.4) | 28.4 | (23.3, 34.4) | ||
Table 3.
Expected mortality and 95% bootstrap confidence intervals for females.
| Age | BMI | WHR | 5-year mortality
|
10-year mortality
|
||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | |||
| 40 | 22 | 0.80 | 0.5 | (0.4, 0.6) | 1.5 | (1.2, 1.8) |
| 0.92 | 0.7 | (0.5, 0.9) | 2.2 | (1.7, 2.7) | ||
|
| ||||||
| 27.5 | 0.80 | 0.5 | (0.4, 0.6) | 1.6 | (1.3, 1.9) | |
| 0.92 | 0.7 | (0.6, 0.9) | 2.3 | (1.9, 2.8) | ||
|
| ||||||
| 33 | 0.80 | 0.5 | (0.4, 0.7) | 1.6 | (1.3, 2.0) | |
| 0.92 | 0.8 | (0.6, 1.0) | 2.4 | (2.0, 3.0) | ||
|
| ||||||
| 37 | 0.80 | 0.5 | (0.4, 0.7) | 1.7 | (1.3, 2.1) | |
| 0.92 | 0.8 | (0.6, 1.0) | 2.5 | (2.0, 3.2) | ||
|
| ||||||
| 50 | 22 | 0.80 | 1.1 | (0.8, 1.3) | 3.3 | (2.7, 3.9) |
| 0.92 | 1.6 | (1.3, 1.9) | 4.8 | (4.1, 5.7) | ||
|
| ||||||
| 27.5 | 0.80 | 1.1 | (0.9, 1.4) | 3.5 | (2.9, 4.1) | |
| 0.92 | 1.7 | (1.4, 2.0) | 5.1 | (4.4, 5.9) | ||
|
| ||||||
| 33 | 0.80 | 1.2 | (0.9, 1.5) | 3.7 | (3.0, 4.4) | |
| 0.92 | 1.7 | (1.4, 2.1) | 5.4 | (4.6, 6.3) | ||
|
| ||||||
| 37 | 0.80 | 1.2 | (1.0, 1.6) | 3.8 | (3.1, 4.7) | |
| 0.92 | 1.8 | (1.4, 2.3) | 5.6 | (4.7, 6.7) | ||
|
| ||||||
| 60 | 22 | 0.80 | 2.4 | (1.9, 2.9) | 7.3 | (6.2, 8.3) |
| 0.92 | 3.5 | (3.0, 4.1) | 10.6 | (9.3, 11.9) | ||
|
| ||||||
| 27.5 | 0.80 | 2.5 | (2.1, 3.0) | 7.7 | (6.7, 8.8) | |
| 0.92 | 3.7 | (3.2, 4.3) | 11.2 | (10.1, 12.3) | ||
|
| ||||||
| 33 | 0.80 | 2.7 | (2.2, 3.2) | 8.1 | (6.9, 9.5) | |
| 0.92 | 3.9 | (3.3, 4.6) | 11.8 | (10.4, 13.2) | ||
|
| ||||||
| 37 | 0.80 | 2.8 | (2.2, 3.5) | 8.5 | (6.9, 10.1) | |
| 0.92 | 4.1 | (3.3, 5.0) | 12.2 | (10.5, 14.1) | ||
|
| ||||||
| 70 | 22 | 0.80 | 5.3 | (4.3, 6.3) | 15.7 | (13.5, 17.8) |
| 0.92 | 7.7 | (6.7, 9.0) | 22.2 | (20.0, 24.3) | ||
|
| ||||||
| 27.5 | 0.80 | 5.6 | (4.6, 6.6) | 16.5 | (14.2, 18.5) | |
| 0.92 | 8.2 | (7.1, 9.4) | 23.3 | (21.5, 25.0) | ||
|
| ||||||
| 33 | 0.80 | 5.9 | (4.7, 7.2) | 17.3 | (14.6, 19.9) | |
| 0.92 | 8.6 | (7.4, 10.0) | 24.4 | (22.0, 26.8) | ||
|
| ||||||
| 37 | 0.80 | 6.2 | (4.8, 7.8) | 18.0 | (14.6, 21.2) | |
| 0.92 | 8.9 | (7.4, 10.8) | 25.2 | (22.0, 28.5) | ||
Discussion
Our analyses of data from a large cohort of NHANES III participants show that US adults with normal weight but central obesity have the worst long-term survival compared with participants with normal fat distribution, regardless of BMI category, and even after adjusting for potential mediators. These results confirm and expand the findings of other population-based studies in adults aged 18 years or older by addressing the value of combining measures of central obesity and overall adiposity for predicting mortality risk.(2, 3, 7) Prior studies showed that, even in people with normal weight by BMI, measures of central obesity were independently related to the increased risk of mortality in the general population.
Our study not only specifically addressed the mortality risk associated with central obesity in persons with normal weight, but also compared the absolute mortality risk in this group with overweight and obese persons by BMI with or without central obesity. We also tested the independence of the association by adjusting for obesity-related cardiovascular risk factors, demonstrating that the association between normal weight central obesity and increased mortality cannot be solely attributed to those risk factors. Our study demonstrates for first time, that normal-weight central obesity, as determined by WHR, is associated with an increased risk of cardiovascular mortality. Our findings may have significant clinical implications, as individuals with normal BMI but central obesity were not considered a priority population for prevention programs by guideline developers.” Indeed, the 2013 AHA/ACC Obesity Management Guidelines recommend measuring waist circumference only in individuals with elevated BMI and do not recommend calculating the waist to hip ratio at all(9); thereby implying that people with normal BMI are free of any particular adiposity-related risk.
While this and other studies have shown that WHR and waist circumference are superior to BMI in prediction of total and cardiovascular disease mortality rates,(2, 12, 22) there are other studies showing different results.(6) Data from the Emerging Risk Factors Collaboration showed that WHR, waist circumference, and BMI had a similar strength of association with cardiovascular disease risk only after accounting for intermediate cardiovascular risk factors between obesity and mortality, such as blood pressure, history of diabetes, and cholesterol values, and analyzing the variables assuming linearity of any association.(6) In their secondary analyses, the authors reported that for any given tertile of BMI, measures of central obesity were still related to mortality, even in persons with a BMI of 20 to 24.5.(6) Our study was based on simultaneous assessment of the influence of individual combinations of BMI and WHR on survival to capture any effect modification that WHR could have at different levels of BMI. Additionally, our study underlined independent prognostic information of central obesity in persons with normal weight by BMI, beyond obesity-related cardiovascular risk factors.
There are several possible explanations for our findings. First, central obesity measured by WHR is associated with visceral fat accumulation and an adverse metabolic profile compared with BMI, which is a measure of both lean and fat mass.(23, 24) Indeed, our analysis showed that BMI was only weakly correlated with WHR, proving that WHR provides different information than BMI. Second, excessive visceral fat is associated with insulin resistance, hypertriglyceridemia, dyslipidemia, and inflammation.(25, 26) A higher WHR is associated with decreased muscle mass in the legs, called sarcopenic adiposity, and accompanied by higher glucose levels and increased cardiovascular risk.(14, 22) Third, persons who are overweight or obese on the basis of their BMI may have larger amounts of subcutaneous fat in the hips and legs—fat linked to healthier metabolic profiles.(17) This may explain the unexpected better survival in overweight or obese persons, even among those who were centrally obese.
The strengths of our study include first, the use of standardized data from a large cohort of participants in a representative US population sample, which increases the external validity of our results. Second, WHR is a simple and reliable measure for visceral obesity (22) and was measured simultaneously with BMI in this study population. At the same time, several limitations of our study should be recognized, including some that are intrinsic to the NHANES surveys. Information on comorbidities, such as hypertension, diabetes, and dyslipidemia, was self- reported by participants, which potentially can lead to error. Waist circumference was measured using a technique different than the one suggested by the World Health Organization or scientific societies. Thus, our results may not apply to studies that assessed the WHR using other techniques. We cannot exclude misclassification bias related to changes in weight and WHR during the follow-up. However, it is a widely accepted strategy in epidemiologic studies to use baseline measures, including exposure and confounding variables. In addition, information on body fat distribution was based on anthropometric indicators alone, such as WHR. Imaging data of adipose tissue would provide additional information but were not collected in the NHANES III survey. Finally, we cannot exclude misclassification related to measurement errors in our exposure variables, such as WHR and BMI.
Our findings suggest that individuals with normal-weight central obesity may represent an important target population for lifestyle modification and other preventive strategies. Future studies should focus on identifying factors associated with development of normal weight central obesity and providing a better understanding of the effect of normal weight central obesity on health outcomes. Until such data are available, use of BMI with measures of central obesity may provide better adiposity-related risk factor stratification in clinical practice than either method alone.
Supplementary Material
Acknowledgments
Primary Funding Source: This work was supported by National Institutes of Health Grant [HL00711-36 to KRS], American Heart Association [11SDG7260046 to PS], European Regional Development Fund [Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123 to VKS, OS, PS, and FLJ]), and Czech Ministry of Health [NT13434-4/2012 to OS].
None
Footnotes
Conflict of Interest: None declared
Reproducible Research Statement
Protocol: available at ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/nhanes/nhanes3/1A/ADULT-acc.pdf Statistical Code and Data are available at http://www.cdc.gov/nchs/nhanes/nh3data.htm
References
- 1.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami HO, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clinic proceedings. 2014;89(3):335–45. doi: 10.1016/j.mayocp.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahn HS, Bullard KM, Barker LE, Imperatore G. Differences between adiposity indicators for predicting all-cause mortality in a representative sample of United States non-elderly adults. PloS one. 2012;7(11):e50428. doi: 10.1371/journal.pone.0050428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA : the journal of the American Medical Association. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. European journal of clinical nutrition. 2007;61(12):1373–9. doi: 10.1038/sj.ejcn.1602656. [DOI] [PubMed] [Google Scholar]
- 6.Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–95. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reis JP, Macera CA, Araneta MR, Lindsay SP, Marshall SJ, Wingard DL. Comparison of overall obesity and body fat distribution in predicting risk of mortality. Obesity. 2009;17(6):1232–9. doi: 10.1038/oby.2008.664. [DOI] [PubMed] [Google Scholar]
- 8.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. The American journal of clinical nutrition. 2009;89(4):1213–9. doi: 10.3945/ajcn.2008.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–38. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashwell M, Mayhew L, Richardson J, Rickayzen B. Waist-to-height ratio is more predictive of years of life lost than body mass index. PloS one. 2014;9(9):e103483. doi: 10.1371/journal.pone.0103483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 12.Coutinho T, Goel K, Correa de Sa D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of “normal weight central obesity”. Journal of the American College of Cardiology. 2013;61(5):553–60. doi: 10.1016/j.jacc.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 13.Romero-Corral A, Somers VK, Sierra-Johnson J, Korenfeld Y, Boarin S, Korinek J, et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010;31(6):737–46. doi: 10.1093/eurheartj/ehp487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. International journal of obesity. 2010;34(5):791–9. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 15.Chowdhury B, Lantz H, Sjostrom L. Computed tomography-determined body composition in relation to cardiovascular risk factors in Indian and matched Swedish males. Metabolism: clinical and experimental. 1996;45(5):634–44. doi: 10.1016/s0026-0495(96)90036-0. [DOI] [PubMed] [Google Scholar]
- 16.Seidell JC, Bjorntorp P, Sjostrom L, Sannerstedt R, Krotkiewski M, Kvist H. Regional distribution of muscle and fat mass in men--new insight into the risk of abdominal obesity using computed tomography. International journal of obesity. 1989;13(3):289–303. [PubMed] [Google Scholar]
- 17.Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. International journal of obesity. 2010;34(6):949–59. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics OoAaE. The Third National Health and Nutrition Examination Survey (NHANES III) Linked Mortality file, Mortality follow-up through 2006: matching methodology. Hyattsville (MD): 2009. May, Available at http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhanes3_final.pdf. [Google Scholar]
- 19.Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. Springer Science & Business Media; 2003. [Google Scholar]
- 20.Makuch RW. Adjusted survival curve estimation using covariates. Journal of chronic diseases. 1982;35(6):437–43. doi: 10.1016/0021-9681(82)90058-3. [DOI] [PubMed] [Google Scholar]
- 21.Survey NHaNE. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Health Statistics; Available at: http://www.cdc.gov/nchs/about/major/nhanes/NHANESIII_Reference_Manuals.htm.Accesses. [Google Scholar]
- 22.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366(9497):1640–9. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 23.Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444(7121):875–80. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 24.Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. The Journal of clinical endocrinology and metabolism. 2004;89(6):2595–600. doi: 10.1210/jc.2004-0372. [DOI] [PubMed] [Google Scholar]
- 25.Navab M, Anantharamaiah GM, Fogelman AM. The role of high-density lipoprotein in inflammation. Trends in cardiovascular medicine. 2005;15(4):158–61. doi: 10.1016/j.tcm.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Despres JP. Intra-abdominal obesity: an untreated risk factor for Type 2 diabetes and cardiovascular disease. Journal of endocrinological investigation. 2006;29(3 Suppl):77–82. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


