Supplemental Digital Content is available in the text.
Summary:
There is renewed interest in sparing the pectoralis major muscle in implant breast reconstruction, placing the implant in the subcutaneous position. This advance is made reliable by improvements in mastectomy skin flap quality, evolution of technique, and increased awareness of breast animation deformity. This retrospective review presents 13 patients (23 breasts) reconstructed immediately with placing the definitive implant in the subcutaneous space without disruption of the underlying chest muscles. None of the 13 patients had breast animation deformity postoperatively. One patient experienced an early hematoma, and 3 patients had small seromas that resolved uneventfully. One morbidly obese patient undergoing chemotherapy using a nearby chest port experienced infection requiring implant removal. This study describes an early experience, demonstrates feasibility, and discusses patient selection considerations that are important because we continue to evolve breast reconstruction approaches.
Paradigm shifts in breast reconstruction have occurred in recent years.1–3 Immediate direct-to-implant (DTI) breast reconstruction has become a routine practice at many institutions.4,5 This approach generally involves partial detachment of the pectoralis major muscle with implant placement in the subpectoral position. The inferolateral pole of the implant is often supported with acellular dermal matrix (ADM) or synthetic mesh.
Although subpectoral DTI breast reconstruction can achieve safe and cosmetically favorable results, there are important drawbacks. Placement of the breast implant underneath the pectoralis major muscle may result in breast animation deformity (BAD) and increased operative time and morbidity.
Functionally and cosmetically, BAD constitutes an unsettling problem for patients after subpectoral DTI reconstruction. In BAD, contraction of the pectoralis muscle dramatically displaces the breast implant laterally and inferiorly, often observable under clothing. BAD is particularly problematic for very active patients. Several methods have been used to correct BAD, including selective nerve transection, botulinum toxin injection, muscle splitting techniques, and more recently staged repositioning of the implant to a subcutaneous position with attempted reinsertion of the pectoralis muscle.6 Each of these approaches requires additional procedures, concomitant morbidity, expense, and inconvenience to the patient. We hypothesize that immediate DTI with subcutaneous implant placement is a viable and safe option in patients to avoid BAD.
PATIENTS AND MATERIALS
A retrospective, institutional review board-approved review was conducted of all patients undergoing breast reconstruction over the past 18 months. Thirteen patients were identified to have undergone subcutaneous DTI reconstruction, all performed by the senior author. Many of these patients approached the senior author preoperatively with concerns about pectoralis dysfunction and to discuss the possibility of pectoralis-sparing approaches. Demographic characteristics are presented in Table 1. No patients were diabetics or smoked within 6 weeks before mastectomy and reconstruction. Patients had a bimodal body mass index distribution (Table 1). Five patients had skin-sparing mastectomies, whereas the remaining 8 had nipple-sparing mastectomies. The reconstructive technique of subcutaneous implant placement is demonstrated in Figure 1. In all cases, the implant was placed in a pocket constructed from woven absorbable mesh. In 3 cases, ADM was used to augment the mesh pocket anteriorly in patients considered high risk for implant rippling and for patients likely to undergo fat grafting in the future. Patients considered at highest risk for implant rippling were thin patients with limited preoperative soft-tissue envelopes, thin mastectomy flaps, and small-volume implant reconstructions.
Table 1.
Patient Demographics
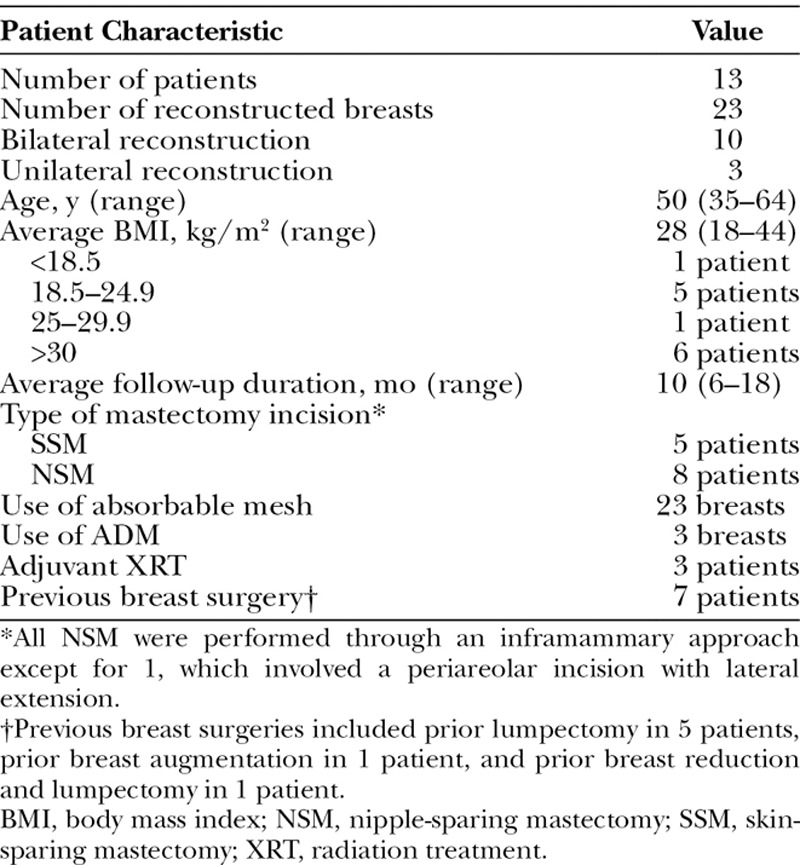
Fig. 1.
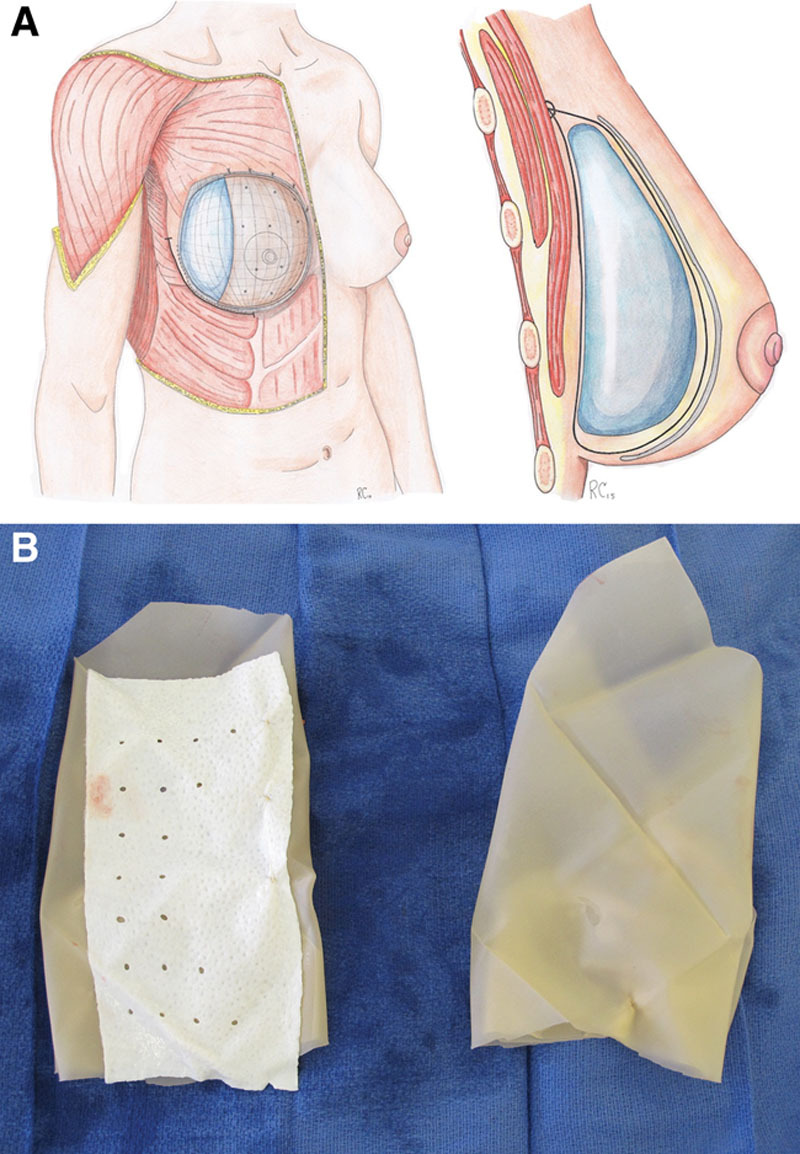
Pectoralis-sparing subcutaneous direct-to-implant immediate breast reconstruction. A, Diagram demonstrating subcutaneous implant placement. A sheet of 20 x 20 cm woven Vicryl mesh was utilized for each case and folded into a pocket configuration. The Vicryl pocket was sutured to the superior-medial aspect on the anterior surface of the pectoralis-major muscle using 2-0 Vicryl. With the pocket opening pointing toward the superomedial aspect, a silicone implant is placed into the pocket. B, Vicryl pocket with and without acellular dermal matrix overlay.
RESULTS
Patient outcomes are presented in Table 2. Representative aesthetic outcomes are presented for a thin patient (Fig 2). There was 1 early hematoma requiring operative intervention. One morbidly obese patient undergoing chemotherapy using a nearby chest port ultimately experienced infection requiring implant removal. Three patients developed small seromas that resolved uneventfully. One patient demonstrated implant rippling postoperatively but did not seek revision. No instances of implant malposition developed. There were no instances of implant extrusion or skin flap necrosis requiring operative intervention. Videos demonstrating BAD in a typical patient after standard subpectoral DTI are compared with that in a patient after subcutaneous pectoralis-sparing DTI, who did not exhibit BAD despite forceful pectoralis contraction. (See Supplemental Digital Content 1, which displays a typical patient after standard immediate breast reconstruction with direct to implant placement below the pectoralis major muscle, using inferolateral acellular dermal matrix, http://links.lww.com/PRSGO/A193. See Supplemental Digital Content 2, which displays a thin patient after immediate breast reconstruction with pectoralis-sparing subcutaneous direct to implant placement, http://links.lww.com/PRSGO/A194.)
Table 2.
Patient Outcomes
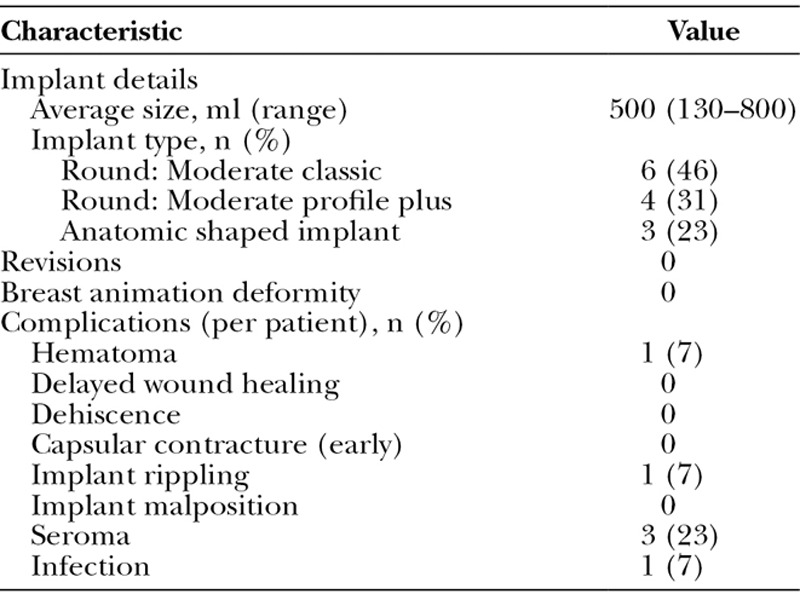
Fig. 2.
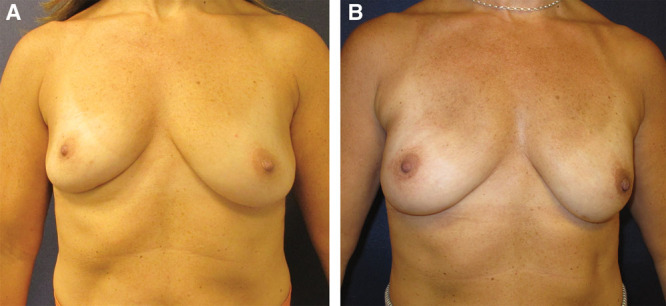
A, Preoperative frontal view of patient with distant history of lumpectomy and radiation on the right breast, with asymmetry. B, Postoperative frontal view of the same patient after pectoralis-sparing implant breast reconstruction. Video documenting absence of breast animation deformity is available online.
DISCUSSION
BAD has renewed interest in subcutaneous (also referred to as pectoralis-sparing or prepectoral) placement of implants for breast reconstruction.6–8 Historically, this technique had been supplanted by subpectoral implant reconstruction given concerns related to capsular contracture, implant rippling, malposition, and lack of soft-tissue coverage. However, considerable advances in mastectomy flap viability coevolving with nipple-sparing dissection techniques have created a new context for reintroduction of this method. Moreover, improved experience with ADM and synthetic meshes enable the secure placement of implants above the muscle. In this study, we demonstrate the feasibility of immediate DTI subcutaneous implant reconstruction using an absorbable mesh pocket, with or without ADM augmentation.
Although our patient sample and follow-up interval are limited, the complication profile was acceptable, and aesthetic results were promising. In addition to the anatomic benefits of this method, we generally observed highly satisfied patients who report less pain, shorter recovery times, and more rapid return to baseline physical activity.
Recent reports detailing subcutaneous implant reconstruction have incorporated an ADM pocket to envelope the implant.7–9 These approaches require more ADM per implant than standard approaches, which may be cost prohibitive. In addition, the potential benefit of ADM in reducing capsular contracture in the setting of subcutaneous implant reconstruction has not been demonstrated. In all of our patients, we instead utilized an absorbable mesh pocket (Vicryl, Ethicon, Inc., Somerville, N.J.), which has been shown to be a cost-effective alternative to ADM in implant breast reconstruction.10 Augmenting a mesh pocket with ADM may be indicated to increase the bulk of soft-tissue cover in cases where rippling is a concern. If medial rippling of the implant becomes visible, the ADM creates a tissue plane into which fat grafting can be carried out safely without entering the implant pocket.
Our technique arose from the desire to avoid the morbidity of pectoralis detachment in thin, highly active patients while simultaneously avoiding animation deformity. We subsequently applied this approach in select obese patients in whom a faster, less morbid reconstruction procedure would be desirable. In many obese patients, we have found the size and distribution of the pectoralis major muscle to be small relative to the required implant size, shifting our preference toward muscle preservation.
We strongly recommend collaborating with an extirpative surgeon and limiting the early experience to patients with robust skin flaps. Once comfortable with this procedure, one can then apply it to athletic patients who desire to minimize BAD. This approach should be avoided in patients who are identified preoperatively to have a chest port for chemotherapy, and if chemotherapy is determined to be necessary after reconstruction, should receive an arm port instead. Larger studies with longer follow-up times are required to better analyze long-term safety endpoints and aesthetic outcomes.
Video Graphic 1.

See video, Supplemental Digital Content 2, which displays a typical patient after standard immediate breast reconstruction with direct-to-implant placement below the pectoralis major muscle, using inferolateral acellular dermal matrix. The patient has an acceptable result without animation. However, because the patient moves her arms to activate pectoralis, the breast shape becomes significantly deformed, with lateral movement of the breast implant and medial flattening and contractures. http://links.lww.com/PRSGO/A193.
Video Graphic 2.

See video, Supplemental Digital Content 3, which displays a thin patient after immediate breast reconstruction with pectoralis-sparing subcutaneous direct-to-implant placement. Here, the implant is positioned above the muscle using a Vicryl pocket with acellular dermal matrix placed along the anterior surface of the mesh, and the implant is placed inside the Vicryl pocket. With forceful activation of the pectoralis muscle, no animation deformity is observed. http://links.lww.com/PRSGO/A194.
Supplementary Material
Footnotes
Disclosure: Dr. Liao has consultant agreements with, but explicitly is not a speaker for, Musculoskeletal Transplant Foundation and LifeCell Inc. Vicryl mesh and FlexHD Pliable acellular dermal matrix materials were used in these cases. The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Ballard TN, Kim Y, Cohen WA, et al. Sociodemographic and clinical variables impacting procedure choice in breast reconstruction. Plast Reconstr Surg. 2015;136(4 Suppl):85–86. doi: 10.1097/01.prs.0000472385.42737.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzpatrick AM, Gao LL, Smith BL, et al. Cost and outcome analysis of breast reconstruction paradigm shift. Ann Plast Surg. 2014;73:141–149. doi: 10.1097/SAP.0b013e318276d979. [DOI] [PubMed] [Google Scholar]
- 3.Gfrerer L, Mattos D, Mastroianni M, et al. Assessment of patient factors, surgeons, and surgeon teams in immediate implant-based breast reconstruction outcomes. Plast Reconstr Surg. 2015;135:245e–252e. doi: 10.1097/PRS.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 4.Gdalevitch P, Ho A, Genoway K, et al. Direct-to-implant single-stage immediate breast reconstruction with acellular dermal matrix: predictors of failure. Plast Reconstr Surg. 2014;133:738e–747e. doi: 10.1097/PRS.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 5.Colwell AS, Damjanovic B, Zahedi B, et al. Retrospective review of 331 consecutive immediate single-stage implant reconstructions with acellular dermal matrix: indications, complications, trends, and costs. Plast Reconstr Surg. 2011;128:1170–1178. doi: 10.1097/PRS.0b013e318230c2f6. [DOI] [PubMed] [Google Scholar]
- 6.Hammond DC, Schmitt WP, O’Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg. 2015;135:1540–1544. doi: 10.1097/PRS.0000000000001277. [DOI] [PubMed] [Google Scholar]
- 7.Reitsamer R, Peintinger F. Prepectoral implant placement and complete coverage with porcine acellular dermal matrix: a new technique for direct-to-implant breast reconstruction after nipple-sparing mastectomy. J Plast Reconstr Aesthet Surg. 2015;68:162–167. doi: 10.1016/j.bjps.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Woo A, Harless C, Jacobson SR. Revisiting an old place: single surgeon experience on post-mastectomy subcutaneous implant based breast reconstruction. Plast Reconstr Surg. 2015;136(4 Suppl):83. doi: 10.1111/tbj.12790. [DOI] [PubMed] [Google Scholar]
- 9.Becker H, Lind JG, II, Hopkins EG. Immediate implant-based prepectoral breast reconstruction using a vertical incision. Plast Reconstr Surg Glob Open. 2015;3:e412. doi: 10.1097/GOX.0000000000000384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tessler O, Reish RG, Maman DY, et al. Beyond biologics: absorbable mesh as a low-cost, low-complication sling for implant-based breast reconstruction. Plast Reconstr Surg. 2014;133:90e–9e. doi: 10.1097/01.prs.0000437253.55457.63. [DOI] [PubMed] [Google Scholar]


