Summary
Introduction.
Health care Workers are exposed to infectious diseases more than the general population. Many of these infections are preventable by vaccination. The objective in this study is to investigate whether, how, and which vaccination underwent Sardinia Health Care Workers (HCWs) and the variability of policies in different Hospital Health Managements of the whole region.
Methods.
In March 2013, we enrolled the Hospital Health Management of all the 32 Sardinia hospitals. We investigate on immunity against vaccine-preventable diseases and education campaigns about recommended vaccinations for HCWs. Flu, hepatitis B, measles-mumps-rubella, varicella and tuberculosis were the objects of our research.
Results.
In most of the hospitals, influenza vaccination coverage among HCWs is less than 6%. Hepatitis B antibody assay was performed in all the respondent hospitals but only 14 had available data as collected electronically. Most of the hospitals did not perform serological tests for the evaluation of antibodies against Varicella, Measles, Mumps and Rubella in their HCWs. In 30 hospitals Mantoux test was replaced or integrated by "in vitro" test for health surveillance protocols.
Conclusions.
This method produced a large amount of data in small time and at a low cost. Sending back data to respective Hospital Health Management (HHM) we took a step towards greater awareness of the issue of biological risks of HCWs and of vaccine coverage.
Key words: Vaccine-preventable disease, Healthcare workers, Infectious diseases
Introduction
Health care workers (HCWs) are defined as persons working in health-care milieu having potential exposure to patients and to infectious materials; they are exposed to infectious diseases more than the general population although many of these infections are preventable by vaccination. When infected, HCWs may transmit the infection to patients or colleagues [1].
Outbreaks due to vaccine-preventable diseases in health care facilities are often associated with serious morbidity and mortality among patients, disruption of healthcare services, and high costs for the National Health Service [2].
Immunization of HCWs is a major infection prevention measure [3] to protect HCWs and, indirectly, the patients who may not be naturally immunized or vaccinated [4]. Vaccination is a very effective tool to promote safety within health care facilities for both HCWs and patients. Nevertheless, inadequate coverage of HCWs against vaccine-preventable diseases is a global problem [5].
In Italy, vaccination policies for HCWs are based – on one hand – on the "National Vaccination Plan" [6] which reinforces the recommendation to vaccinate HCWs against selected vaccine preventable diseases. On the other hand, the Italian Legislative Decree 81/08 reorganizes and revises all the provisions regarding health and safety at work. In particular, the Decree ratifies the obligation to the employers to provide vaccination to workers exposed to biological risk and emphasizes the key role of the Occupational physician for assessing biological risk, identifying and managing susceptible workers, and organizing and implementing vaccine campaigns. Therefore, employers and Occupational physicians have to manage vaccination activities within hospitals for their workers. In this sense, the following vaccinations are strongly recommended: anti-hepatitis B, anti-influenza, anti-measles-mumps-rubella, anti-varicella and anti-pertussis. The Italian law has drastically limited the use of the anti-TB vaccination to very few categories of HCWs: those who are at high risk of exposure to multi- drug-resistant tubercular bacterial strains, and those who work in high-risk environments and – in the case of positive Mantoux Test – they cannot undergo preventive therapy because of clinical contraindications to the use of specific drugs. The aim of our study was to investigate (1) whether, how, and which vaccination underwent the Sardinia HCW's; (2) the variability of policies and solutions in different Hospital Health Managements (HHM) of the whole region.
Consequently, an indirect aim was to raise awareness about HHMs' compliance rate to vaccination programs and orient them in a positive approach towards vaccination in Sardinia.
Methods
In March 2013, we enrolled by both phone and a written questionnaire sent by e-mail the 32 HHM of all Sardinia hospitals which have totally 5,650 beds serving the whole Sardinia population (1.600.000 inhabitants).
A self-reported structured form was completed by HHMs. In case of lacking or inadequate response HHMs were successively contacted by phone to complete information. According to some critical aspects highlighted in 2010 by a team of occupational physicians of the Italian Society of Occupational Health and Industrial Hygiene (SIMLII), the questionnaire included 10 items based on multiple-choice questions. Each hospital was allowed to mark more than one answer per item.
The study investigated about the immunological pattern of HCWs towards Influenza, hepatitis B (HB), measles- mumps-rubella (MMR), varicella and tuberculosis (TBC). Furthermore, information was collected about the performed educational campaign for influenza vaccination. Specifically, five questions concerned flu vaccination and investigated (a) effective accomplishment of the educational campaign on vaccination and its starting, (b) the campaign planners, (c) the different strategies used to inform health professionals about the opportunity to undergo vaccination, (d) the topics used during the campaign, and (e) available data on vaccination coverage. One question regarded HB vaccination and the gathered data about compliance to vaccination. Two questions were addressed to serological surveillance: the first one asked whether serological tests for detection of MMR and Varicella viruses' antibodies were included in routine surveillance of HCWs by Occupational Health Physicians. The other one asked whether serological results were collected. The last two questions concerned TBC: one investigated whether and in which occasions HCWs underwent Mantoux skin test, the other one detected whether Mantoux was replaced or integrated by "in vitro" test.
The results were returned to each HHM in order to provide them a comparison with the other hospitals. In addition, we suggested recommendations about vaccination in HCWs according to National laws and National and International scientific communities.
Results
Out of the 32 hospitals enrolled in the study, 30 joined our survey (94% compliance): three were University Hospitals and 27 were General Hospitals. The two nonresponding hospitals were long-term care institutes. The total number of HCWs of the 30 hospitals was 12,977. Among these, 26% were medical staff, 47% nurses, and 27% represented other hospital staff.
INFLUENZA
Twenty-five out of the 30 hospitals (77%) accomplished the vaccination campaign against flu carried out between October and December 2011, particularly November, in 18 hospitals.
All the hospitals answered to the questions concerning the communication methods during the flu campaign: 18 hospitals (72%) informed HCWs about the chance to be vaccinated by newsletter to unit managers, nursing and technicians coordinator, 8 (32%) sending newsletter to unit managers only, 7 (28%) through active call, 2 (8%) using posters and advertising.
The coordination of the campaign was performed by HHM in 20 hospitals (80%), by Health visitors in 8 (32%) and by Occupational Health Physicians in 7 hospitals (28%). In 8 (32%) hospitals the Prevention Department managed the campaign. Therefore different professionals were involved in managing and coordinating the campaign in the different hospitals at the same time. This heterogeneity may depend on the hospital characteristics in terms of structure, complexity, size, and (urban or rural) area.
Concerning the topics used during the vaccination campaign to inform HCWs all 25 hospitals enlightened about professional and social responsibility in patients' protection; 20 reported also efficacy and safety of the vaccine and 17 warned about the frequency and severity of influenza.
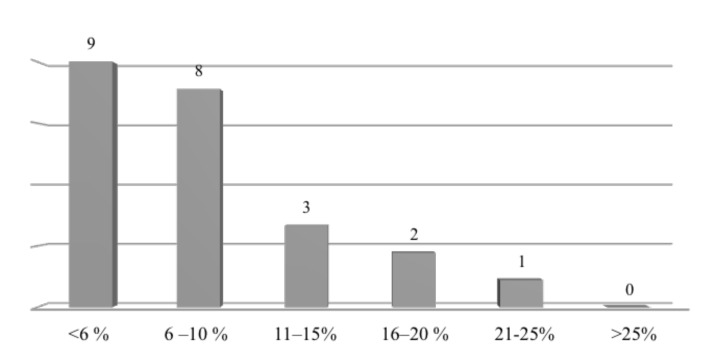
Data of vaccination coverage among HCWs were reported only by 23 hospitals. The coverage rate is shown in Figure 1; 74% of the hospitals indicated a coverage rate lower than 10%.
Fig. 1.
Influenza vaccination coverage rate in HCWs of 23 Sardinia Hospitals.
HEPATITIS B
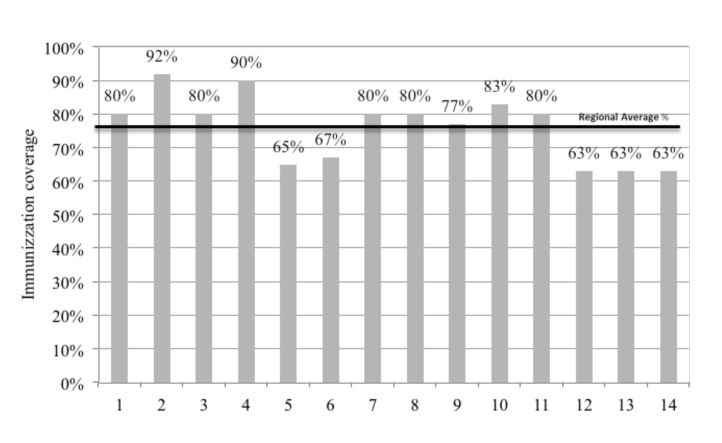
Data on immunization coverage were available in 14 of 30 hospitals (Fig. 2). Regional average was 76%; 5 hospitals were below the average and 9 were above, only one hospital had 92% vaccination coverage. Antibody assay (anti-HBs) was carried out in all the 30 respondent hospitals but only 14 had electronically collected data.
Fig. 2.
Immunization coverage for Hepatitis B in 14 Sardinia Hospitals.
VARICELLA, MEASLES, MUMPS, RUBELLA
Most hospitals did not perform serological tests to detect antibodies against Varicella, Measles, Mumps and Rubella viruses in HCWs.
Three (10%) hospitals applied health surveillance for those viruses and other two hospitals performed serological test for Rubella in higher risk occupational categories.
No hospital had available data on immunity to those infections.
TUBERCULOSIS
Intradermal Mantoux test was used in 29 of 30 hospitals: in 32% of hospitals HCWs were submitted to the Mantoux test at the hiring time and/or in post exposure situations.
In 1 hospital, Mantoux test was replaced by "in vitro" test (Quantiferon) and in 20 hospitals Quantiferon integrated Mantoux test.
Discussion
Vaccination is an important prophylactic action to reduce the number of susceptible HCWs and to indirectly protect susceptible patients and colleagues [7]. An additional benefit is a reduction in work time lost due to illness. Despite the persistence of outbreaks of vaccinepreventable diseases in health care facilities, HCWs vaccination rates remain suboptimal globally. Higher vaccination coverages among HCWs than the actual would be useful both to reinforce occupational safety in health care facilities and to prevent nosocomial outbreaks [1, 8, 9].
The Italian Health Ministry recommends HCWs to undergo vaccinations (i.e. anti-hepatitis B, anti-flu, antimeasles- mumps-rubella, varicella, anti-pertussis and, when indicated, anti-tuberculosis) not only to reduce employees' absenteeism that may increase workload for staff, but also to prevent the nosocomial infection risk, especially in elderly or immunocompromised patients [6]. The same Institution have also included among the new objectives of the National Prevention Plan 2014-2018 an increasing vaccination coverage for both general and high-risk population including HCWs, by looking for a cooperation between regions in which regions more experienced can support regions with the lowest vaccination coverage [10].
Several outbreaks of health care facility-acquired influenza, including immunosuppressed or old patients, have been documented as a consequence of low vaccine effectiveness, thus requiring consequently an indirect protection. Influenza vaccination of all HCWs is recommended by the World Health Organization (WHO), [11] US Centers for Disease Control and Prevention (CDC) [1], and by the Italian Ministry of Health [6] in order to prevent transmission of influenza from HCWs to patients. Nevertheless, the same countries show a low uptake of influenza vaccine in HCWs [12]. A global literature review on vaccination programs in HCWs reported a percentage of vaccination coverage ranging from 2.1% to 82%, with highest uptake rates occurring in USA [13] (from 40% to 87.4%) [14, 15, 16, 17], followed by Germany (26.9%) [18], and Spain (from 14.7% to 38%) [19]. In Italy, data on vaccination coverage among HCWs are not regularly collected and the few ad-hoc studies have shown low coverage rates of 0-29% [20], and 20.8% [21]. In the 2012-2013 season, the coverage rate for the working-age population was 10% [22]. In our survey most of Sardinia hospitals had an influenza coverage rate lower than 6%.
Some studies highlighted how compulsory influenza vaccination with forfeit for non-adhesions was associated with larger compliance to vaccination programs [23]. Other authors asserted that voluntary vaccination of HCWs against influenza would represent the most effective strategy [24]. Hospitals that used personal contact approach had higher vaccination rates [24, 25]. Differently, newsletters sent by HHM to unit managers, and both nurse and technician coordinators were the most frequent tool used by Sardinia hospitals. Nevertheless, this tool obtained a vaccination coverage lower than 10% in 74% of the involved hospitals. A recent Italian study implemented different actions such as education, promotion, and easy access to staff vaccination in order to increase HCWs vaccination coverage [26]. Despite these efforts, the results showed that the vaccination coverage in the hospital staff was underperforming. On the light of these results, new techniques of information and empowerment on the importance of flu vaccination for HCWs should be considered and activated.
In 1997, CDC recommended HBV vaccination for all HCWs [27]; nevertheless, HBV vaccine coverage rate in USA was 63.4%, well below the 90% goal [28]. Similar percentages were reported in other countries (85% for Belgium, 55.4% for India, and 55% for Morocco) [29, 30, 31].
In 1991, Italy introduced HBV mandatory vaccination for infants and 12-year-old adolescents until 2003 when the two cohorts joined together [32]. In persons who received primary immunization in the first year of life, immune memory for HBsAg lasted for at least 17 years and additional booster doses were not needed to enhance long-term immunization [33, 34, 35, 36]. In Italian HCWs who did not receive HBV vaccination as adolescents and are older than 35-36 years, testing HCWs at hiring time and administering the vaccine to those who prove susceptible to HBV infection is strongly advised. In Italy, the coverage rate of HBV vaccination ranged from 43% to 87% [37]. Thus, we emphasize that efforts should be made to increase the number of vaccinated HCWs for HBV protection.
Measles, mumps, rubella, and varicella (MMRV) are highly contagious diseases, and pose a high risk for both HCWs and patients [2]. In Italy, the percentage of immunization in HCWs ranged from 85.7% to 95.1% for varicella, from 47% to 96.8% for rubella, from 71.4% to 97.8% for measles, and from 52.5% to 87.6% for mumps [38, 39]. These results show a significant proportion of unprotected workers. In fact, most of the Sardinia hospitals did not perform serological tests for MMVR on HCWs.
Furthermore, tuberculosis still remains a severe worldwide health problem, especially among immunocompromised patients. High percentage of latent Mycobacterium tuberculosis infection among HCWs and the increasing number of Mycobacterial strains resistant to the main drug therapies increases the need for prevention programs health care workers.
Tuberculin skin test (TST) is still globally recommended to screen HCWs [40] despite its limitations. In effect, the need for a return visit to assess the test effect, often, results in a low compliance to follow-up [41]. These limits could be overtaken by advancement in the in vitro test, which detects the interferon-g production in response to other Mycobacterium tuberculosis antigens. QuantiFERON- in tube test (QFT-in tube) does not need for a second visit to interpret results and it has a higher specificity than TST [42]. An Australian study compared QFT-in tube test to the TST in HCWs. The results demonstrated that positive QFT-in tube test strongly correlated with risk factors for TB exposure more than positive TST, especially in a low tuberculosis prevalence population. Yet, a positive TST strongly correlated with a prior history of BCG vaccination [43].
The main limitation of the study regards the data collection method. Specifically, we have used a nonvalidated questionnaire, which can result in a low level of reliability of the data. Furthermore, we did not examine the vaccination coverage according to the different occupational categories and healthcare settings. This did not allow us to identify specific professionals or healthcare areas that mainly need for specific intervention strategies to increase vaccination coverages.
Nevertheless, there are several advantages from this research. The data from the whole Sardinia district have shown in HHM a low level of awareness about HCWs vaccination. Furthermore, we have highlighted some critical aspects that can be considered by the local policy- makers to organize tailored preventive interventions. We, thus, emphasize the strong need to implement information programs addressed to HCWs about vaccinationpreventable diseases for potentially spreading in hospital settings complying with a patient-centered care system.
Another key-point of our study is a pragmatic low-budget method to communicate with health managers; this method has allowed us to get a large amount of data in a small lapse of time, thus reducing costs. Finally, our study provides evidence for stimulating health managers of Sardinia about the need to identify HCWs susceptible to threats of some infectious diseases damaging the hospital setting. This step is essential to achieve preventive strategies aimed to guarantee the health of both patients and HCWs.
Acknowledgements
The study was supported by Department of Public Health, Clinical and Molecular Medicine – University of Cagliari (Italy). The authors declare that they have no competing interests. The authors would like to thank Hospital Health Managements and Occupational Physicians from Ospedale Civile Paolo Merlo, La Maddalena (OT), Ospedale Civile Paolo Dettori, Tempio, Ospedale Giovanni Paolo II, Olbia, Ospedale S.S. Annunziata Azienda Ospedaliero Universitaria, Sassari, Ospedale A. Segni and Ospedale Civile, Alghero, San Camillo, Sorgono (NU) Ospedale San Francesco, Nuoro, Ospedale Cesare Zonchello, Bosa (OR), Ospedale G.A. Mastino, Lanusei (OG), Ospedale Nostra Signora delle Mercede, Oristano, Ospedale San Martino, Ghilarza (OR), Ospedale Delogu, Isili (CA), Ospedale San Giuseppe, San Gavino Monreale (VS), Ospedale Nostra Signora di Bonaria, Ospedale CTO and Ospedale Santa Barbara, Iglesias, Ospedale Sirai, Carbonia, Ospedale San Marcellino, Muravera (CA), Ospedale Roberto Binaghi, Ospedale Marino, Ospedale SS. Trinità, Ospedale Businco, Ospedale Microcitemico, Azienda Ospedaliera Brotzu, Azienda Ospedaliero Universitaria di Cagliari, Cagliari.
Footnotes
The authors declared that no competing interests exist.
Funding: none.
References
- 1. Centers for Disease Control and Prevention , author. Immunization of health care workers. Immunization of Health Care Personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recommendations and Reports. 2011/60(RR07) :1–45. [PubMed] [Google Scholar]
- 2.Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine. 2014;32:4876–4880. doi: 10.1016/j.vaccine.2013.10.046. [DOI] [PubMed] [Google Scholar]
- 3.Maltezou HC, Wicker S, Borg M, Heininger U, Puro V, Theodoridou M, Poland GA. Vaccination policies for health care workers in acute health care facilities in Europe. Vaccine. 2011;29:9557–9562. doi: 10.1016/j.vaccine.2011.09.076. [DOI] [PubMed] [Google Scholar]
- 4.Poland GA, Jacobson RM. The age-old struggle against the antivaccinationists. New Engl J Med. 2011;364:97–99. doi: 10.1056/NEJMp1010594. [DOI] [PubMed] [Google Scholar]
- 5.Trevisan A, Frasson C, Morandin M, Beggio M, Bruno A, Davanzo E, Marco L, Simioni L, Amato G. Immunity against infectious diseases: a predictive value of self-reported history of vaccination and disease. Infect Control Hosp Epidemiol. 2007;28:564–569. doi: 10.1086/516657. [DOI] [PubMed] [Google Scholar]
- 6.Piano Nazionale Prevenzione Vaccinale (PNPV) 2012-2014. Ministero della Salute. pp. 24–25.
- 7.Dinelli MI, Moreira Td, Paulino ER, Rocha MC, Graciani FB, Moraes-Pinto MI. Immune status and risk perception of acquisition of vaccine preventable diseases among health care workers. Am J Infect Control. 2009;37:858–860. doi: 10.1016/j.ajic.2009.04.283. [DOI] [PubMed] [Google Scholar]
- 8.Bolyard EA, Tablan OC, Williams WW, Pearson ML, Shapiro CN, Deitchman SD. Hospital Infection Control Practices Advisory Committee (HICPAC). Guideline for infection control in healthcare personnel, 1998. Infect Control Hosp Epidemiol. 1998;19:407–463. doi: 10.1086/647840. [DOI] [PubMed] [Google Scholar]
- 9.Maltezou HC, Katerelos P, Poufta S, Pavli A, Maragos A, Theodoridou M. Attitudes toward mandatory occupational vaccinations and vaccination coverage against vaccine-preventable diseases of health care workers in primary health care centers. Am J Infect Control. 2013;41:66–70. doi: 10.1016/j.ajic.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 10.Piano Nazionale della Prevenzione 2014-2018. Ministero della Salute. pp. 61–65.
- 11. Summary of WHO Position Paper – Immunization of Health Care Workers. Updated 30th May 2014.
- 12.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals A review of studies on attitudes and predictors. Vaccine. 2009;27:3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 13.Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34:142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 14.Quan K, Tehrani DM, Dickey L, Spiritus E, Hizon D, Heck K, Samuelson P, Kornhauser E, Zeitany R, Mancia S, et al. Voluntary to mandatory: evolution of strategies and attitudes toward influenza vaccination of healthcare personnel. Infect Control Hosp Epidemiol. 2012;33:63–70. doi: 10.1086/663210. [DOI] [PubMed] [Google Scholar]
- 15.Helms C, Polgreen P, Polgreen L, Evans T, Roberts LL, Clabaugh G, Quinlisk P. Voluntary reporting of employee influenza vaccination rates by acute care hospitals in Iowa: the impact of a four year provider-based statewide performance improvement project. Vaccine. 2011;29:3483–3488. doi: 10.1016/j.vaccine.2011.02.056. [DOI] [PubMed] [Google Scholar]
- 16.Sawyer MH, Peddecord KM, Wang W, Deguire M, Miskewitch-Dzulynsky M, Vuong DD. A public health initiative to increase annual influenza immunization among hospital health care personnel: the San Diego Hospital Influenza Immunization Partnership. Am J Infect Control. 2012;40:595–600. doi: 10.1016/j.ajic.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Cadena J, Prigmore T, Bowling J, Ayala BA, Kirkman L, Parekh A, Scepanski T, Patterson JE. Improving influenza vaccination of healthcare workers by means of quality improvement tools. Infect Control Hosp Epidemiol. 2011;32:616–618. doi: 10.1086/660198. [DOI] [PubMed] [Google Scholar]
- 18.Wicker S, Rabenau HF, Doerr HW, Allwinn R. Influenza vaccination compliance among health care workers in a German University Hospital. Infection. 2009;37:197–202. doi: 10.1007/s15010-008-8200-2. [DOI] [PubMed] [Google Scholar]
- 19.Jiménez-García R, Hernández-Barrera V, Carrasco-Garrido P, López de Andrés A, Pérez N, Miguel AG. Influenza vaccination coverage among children, adults, health care workers and immigrants in Spain: related factors and trends, 2003-2006. J Infect. 2008;57:472–480. doi: 10.1016/j.jinf.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Placidi D, Bacis M, Belotti L, Biggi N, Carrer P, Cologni L, Gattini V, Lodi V, Magnavita N, Micheloni G, et al. La tubercolosi. Focus sulla valutazione del rischio e la sorveglianza sanitaria dei lavoratori della sanit�: risultati e prospettive di un gruppo di lavoro multicentrico. G Ital Med Lav Erg. 2010;32:273–281. [PubMed] [Google Scholar]
- 21.Barbadoro P, Marigliano A, Tondo E, Chiatti C, Stanislao F, D'Errico MM, Prospero E. Determinants of influenza vaccination uptake among Italian healthcare workers. Hum Vaccin Immunother. 2013;9:911–916. doi: 10.4161/hv.22997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Istituto superiore di Sanità. Vaccinazione antinfluenzale: stagione 2012-2013. Coperture vaccinali per 100 abitanti. Ministero della Salute, 2013.
- 23.Nowalk MP, Lin CJ, Raymund M, Bialor J, Zimmerman RK. Impact of hospital policies on health care workers' influenza vaccination rates. Am J Infect Control. 2013;41:697–701. doi: 10.1016/j.ajic.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Gazmararian JA, Coleman M, Prill M, Hinman AR, Ribner BS, Washington ML, Janssen A, Orenstein WA. Influenza vaccination of health care workers: policies and practices of hospitals in a community setting. Am J Infect Control. 2007;35:441–447. doi: 10.1016/j.ajic.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Talbot TR, Dellit TH, Hebden J, Sama D, Cuny J. Factors associated with increased healthcare worker influenza vaccination rates: results from a national survey of university hospitals and medical centers. Infect Control Hosp Epidemiol. 2010;31:456–462. doi: 10.1086/651666. [DOI] [PubMed] [Google Scholar]
- 26.Alicino C, Iudici R, Barberis I, Paganino C, Cacciani R, Zacconi M, Battistini A, Bellina D, Bella AM, Talamini A, et al. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother. 2015;11:95–100. doi: 10.4161/hv.34362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Immunization of Health-Care Workers: Recommendation of advisory committee on immunization practice (ACIP) and the Hospital Infection Control Practice Advisory committee (HICPAC). MMWR, Recommendation and report 26;12/26/97. [PubMed]
- 28.Byrd KK1, Lu PJ, Murphy TV. Hepatitis B vaccination coverage among health-care personnel in the United States. Public Health Rep. 2013;128:498–509. doi: 10.1177/003335491312800609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vranckx R, Jacques P, Schrijver A, Moens G. Hepatitis B vaccination coverage in Belgian health care workers. Infection. 2004;32:278–281. doi: 10.1007/s15010-004-2204-3. [DOI] [PubMed] [Google Scholar]
- 30.Sukriti, Pati NT, Sethi A, Agrawal K, Agrawal K, Kumar GT, Kumar M, Kaanan AT, Sarin SK. Low levels of awareness, vaccine coverage, and the need for boosters among health care workers in tertiary care hospitals in India. J Gastroenterol Hepatol. 2008;23:1710–1715. doi: 10.1111/j.1440-1746.2008.05483.x. [DOI] [PubMed] [Google Scholar]
- 31.Djeriri K, Laurichesse H, Merle JL, Charof R, Abouyoub A, Fontana L, Benchemsi N, Elharti E, Aouad R, Chamoux A, et al. Hepatitis B in Moroccan health care workers. Occup Med (Lond) 2008;58:419–424. doi: 10.1093/occmed/kqn071. [DOI] [PubMed] [Google Scholar]
- 32.Mele A, Stroffolini T, Zanetti AR. Hepatitis B in Italy: where we are ten years after the introduction of mass vaccination. J Med Virol. 2002;67:440–443. doi: 10.1002/jmv.10092. [DOI] [PubMed] [Google Scholar]
- 33.Zanetti AR, Mariano A, Romanò L, D'Amelio R, Chironna M, Coppola RC, Cuccia M, Mangione R, Marrone F, Negrone FS, et al. Study Group, author. Long-term immunogenicity of hepatitis B vaccination and policy for booster: an Italian multicentre study. Lancet. 2005;366:1379–1384. doi: 10.1016/S0140-6736(05)67568-X. [DOI] [PubMed] [Google Scholar]
- 34.Campagna M, Siddu A, Meloni A, Murru C, Masia G, Coppola RC. Epidemiological impact of mandatory vaccination against hepatitis B in Italian young adults. Hepat Mon. 2011;11:750–752. doi: 10.5812/kowsar.1735143X.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coppola RC, Meloni A, Campagna M. Impact of universal vaccination against hepatitis B: the Italian model. Hepat Mon. 2012;12:417–419. doi: 10.5812/hepatmon.6396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spada E, Romanò L, Tosti ME, Zuccaro O, Paladini S, Chironna M, Coppola RC, Cuccia M, Mangione R, Marrone F, et al. Study Group, author. Hepatitis B immunity in teenagers vaccinated as infants: an Italian 17-year follow-up study. Clin Microbiol Infect. 2014;20:680–686. doi: 10.1111/1469-0691.12591. [DOI] [PubMed] [Google Scholar]
- 37.Carrer P, Micheloni G, Campagna M, Bacis M, Belotti L, Biggi N, Cologni L, Gattini V, Fostinelli J, Lodi V, et al. Focus sulla sorveglianza sanitaria dei lavoratori della sanità esposti ad agenti biologici trasmissibili per via ematogena: risultati e prospettive di un gruppo di lavoro multicentrico. G Ital Med Lav Erg. 2010;32:249–255. 3. [PubMed] [Google Scholar]
- 38.Campagna M, Bacis M, Belotti L, Biggi N, Carrer P, Cologni L, Gattinis V, Lodi V, Magnavita N, Micheloni G, et al. Exanthemic diseases (measles, chickenpox, rubella and parotitis). Focus on screening and health surveillance of health workers: results and perspectives of a multicenter working group. G Ital Med Lav Ergon. 2010;32:298–303. [PubMed] [Google Scholar]
- 39.Porru S, Campagna M, Arici C, Carta A, Placidi D, Crotti A, Parrinello G, Alessio L. Susceptibility to varicella-zoster, measles, rosacea and mumps among health care workers in a Northern Italy hospital. G Ital Med Lav Ergon. 2007;29(Suppl 3):407–409. [PubMed] [Google Scholar]
- 40. Centers for Disease Control and Prevention , author. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities, 1994. MMWR Recomm Rep. 1994;43:1–132. [PubMed] [Google Scholar]
- 41.Alvarez-León EE, Espinosa-Vega E, Santana-Rodríguez E, Molina-Cabrillana JM, Pérez-Arellano JL, Caminero JA, Serrano-Aguilar P. Screening for Tuberculosis Infection in Spanish Healthcare Workers: Comparison of the QuantiFERON-TB Gold In-Tube Test with the Tuberculin Skin Test. Infect Control Hosp Epidemiol. 2009;30:876–883. doi: 10.1086/598519. [DOI] [PubMed] [Google Scholar]
- 42. Centre for Disease Control and Prevention , author. Guidelines for Using the QuantiFERON®-TB Gold Test for Detecting Mycobacterium tuberculosis Infection, United States. MMWR Recommendation and Reports. 2005;54(RR15):49–55. [PubMed] [Google Scholar]
- 43.Vinton P, Mihrshahi S, Johnson P, Jenkin GA, Jolley D, Biggs BA. Comparison of QuantiFERON-TB Gold In-Tube Test and tuberculin skin test for identification of latent Mycobacterium tuberculosis infection in healthcare staff and association between positive test results and known risk factors for infection. Infect Control Hosp Epidemiol. 2009;30:215–221. doi: 10.1086/595695. [DOI] [PubMed] [Google Scholar]