Abstract
Objective:
The present study is designed to evaluate the role of pleural fluid analysis in diagnosing pleural diseases and to study the advantages and disadvantages of thoracocentasis and pleural biopsy.
Materials and Methods:
We prospectively included 66 consecutive indoor patients over a duration of 1 year. Pleural fluid was collected and cytological smears were made from the fluid. Plural biopsy was done in the same patient by Cope needle. Adequate pleural biopsy tissue yielding specific diagnosis was obtained in 47 (71.2%) cases.
Results:
Tuberculosis was the commonest nonneoplastic lesion followed by chronic nonspecific pleuritis comprising 60% and 33.3% of the nonneoplastic cases respectively and tuberculosis was predominantly diagnosed in the younger age group. Majority (70.8%) of malignancy cases were in the age group of >50-70. Adenocarcinoma was found to be the commonest (66.7%) malignant neoplasm in the pleurae followed by small-cell carcinoma (20.8%).
Conclusion:
Pleural biopsy is a useful and minimally invasive procedure. It is more sensitive and specific than pleural fluid smears.
Keywords: Adenocarcinoma, pleural biopsy, pleural fluid, tuberculosis
Introduction
The pleural space is a potential space between the visceral and parietal layers of the pleurae that normally contains 0.1-0.2 mL/kg body weight of fluid.[1] Pleural effusion is an abnormal accumulation of fluid in the pleural cavity and remains the most common manifestation of pleural pathology.[2] Although, a variety of clinical conditions such as heart failure, malignancy, pneumonia, tuberculosis may be the cause of a pleural effusion, the possibility of a malignant involvement of pleural cavity should always be considered in difficult-to-diagnose cases. Because percutaneous access of the pleural space is relatively simple, techniques such as pleural biopsy and thoracoscopy have become very popular. However, such facilities are available only in advanced pulmonary medicine centers, pleural fluid analysis and cytology remain the mainstay for diagnosing the various pulmonary diseases.[3]
Analysis of pleural fluid can have an important contribution for investigation of patients with pleural effusion.[4] Cytological examination not only helps for diagnosing cancer but also for staging and prognosis of diseases.[5] Levels of adenosine deaminase (ADA) are particularly useful in areas where the prevalence of tuberculosis is high.[6] Closed pleural biopsy provides the highest diagnostic yield in cases of pleural tuberculosis and malignancy, the two most important causes of exudative pleural effusion.[7]
The aim of this study was to obtain pleural fluid sample by thoracocentesis and to compare with pleural biopsy to determine the etiology by various histopathological, cytological, and biochemical tests and to analyze the results.
Materials and Methods
We prospectively included 66 consecutive indoor patients over a duration of 1 year. Pleural fluid was categorized as exudative or transudative according to Light's criteria.[8] Patients with transudative pleural effusion, pyothorax, and chylothorax were excluded. Pleural fluid was collected, ADA level of the fluid was measured, and cytological smears were made from the fluid. Plural biopsy was done in the same patient by Cope needle.[9] Adequate pleural biopsy tissue yielding specific diagnosis was obtained in 47 (71.2%) cases. The cytological smears were stained with Giemsa stain and PAP stain. Pleural biopsy was stained with hematoxylin and eosin staining.
Observation and Result
Age range of the patients was 18-84 years with a mean age of 51 years and 66.6% were males. The most common presenting symptom was shortness of breath (95.4%), followed by chest pain (89.4%) and productive cough (69.7%) and 48.5% patients had a history of smoking. Majority of the pleural fluid (69.7%) were hemorrhagic and the rest (30.3%) were straw colored.
Out of 36 cases of malignancy, 34 cases (94.4%) had ADA value <40 IU/L. Only two cases (5.6%) had ADA value >40 IU/L. Out of nine cases of tuberculosis, seven cases (77.8%) showed ADA value >40 IU/L, and two cases (22.2%) showed ADA value <40 IU/L. All the six cases of chronic nonspecific pleuritis (diagnosed on biopsy) showed ADA value <40 IU/L.
Tuberculosis was the commonest nonneoplastic lesion [Figure 1d, Figure 2c and d] followed by chronic nonspecific pleuritis comprising 60% and 33.3% of the nonneoplastic cases respectively. Tuberculosis was the commonest nonneoplastic disease in the younger age group (11-30 years) comprising 55.5% of all cases of tuberculosis.
Figure 1.
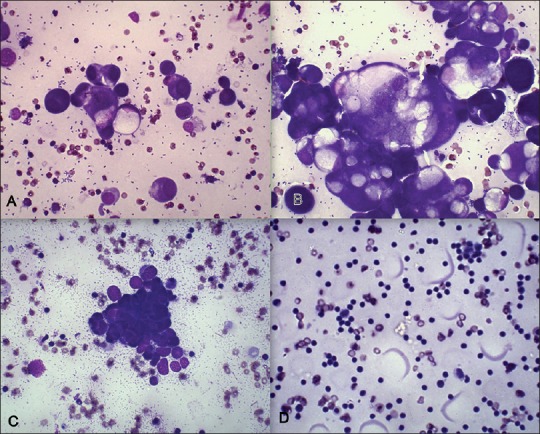
(a) Adenocarcinoma, pleural fluid, (Giemsa, × 100) (b) Adenocarcinoma, pleural fluid, (Giemsa, 400×) (c) Small cell carcinoma, pleural fluid, (Giemsa, 400×) (d) Smear shows predominantly Lymphocytes and absence of Mesothelial cells; Suspicious for Tuberculosis, (Giemsa, 100×)
Figure 2.
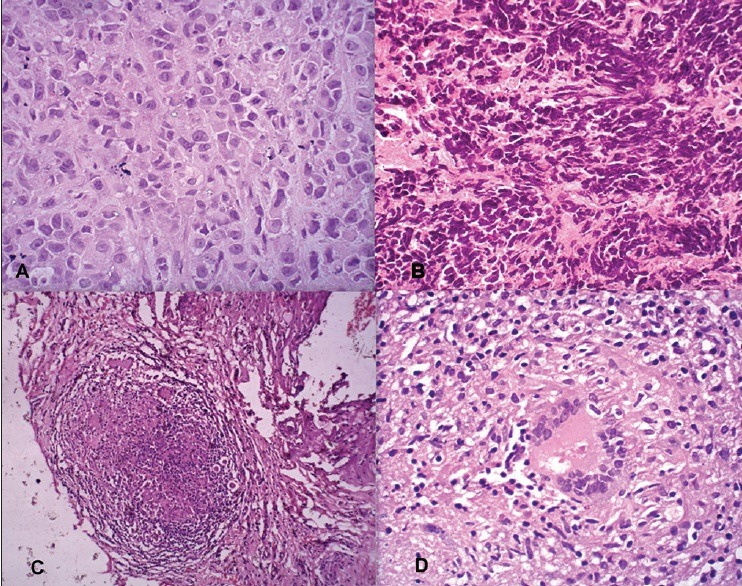
(a) Adenocarcinoma, pleural biopsy (H and E, 400×) (b) Small cell carcinoma, pleural biopsy (H and E, 400×) (c) Epithelioid granuloma and langhans giant cell, pleural biopsy (H and E, 100×) (d) Epithelioid Granuloma and Langhans Giant cell, pleural biopsy (H and E, 400×)
Majority (70.8%) of malignancy were in the age group of >50-70. Adenocarcinoma [Figures 1a,b and 2a] was found to be the commonest (66.7%) malignant neoplasm in the pleurae followed by small-cell carcinoma [Figure 1c and 2b] (20.8%) and additionally these were more commonly encountered in male patients.
Discussion
Thoracocentesis has been a very popular diagnostic as well as therapeutic procedure for tapping pleural effusions and with very few procedural complications.[3] It is usually done through the 2nd intercostal space below the fluid level.[10] Medical thoracoscopy by a pulmonologist is a safe and effective procedure for the diagnosis and therapy of various pleural diseases, but it is more invasive and expensive procedure, with a risk of complications such as pneumothorax. Very few pulmonologists are trained in thoracoscopy and it is available only at selected centers, and furthermore, its cost is very high for an economically average person in a developing country such as India.[3] A recent survey has additionally revealed that even in the USA, only 6% of pulmonologists are currently trained in and perform thoracoscopy.[11] Hence, thoracocentesis still remains a popular diagnostic procedure in cases of pleural effusion.
It is chiefly the protein and LDH levels that decide the nature of pleural fluid as exudate or transudate. According to Light's criteria, a pleural fluid is exudative in nature if its protein content is >3.5 gm/dL or LDH is ≥150 IU/L.[8]
ADA is an enzyme involved in purine metabolism. It is needed for the breakdown of nucleic acids in tissues. ADA value above 40 IU/L are known to well correlate with tubercular pathology in various studies and help to differentiate between tubercular and nontubercular exudative pleural effusion.[2,5,12] In majority of studies, ADA levels in tubercular effusions were found to be more than 40 IU/L in majority of cases.[2,5,12,13,14] In the present study as well in majority (77.8%) of fluids having ADA levels >40 IU/L were found to be tubercular on biopsy or culture. or both. However. in 22.2% of biopsy-proven tuberculosis, ADA levels were below 40 IU/L. Pandit et al. (2010) inferred that pleural fluid ADA levels 70 IU/L or more are almost diagnostic of tuberculosis and recommended that in these cases, pleural biopsy may not be mandatory.[2] In the present study as well, all patients with high ADA level (≥81 IU/L) were diagnosed as tuberculosis.
Similarly, in malignant pleural effusion as well the ADA levels in different studies have been reported as usually less than 40 IU/L. In the present study as well in 94.4% of malignant pleural effusions, ADA levels were below 40 IU/L.[2,5,12,13,14] However, two patients (5.6%) had ADA levels 46.2 IU/L and 46.7 IU/L respectively who were diagnosed to have malignancy on pleural biopsy subsequently.
Different complications have been noted in patients after pleural biopsy procedure, some of them being pain at the site of biopsy, pneumothorax, and hemothorax.[15,16,17]
In their study Bhattacharya et al. (2012) observed that cytological analysis of three consecutive samples of patients of pleural effusion increased the diagnosis rate of malignancy.[18] However, in the present study, only one sample of pleural fluid was obtained and compared with pleural biopsy.
In pleura, secondary tumors are more common than the primary tumors. The primary tumor may be pulmonary or extrapulmonary. The common pulmonary tumors infiltrating into the pleurae are squamous cell carcinoma, small cell carcinoma, and adenocarcinomas and extrapulmonary neoplasms metastasizing into pleura are usually from breast, ovary, gastrointestinal tract (GIT), stomach, and the pancreas.[19] Adenocarcinoma is the most common malignancy encountered in pleural biopsy.[3,18,20] The second commonest being small-cell carcinoma.[3,18] However, Khan et al. (2010) in their study of 26 malignancies found mesothelioma as the second most common malignancy. In the present study as well, the most common malignancy metastasizing to pleura was adenocarcinoma (43.7%) followed by small-cell carcinoma (15.6%) and squamous-cell carcinoma (9.4%), which was quite similar to previous studies.[3,18]
Combining pleural fluid analysis with pleural needle biopsy can help in the diagnosis and morphological classification of majority of malignant pleural lesions, leaving around 7-12% undiagnosed cases.[21] Thoracoscopy is the ideal procedure available to directly explore the pleural cavity and visualize the malignancies in early stages, which are confined up to visceral pleura of the lung. However, even after thoracoscopy, around 10% of effusions remain undiagnosed.[22,23]
Conclusion
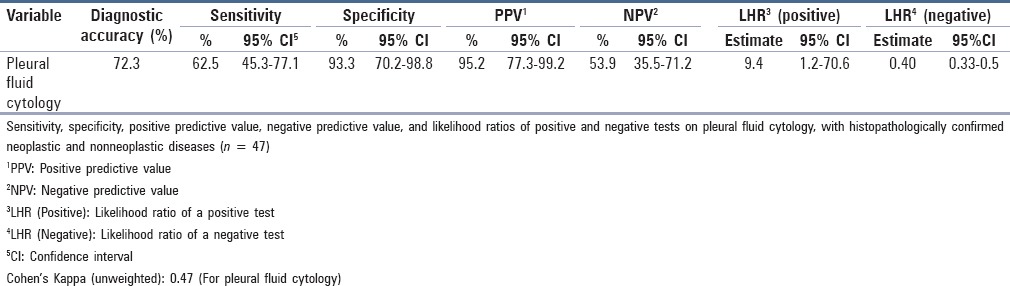
Pleural biopsy is a useful and minimally-invasive procedure. It is more sensitive and specific than pleural fluid smears. High ADA value in pleural fluid helps to distinguish tubercular pleural effusions from malignant ones. In a developing country such as India, where investigations and health facilities are inadequate and cost of treatment is often high, pleural fluid analysis for ADA and cytology should continue to be the first line of investigation in patients presenting with pleural effusion. It is not only cost-effective but a reasonably safe procedure that shows reasonably good sensitivity and specificity in diagnosing primary as well as metastatic pleural malignancies [Table 1, Table 2].
Table 1.
True positive, true negative, false positive, false negative, sensitivity, specificity, positive predictive value, and negative predictive value of pleural fluid cytology
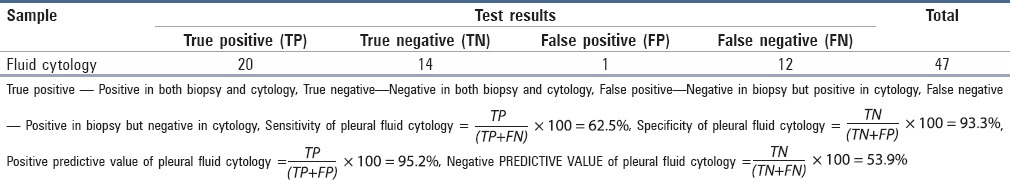
Table 2.
Comparison of sensitivity, specificity, and predictive values of pleural fluid cytology with pleural biopsy findings by Epi Info and open Epi software
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rahman NM, Chapman SJ, Davies RJ. Pleural effusion: A structured approach to care. Br Med Bull. 2004;72:31–47. doi: 10.1093/bmb/ldh040. [DOI] [PubMed] [Google Scholar]
- 2.Pandit S, Chaudhuri AD, Datta SB, Dey A, Bhanja P. Role of pleural biotpsy in etiological diagnosis of pleural effusion. Lung India. 2010;27:202–4. doi: 10.4103/0970-2113.71941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaur DS, Chauhan N, Kusum A, Harsh M, Talekar M, Kishore S, et al. Pleural fluid analysis - Role in diagnosing pleural malignancy. J Cytol. 2007;24:183–8. [Google Scholar]
- 4.Soe Z, Shwe WH, Moe S. A study on tuberculous pleural effusion. Int J Collab Res Intern Med Public Health. 2010;2:32–48. [Google Scholar]
- 5.Maldhure BR, Bedarkar SP, Kulkarnl HR, Paplnwar SP. Pleural biopsy and adenosine deaminase in pleural fluid for the diagnosis of tubercular pleural effusion. Ind J Tub. 1994;41:161–5. [Google Scholar]
- 6.McGrath EE, Anderson PB. Diagnosis of pleural effusion: A systematic approach. Am J Crit Care. 2011;20:119–28. doi: 10.4037/ajcc2011685. [DOI] [PubMed] [Google Scholar]
- 7.Anwar R, Farooqi JI. Diagnostic yield of pleural biopsy in lymphocytic exudative pleural effusion. Rawal Med J. 2004;29:61–4. [Google Scholar]
- 8.Light RW, Macgregor MI, Luchsinger PC, Ball WC., Jr Pleural effusions: The diagnostic separation of transudates and exudates. Ann Intern Med. 1972;77:507–13. doi: 10.7326/0003-4819-77-4-507. [DOI] [PubMed] [Google Scholar]
- 9.Cope C. New pleural biopsy needle; preliminary study. J Am Med Assoc. 1958;167:1107–8. doi: 10.1001/jama.1958.72990260005011a. [DOI] [PubMed] [Google Scholar]
- 10.Ihsanullah, Khan N, Jadoon H, Zaman M, Ahmed A. Yield of Abrams needle pleural biopsy in exudative pleural effusion. J Ayub Med Coll Abbottabad. 2009;21:116–8. [PubMed] [Google Scholar]
- 11.Mathur PN, Loddenkemper R. Biopsy techniques in the diagnosis of pleural diseases. Eur Respir J. 2002;7:120–30. [Google Scholar]
- 12.Porcel JM, Light RW. Diagnostic approach to pleural effusion in adults. Am Fam Physician. 2006;73:1211–20. [PubMed] [Google Scholar]
- 13.Hira HS, Ranjan R. Role of percutaneous closed needle pleural biopsy among patients of undiagnosed exudative pleural effusion. Lung India. 2011;28:101–4. doi: 10.4103/0970-2113.80319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verma SK, Dubey AL, Singh PA, Tewerson SL, Sharma D. Adenosine deaminase (ADA) level in tubercular pleural effusion. Lung India. 2008;25:109–10. doi: 10.4103/0970-2113.44121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gouda AM, Dalati TA, Al-Shareef NS. A comparison between Cope and Abrams needle in the diagnosis of pleural effusion. Ann Thorac Med. 2006;1:12–5. [Google Scholar]
- 16.Shah D, Amanullah, Shah N, Attaullah S, Haq A. Diagnostic yield of pleural biopsy in exudative pleural effusion. J Postgrad Med Inst. 2007;21:278–82. [Google Scholar]
- 17.Khattak MI, Amin S, Shabbier G, Rehman S. Diagnostic value of pleural biopsy in exudative pleural effusion. GJMS. 2011;9:156–8. [Google Scholar]
- 18.Bhattacharya S, Bairagya TD, Das A, Mandal A, Das SK. Closed pleural biopsy is still useful in the evaluation of malignant pleural effusion. J Lab Physicians. 2012;4:35–8. doi: 10.4103/0974-2727.98669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Husain AN. The lung. In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. Robbins and Cotran Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Saunders Elsevier; 2012. p. 732. [Google Scholar]
- 20.Khan Y, Bilal, Zia S. Etiological spectrum of exudative pleural effusion in a tertiary care hospital based on closed pleural biopsy. Ann Pak Inst Med Sci. 2011;7:133–6. [Google Scholar]
- 21.Prakash UB, Reiman HM. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusions: Analysis of 414 cases. Mayo Clin Proc. 1985;60:158–64. doi: 10.1016/s0025-6196(12)60212-2. [DOI] [PubMed] [Google Scholar]
- 22.Mårtensson G, Petterson K, Thiringer G. Differentiation between malignant and non-malignant pleural effusion. Eur J Respir Dis. 1985;67:326–34. [PubMed] [Google Scholar]
- 23.Canto A, Blasco E, Casillas M, Zarza AG, Padilla J, Pastor J, et al. Thoracoscopy in the diagnosis of pleural effusions. Thorax. 1977;32:550–4. doi: 10.1136/thx.32.5.550. [DOI] [PMC free article] [PubMed] [Google Scholar]


