Abstract
Resident participation in international health electives (IHEs) has been shown to be beneficial, yet not all residents have the opportunity to participate. We sought to determine whether participating in simulated global health cases, via the standardized Simulation Use for Global Away Rotations (SUGAR) curriculum, was useful for all pediatric residents, not merely those planning to go on an IHE. Pediatric residents in our program took part in 2 SUGAR cases and provided feedback via an online survey. Thirty-six of 40 residents participated (90%); 72% responded to the survey. Three of 10 residents not previously planning to work in resource-limited settings indicated participation in SUGAR made them more likely to do so. Nearly all residents (88%) felt SUGAR should be part of the residency curriculum. All felt better prepared for working cross-culturally. While designed to prepare trainees for work in resource-limited settings, SUGAR may be beneficial for all residents.
Keywords: SUGAR, global health, global health simulation, international health elective, IHE, pediatrics, debriefing
Introduction
In 2014, nearly 1 in 6 pediatric residents in the United States participated in an international health elective (IHE) in a resource-limited setting.1 This increased activity occurs against a backdrop of a growing awareness of the importance of providing global health (GH) education for all residents, not merely those planning to travel during residency.2-5 Much of what is known about the benefits of GH education comes from residents who have participated in IHEs. Many report feeling better equipped to handle complex diseases and advanced stages of disease presentation and cite a newfound appreciation of the value of a physical examination over complex and expensive investigations.6-10 During these IHEs, residents report being able to hone interpersonal skills, work on effective communication, improve empathy, and better understand the importance of cultural humility.2,11,12 Despite these benefits, many residency programs are not able to offer IHEs to their residents for reasons including lack of international partnerships or institutional mentors or the inability to support residents’ salaries.1
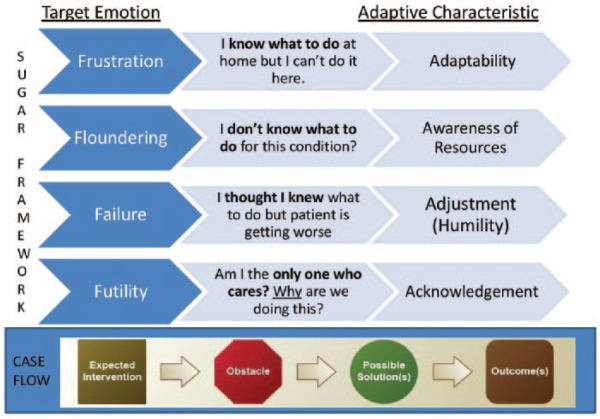
Simulation Use for Global Away Rotations (SUGAR) is a standardized simulation-based curriculum developed and evaluated by a multi-institutional consortium to give residents the opportunity to experience and debrief common practical and emotional challenges of working in resource-limited settings prior to their IHE.13 Participation in SUGAR has been shown to increase a sense of preparedness for IHEs with residents reporting that the simulations elicited strong emotions mirroring those encountered abroad and led to anticipated changes to pretravel preparation.13 Residents continued to report that the sessions were valuable on returning from their electives.14 The curriculum is open-source and available online with facilitator training and downloadable cases (sugarprep.org), and is used widely in residency programs across the country.14 The SUGAR paradigm for eliciting the desired emotions and adaptive characteristics through simulation and debriefing is summarized in Figure 1.
Figure 1.
The SUGAR paradigm.
While SUGAR has been shown to be beneficial in preparing residents to participate in IHEs, it had not been evaluated for residents without a dedicated GH interest. As participation in IHEs has been shown to have benefits to learners, and not all residents will go on an IHE either by choice or due to lack of opportunity, we sought to determine whether this curriculum could be beneficial for all pediatric residents, regardless of whether they planned to participate in an IHE.
Methods
This study took place within the pediatric residency program at the Mayo Clinic in Rochester, Minnesota, with approval from of the institutional review board. During the study period, the residency program consisted of 40 residents; 36 categorical pediatric residents and 4 pediatric neurology residents whose first 2 years are spent in the pediatric residency.
Two Mayo Clinic faculty members (JRR and PRF) were involved in the consortium responsible for piloting SUGAR along with 2 offsite faculty members who cocreated the curriculum (MBP and SMB). One additional Mayo Clinic faculty member (GMA) received in-person training in SUGAR facilitation. The 3 Mayo Clinic faculty members carried out the simulations and debriefing.
Each resident was scheduled to participate in 2 SUGAR scenarios during 1 of 3 afternoon sessions. The scenarios chosen were previously validated as part of the SUGAR curriculum,13 and were held in the Mayo Clinic Simulation Center between July and September 2014 lasting 3 hours each. Residents were divided into 2 groups of 2 to 4 residents per scenario. As perception of the value of SUGAR was shown to be no different between observers and active participants in the sessions,13 the groups alternated roles between active participation and observation during the simulation, with observers watching a live video stream of the participants in the scenario.
The same 2 scenarios were used for all groups. In the first scenario, residents are confronted with the presentation of a diagnosis they likely know little about—lymphocytic interstitial pneumonitis (LIP), a complication seen in HIV infection. During the scenario, the residents must figure out how to set up an oxygen tank and improvise an oxygen delivery device urgently while trying to diagnose the patient’s symptoms without access to immediate chest radiography, laboratory examinations, or the needed medications. This scenario was designed to guide the residents from a feeling of floundering to a sense of awareness and empowerment as they utilize available resources and manage an unfamiliar disease.
The second scenario was designed to help usher residents from a feeling of failure to adjustment and humility. In this scenario, residents often initially feel confident in treating what they believe to be nephrotic syndrome. However, as the patient’s clinical status worsens with therapy, they ideally realize that the patient is presenting with severe acute malnutrition that can have a similar clinical presentation but requires different treatment. Learners recognize that falsely presuming that patients will have the same diseases that residents are accustomed to managing can be harmful.
On completion of the first scenario, participants and observers for each scenario then engaged in a debriefing session together with a faculty facilitator using the scripted debriefing tool provided in the SUGAR curriculum.13,15 Participants and observers then switched roles and engaged in the second scenario followed by a second debriefing period.
After the simulation experience, an anonymous, voluntary online survey was sent to all of the pediatric residents. In addition to the 11 Likert-type scale questions, residents were provided with an open-ended comment box to expand on any question and/or provide feedback. The principle outcomes of interest included (1) residents’ perception of the usefulness of SUGAR for all pediatric residents, not only for residents interested in GH and (2) whether the residents considered themselves better prepared to deal with cross-cultural patient interactions following the sessions.
Results
Results are summarized in Figure 2. Thirty-six of the 40 pediatric residents participated in the sessions (90%). Twenty-six participants responded to the survey (72%). Nearly all respondents (23/26, 88%) felt these sessions should be part of the general pediatric curriculum. Sixteen of the respondents (61%) had planned to participate in GH experiences prior to the SUGAR sessions including pursuing an IHE during residency (13), volunteering (15), or working in resource-limited settings (14). All residents in each of these categories remained as likely (31%, 47%, 36%, respectively) or became more likely (69%, 53%, 64%) to pursue GH opportunities after the sessions. After participating in the SUGAR curriculum, none of the 26 respondents reported being less likely to participate in IHEs, volunteer, or work in resource-limited settings. Three of the 10 residents (30%) who had not previously planned to volunteer or work in a resource-limited setting and 2 (2/13, 15%) of the residents not planning to engage in IHEs prior to the sessions indicated they were more likely to do so. All respondents reported that they felt better prepared for providing cross-cultural care.
Figure 2.
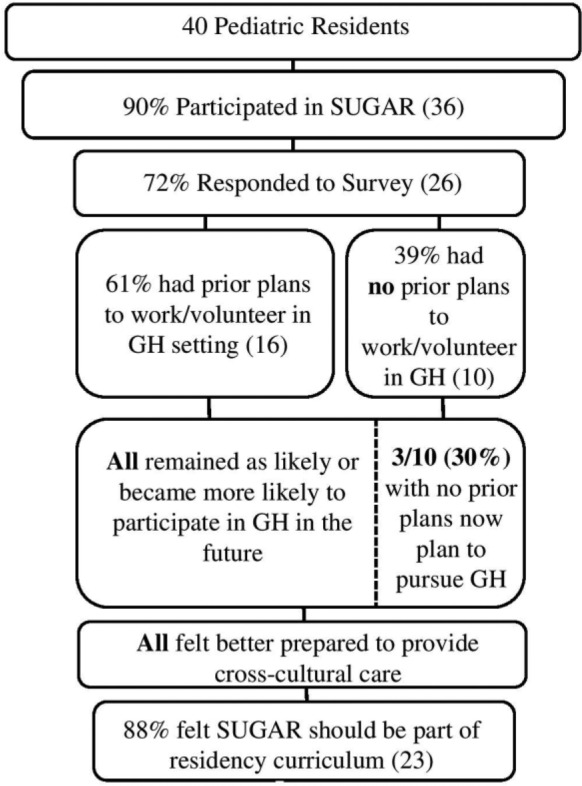
Survey results and pediatric resident’s responses to SUGAR sessions.
Five residents provided written comments. A trainee who had already planned to engage in GH work prior to the session and who indicated being even more likely to do so after the session commented,
Given increased travels in and around the world I believe a better appreciation of global health will be useful to all clinician[s] whether you plan to incorporate global health into a long or short term career goal or not. It is a learning opportunity that all residents must avail themselves to.
One resident who had no prior plans to volunteer/work in resource-limited settings before or after the session felt that everyone should participate in these simulated scenarios whether or not they planned to engage in GH efforts. That resident commented, “I will admit it was a very nerve-wracking experience, but it was also eye opening for me as far as how little I know about some global health/limited resource setting issues.”
Discussion
Our study showed that SUGAR may be helpful for all residents, regardless of their plans or ability to do an IHE. Participation in IHEs in settings with limited resources has been shown to have several benefits for the learners who report feeling better prepared to identify and manage advanced complex diseases, gain confidence in the use of physical exam skills rather than relying on expensive diagnostic tests and procedures, and refine communication skills and awareness of the need for cultural humility.2,6-12 Yet most residents do not participate in an IHE during residency either by choice or lack of opportunity. Participating in simulated scenarios that mimic the experiences residents encounter on IHEs may allow some of the benefits of these experiences to be gained by residents not planning to do an IHE.
SUGAR scenarios were initially developed to allow trainees to confront common emotionally uncomfortable situations while remaining in a psychologically safe and controlled environment with ample time for debriefing and reflection. Residents who have participated in this curriculum prior to their IHE described feeling strong emotions during the simulations, the majority of which were negative (eg, frustration, helplessness) mirroring the types of emotions often encountered on an IHE.13 We wondered whether participating in these scenarios prior to travel might deter residents’ eagerness to pursue international rotations or future GH work. If this process did lead some to reconsider their plans based on how they coped during the simulated scenarios, then we felt this could actually be a potential benefit to the learner who might reassess their goals and possibly be protected from encountering these challenging emotions thousands of miles from home without readily available support structures. In our study, however, all of the residents who had planned to engage in GH activities as part of their short-term (IHE) or long-term career goals were as likely or more likely to follow these ambitions after the session. An unexpected finding was that as a result of participating in the sessions, some (3/10) of those who had not previously planned to participate in GH activities reported that they were more likely to do so after the SUGAR sessions. While it is premature to determine whether this desire will manifest, the possibility of expanding the GH workforce and resultant benefit to society may be a positive unintended consequence of providing this curriculum to all residents. We know, for example, that residents who participate in IHEs are more likely to work in underserved or multicultural communities in the United States, pursue public health careers, and engage in community service in the future.16
In addition, regardless of plans to work in GH, all pediatricians will continue to care for an increasing number of children from different cultural backgrounds and confront diseases and conditions previously thought to be constrained by borders. Because all pediatricians will ultimately be faced with challenges relevant to GH in their careers, there is a growing demand for GH education to be a core topic for all residents.2-5,17 Yet in 2014 just slightly more than half (107/198; 54%) of pediatric residency programs were offering GH education for all.1 The fact that SUGAR is open-source and relatively easy to implement may provide an avenue for programs to begin to share GH educational content with their residents.
In this study, 100% of respondents indicated they felt better prepared to provide cross-cultural care as a result of participating in SUGAR. This has been previously reported by residents who engaged in SUGAR prior to IHEs. This perceived benefit increased dramatically once residents actually experienced the cultural differences of working abroad with a nearly 13-fold increase in the frequency of this feeling of cross-cultural preparedness on returning from the IHE relative to what they had indicated immediately after the simulation session.14 In our study, we found that even for those not planning to participate in GH work, involvement in the SUGAR sessions led to a perceived increase in the ability to provide cross-cultural care. Beyond the benefits to patients that this increased comfort may provide, it has also been found that residents with increased exposure to cross-cultural care have better job satisfaction and preparedness post residency.16
In the written comments, residents reported feeling better prepared to work with limited resources. This increased sense of preparation reflects the findings of the initial multi-institutional SUGAR study where comfort working with limited resource was cited as the greatest benefit of the cirriculum.13 Anecdotally, one resident later encountered an in-flight emergency in the United States and reported to the facilitators that the SUGAR session proved very helpful in dealing with that medical emergency. This sentiment highlights that resource limitation in health care is not limited to those working in low and middle income countries.
Our study has several limitations. First, it was carried out at a single institution. Second, while a response rate of 72% is reasonable, because of the limitation of numbers, those who did not respond could have had a measurable impact on the results. Also, while we aimed for consistency by having the same 2 SUGAR scenarios carried out for each group, we are limited in our ability to extrapolate the benefits of using different SUGAR scenarios which are available. However, since the themes of these different scenarios are similar, we hypothesize the effects would be comparable.
Conclusion
Simulating the challenges of providing care for children in resource-limited settings was deemed useful by nearly all of the residents in our program, regardless of their prior interest in GH. Several residents reported that as a result of participating in the scenarios they were more likely to work in GH in the future and all residents felt better prepared to provide cross-cultural care. As it is becoming increasingly evident that all pediatricians require training in GH as part of their residency, SUGAR—an open-source GH simulation curriculum previously studied in those planning on rotating at an international site—may provide an opportunity for residency programs to implement meaningful GH training for all of their residents, including those not able to offer IHEs.
Author Contributions
JRR contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
PRF contributed to conception and design; contributed to acquisition, analysis, and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
GMA contributed to acquisition and analysis; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MH contributed to interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
SMB contributed to conception and design; contributed to interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MBP contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Drs Butteris and Pitt have received institutional grant support from the University of Wisconsin Simulation Center and University of Minnesota African Studies Initiative for the dissemination of the SUGAR curriculum; none of this funding was used explicitly for this study.
References
- 1. Butteris SM, Schubert CJ, Batra M, et al. Global health education in US pediatric residency programs. Pediatrics. 2015;136:458-465. [DOI] [PubMed] [Google Scholar]
- 2. Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P. Global health in medical education: a call for more training and opportunities. Acad Med. 2007;82:226-230. [DOI] [PubMed] [Google Scholar]
- 3. Pitt MB, Gladding SP, Suchdev PS, Howard CR. Pediatric global health education past, present, and future. JAMA Pediatr. 2016;170:78-84. [DOI] [PubMed] [Google Scholar]
- 4. Garfunkel LC, Howard CR. Expand education in global health: it is time. Acad Pediatr. 2011;11:260-262. doi: 10.1016/j.acap.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 5. Stanton B, Huang CC, Armstrong RW, et al. Global health training for pediatric residents. Pediatr Ann. 2008;37:786-787, 792-796. [DOI] [PubMed] [Google Scholar]
- 6. Federico SG, Zachar PA, Oravec CM, Mandler T, Goldson E, Brown J. A successful international child health elective: the University of Colorado Department of Pediatrics’ experience. Arch Pediatr Adolesc Med. 2006;160:191-196. [DOI] [PubMed] [Google Scholar]
- 7. Daniels AH. International rotations during residency: spine deformity surgery in Ghana. R I Med J (2013). 2013;96(5):15-17. [PubMed] [Google Scholar]
- 8. Bjorklund AB, Cook BA, Hendel-Paterson BR, Walker PF, Stauffer WM, Boulware DR. Impact of global health residency training on medical knowledge of immigrant health. Am J Trop Med Hyg. 2011;85:405-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hau DK, Dipace JI, Peck RN, Johnson WD. Global health training during residency: the Weill Cornell Tanzania experience. J Grad Med Educ. 2011;3:421-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sawatsky AP, Rosenman DJ, Merry SP, McDonald FS. Eight years of the Mayo International Health Program: what an international elective adds to resident education. Mayo Clin Proc. 2010;85:734-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gladding S, Zink T, Howard C, Campagna A, Slusher T, John C. International electives at the university of Minnesota global pediatric residency program: opportunities for education in all Accreditation Council for Graduate Medical Education competencies. Acad Pediatr. 2012;12:245-250. [DOI] [PubMed] [Google Scholar]
- 12. Thompson MJ, Huntington MK, Hunt DD, Pinsky LE, Brodie JJ. Educational effects of international health electives on U.S. and Canadian medical students and residents: a literature review. Acad Med. 2003;78:342-347. [DOI] [PubMed] [Google Scholar]
- 13. Butteris SM, Gladding SP, Eppich WJ, Hagen SA, Pitt MB. Simulation Use for Global Away Rotations (SUGAR): preparing residents for emotional challenges abroad—a multicenter study. Acad Pediatr. 2014;14:533-541. doi: 10.1016/j.acap.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 14. Pitt MB, Gladding SP, Butteris SM. Using simulation for global health preparation. Pediatrics. 2016;137(5):e20154500. [DOI] [PubMed] [Google Scholar]
- 15. Eppich W, Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015;10:106-115. [DOI] [PubMed] [Google Scholar]
- 16. Ramsey AH, Haq C, Gjerde CL, Rothenberg D. Career influence of an international health experience during medical school. Fam Med. 2004;36:412-416. [PubMed] [Google Scholar]
- 17. Arnold LD. Improving global child health: why all pediatricians must “be the change.” Pediatrics. 2016;137(2):e20152748. [DOI] [PubMed] [Google Scholar]