Supplemental Digital Content is available in the text.
Summary:
Traditional microsurgery can lead surgeons to use postures that cause musculoskeletal fatigue, leaving them more prone to work-related injuries. A new technology from TrueVision transmits the microscopic image onto a 3-dimensional (3D) monitor, allowing surgeons to operate while sitting/standing in a heads-up position. The purpose of this study was to evaluate the feasibility of performing heads-up 3D microscopy as a more ergonomic alternative to traditional microsurgery. A feasibility study was conducted comparing heads-up 3D microscopy and traditional microscopy by performing femoral artery anastomoses on 8 Sprague-Dawley rats. Operative times and patency rates for each technology were compared. The 8 microsurgeons completed a questionnaire comparing image quality, comfort, technical feasibility, and educational value of the 2 technologies. Rat femoral artery anastomoses were successfully carried out by all 8 microsurgeons with each technology. There was no significant difference in anastomosis time between heads-up 3D and traditional microscopy (average times, 34.5 and 33.8 minutes, respectively; P = 0.66). Heads-up 3D microscopy was rated superior in neck and back comfort by 75% of participants. Image resolution, field of view, and technical feasibility were found to be superior or equivalent in 75% of participants, whereas 63% evaluated depth perception to be superior or equivalent. Heads-up 3D microscopy is a new technology that improves comfort for the microsurgeon without compromising image quality or technical feasibility. Its use has become prevalent in the field of ophthalmology and may also have utility in plastic and reconstructive surgery.
Over the past 2 decades, new innovations have led to a dramatic increase in the prevalence of microsurgery. Despite these advancements, traditional binocular microsurgery can lead surgeons to use neck and back postures that cause musculoskeletal fatigue and injuries.1–3 As a result, chronic poor posture and musculoskeletal strain can lead to increased rates of disability and reduced surgical longevity.2–4
In 2010, TrueVision Systems (Santa Barbara, Calif.) developed a new 3-dimensional (3D) technology that allows the microsurgeon to sit or stand in a more physiologic “heads-up” posture while operating. We have described this as “heads-up 3D microscopy.” This system transmits the surgical microscopic image to a high-definition 3D monitor for the surgeon and students to view in a more comfortable position. Despite its increased use in the field of ophthalmology with cataract and corneal surgery, heads-up 3D microscopy has not been utilized for microvascular surgical procedures in plastic and reconstructive surgery. The purpose of this study was to evaluate the feasibility of using heads-up 3D microscopy to perform rat femoral artery anastomoses and compare this technology with traditional microscopy. We hypothesize that this new technology is a more ergonomic and educational alternative to traditional microscopy and may have useful applications in the field of plastic and reconstructive surgery.
MATERIALS AND METHODS
After obtaining approval from the Institutional Animal Care and Use Committee, a feasibility study was conducted comparing TrueVision 3D microscopy and traditional microscopy by performing rat femoral artery anastomoses. The setup for the TrueVision fifth-generation digital visualization system (cost of $64,000) involves attachment of an image capture module to the oculars of a standard surgical microscope (Fig. 1). The image capture module processes the microsurgical optical image into a digital 3D image displayed onto a mobile, flat-screen 46-inch 1080p monitor, which can be viewed with polarized 3D goggles (Fig. 2).
Fig. 1.
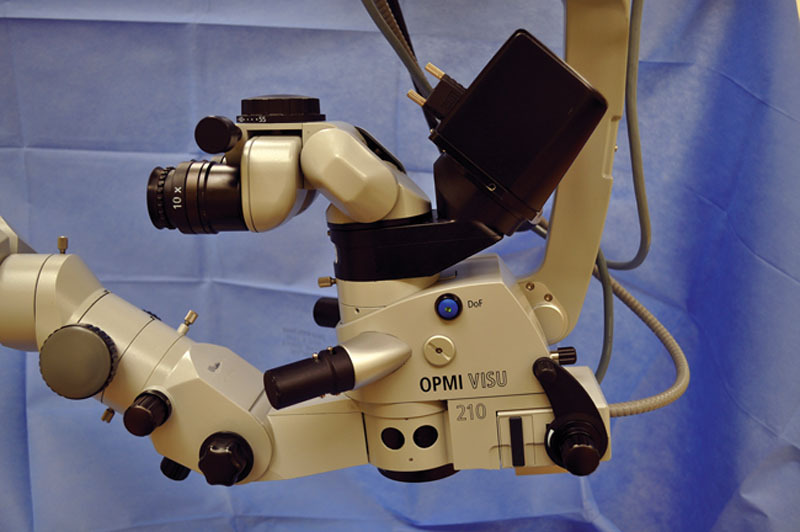
TrueVision image capture module (black box-shaped apparatus) attached to oculars of standard surgical microscope.
Fig. 2.
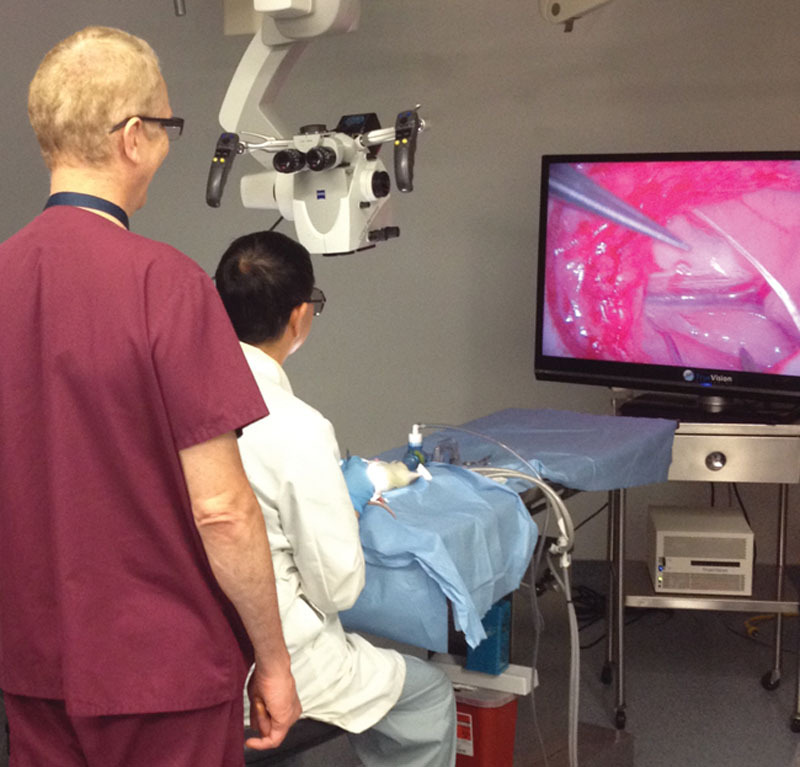
Microsurgeon using heads-up 3-dimensional (3D) microscopy in a seated position with 3D goggles.
By using both the heads-up 3D microscopy system and traditional microscopy, 8 microsurgeons (each described in first column of Table 1) performed anastomoses on 8 Sprague-Dawley rat femoral arteries with a Zeiss OPMI Pentero microscope (Zeiss Microscopy, Jena, Germany) using 10-0 nylon suture. The microsurgical technique used for the rat femoral artery anastomosis has been previously described by Tosun et al.5 All microvascular anastomoses were performed under ×13 magnification. The skin-to-skin operative times, patency rates, and questionnaire responses with both technologies were measured and statistically compared using the Student’s t test. Once the anastomoses were complete, each microsurgeon completed a questionnaire comparing on a 1 to 10 scale (1 = vastly inferior to traditional microscopy, 5 = equivalent, and 10 = vastly superior) the image quality, comfort, technical difficulty, and educational value of heads-up 3D microscopy to traditional binocular microsurgery.
Table 1.
Results of Questionnaire Completed by 8 Microsurgeons Rating Heads-up 3D Microscopy on a 1 to 10 Scale Relative to Traditional Binocular Microscopy (1 = Vastly Inferior to Traditional Microscopy, 5 = Equivalent, 10 = Vastly Superior)

RESULTS
Bilateral femoral artery anastomoses were successfully carried out by all 8 microsurgeons using heads-up 3D microscopy and traditional microscopy. On completion, both groups of anastomoses had a 100% patency rate as measured by clinical examination and Doppler ultrasound. The average rat weight was 350 g, and the femoral artery diameters ranged from 0.6 to 0.8 mm. The ages of the microsurgeons ranged from 30 to 61 years, with an average age of 43 years. There was no significant difference in operative times between the 2 technologies (P = 0.660), with an average operative time for heads-up 3D microscopy of 34.5 minutes (range, 31–38 minutes) and 33.8 minutes (range, 29–39 minutes) for traditional microscopy. Questionnaire responses (Table 1) demonstrated that 6 of the 8 participants (75%) rated neck and back comfort to be superior with heads-up 3D microscopy compared with traditional microsurgery (both with average rating of 6.9 of 10), whereas the remaining 2 participants rated comfort to be equivalent (P = 0.048). A more advanced age did not correlate with reduced comfort levels. With regard to image resolution, field of view, and technical feasibility, 75% of participants found heads-up microscopy to be equivalent or superior to traditional microsurgery (P = 0.048), with an average rating of 5.0 of 10 for all 3 variables. In 63% of participants, depth perception was found to be equivalent or superior with heads-up 3D microscopy (P = 0.480), with an average rating of 4.5 of 10. In addition, 100% of participants found heads-up 3D microscopy to be a more valuable educational and interactive experience (average rating, 10 of 10).
DISCUSSION
Neck and back postures used in traditional binocular microsurgery can expose surgeons to higher biomechanical joint loads and an increased risk of work-related injuries.1–3 In 2010, Capone et al4 reported >75% of plastic surgeons having work-related neck and back symptoms, with a 3-fold higher likelihood in surgeons performing >3 hours per week of microsurgery. In the same study, symptomatic surgeons were 5 times more likely to develop impairment or disability during their career.
Heads-up 3D microscopy eliminates the constraints imposed by using the binocular surgical microscope and minimizes fatigue by providing microsurgeons with greater degrees of freedom to operate in a more neutral and physiologic position.6 Our data demonstrate that a large majority of participants (75%) rated neck and back comfort to be superior with heads-up 3D microscopy. This superior comfort did not seem to compromise image quality or technical difficulty as a majority of participants found heads-up 3D microsurgery to be equivalent or superior in these categories. Similar findings have been demonstrated by Liu et al.7 In their study comparing a different type of 3D microsurgical video system with conventional microscopy, there was no significant difference in anastomosis time or patency rates.
One limitation of the study was the relatively short operative time. Given that our average operative time was 34 minutes, this may not have been sufficient time to cause significant neck and back discomfort. Another limitation of the study was the bulkiness of the surgical microscope used. Participants who rated heads-up 3D microscopy more technically difficult commented that the bulky microscopic hand controls prevented full visualization of the 3D viewing monitor. The use of smaller voice or foot-pedal controlled microscopes, similar to those currently used with heads-up 3D microscopy in ophthalmologic surgery (Leica M844, Leica M822, and Leica Microsystems, Buffalo Grove, Ill.), would help to optimize visualization of the 3D viewing monitor for both the operating surgeon and the surgical assistant (standing facing each other similar to laparoscopic surgery). One last limitation was the sample size of microsurgeons. More participants would have increased the power of the study; however, we were limited by the number of microsurgeons available at our institution.
SUMMARY
Heads-up 3D microscopy can improve posture and comfort and potentially reduce work-related injuries for the plastic surgeon performing microsurgery without affecting the image quality or technical difficulty. This technology offers not only a more ergonomic working environment but also a better educational experience for both the teacher and the student. Further improvement of the 3D microsurgical system should focus on the use with smaller microscopes controlled by voice or foot pedals. With improved visualization, heads-up 3D microscopy could be used in the field of plastic and reconstructive surgery for neurorrhaphy and microvascular anastomoses.
Footnotes
Presented orally at the annual meeting of the American Society of Plastic Surgeons, October 10–14, 2014, Chicago, Ill.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Research and Graduate Program at Loyola University Medical Center, Stritch School of Medicine funded the animal laboratory equipment and rats used in this study. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Yu D, Sackllah M, Woolley C, et al. Quantitative posture analysis of 2D, 3D, and optical microscope visualization methods for microsurgery tasks. Work. 2012;41(Suppl 1):1944–1947. doi: 10.3233/WOR-2012-0412-1944. [DOI] [PubMed] [Google Scholar]
- 2.RB Wallace., III The 45 degree tilt: improvement in surgical ergonomics. J Cataract Refract Surg. 1999;25:174–176. doi: 10.1016/s0886-3350(99)80122-9. [DOI] [PubMed] [Google Scholar]
- 3.Bhadri PR, Rowley AP, Khurana RN, et al. Evaluation of a stereoscopic camera-based three-dimensional viewing workstation for ophthalmic surgery. Am J Ophthalmol. 2007;143:891–892. doi: 10.1016/j.ajo.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 4.Capone AC, Parikh PM, Gatti ME, et al. Occupational injury in plastic surgeons. Plast Reconstr Surg. 2010;125:1555–1561. doi: 10.1097/PRS.0b013e3181d62a94. [DOI] [PubMed] [Google Scholar]
- 5.Tosun Z, Karabekmez FE, Duymaz A, et al. Preventing negative effects of smoking on microarterial anastomosis. Ann Plast Surg. 2010;65:91–95. doi: 10.1097/SAP.0b013e3181b404fa. [DOI] [PubMed] [Google Scholar]
- 6.Kantor E, Berci G, Partlow E, et al. A completely new approach to microlaryngeal surgery. Laryngoscope. 1991;101(6 Pt 1):676–679. doi: 10.1288/00005537-199106000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Chen B, Ni Y, et al. Application of a three-dimensional microsurgical video system for a rat femoral vessel anastomosis. Chin Med J (Engl) 2014;127:348–352. [PubMed] [Google Scholar]


