Abstract
Introduction
Health outcomes research has gained considerable traction over the past decade as the medical community attempts to move beyond traditional outcome measures such as morbidity and mortality. Since its inception in 2009, the BREAST-Q has provided meaningful and reliable information regarding health related – quality of life (HR-QOL) and patient satisfaction for use in both clinical practice and research. Now five years from its initial publication, we review how researchers have utilized the BREAST-Q and how it has enhanced our understanding and practice of plastic and reconstructive breast surgery.
Methods
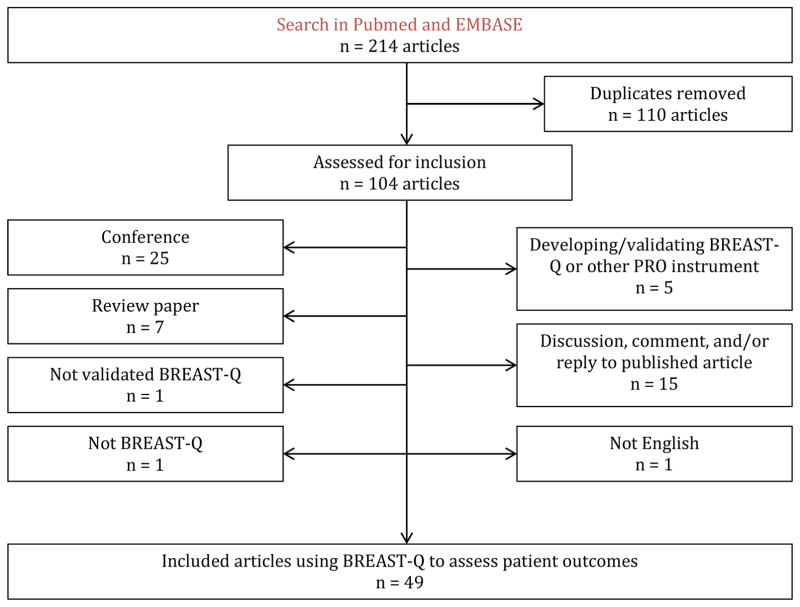
An electronic literature review was performed to identify publications that used the BREAST-Q to assess patient outcomes. Studies developing and/or validating the BREAST-Q or an alternate patient reported outcome measure (PROM), review papers, conference abstracts, discussions, comments and/or responses to previously published papers, studies that modified a version of BREAST-Q, and studies not published in English were excluded.
Results
Our literature review yielded 214 unique articles, 49 of which met our inclusion criteria. Important trends and highlights were further examined.
Discussion
The BREAST-Q has provided important insights in breast surgery highlighted by literature concerning autologous reconstruction, implant type, fat grafting, and patient education. The BREAST-Q has increased the use of PROMs in breast surgery and provided numerous important insights in its brief existence. The increased interest in PROMs as well as the under utilized potential of the BREAST-Q should permit its continued use and ability to foster new innovations and improve quality of care.
Introduction
Health outcomes research in surgery has gained considerable traction over the past decade as the surgical community attempts to curb soaring health care costs and move past traditional outcome measures such as morbidity and mortality.1 As a component of this change, patient-reported outcome measures (PROMs), wherein the patient’s perception of his or her outcomes is quantified, have become increasingly important.2 In plastic surgery, patient-centered outcomes data is of particular importance as the majority of operative interventions aim to improve appearance, function and/or quality of life. Thus, while photographic analysis remains indispensable, the new focus on patient perceptions offers potentially valuable insights into the effectiveness of surgical interventions.
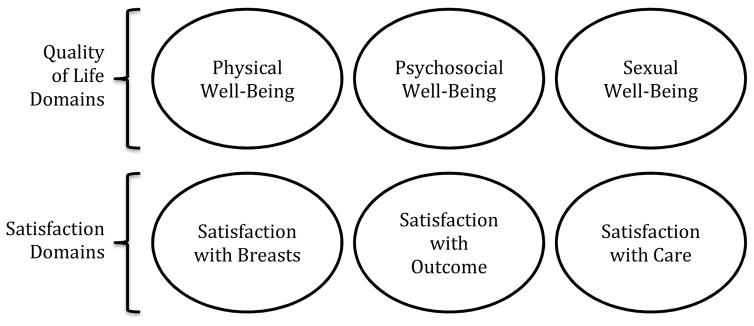
The BREAST-Q, a validated PROM now translated into thirty languages, quantifies the impact of cosmetic and reconstructive breast surgery (i.e., augmentation, reduction/mastopexy, mastectomy, reconstruction, and breast conserving-therapy), pre- and post-operatively, on health-related quality of life (HR-QOL; including physical, psychosocial, and sexual well-being) and patient satisfaction (including satisfaction with breasts, outcome, and care) (see Figure 1). Investigators and clinicians can choose to use only those scales that are pertinent to their research question. The questionnaire items in each scale are arranged in a clinically relevant hierarchy (e.g., Satisfaction with Breasts scale ranges from “How satisfied are you with how you look in a mirror clothed?” to “How satisfied are you with how you look in the mirror unclothed?”). While each scale produces an independent score from 0–100, there is no overall BREAST-Q score. Scores are transformed via the Q-Score program (https://webcore.mskcc.org/breastq/) or designated tables.2,3
Figure 1.
BREAST-Q conceptual framework. (Pusic A, Klassen A, Scott A, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. with permission.)
In this review, we examine the use of the BREAST-Q in the surgical research literature, and in particular how use of the BREAST-Q has enhanced the understanding and the practice of plastic and reconstructive breast surgery.
Methods
An electronic literature review was performed to identify publications that used the BREAST-Q as an outcome measure. Two search engines, PubMed and EMBASE, were queried with the terms “BREAST-Q” and “BREASTQ” from inception to January 2015. Two authors (WC and LM) separately reviewed all of the titles and abstracts of all articles identified in the search to exclude non-relevant articles. Any differences in opinion were resolved by a third author (AP). Included articles described the use of the BREAST-Q in a primary research study that assessed patient outcomes in a breast surgery population. Studies developing and/or validating the BREAST-Q or an alternate PROM, review papers, conference abstracts, thesis, commentaries, letters to the editor, studies that used a modified a version of BREAST-Q, and studies not published in English were excluded. A citation review of included articles was performed to identify any additional articles.
For publications that met the study inclusion criteria, we extracted the following information: country of origin, study aim, study design, sample size, BREAST-Q module utilized, and key findings. Study design was classified as prospective cohort or cross-sectional. Prospective cohort studies were defined as studies in which patients completed the BREAST-Q at multiple time points. Cross sectional studies were defined as those in which patients completed the BREAST-Q at a single time point. BREAST-Q data collection was classified as pre-operative, post-operative, or both.
Results
Our literature review yielded 214 unique articles. After implementing the exclusion criteria, 49 manuscripts from peer-reviewed journals met our inclusion criteria and were included in the analysis (Figure 2).
Figure 2.
Article inclusions and exclusions
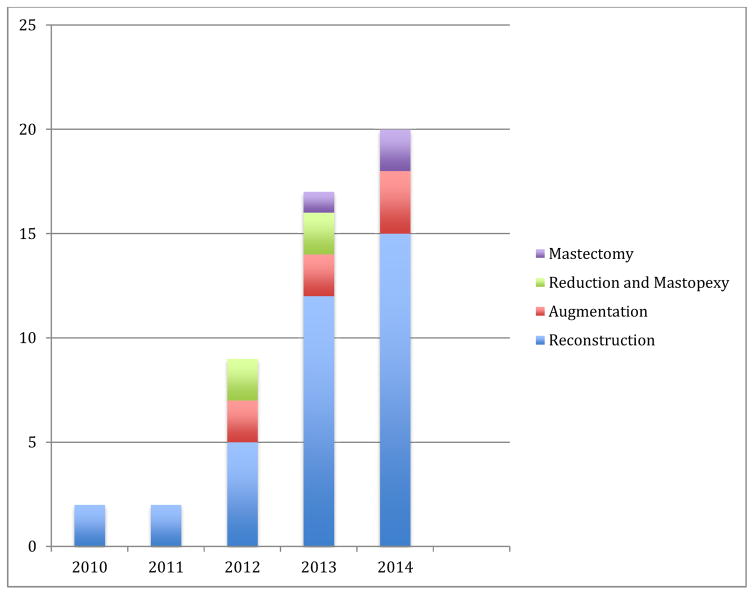
Since its inception in 2009, the number of publications incorporating the BREAST-Q has increased each year (Figure 3). From the 49 publications, a total of 22,457 patients completed at least one subdomain of the BREAST-Q. Of these participants, 20,390 patients completed one or more scales from the breast reconstruction module. The breast reconstruction module was utilized in 39 references; the augmentation module was reported in 7 references; the reduction module in four; and the mastectomy module in three.
Figure 3.
Frequency of BREAST-Q by year.
The cross sectional study design was the most prevalent, being used in 71% of publications (n=35). The BREAST-Q was administered in a prospective study design in 29% of studies (n = 14). Two studies distributed the questionnaire only pre-operatively, 29 only post-operatively, and 18 both pre- and postoperatively. Within the augmentation module, the majority of studies included both pre- and post-operative assessments (71%), while among the reconstruction module, post-operative assessment only was more common (72%).
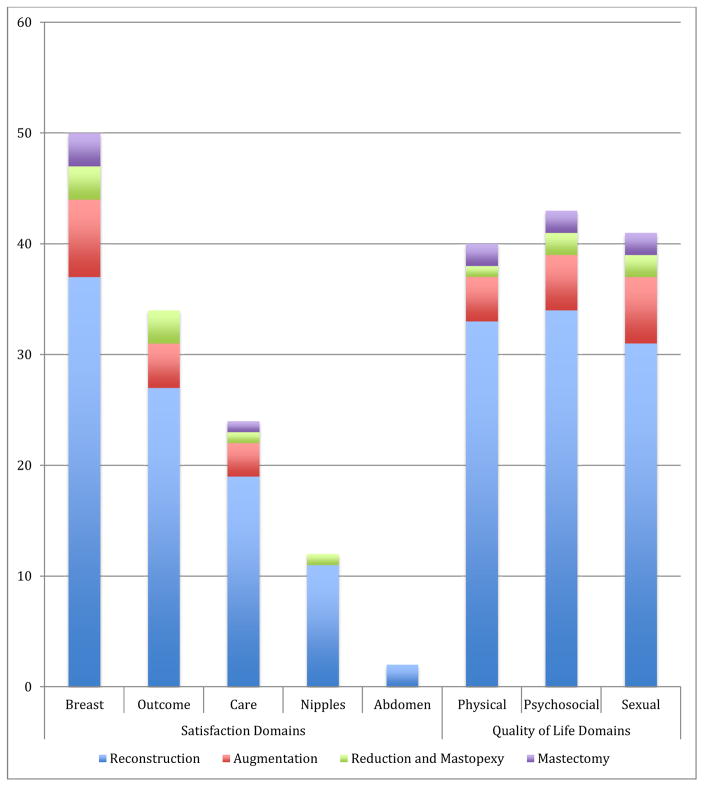
In all but one publication, the Satisfaction with Breasts scale was used. Within the HR-QOL domain, the sexual, physical, and psychosocial domains were used with almost equal frequency in 41, 40, and 43 studies, respectively (Figure 4).
Figure 4.
Domain and subdomain frequency.
Table 1 provides a summary of findings from the 49 publications identified by this review. The comparative effectiveness of different approaches to breast reconstruction was a popular topic; authors investigated outcomes of silicone versus saline implants, and also of autologous versus implant reconstruction. The BREAST-Q was used to highlight emerging techniques in plastic surgery with fat grafting figuring prominently. It was also used in one large UK study to compare the performance of different hospital providers. Lastly, while much of the literature focused on surgical outcomes, a number of studies also used the BREAST-Q to evaluate the patient experience.
Table 1.
Summary of BREAST-Q publications
| First Author | Year | Country of Origin | Level of Evidence | Title | n | Study Design | Relevant Key Findings |
|---|---|---|---|---|---|---|---|
| Augmentation | |||||||
| McCarthy | 2012 | USA | 2c | The magnitude of effect of cosmetic breast augmentation on patient satisfaction and health-related quality of life | 41 | Prospective | Breast augmentation was associated with an increase in satisfaction with breasts, psychosocial, and sexual well-being compared to preop. |
| Coriddi | 2013 | USA | 2c | Analysis of Satisfaction and Well-Being in the Short Follow-up From Breast Augmentation Using the BREAST-Q, a Validated Survey Instrument | 129 | Prospective | Breast augmentation was associated with higher scores for satisfaction with breasts, psychosocial and sexual well-being, and lower scores for physical well-being compared to pre-op. Satisfaction with outcome was associated most strongly with satisfaction with breasts. |
| Weigert | 2013 | France | 2c | Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals | 35 | Prospective | Breast augmentation was associated with improved satisfaction with breasts, sexual and psychosocial well-being at least 4 months post-op compared to preop. |
| Alderman | 2014 | USA | 2c | Understanding the Effect of Breast Augmentation on Quality of Life: Prospective Analysis Using the BREAST-Q | 611 | Prospective | Breast augmentation was associated with higher patient satisfaction with breasts, psychosocial, and sexual well-being, and a decrease in physical well-being compared to preop. Older patients were found to have less satisfaction with breasts compared to younger patients. |
| Gryskiewicz | 2014 | USA | 2c | Transaxillary Nonendoscopic Subpectoral Augmentation Mammaplasty: A 10-Year Experience With Gel vs Saline in 2000 Patients—With Long-Term Patient Satisfaction Measured by the BREAST-Q | 670 | Cross-sectional | Axillary augmentation compared with non-axillary augmentation was associated with higher satisfaction with breasts and outcome. Satisfaction with outcome was greater in patients with silicone gel compared with saline implants. |
| Spear | 2014 | USA | 2c | A Prospective Study on Lipoaugmentation of the Breast | 10 | Prospective | Satisfaction with breasts and sexual well-being was higher after lipoaugmentation compared to preop, however statistical significance was not reported. |
| Reduction/Mastopexy | |||||||
| Carty | 2012 | USA | 2c | Patient satisfaction and surgeon experience: A follow-up to the reduction mammaplasty learning curve study | 279 | Cross-sectional | Older patients compared with younger were more satisfied with breasts after reduction mammaplasty. Post-operative soft tissue necrosis was associated with lower satisfaction with breasts and outcome. No differences were found in patient satisfaction with outcomes and/or breasts based on surgeon age or experience. |
| Gonzalez | 2012 | USA | 2c | Quality of life after breast reduction surgery: a 10-year retrospective analysis using the Breast Q questionnaire: does breast size matter? | 178 | Cross-sectional | Breast reduction was associated with high satisfaction with outcome. No difference was found in satisfaction with outcome by quantity of breast tissue removed. |
| Coriddi | 2013 | USA | 2c | Analysis of satisfaction and well-being following breast reduction using a validated survey instrument: The BREAST-Q | 49 | Prospective | Breast reduction was associated with higher satisfaction with breasts, psychosocial, sexual, and physical well-being compared to preop. Satisfaction with outcome and breast after reduction were highly correlated. |
| Gurunluoglu | 2013 | USA | 2c | Outcomes analysis of patients undergoing autoaugmentation after breast implant removal | 20 | Prospective | Breast implant removal and autoaugmentation was associated with higher satisfaction with breasts, psychosocial and sexual well-being compared to preop. |
| Reconstruction | |||||||
| Macadam | 2010 | Canada | 2c | Patient Satisfaction and Health-Related Quality of Life following Breast Reconstruction: Patient-Reported Outcomes among Saline and Silicone Implant Recipients | 143 | Prospective | Silicone implants compared with saline implants in breast reconstruction was associated with higher satisfaction with outcome, surgeon, psychosocial and sexual well-being. Saline implants were associated with higher systemic side effects. |
| McCarthy | 2010 | USA | 2c | Patient satisfaction with postmastectomy breast reconstruction a comparison of saline and silicone implants | 482 | Cross-sectional | Silicone implants compared with saline implants in breast reconstruction was associated with higher satisfaction with breasts. Post-mastectomy radiotherapy and a longer time since reconstruction was negatively associated with satisfaction with breasts. |
| Goyal | 2011 | UK | 2c | Outcomes after autologous dermal sling-assisted immediate breast reconstruction | 14 | Cross-sectional | Breast reconstruction using a dermal sling was associated with high satisfaction with breasts and outcome. |
| Huang | 2011 | Taiwan | 2c | Simultaneous scarless contralateral breast augmentation during unilateral breast reconstruction using bilateral differentially split DIEP flaps | 6 | Prospective | Breast reconstruction was associated with higher satisfaction with breasts, psychosocial, and sexual well-being compared to preop. |
| Salgarello | 2012 | Italy | 2c | Fat Grafting and Breast Reconstruction with Implant: another option for irradiated breast cancer patients | 16 | Cross-sectional | Fat grafting followed by implant-based reconstruction of radiated breasts was associated with high patient satisfaction and well-being across all domains. |
| Salgarello | 2012 | Italy | 2c | Immediate breast reconstruction after skin-nipple-sparing mastectomy for previously augmented patients: A personal technique | 24 | Cross-sectional | Breast reconstruction in patients with previous augmentation was associated with higher satisfaction with breasts. |
| Dean | 2013 | Australia | 2c | Rotation flap approach mastectomy | 37 | Cross-sectional | Breast reconstruction compared to mastectomy only was associated with greater satisfaction with breasts and psychosocial well-being. |
| Inbal | 2012 | Israel | 2c | Simultaneous Contralateral Breast Adjustment in Unilateral Deep Inferior Epigastric Perforator Breast Reconstruction | 51 | Cross-sectional | Unilateral DIEP with simultaneous, delayed or no contralateral surgeries were compared. No differences in BREAST-Q scores between simultaneous or delayed adjustments. |
| Salgarello | 2012 | Italy | 2c | Inverted-T skin-reducing mastectomy with immediate implant reconstruction using the submuscular-subfascial pocket | 14 | Cross-sectional | Breast reconstruction was associated with high satisfaction and well-being in all subdomains except in two patients who had substantial skin necrosis. |
| Zhong | 2012 | Canada | 2c | Patient satisfaction and health-related quality of life after autologous tissue breast reconstruction: A prospective analysis of early postoperative outcomes | 51 | Prospective | Breast reconstruction was associated with an improvement in satisfaction with breasts, sexual well-being and psychosocial well being. Physical well-being of chest and abdomen was lowest at 3 weeks postoperative, with significant improvement at 3 months. |
| Cha | 2013 | New Zealand | 2c | Patient-reported outcomes following breast reconstruction surgery in a public hospital: use of the Breast-Q questionnaire | 75 | Cross-sectional | Satisfaction with medical team and office staff after breast reconstruction varied by ethnicity, with Europeans more satisfied than Maori or other ethnicities. |
| Eltahir | 2013 | The Netherlands | 2c | Quality-of-life Outcomes between Mastectomy Alone and Breast Reconstruction: Comparison of patient-reported Breast-Q and other Health related QOL measures | 137 | Cross-sectional | Breast reconstruction compared with mastectomy alone was associated with greater satisfaction with appearance of chest and breasts, and psychosocial, sexual, and physical well-being. |
| Eriksson | 2013 | Hungary/Sweden | 2c | Radiotherapy in implant-based immediate breast reconstruction: risk factors, surgical outcomes, and patient-reported outcome measures in a large Swedish multicenter cohort | 725 | Cross-sectional | Radiation therapy compared with none in patients with implant-based immediate breast reconstruction was associated with worse outcomes for satisfaction with breasts, outcome, and physical, sexual, and psychosocial well-being. Higher BMI was associated with lower satisfaction with breasts, and worse sexual and psychosocial well-being. Pre-op chemo was associated with lower satisfaction with breasts and psychosocial well-being. Psychosocial well-being was lowest in those younger than 40 years and highest in those older than 66 years. |
| Ho | 2013 | Canada | 2c | Optimizing patient-centered care in breast reconstruction: the importance of preoperative information and patient-physician communication | 510 | Cross-sectional | Satisfaction with information and the plastic surgeon was associated with higher satisfaction with breasts and outcome in breast reconstruction patients. |
| Koslow | 2013 | USA | 2c | Long-term patient-reported satisfaction after contralateral prophylactic mastectomy and implant reconstruction | 294 | Prospective | In patients with unilateral breast cancer, contralateral prophylactic mastectomy with reconstruction was associated with higher satisfaction with breasts and outcome compared to unilateral mastectomy with reconstruction. The absence of lymphedema was associated with higher satisfaction with outcome. |
| Macadam | 2013 | Canada | 2c | Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recipients | 128 | Cross-sectional | The use of shaped versus round silicone based-implants in breast reconstruction was not associated with differences on any satisfaction and well-being scale. |
| Rosson | 2013 | USA | 2c | Quality of life before reconstructive breast surgery: A preoperative comparison of patients with immediate, delayed, and major revision reconstruction | 170 | Cross-sectional | Satisfaction with breasts, psychosocial, sexual, and physical well-being prior to breast reconstruction was highest in patients undergoing immediate reconstruction, followed by patients undergoing delayed reconstruction, and lastly in patients undergoing major revision reconstruction. |
| Sugrue | 2013 | Ireland | 2c | An evaluation of patient reported outcomes following breast reconstruction utilizing the Breast Q | 30 | Cross-sectional | There were no differences in satisfaction with breasts, physical, psychosocial and sexual well-being for breast reconstruction patients who retrospectively reported their pre- and post-operative results. |
| Tadiparthi | 2013 | UK | 2c | An analysis of the motivating and risk factors for conversion from implant-based to total autologous breast reconstruction | 118 | Prospective | Conversion to autologous reconstruction from failed implant reconstruction was associated with increased satisfaction with breasts. |
| Wu | 2013 | USA | 2c | Human acellular dermal matrix (AlloDerm) dimensional changes and stretching in tissue expander/implant breast reconstruction | 76 | Cross-sectional | Breast reconstruction with acellular dermal matrix compared to no acellular dermal matrix was not associated with differences in satisfaction with breasts, outcomes, information, or physical or psychosocial well-being in patients at 3 months postop. |
| Zhong | 2013 | Canada | 2c | Decision regret following breast reconstruction: the role of self-efficacy and satisfaction with information in the preoperative period | 100 | Cross-sectional | Higher satisfaction with information was associated with lower regret after breast reconstruction. Increased self-efficacy was associated with higher satisfaction with information. |
| Albornoz | 2014 | USA | 2c | Implant breast reconstruction and radiation: A multicenter analysis of long-term health-related quality of life and satisfaction | 633 | Cross-sectional | Patients who had undergone implant-based breast reconstruction with radiation therapy had lower scores for satisfaction with breasts, outcome, psychosocial, sexual, and physical well-being compared to non-radiated patients. |
| Atisha | 2014 | USA | 2c | A National Snapshot of Satisfaction with Breast Cancer Procedures | 7619 | Cross-sectional | Women who underwent autologous tissue reconstruction reported the highest breast satisfaction scores compared to prostheses, breast-conserving- therapy, or mastectomy only. Women undergoing mastectomy without reconstruction reported the lowest satisfaction with breasts. |
| Chao | 2014 | Taiwan | 2c | Monitoring patient-centered outcomes through the progression of breast reconstruction: a multicentered prospective longitudinal evaluation | 100 | Prospective | Satisfaction with breasts, psychosocial, physical, and sexual well-being were higher pre-operatively for women with mastectomy only compared to mastectomy with reconstruction. Scores across all domains were initially lower in patients with delayed compared to immediate reconstruction, with equalization at 9 months post-op. |
| Davis | 2014 | USA | 2c | Breast reconstruction satisfaction rates at a large county hospital | 65 | Cross-sectional | A major complication versus no complication was associated with lower scores for satisfaction with breasts and outcome. Delayed versus immediate reconstruction was associated with increased satisfaction with breast. |
| Howes | 2014 | Australia | 2c | Autologous fat grafting for whole breast reconstruction | 1 | Prospective | Case report of one woman who underwent single-stage large-volume breast reconstruction with autologous fat grafting, with an increase in satisfaction with breasts, outcome, psychosocial, sexual and physical well-being after fat grafting. |
| Jeevan | 2014 | England | 2c | Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England | 7110 | Prospective | Women who underwent immediate reconstruction had higher satisfaction with breasts and overall well-being compared to mastectomy only. |
| Lee | 2014 | Australia | 2c | The scarless latissimus dorsi flap provides effective lower pole prosthetic coverage in breast reconstruction | 32 | Cross-sectional | Scarless latissimus dorsi flap and traditional latissimus dorsi flap techniques are not significantly different for satisfaction with breasts, outcome, psychosocial, sexual and physical well-being. |
| Liu | 2014 | China/USA | 2c | Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q | 119 | Cross-sectional | Microsurgical abdominal flap breast reconstruction compared to staged implant-based reconstruction was associated with higher satisfaction with outcome, breasts, information, plastic surgeon, psychosocial, and sexual well-being. |
| Matros | 2014 | USA | 2c | Cost-effectiveness analysis of implants versus autologous perforator flaps using the BREAST-Q | 309 | Cross-sectional | BREAST-Q scores and cost of care were higher for DIEP reconstruction compared to implants. |
| McCarthy | 2014 | USA | 2c | Chest and upper body morbidity following immediate postmastectomy breast reconstruction | 308 | Cross-sectional | Women who underwent autologous reconstruction had the highest physical well-being scores, while women who underwent prosthetic based reconstruction had decreased chronic physical morbidity. |
| Mestak | 2014 | Czech Republic | 2c | Centrifugation versus puregraft for fatgrafting to the breast after breast-conserving therapy | 30 | Prospective | Satisfaction with breasts, psychosocial and sexual well-being improved after fat grafting. Satisfaction with breasts was higher with pure graft compared with centrifugation. |
| Ng | 2014 | Australia | 2c | Breast reconstruction post mastectomy: patient satisfaction and decision making | 143 | Cross-sectional | Reconstruction compared with mastectomy alone was associated with higher satisfaction with breasts, psychosocial, and sexual well-being. Patients who underwent reconstruction reported higher self-image, more clothing choices, and feelings of overcoming cancer. |
| Peled | 2014 | USA | 2c | Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction | 28 | Prospective | Satisfaction with breasts, psychosocial, and sexual well-being after breast reconstruction was lowest at 1 month post-op, but returned to baseline by 1 year. |
| Simpson | 2014 | Canada | 2c | Multidisciplinary assessment for immediate breast reconstruction: A new approach | 26 | Prospective | Prior to reconstruction, women who would undergo delayed reconstruction had lower satisfaction with breasts, psychosocial, and sexual well-being compared to women who would undergo immediate delayed reconstruction. Post-operative satisfaction with breasts, physical, and sexual well-being between immediate and delayed reconstruction patients were not significant. |
| Sun | 2014 | USA | 2c | Assessing Women’s Preferences and Preference Modeling for Breast Reconstruction Decision-Making | 36 | Cross-sectional | The risk averse multiplicative model was the best fit for modeling the theoretical breast reconstructive preferences of women. |
| Eltahir | 2015 | The Netherlands | 2c | Which Breast Is the Best? Successful Autologous or Alloplastic Breast Reconstruction: Patient-Reported Quality-of-Life Outcomes | 92 | Cross-sectional | Women with autologous versus implant-based reconstruction were more satisfied with their breasts. |
| Sisco | 2015 | USA | 2c | The quality-of-life benefits of breast reconstruction do not diminish with age | 315 | Cross-sectional | Older women (>=65 years) undergoing post-mastectomy breast reconstruction versus mastectomy alone had higher reported satisfaction with breasts and psychosocial well-being. There were no differences in satisfaction with breasts, outcome, or psychosocial well-being between younger and older women undergoing post-mastectomy breast reconstruction. |
| Susarla | 2015 | USA | 2c | Comparison of Clinical Outcomes and Patient Satisfaction in Immediate Single-Stage versus Two-Stage Implant-Based Breast Reconstruction | 268 | Cross-sectional | Women undergoing direct to implant reconstruction versus two-stage reconstruction with tissue expander had higher sexual well-being, but lower satisfaction with medical and office staff. |
n = number of study participants; Country of Origin determined using corresponding author’s address; USA = United States of America; UK = United Kingdom Level of Evidence based off of the Oxford Centre for Evidence Based Medicine, 2009 guidelines (http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/)
Discussion
Since its inception in 2009, the BREAST-Q has been used to study breast surgery providing meaningful and reliable information regarding HR-QOL and patient satisfaction when used in clinical practice, in surgical research and quality improvement initiatives. This condition-specific PROM has been rapidly accepted by academic and private clinicians alike. Use of the BREAST-Q will continue to expand as HR-QOL and patient satisfaction becomes increasingly important as a metric for evaluating patient care from clinical, policy, and research perspectives. Below we consider five key areas of surgical practice, and elaborate upon the findings of this review to more fully describe where the BREAST-Q has and can be further used to better understand evidence-based, patient-centered surgical practice.
Why choose autologous reconstruction?
Reconstructive surgeons and their patients must choose between autologous and implant-based reconstruction following mastectomy. While traditional outcomes, such as rates of failure and re-operation have been well studied, the BREAST-Q has been used to provide a better understanding the impact of this decision on patients.4–6 There are now a number of studies that suggest the outcomes are better for patients receiving autologous reconstruction in comparison to implants.7–11 While the studies did not make a distinction between microsurgical techniques, the authors report that patients had higher levels of satisfaction, increased HR-QOL, and less chest and upper body morbidity with autologous reconstruction compared to implants.
The superior outcomes in the autologous reconstruction patients is additionally supported by previous studies not utilizing the BREAST-Q, which demonstrated superior aesthetic results when comparing transverse rectus abdominis myocutaneous (TRAM) reconstruction with implant-based reconstruction. 6,12–17 Additionally, Matros et al conducted a cost-effectiveness analysis, and reported that the more expensive procedure (autologous reconstruction) is worthwhile when cost and quality of life were factored together.17 The BREAST-Q provides researchers with the ability to quantify and compare patient perspectives, which is essential to demonstrate the value of potentially more time intensive or costly reconstructive options, such as free-tissue flap based reconstruction.
Which is better – saline or silicone?
With the moratorium on silicone implants now lifted,18 patients are presented with an option of silicone or saline implants. While some surgeons recommend silicone implants for their natural feeling and appearance, studies using the BREAST-Q provide evidence that can be used to help guide patients in their decision making process.4,19 In augmentation patients, Gryskiewicz et al. demonstrated that patients who received silicone implants were more satisfied with their overall outcome than patients who received saline. 20 In breast reconstruction patients, multiple studies have demonstrated similar findings with higher overall satisfaction, psychological well-being, sexual well-being, physical function, and satisfaction with their surgeon in patients receiving silicone implants in comparison to saline. 20–23 The BREAST-Q has been instrumental in helping to demonstrate greater patient satisfaction with silicone implants compared to saline, providing essential information to help future patients make educated decisions about reconstructive options.
Why perform fat grafting?
The use of fat grafting in breast surgery is becoming increasingly popular. 24 Multiple authors demonstrated high rates of satisfaction with breasts using the BREAST-Q in fat grafting for both reconstruction and augmentation. 24,25 Salgarello et al. demonstrated that fat grafting followed by autologous or implant-based reconstruction produced high satisfaction with breasts among patients who had previously undergone breast radiation, while Spear and Pittman found high patient satisfaction with breasts following fat grafting when used for breast augmentation.24,25 In a case report, Howes et al demonstrated the potential for autologous fat grafting as an option for whole breast reconstruction.24 While multiple questions remain regarding fat grafting’s safety, efficacy, and post-operative breast cancer screening, the BREAST-Q should help assess patient satisfaction with the procedure.
Why focus on patient education?
An important component of overall patient satisfaction is the patient experience of care, which can be measured using the BREAST-Q scales, satisfaction with information; surgeon; medical team; and office staff. These scales were utilized in only 49% of studies. In order to deliver patient-centered care and improve patient outcomes, surgeons and their teams should make the patient feel at ease and provide adequate pre-operative information. Ho et al. demonstrated that when a patient is satisfied with the information provided to her and also with the plastic surgeon, she is more likely to be satisfied with her surgical outcome. 26 These findings are supported by expectancy theory, which hypothesizes that pre-operative expectations play an important role in the patient’s assessment of outcomes and strongly predicts satisfaction and HR-QOL. 27–29
While most institutions track patient satisfaction, current methods using questionnaires, like those employed by Press-Ganey, which are not condition-specific, are often used for promotional advertising. The BREAST-Q, developed based on patient interview data, with its inclusion of different features of the patient experience, imparts providers with a surgery specific metric to improve their weaknesses, while reinforcing their strengths.
Is the BREAST-Q feasible in large-scale studies?
The National Health Service (NHS) audit on mastectomy and breast reconstruction included data from more than 8,000 women seen at 270 different hospitals throughout the United Kingdom.9 Postal surveys utilizing the BREAST-Q were returned at a rate of 81% during the study. This audit provided clinicians with important HR-QOL and patient satisfaction data, while highlighting the importance of adequate pre-operative information to patients. 9
In another study, Atisha et al conducted a study utilizing the Love/AVON Army of Women program.10 The cross sectional study surveyed women who had previously undergone surgery for breast cancer to compare different reconstructive procedures and how satisfaction changes over time for specific patient populations. 7,619 patients completed the BREAST-Q, electronically with an 82% response rate. Women who underwent autologous tissue reconstruction reported the highest breast satisfaction, while women who underwent a mastectomy without reconstruction reported the lowest.
Finally, the BREAST-Q is featured prominently in the Mastectomy Reconstruction Outcomes Consortium (MROC) Study, a five-year prospective, multicenter cohort study of mastectomy reconstruction patients funded by the National Cancer Institute. Over 60 plastic surgeons from 10 centers in the USA and Canada have contributed nearly 4,000 patients to the study, which began in February 2012.
These studies illustrate that the BREAST-Q is scalable to national and international levels and is able to achieve high response rates even with web-based administration. Large-scale studies such as those highlighted above will continue to produce generalizable PROs that clinicians and patients can utilize in future decision making.30
Where do we go from here?
While there has been a focus on breast reconstruction, relatively few studies have utilized the augmentation or reduction/mastopexy modules. The reconstruction module is the most frequently utilized, both in the number of studies and total number of patients, most likely secondary to its duration of availability and the academic and public interest in breast cancer and reconstruction.
However, over 290,000 breast augmentations and over 125,000 breast reductions were performed in 2013 compared to 95,000 breast reconstructions.31 This disparity in usage of the BREAST-Q provides an opportunity for research to enhance understanding of patient satisfaction and HR-QOL for patients undergoing breast augmentation or reduction.
The BREAST-Q’s multiple domains, which provide a near comprehensive view of patient HR-QOL and satisfaction, are also not consistently being utilized to their full potential. Investigators were most interested in the patients’ satisfaction with their breasts, reflecting a common primary endpoint of the reconstructive breast surgeon. Increased attention on the remaining domains, including psychosocial, sexual, and physical well-being, may provide an opportunity to optimize outcomes and deliver comprehensive patient-centered care.
When combined with a rigorous study design, the BREAST-Q can provide reliable evidence based data. The BREAST-Q was used most frequently as a cross sectional tool, assessing patient outcomes at a snapshot in time, often post-operatively. While this design allows a straightforward, singular administration of the BREAST-Q and provides clinicians and researchers the opportunity to compare patient outcomes and quantify potential causal associations between treatment variables, this approach does not provide information regarding changes in outcomes over time.32 Greater usage of prospective study designs, while often more cumbersome, allows data findings to be translated more reliably to patient-centered care.
The BREAST-Q and our review of studies have several limitations. We did not include non-peer reviewed studies, or those from conferences, which may provide additional meaningful clinical data. Also, in order to minimize bias, survey response rates need to be high. While this has been achieved in large-scale studies,9,10 local staff, both clinical and non-clinical, may need practical and methodological support, including training, when they are asked to assist in the collection of BREAST-Q data, which may be an even greater challenge in multicenter trials. Also, inherent in its use is selection bias – patients who fill out questionnaires may be more likely to either be very satisfied or very dissatisfied.33
Our review was not systematic and therefore there may be some omissions. However, we did not set out to conduct a systematic review, as the goal of this article was to provide surgeons with a general overview of the current published surgical research, as opposed to answering a specific research question. In addition, as is the case with most plastic surgery literature, studies that used the BREAST-Q were unlikely to be randomized controlled trials, as it is often not feasible to randomize patients. Furthermore, as the BREAST-Q becomes more ubiquitous, it is important that it is used as intended: changing questions, merging scales, and not using the scoring system as instructed will invalidate results.
Conclusion
The BREAST-Q is a PROM that allows both researchers and clinicians to answer important questions on patient satisfaction and HR-QOL. Its multiple modules and domains allow researchers and clinicians to comprehensively answer clinical questions specific to mastectomy, breast reconstruction, augmentation, and reduction/mastopexy patient populations. The standardized scoring methodology is simple to use and allows for comparisons between studies. The BREAST-Q has greatly improved our ability to understand PROs in patients undergoing breast surgery, and while it has already provided numerous important insights to date, the increased interest in PROs guarantees its continued use and ability to foster new innovations and standards of care.
Footnotes
Confliction of Interest
Drs. Pusic, Klassen, and Cano are co-developers of the BREAST-Q, which is owned by Memorial Sloan-Kettering Cancer Center. They receive a portion of licensing fees (royalty payments) when the BREAST-Q is used in industry sponsored clinical trials.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Curtin CM, Chung KC. A reflection of outcomes research and its impact on the practice of hand surgery. The Journal of hand surgery, European volume. 2014;39:790–3. doi: 10.1177/1753193414524138. [DOI] [PubMed] [Google Scholar]
- 2.Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plastic and reconstructive surgery. 2009;123:98e–106e. doi: 10.1097/PRS.0b013e31819565c1. [DOI] [PubMed] [Google Scholar]
- 3.Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The BREAST-Q: further validation in independent clinical samples. Plastic and reconstructive surgery. 2012;129:293–302. doi: 10.1097/PRS.0b013e31823aec6b. [DOI] [PubMed] [Google Scholar]
- 4.Cordeiro PG. Breast reconstruction after surgery for breast cancer. The New England journal of medicine. 2008;359:1590–601. doi: 10.1056/NEJMct0802899. [DOI] [PubMed] [Google Scholar]
- 5.Saulis AS, Mustoe TA, Fine NA. A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: comparison of three common procedures. Plastic and reconstructive surgery. 2007;119:1669–76. doi: 10.1097/01.prs.0000258827.21635.84. discussion 77–8. [DOI] [PubMed] [Google Scholar]
- 6.Alderman AK, Kuhn LE, Lowery JC, Wilkins EG. Does patient satisfaction with breast reconstruction change over time? Two-year results of the Michigan Breast Reconstruction Outcomes Study. Journal of the American College of Surgeons. 2007;204:7–12. doi: 10.1016/j.jamcollsurg.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Liu C, Zhuang Y, Momeni A, et al. Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast cancer research and treatment. 2014;146:117–26. doi: 10.1007/s10549-014-2981-z. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy CM, Mehrara BJ, Long T, et al. Chest and upper body morbidity following immediate postmastectomy breast reconstruction. Annals of surgical oncology. 2014;21:107–12. doi: 10.1245/s10434-013-3231-z. [DOI] [PubMed] [Google Scholar]
- 9.Jeevan R, Cromwell DA, Browne JP, et al. Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2014;67:1333–44. doi: 10.1016/j.bjps.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Atisha DM, Cox CE, Rushing CN, Samsa GP, Pusic AL, Abernethy AP. A national snapshot of satisfaction with breast cancer procedures. Annals of surgical oncology. 2014;21:10–1. doi: 10.1245/s10434-014-4246-9. [DOI] [PubMed] [Google Scholar]
- 11.Eltahir Y, Werners LL, Dreise MM, et al. Reply: quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported breast-Q and other health-related quality-of-life measures. Plastic and reconstructive surgery. 2014;133:595e. doi: 10.1097/PRS.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 12.Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA. Determinants of patient satisfaction in postmastectomy breast reconstruction. Plastic and reconstructive surgery. 2000;106:769–76. doi: 10.1097/00006534-200009040-00003. [DOI] [PubMed] [Google Scholar]
- 13.Giacalone PL, Bricout N, Dantas MJ, Daures JP, Laffargue F. Achieving symmetry in unilateral breast reconstruction: 17 years experience with 683 patients. Aesthetic plastic surgery. 2002;26:299–302. doi: 10.1007/s00266-002-2034-6. [DOI] [PubMed] [Google Scholar]
- 14.Hu ES, Pusic AL, Waljee JF, et al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship Period. Plastic and reconstructive surgery. 2009;124:1–8. doi: 10.1097/PRS.0b013e3181ab10b2. [DOI] [PubMed] [Google Scholar]
- 15.Spear SL, Newman MK, Bedford MS, Schwartz KA, Cohen M, Schwartz JS. A retrospective analysis of outcomes using three common methods for immediate breast reconstruction. Plastic and reconstructive surgery. 2008;122:340–7. doi: 10.1097/PRS.0b013e31817d6009. [DOI] [PubMed] [Google Scholar]
- 16.Tonseth KA, Hokland BM, Tindholdt TT, Abyholm FE, Stavem K. Quality of life, patient satisfaction and cosmetic outcome after breast reconstruction using DIEP flap or expandable breast implant. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2008;61:1188–94. doi: 10.1016/j.bjps.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plastic and reconstructive surgery. 2010;125:1585–95. doi: 10.1097/PRS.0b013e3181cb6351. [DOI] [PubMed] [Google Scholar]
- 18.Regulatory History of Breast Implants in the US. 2013 at http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants/ucm064461.htm.
- 19.Rohrich RJ, Reece EM. Breast augmentation today: saline versus silicone--what are the facts? Plastic and reconstructive surgery. 2008;121:669–72. doi: 10.1097/01.prs.0000298115.96337.72. [DOI] [PubMed] [Google Scholar]
- 20.Gryskiewicz J, LeDuc R. Transaxillary Nonendoscopic Subpectoral Augmentation Mammaplasty: A 10-Year Experience With Gel vs Saline in 2000 Patients-With Long-Term Patient Satisfaction Measured by the BREAST-Q. Aesthetic surgery journal/the American Society for Aesthetic Plastic surgery. 2014;34:696–713. doi: 10.1177/1090820X14530552. [DOI] [PubMed] [Google Scholar]
- 21.Macadam SA, Ho AL, Cook EF, Jr, Lennox PA, Pusic AL. Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plastic and reconstructive surgery. 2010;125:761–71. doi: 10.1097/PRS.0b013e3181cb5cf8. [DOI] [PubMed] [Google Scholar]
- 22.Macadam SA, Ho AL, Lennox PA, Pusic AL. Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recipients. Plastic and reconstructive surgery. 2013;131:431–41. doi: 10.1097/PRS.0b013e31827c6d55. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010;116:5584–91. doi: 10.1002/cncr.25552. [DOI] [PubMed] [Google Scholar]
- 24.Spear SL, Pittman T. A prospective study on lipoaugmentation of the breast. Aesthetic surgery journal/the American Society for Aesthetic Plastic surgery. 2014;34:400–8. doi: 10.1177/1090820X13520449. [DOI] [PubMed] [Google Scholar]
- 25.Salgarello M, Visconti G, Barone-Adesi L. Fat grafting and breast reconstruction with implant: another option for irradiated breast cancer patients. Plastic and reconstructive surgery. 2012;129:317–29. doi: 10.1097/PRS.0b013e31822b6619. [DOI] [PubMed] [Google Scholar]
- 26.Ho AL, Klassen AF, Cano S, Scott AM, Pusic AL. Optimizing patient-centered care in breast reconstruction: the importance of preoperative information and patient-physician communication. Plastic and reconstructive surgery. 2013;132:212e–20e. doi: 10.1097/PRS.0b013e31829586fa. [DOI] [PubMed] [Google Scholar]
- 27.Pusic AL, Klassen AF, Snell L, et al. Measuring and managing patient expectations for breast reconstruction: impact on quality of life and patient satisfaction. Expert review of pharmacoeconomics & outcomes research. 2012;12:149–58. doi: 10.1586/erp.11.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mancuso CA, Graziano S, Briskie LM, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clinical orthopaedics and related research. 2008;466:424–31. doi: 10.1007/s11999-007-0052-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hudak PL, Hogg-Johnson S, Bombardier C, McKeever PD, Wright JG. Testing a new theory of patient satisfaction with treatment outcome. Medical care. 2004;42:726–39. doi: 10.1097/01.mlr.0000132394.09032.81. [DOI] [PubMed] [Google Scholar]
- 30.Sun CS, Cantor SB, Reece GP, Crosby MA, Fingeret MC, Markey MK. Assessing Women’s Preferences and Preference Modeling for Breast Reconstruction Decision-Making. Plastic and reconstructive surgery Global open. 2014;2:e125. doi: 10.1097/GOX.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. [Accessed 1/15/15, 2015];Plastic Surgery Statistics Report. 2013 at http://www.plasticsurgery.org/Documents/news-resources/statistics/2013-statistics/plastic-surgery-statistics-full-report-2013.pdf.
- 32.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. International journal of surgery. 2014 [Google Scholar]
- 33.Edwards P, Roberts I, Clarke M, et al. Increasing response rates to postal questionnaires: systematic review. Bmj. 2002;324:1183. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCarthy CM, Cano SJ, Klassen AF, et al. The magnitude of effect of cosmetic breast augmentation on patient satisfaction and health-related quality of life. Plastic and reconstructive surgery. 2012;130:218–23. doi: 10.1097/PRS.0b013e318254b3bc. [DOI] [PubMed] [Google Scholar]
- 35.Coriddi M, Angelos T, Nadeau M, Bennett M, Taylor A. Analysis of satisfaction and well-being in the short follow-up from breast augmentation using the BREAST-Q, a validated survey instrument. Aesthetic surgery journal/the American Society for Aesthetic Plastic surgery. 2013;33:245–51. doi: 10.1177/1090820X12472980. [DOI] [PubMed] [Google Scholar]
- 36.Weigert R, Frison E, Sessiecq Q, Al Mutairi K, Casoli V. Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plastic and reconstructive surgery. 2013;132:1421–9. doi: 10.1097/01.prs.0000434415.70711.49. [DOI] [PubMed] [Google Scholar]
- 37.Alderman AK, Bauer J, Fardo D, Abrahamse P, Pusic A. Understanding the effect of breast augmentation on quality of life: prospective analysis using the BREAST-Q. Plastic and reconstructive surgery. 2014;133:787–95. doi: 10.1097/PRS.0000000000000023. [DOI] [PubMed] [Google Scholar]
- 38.Carty MJ, Duclos A, Gu X, Elele N, Orgill D. Patient satisfaction and surgeon experience: a follow-up to the reduction mammaplasty learning curve study. Eplasty. 2012;12:e22. [PMC free article] [PubMed] [Google Scholar]
- 39.Gonzalez MA, Glickman LT, Aladegbami B, Simpson RL. Quality of life after breast reduction surgery: a 10-year retrospective analysis using the Breast Q questionnaire: does breast size matter? Annals of plastic surgery. 2012;69:361–3. doi: 10.1097/SAP.0b013e31824a218a. [DOI] [PubMed] [Google Scholar]
- 40.Coriddi M, Nadeau M, Taghizadeh M, Taylor A. Analysis of satisfaction and well-being following breast reduction using a validated survey instrument: the BREAST-Q. Plastic and reconstructive surgery. 2013;132:285–90. doi: 10.1097/PRS.0b013e31829587b5. [DOI] [PubMed] [Google Scholar]
- 41.Gurunluoglu R, Sacak B, Arton J. Outcomes analysis of patients undergoing autoaugmentation after breast implant removal. Plastic and reconstructive surgery. 2013;132:304–15. doi: 10.1097/PRS.0b013e31829e7d9e. [DOI] [PubMed] [Google Scholar]
- 42.Goyal A, Wu JM, Chandran VP, Reed MW. Outcome after autologous dermal sling-assisted immediate breast reconstruction. The British journal of surgery. 2011;98:1267–72. doi: 10.1002/bjs.7531. [DOI] [PubMed] [Google Scholar]
- 43.Huang JJ, Chao LF, Wu CW, Nguyen DH, Valerio IL, Cheng MH. Simultaneous scarless contralateral breast augmentation during unilateral breast reconstruction using bilateral differentially split DIEP flaps. Plastic and reconstructive surgery. 2011;128:593e–604e. doi: 10.1097/PRS.0b013e318230c312. [DOI] [PubMed] [Google Scholar]
- 44.Salgarello M, Rochira D, Barone-Adesi L, Farallo E. Immediate breast reconstruction after skin- or nipple-sparing mastectomy for previously augmented patients: a personal technique. Aesthetic plastic surgery. 2012;36:313–22. doi: 10.1007/s00266-011-9809-6. [DOI] [PubMed] [Google Scholar]
- 45.Dean NR, Yip JM, Birrell S. Rotation flap approach mastectomy. ANZ journal of surgery. 2013;83:139–45. doi: 10.1111/ans.12008. [DOI] [PubMed] [Google Scholar]
- 46.Inbal A, Gur E, Otremski E, et al. Simultaneous contralateral breast adjustment in unilateral deep inferior epigastric perforator breast reconstruction. Journal of reconstructive microsurgery. 2012;28:285–92. doi: 10.1055/s-0032-1311682. [DOI] [PubMed] [Google Scholar]
- 47.Salgarello M, Visconti G, Barone-Adesi L, et al. Inverted-T skin-reducing mastectomy with immediate implant reconstruction using the submuscular-subfascial pocket. Plastic and reconstructive surgery. 2012;130:31–41. doi: 10.1097/PRS.0b013e3182547d42. [DOI] [PubMed] [Google Scholar]
- 48.Zhong T, McCarthy C, Min S, et al. Patient satisfaction and health-related quality of life after autologous tissue breast reconstruction: a prospective analysis of early postoperative outcomes. Cancer. 2012;118:1701–9. doi: 10.1002/cncr.26417. [DOI] [PubMed] [Google Scholar]
- 49.Cha R, Barnes E, Locke MB. Patient-reported outcomes following breast reconstruction surgery in a public hospital: use of the Breast-Q questionnaire. The New Zealand medical journal. 2013;126:43–55. [PubMed] [Google Scholar]
- 50.Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plastic and reconstructive surgery. 2013;132:201e–9e. doi: 10.1097/PRS.0b013e31829586a7. [DOI] [PubMed] [Google Scholar]
- 51.Eriksson M, Anveden L, Celebioglu F, et al. Radiotherapy in implant-based immediate breast reconstruction: risk factors, surgical outcomes, and patient-reported outcome measures in a large Swedish multicenter cohort. Breast cancer research and treatment. 2013;142:591–601. doi: 10.1007/s10549-013-2770-0. [DOI] [PubMed] [Google Scholar]
- 52.Koslow S, Pharmer LA, Scott AM, et al. Long-term patient-reported satisfaction after contralateral prophylactic mastectomy and implant reconstruction. Annals of surgical oncology. 2013;20:3422–9. doi: 10.1245/s10434-013-3026-2. [DOI] [PubMed] [Google Scholar]
- 53.Rosson GD, Shridharani SM, Magarakis M, et al. Quality of life before reconstructive breast surgery: A preoperative comparison of patients with immediate, delayed, and major revision reconstruction. Microsurgery. 2013;33:253–8. doi: 10.1002/micr.22081. [DOI] [PubMed] [Google Scholar]
- 54.Sugrue R, MacGregor G, Sugrue M, Curran S, Murphy L. An evaluation of patient reported outcomes following breast reconstruction utilizing Breast Q. Breast (Edinburgh, Scotland) 2013;22:158–61. doi: 10.1016/j.breast.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 55.Tadiparthi S, Staley H, Collis N, O’Donoghue JM. An analysis of the motivating and risk factors for conversion from implant-based to total autologous breast reconstruction. Plastic and reconstructive surgery. 2013;132:23–33. doi: 10.1097/PRS.0b013e318290f83e. [DOI] [PubMed] [Google Scholar]
- 56.Wu C, Cipriano J, Osgood G, Jr, Tepper D, Siddiqui A. Human acellular dermal matrix (AlloDerm(R)) dimensional changes and stretching in tissue expander/implant breast reconstruction. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2013;66:1376–81. doi: 10.1016/j.bjps.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 57.Zhong T, Temple-Oberle C, Hofer S, et al. The Multi Centre Canadian Acellular Dermal Matrix Trial (MCCAT): study protocol for a randomized controlled trial in implant-based breast reconstruction. Trials. 2013;14:356. doi: 10.1186/1745-6215-14-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Albornoz CR, Matros E, McCarthy CM, et al. Implant breast reconstruction and radiation: a multicenter analysis of long-term health-related quality of life and satisfaction. Annals of surgical oncology. 2014;21:2159–64. doi: 10.1245/s10434-014-3483-2. [DOI] [PubMed] [Google Scholar]
- 59.Chao LF, Patel KM, Chen SC, et al. Monitoring patient-centered outcomes through the progression of breast reconstruction: a multicentered prospective longitudinal evaluation. Breast cancer research and treatment. 2014;146:299–308. doi: 10.1007/s10549-014-3022-7. [DOI] [PubMed] [Google Scholar]
- 60.Davis GB, Lang JE, Peric M, et al. Breast reconstruction satisfaction rates at a large county hospital. Annals of plastic surgery. 2014;72(Suppl 1):S61–5. doi: 10.1097/SAP.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 61.Mestak O, Sukop A, Hsueh YS, et al. Centrifugation versus PureGraft for fatgrafting to the breast after breast-conserving therapy. World journal of surgical oncology. 2014;12:178. doi: 10.1186/1477-7819-12-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ng SK, Hare RM, Kuang RJ, Smith KM, Brown BJ, Hunter-Smith DJ. Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making. Annals of plastic surgery. 2014 doi: 10.1097/SAP.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 63.Peled AW, Duralde E, Foster RD, et al. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Annals of plastic surgery. 2014;72(Suppl 1):S48–52. doi: 10.1097/SAP.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 64.Simpson JS, Baltzer H, McMillian CR, et al. Multidisciplinary assessment for immediate breast reconstruction: A new approach. Surgical Practice. 2014;18:111–6. [Google Scholar]