Abstract
Calcinosis cutis is an uncommon condition characterized by the deposition of calcium salts in the subcutaneous tissues of the body. Calcifications can also occur in a variety of other clinical settings and can be subjected to fine-needle aspiration (FNA). Since cutaneous calcific deposits may clinically mimic a tumor, it is feasible to diagnose them by FNA cytology (FNAC). We reported a case of calcinosis cutis by FNA in a 36-year-old male who presented with a solitary subcutaneous nodule in cubital fossa. Smears showed amorphous granular material consistent with calcium and occasional histiocytes. The diagnosis was confirmed when cytosmears were subjected to a special stain such as the von Kossa stain.
Keywords: Calcinosis cutis, cytology, iatrogenic
Introduction
Virchow initially described calcinosis cutis in 1855. Calcinosis cutis is a group of disorders characterized by deposition of calcium salts in the skin. Calcinosis cutis is classified into four major types according to etiology — dystrophic, metastatic, iatrogenic, and idiopathic. A few rare types have been variably classified as dystrophic and idiopathic. These include calcinosis cutis circumscripta, calcinosis cutis universalis, tumoral calcinosis, and transplant-associated calcinosis cutis.[1]
Calcifications occur in a variety of other clinical settings. Metabolic calcification usually results in generalized mineral deposition in visceral organs. It is associated with abnormal calcium and/or phosphate levels. Dystrophic calcification, occurring in either a localized or a generalized pattern, results from an underlying inflammatory process, and it is found in patients with normal serum chemistry levels. Metastatic calcifications are complications found in patients with hyperparathyroidism and end-stage renal disease.[2]
Idiopathic calcification occurs without any underlying tissue damage or metabolic disorder. Skin calcification in iatrogenic calcinosis cutis is a side effect of therapy. Calciphylaxis presents with small vessel calcification mainly affecting the blood vessels of dermis or subcutaneous fat.[1]
Tumoral calcinosis is a hereditary disease of phosphate metabolic dysfunction but it is commonly mistaken for a lesion. The soft-tissue lesions of tumoral calcinosis are typically lobulated and well-demarcated calcifications that are most often distributed along the extensor surfaces of large joints.[3]
Family history, history of trauma or injection, tropical or subtropical residence, number and location of calcium deposits, serum calcium and phosphate level, and autoimmune screening are to be evaluated for the appropriate classification of a case.[4]
This report aimed to raise doctors’ awareness of the presentation, etiopathogenesis, and the course of the relatively rare iatrogenic calcinosis cutis and possible confirmation of diagnosis by fine needle aspiration cytology.
Case Report
A 36-year-old male presented with a subcutaneous nodule of about 2 cm × 2 cm size in cubital fossa, who was administered multiple intravenous injection at the same site in the past during his hospital stay for diarrhea and dehydration, 1.5 years ago. FNA was attempted twice that yielded little amount of whitish granular material. Papanicolaou and hematoxylin and eosin stained smears showed paucicellularity and crystalloid background with occasional multinucleated cells and a few histiocytes. Occasional groups of stromal cells were also seen. Alcohol-fixed smears were subjected to von Kossa silver stain and the presence of calcium deposits in them was confirmed. Based on these cytological findings, the diagnosis of calcinosis cutis was made [Figures 1 and 2].
Figure 1.

Subcutaneous nodule of about 2 cm × 2 cm size in cubital fossa
Figure 2.
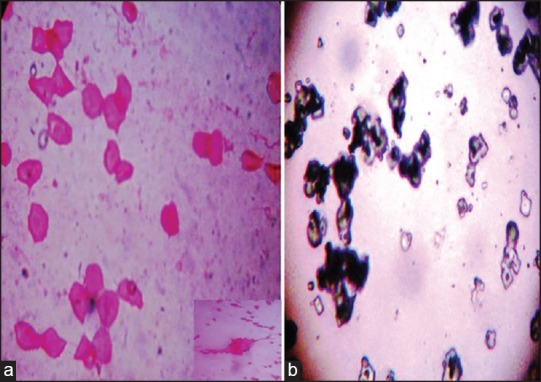
(a) Smear showing calcium crystals and multinucleated giant cell (inset). (H and E stain, ×100) (b) von Kossa silver stain showing black colored calcium crystals (von Kossa stain, ×100)
Discussion
Iatrogenic calcinosis cutis is a cutaneous condition characterized by calcification of skin resulting from the deposition of calcium and phosphorus introduced by a medical procedure, either inadvertently or as a specific therapy.[5]
Various types of calcinosis cutis have been previously described. It is very important to identify the exact type of calcinosis so that an accurate treatment can be started for the effective management of the disease.
In the present case, all the investigations to evaluate abnormal calcium metabolism (serum calcium, serum phosphorus, and serum alkaline phosphatase) revealed results within normal limits. But history of intravenous administration of solutions containing calcium or phosphate was present, hence the diagnosis of iatrogenic calcinosis cutis was considered.
Iatrogenic calcinosis cutis arises secondary to a treatment or procedure. It can also occur as a complication of either intravenous calcium chloride or calcium gluconate therapy, as demonstrated in our patient. Other reported causes of iatrogenic calcinosis cutis include minor trauma in association with prolonged contact with saturated calcium chloride electrode paste in patients undergoing electroencephalographic or electromyographic examination and cutaneous calcification associated with tumor lysis syndrome and repeated heel sticks in newborns.[6,7]
The exact pathogenesis of this condition is unknown; however, it is thought to involve both a transient elevation of the local concentration of calcium after infusion and a tissue damage at the site of the extravasations of calcium solution. The final step of calcification is the formation of crystalline and insoluble calcium phosphate mineral, in the form of hydroxyapatite.
Deshpande et al. diagnosed a case of calcinosis cutis in a 20-year-old male who presented with a solitary subcutaneous nodule near the ankle, as found on the lateral malleolus by FNA.[8]
Shivkumar et al. studied the cytological features of idiopathic scrotal calcinosis and noted the presence of intense, basophilic, amorphous, and granular deposits surrounded by lymphocytes, histiocytes, and foreign body giant cells without any evidence of epithelial cells in the smears.[9]
In the present case, we made the diagnosis of calcinosis cutis on FNA with similar cytological findings that are confirmed by von Kossa silver stain for calcium salts.
Most lesions of calcinosis cutis that develop gradually are asymptomatic. However, the history and evolution of the lesions depend on the etiology of the calcification. The patients with dystrophic calcification may provide a history of an underlying disease, a preexisting dermal nodule (which represents a tumor), or an inciting traumatic event. The patients with metastatic calcification most frequently have a history of chronic renal failure. The cases of idiopathic calcinosis cutis are usually not associated with previous trauma or disease. Those who develop iatrogenic calcinosis cutis generally have a history of recent hospitalization.
Although there is no uniformly effective treatment for calcinosis cutis, several surgical and medical therapies have demonstrated varying degrees of benefit in the treatment of calcinosis, such as surgical excision, laser therapy, extracorporeal shock wave lithotripsy, diltiazem, minocycline, colchicine, and topical sodium thiosulfate, along with others.
Conclusion
Performing FNAC on soft-tissue lesions can obviate needless tissue biopsies for lesions, such as calcinosis cutis, in appropriate patients, thus avoiding the risks and complications associated with more invasive procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reiter N, El-Shabrawi L, Leinweber B, Berghold A, Aberer E. Calcinosis cutis: Part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:1–14. doi: 10.1016/j.jaad.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 2.Maize J, Metcalf . Metabolic Diseases of the skin. In: Elder D, editor. Lever's Histopathology of the Skin. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 1999. pp. 379–82. [Google Scholar]
- 3.Olsen KM, Chew FS. Tumoral calcinosis: Pearls, polemics, and alternative possibilities. Radiographics. 2006;26:871–85. doi: 10.1148/rg.263055099. [DOI] [PubMed] [Google Scholar]
- 4.Datta C, Bandyopadhyay D, Bhattacharyya S, Ghosh S. Tumoral calcinosis. Indian J Dermatol Venereol Leprol. 2005;71:293–4. doi: 10.4103/0378-6323.16631. [DOI] [PubMed] [Google Scholar]
- 5.James WD, Berger TG, Elson DM. Errors in metabolism. In: James WD, Berger TG, Elston DM, editors. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Canada: Saunders Elsevier; 2006. pp. 519–46. [Google Scholar]
- 6.Aksoy HM, Ozdemir R, Karaaslan O, Tiftikcioglu YO, Oruç M, Koçer U. Incidental idiopathic calcinosis cutis in a rhytidectomy patient. Dermatol Surg. 2004;30:1145–7. doi: 10.1111/j.1524-4725.2004.30342.x. [DOI] [PubMed] [Google Scholar]
- 7.Stewart VL, Herling P, Dalinka MK. Calcification in soft tissues. JAMA. 1983;250:78–81. [PubMed] [Google Scholar]
- 8.Deshpande A, Munshi M. Calcinosis cutis: Diagnosis by aspiration cytology — A case report. Diagn Cytopathol. 1999;21:200–2. doi: 10.1002/(sici)1097-0339(199909)21:3<200::aid-dc11>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 9.Shivkumar VB, Gangane N, Kishore S, Sharma S. Cytological features of idiopathic scrotal calcinosis. Acta Cytol. 2003;47:110–1. [PubMed] [Google Scholar]


