Abstract
Primary care of children with autism spectrum disorders (ASD) is an important public health concerns. In this survey study of 73 pediatricians, we determined whether pediatricians’ practice of autism screening and perception of management of ASD is associated with participation in a learning collaborative, “Activated Autism Practice”. Overall, the majority recognized the lack of care coordination, inadequate time, poor reimbursement, and language difference as barriers to the delivery of medical care to children with ASD. Pediatricians with prior training were more likely to report use of autism-specific screening and understanding the different aspects of ASD management including the need to coordinate special services and long-term surveillance at pediatric sites. Therefore, participation in “Activated Autism Practice” may facilitate use of ASD-specific screening and manage ASD cases as a complex of neurodevelopmental/underlying problems with the need for enhancement of clinical attention and coordination of medical care at the pediatric primary care level.
Keywords: pediatricians, practice, autism, office-based education
Introduction
Autism spectrum disorders (ASD) is a group of lifelong neurodevelopmental disabilities that have been declared a public health emergency in the United States due to the significant increase in its prevalence over the past decade.1-3 Timely referral, treatment, and surveillance of children with ASD is improved with the use of the standardized autism-specific screening tool by general pediatricians.4-6 The American Academy of Pediatrics identified the fundamental role of pediatricians in ASD as screening and creating a medical home environment to coordinate and deliver services to the affected children.4 Besides, pediatricians and parents of children with ASD view the primary care pediatric setting as a resource for medical and developmental surveillance, navigation of specific health care services, and coordination of comprehensive family-centered care for children with ASD.7,8 Nevertheless, practicing pediatricians and pediatricians in training reported the need for special education to improve their competence for screening and management of children with autism.7,9 The effectiveness of several office-based training programs with a goal to improve screening and diagnostic of ASD have been evaluated.10-13 Significant improvement of ASD-related diagnostic attitudes and accuracy was shown by 27 community pediatricians who participated in a 2-day workshop that focused on ASD screening, diagnosis, and coding.10 Warren et al11 reported improvement of skills for evaluation and diagnosis of ASD in the 5 community pediatricians who participated in the “Screening Tools and Referral Training-Evaluation and Diagnosis Training” program. Training of 9 pediatricians by an autism specialist, at a community-based pediatric site, enabled the implementation of universal autism-specific screening.12 A study from Connecticut showed that delivery by child development specialists of a program “Educating Practices in the Community (EPIC)” improved the pediatricians’ practice of developmental screening in young children.13
In the present survey study, we intended to determine the extent to which prior participation of pediatricians in the office-based “Activated Autism Practice” program made a difference to their practice of autism-specific screening and perception regarding the role of pediatricians in the organization, coordination, and management of ASD children at community pediatric sites.
Methods
We conducted an anonymous mailing survey of 73 private pediatricians affiliated with Jersey Shore University Medical Center (JSUMC) including 34 who had previously participated in the “Activated Autism Practice” educational program (Group 1) and 39 pediatricians who had not (Group 2). The survey included 21 questions that allowed the obtaining of demographic data (board certification and type of practices) and information concerning (a) the use of autism-specific screening and subspecialty-referral system, (b) pediatrician’s role and potential barriers to management of children with autism at the primary care setting, (c) knowledge of early sign and autism associated medical conditions, and (d) belief in early recognition, surveillance, and continuation of medical care of patients with ASD at community pediatric sites. This survey study was approved by the Meridian Health Institutional Review Board.
Description of the “Activated Autism Practice” Educational Program
The main goal of the “Activated Autism Practice” educational program was to enhance ASD screening at primary care pediatric sites through the involvement of the entire practice staff in the autism-screening process and pediatric office workflow: (a) implementation of the Modified Checklist for Autism (M-CHAT) screening tool for well-baby visits at 18 months to 2 year old infants, (b) early referral of suspected ASD children for subspecialty evaluation, (c) office-based follow-up, and (d) parental education. In the frame of this program, neurodevelopmental pediatricians educated the primary care pediatricians regarding early autism-specific screening, clinical presentation of this condition, availability of community resources, and ways to access additional support services. During the implementation of the “Activated Autism Practice” educational program the neurodevelopmental pediatricians remained accessible for additional calls and to help with coordination of community support services. The scope of this service program did not include a formal evaluation of the results. Pediatricians affiliated with JSUMC were approached for participation in the “Activated Autism Practice” educational program at random, with 100% agreement to participate. Pediatricians who were also affiliated with the same hospital but were not previously approached to be part of the “Activated Autism Practice” educational program were included in Group 2
Data Presentation and Statistical Analysis
The study results are presented as a comparison of the demographic characteristics and responses to the autism-related questions by Group 1 pediatricians versus those in Group 2 using ANOVA and χ2 tests for the comparison of the continuous and categorical variables, respectively. A difference at 2-tailed P values of <.05 was considered statistically significant. Statistical analysis was performed using STATISTICA 12.0 for Windows (StatSoft Inc, Tulsa, OK).
Results
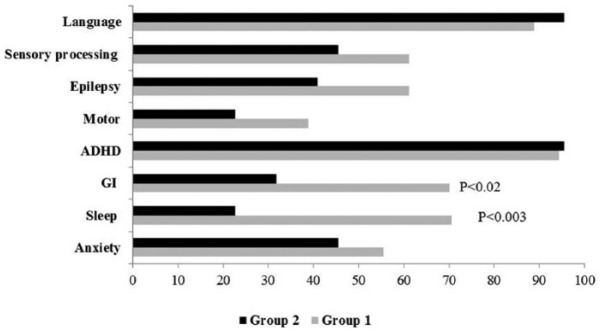
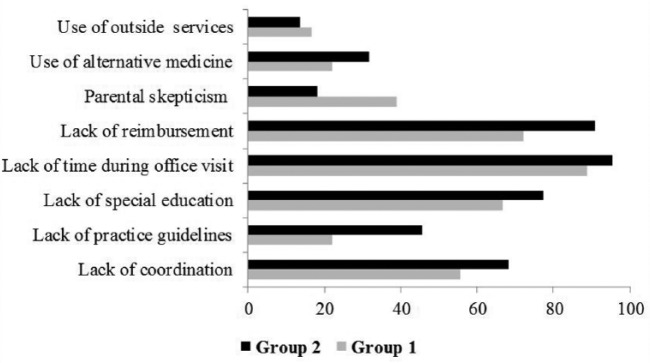
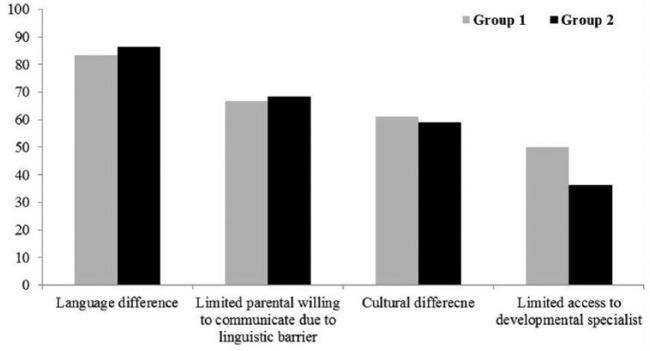
Among the surveyed pediatricians, 34 in Group 1 and 39 in Group 2, 52.9% and 56.4%, respectively, responded. All the respondent pediatricians were board certified, and the groups were comparable for years in practice (22.2 ± 9.5 vs 20.0 ± 9.5, P = .48). The majority of the pediatricians in Groups 1 and 2 were private practice groups (77.8% vs 59.0%, P = .36) and the rest were in solo practices. Pediatricians in Group 1 were more likely than those in Group 2 to report use of a modified checklist for autism-specific screening (Table 1). Almost half of the pediatricians in Group 2 performed neurodevelopmental evaluation without using screening tools and initiated assessment only if there was parental concern about the child’s condition. The age of screening reported by the pediatricians in Groups 1 and 2 was 53.9% and 35.3%, respectively, at 18 months, and 38.5% and 58.8%, respectively, at 24 months, P = .54. Irrespective of the group allocation, the majority identified problems with language development as the most specific and earliest sign of autism (Table 1). Language and social skill were reported by the majority of the pediatricians as probes that can be used for surveillance of patients with autism. Almost all identified family support as the mainstay for long-term management of children with autism. Pediatricians in Group 1 were more likely than those in Group 2 to recognize the development of functional independence, community engagement, and minimizing maladaptive behavior and psychiatric problems as goals for long-term management of children with ASD (P < .04-.001). The majority reported referring their suspected ASD patients for comprehensive diagnostic evaluation to neurodevelopmental pediatricians (72.25% vs 63.6%, P = .56), and the rest preferred to refer them to the pediatric neurologist. Pediatricians in Group 1 were more likely than those in Group 2 to list sleep disturbances and gastrointestinal problems as medical conditions associated with autism (Figure 1). In both groups, the majority believed in early recognition of autism for the prevention of severe maladaptive behavior and/or cognitive dysfunction/intellectual disability (87.5% vs 95.5%, respectively, P = .47) and early intensive behavioral therapy for the improvement of cognitive, language, and adaptive skills of children with autism (93.8% vs 100%, respectively). Lack of time during office visits, reimbursements, coordination of services, and special education were reported by the majority of pediatricians in Groups 1 and 2 as barriers to the provision of adequate primary care for children with ASD (Figure 2). Lack of practice guidelines was identified by 44.5% of pediatricians in Group 2 and 22.2% in Group 1 as a barrier for the primary care of children with autism (P = .12). In general, more pediatricians in Group 1 than in Group 2 identified the need for 3 or more primary care visits to the pediatric office, strongly agreed that the primary care pediatrician has an essential role in delivering general medical care, and were able to successfully coordinate special services for children with autism (Table 2). Only 29.4% of pediatricians in Group 1 and 13.6% in Group 2 thought that inclusion of nurse coordinators would have practical implications on management of children with autism (P = .22), and irrespective of the group allocation, the majority believed that the primary care pediatrician is not able to deliver special neurological services to children diagnosed with ASD. Responses of pediatricians in Groups 1 and 2 to the question regarding the barriers that may affect effectiveness of medical care of children with autism from Hispanic families with limited English proficiency were comparable (Figure 3).
Table 1.
Comparison of Pediatricians’ Responses Regarding Autism Screening, Surveillance, and Need for Long-Term Management.
| Characteristics | Group 1 (n = 18) | Group 2 (n = 22) |
|---|---|---|
| Use of autism-specific screening | 94.4% | 50.0%* |
| Screening tool used to screen for ASD | ||
| Checklist for autism | 11.1% | 18.2%* |
| Modified Checklist for Autism (M-CHAT) | 77.8% | 22.7% |
| Questions asked without using an actual screening tool | 5.6% | 31.8% |
| Other: Check card | 5.5% | — |
| Other: Parental concern | — | 27.3% |
| Specific and earliest sign of autism | ||
| Language probes | 70.6% | 77.3% |
| Restricted interests | 11.8 | 9.1% |
| Repetitive behavior probes | 0 | 4.6% |
| Delayed attainment of social skill | 17.7% | 9.1% |
| Clinical probes that can be used for autism surveillance | ||
| Social skill | 77.8% | 100%** |
| Language | 72.2% | 90.1% |
| Restricted interest | 33.3% | 31.8% |
| Repetitive behavior | 50.0% | 31.8% |
| Purpose of long-term management of children with autism | ||
| Provide support to the family | 94.4% | 95.5% |
| Maximize functional independence and community engagement | 94.4% | 54.6%* |
| Minimize maladaptive behavior | 83.3% | 27.3%** |
| Minimize psychiatric condition | 50.0% | 18.2%* |
Abbreviation: ASD, autism spectrum disorder.
P < .04-.02. **P <.01-.001.
Figure 1.
Comparison of pediatricians’ responses regarding medical problems, disorders, and impairments associated with autism.
Figure 2.
Comparison of physicians’ responses regarding the barriers to providing primary care for children with autism spectrum disorder.
Table 2.
Comparison of Pediatricians’ Responses Regarding Organization of Clinical Practices for Children With Autism.
| Questions | Group 1 (n = 18) | Group 2 (n = 22) |
|---|---|---|
| Do you think it would be practical to have a nurse coordinator in the primary care setting for the medical management of child with autism? | ||
| Yes | 29.4% | 13.6% |
| No | 47.1% | 72.7% |
| Not sure | 23.5% | 13.6% |
| How many times a year should a child with ASD be seen at the pediatrician office? | ||
| Once | 6.3% | 4.6%* |
| Two times | 43.8% | 68.2% |
| Three or more times | 44.4% | 18.2% |
| Not sure | — | 9.1% |
| Do you agree that for children with autism the primary care pediatrician has an essential role in delivering general medical care? | ||
| Strongly agree | 76.5% | 27.3%** |
| Agree | 23.5% | 54.6% |
| Neutral | 0 | 18.1% |
| Do you agree that for children with autism the primary care pediatrician is able to successfully deliver special neurological services? | ||
| Strongly agree | 12.5% | 4.8% |
| Agree | 12.5% | — |
| Neutral | 12.5% | 19.1% |
| Strongly disagree | 18.8% | 33.3% |
| Disagree | 43.8% | 42.9% |
| Do you agree that for children with autism the primary care pediatrician is able to successfully coordinate special services? | ||
| Strongly agree | 23.5% | 13.6%** |
| Agree | 52.9% | 9.1% |
| Neutral | 23.5% | 40.9% |
| Strongly disagree/disagree | — | 36.3% |
Abbreviation: ASD, autism spectrum disorder.
P < .04-.02. **P < .01-.001.
Figure 3.
Pediatricians’ opinion regarding factors that may affect effectiveness of medical care of children with autism from Hispanic families with limited English proficiency.
Discussion
Our survey study showed that community pediatricians who had previously participated in the office-based “Activated Autism Practice” training program were significantly more likely to report use of the autism-specific screening tool as compared to those who had not. Importantly, pediatricians in our study reported use of an appropriate screening tool 1 year after their participation in a training program, which demonstrates significance of office-based training for achievement of universal use of autism-specific screening of infants at the pediatric sites. In addition to previous reports,10-13 we identified an association between prior participation of pediatricians in the “Activated Autism Practice” training program and understanding of things necessary for management of ASD cases at community pediatric sites including autism-related comorbidities, surveillance, and coordination of specialized and medical care. We also found that irrespective of participation in a training program, the majority of pediatricians reported insufficiency of their knowledge regarding neurological and behavioral aspects of ASD, and barriers for the delivery of efficient care for children with autism. Comparable with other reports,8,14 pediatricians in our study identified lack of coordination of services, limited time for providing sufficient care, poor reimbursement, and linguistic as well as cultural differences for ASD patients from Hispanic families as the barriers to the delivery of quality care for ASD patients.
The results of our study should be discussed in light of the several limitations including risk for selection and nonresponse bias. Risk for selection bias is questionable because pediatricians were selected for participation in the “Activated Autism Practice” program at random from a group of community pediatricians comparable for the type and area of practice. Because of the anonymous nature of the survey, the demographic data of pediatricians who did not respond to the survey was not collected. A previous study showed that anticipated risk for nonresponse bias of surveyed pediatricians is associated with response rate. As such, the nonresponse bias for the demographic factors of surveyed pediatricians with a response rate of more than 52% is minimal.15 An overall response rate of 54.8% (40/73) was achieved in our study. Moreover, we surveyed only pediatricians from one area of New Jersey who are affiliated with JSUMC. However, replication of the study in other settings with larger samples is needed to validate and increase the external validity of the obtained results.
Despite the discussed limitations, we conclude that participation in “Activated Autism Practice” training program may possibly advance the practice of ASD-specific screening, delivery of comprehensive medical care, coordination of specialty services, and support for children with ASD and their families at community pediatric sites. In this regard, implementation of an office-based ASD educational program can be helpful for building a medical home environment for children with ASD at pediatric primary care settings. There is a need for the incorporation of special components in the training program to overcome gaps in specific medical knowledge, ability for coordination of disease-specific services, and cultural competence in addition to the implementation of the recommendations for office time utilization and reimbursement for ASD care at the pediatric primary care settings.
Author Contributions
SWK contributed to conception and design; contributed to acquisition of data; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
AP contributed to design; contributed to analysis and interpretation of data; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Acknowledgments
We would like to thank the general pediatricians who despite their time constraints participated in our survey study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005-2006. Pediatrics. 2008;122:e1149-e1158. [DOI] [PubMed] [Google Scholar]
- 2. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR Surveill Summ. 2009;58(10):1-20. [PubMed] [Google Scholar]
- 3. Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States. MMWR Surveill Summ. 2014;63(2):1-21. [PubMed] [Google Scholar]
- 4. Myers SM, Johnson CP. Management of children with autism spectrum disorders. Pediatrics. 2007;120:1162-1182. [DOI] [PubMed] [Google Scholar]
- 5. Robins DL. Screening for autism spectrum disorders in primary care settings. Autism. 2008;12:537-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pinto-Martin JA, Young LM, Mandell DS, Poghosyan L, Giarelli E, Levy SE. Screening strategies for autism spectrum disorders in pediatric primary care. J Dev Behav Pediatr. 2008;29:345-350. [DOI] [PubMed] [Google Scholar]
- 7. Dosreis S, Weiner CL, Johnson L, Newschaffer CJ. Autism spectrum disorder screening and management practices among general pediatric providers. J Dev Behav Pediatr. 2006;27(2 suppl):S88-S94. [DOI] [PubMed] [Google Scholar]
- 8. Golnik A, Ireland M, Borowsky IW. Medical homes for children with autism: a physician survey. Pediatrics. 2009;123:966-971. [DOI] [PubMed] [Google Scholar]
- 9. Major NE, Peacock G, Ruben W, Thomas J, Weitzman CC. Autism training in pediatric residency: evaluation of a case-based curriculum. J Autism Dev Disord. 2013;43:1171-1177. [DOI] [PubMed] [Google Scholar]
- 10. Swanson AR, Warren ZE, Stone WL, Vehorn AC, Dohrmann E, Humberd Q. The diagnosis of autism in community pediatric settings: does advanced training facilitate practice. Autism. 2014;18:555-561. [DOI] [PubMed] [Google Scholar]
- 11. Warren Z, Stone W, Humberd Q. A training model for the diagnosis of autism in community pediatric practice. J Dev Behav Pediatr. 2009;30:442-446. [DOI] [PubMed] [Google Scholar]
- 12. Miller JS, Gabrielsen T, Villalobos M, et al. The each child study: Systematic screening for autism spectrum disorders in a pediatric setting. Pediatrics. 2011;127:866-871. [DOI] [PubMed] [Google Scholar]
- 13. Honigfeld L, Chandhok L, Spiegelman K. Engaging pediatricians in developmental screening: the effectiveness of academic detailing. J Autism Dev Disord. 2012;42:1175-1182. [DOI] [PubMed] [Google Scholar]
- 14. Zuckerman KE, Mattox K, Donelan K, Batbayar O, Baghaee A, Bethel C. Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics. 2013;132:445-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cull WL, O’Connor KG, Sharp S, Tang SS. Response rates and response bias for 50 surveys of pediatricians. Health Serv Res. 2005;40:213-226. [DOI] [PMC free article] [PubMed] [Google Scholar]