Abstract
Background
The aim of this study was to improve the accuracy of guidewire insertion in the femoral neck fracture surgery using cannulated screw fixation.
Material/Methods
A novel aiming device was designed and manufactured. Between January 2010 and June 2012, 64 femoral neck fracture patients were included into the study. All 64 patients were divided into 2 groups randomly. The aiming device was used during the operation for patients in the experimental group, but not in the control group.
Results
There were no statistically significant differences in operative time or bleed volume between the groups (P>0.05). The frequency of guidewire drilling was significantly lower in the experimental group than in the control group (P<0.05). The angle between the first cannulated screw and the central axis of the femoral neck in coronal plane and sagittal plane, and the distance between the bottom cannulated screw and the medial calcar femorale rim, were significantly smaller in the experimental group than in the control group (P<0.05).
Conclusions
The aiming device is simple in structure and easy to use. It could help surgeons to accurately insert cannulated screw guidewires. The aiming device is suitable for broad clinical use.
MeSH Keywords: Bone Screws; Femoral Neck Fractures; Fracture Fixation, Internal; Surgical Instruments
Background
Femoral neck fractures are common in the field of orthopedic trauma, costing over $12 billion dollars annually in United States[1]. For young patients and elderly patients with undisplaced fractures, the goal of treatment is to achieve union with the preservation for femoral head [2]. Therefore, it is generally accepted that closed reduction and internal fixation may be the ideal management for these patients [3–5]. Several internal fixation devices have been described in the past, among which cannulated screws is the most common [6–8].
However, various complications, including osteonecrosis of the femoral head, nonunion, and fixation failure, frequently accompany cannulated screw fixation [9]. Anatomical reduction and stable fixation are known to be paramount for a good outcome [2]. With regard to cannulated screw fixation, appropriate cannulated screw placement is one of the most important factors in achieving good fixation quality [10–12]. Thus, appropriate placement of the guidewire is crucial. However, to date, surgeons mainly rely on their experience to insert cannulated screw guidewires, which is considered to be more of an arbitrary decision.
Therefore, we designed a guidewire aiming device to assist surgeons in inserting cannulated screw guidewires accurately in femoral neck fracture surgery. The purpose of the present study was to evaluate the efficacy of this novel device.
Material and Methods
Patients
The protocol of this trial and CONSORT checklist are available as supporting information (see S1 Protocol and S1 CONSORT Checklist). Potential trial participants with femoral neck fracture were recruited between January 2010 and June 2012 from the Shanghai Sixth People’s Hospital. All patients who were to be treated surgically with closed reduction and internal fixation with 3 cannulated screws (Depuy, Depuy, and Synthesis, Warsaw, Indiana, USA) were considered for inclusion in this trial. The exclusion criteria were: age over 60 years, pathological fractures, Garden type IV femoral neck fractures, an injury-to-surgery interval longer than 72 h, and rheumatoid arthritis or osteoarthritis. Sixty-four patients with a mean age of 42.44±9.12 years (range, 19 to 60 years) were included in the study. Thirty-nine patients were male, and 25 patients were female. Five fractures were classified as Garden type I, 35 as Garden type II, and 24 as Garden type III. The mean injury-to-surgery interval was 39.42±11.18 h (range, 9 to 64 h). The patients were divided randomly into the novel device group and the conventional technique group. All operative procedures were performed by 2 senior orthopedic surgeons. Each participant had a follow-up period of at least 1 year to assess the fracture healing. Patients were followed-up clinically and radiologically at 1, 3, 6, 9, and 12 months postoperatively.
Structure of the device
The guidewire aiming device consists of 4 components: an aiming component, an adjusting component, a locking component, and a fastening component (Figure 1). The aiming component consists of 1 interior sleeve and 1 exterior sleeve. The exterior sleeve is welded onto 1 side of the adjusting component. The interior sleeve can be inserted into the incision through the exterior sleeve serves as the marker for fluoroscopic imaging intraoperatively. The adjusting component consists of 1 direction-adjusting ball, 1 position-adjusting hinge, and 1 position-adjusting rod. The direction-adjusting ball can rotate in the cotyle 3-dimensionally and adjust the direction of the exterior sleeve. The direction of exterior sleeve can be adjusted according to the collodiaphyseal angle and the anteverted angle of the femoral neck. The position-adjusting hinge can rotate on the sagittal plane and adjust the anteroposterior position of the interior sleeve tip. The position adjusting rod can slide proximodistally and adjust the proximodistal position of the interior sleeve tip. The locking component consists of a large T-shaped bolt and small T-shaped bolt 1. The former bolt is used to lock the direction-adjusting ball and the position-adjusting hinge, while the latter is used to lock the position-adjusting rod. The fastening component consists of 2 splints and small T-shaped bolt 2, which are used to fasten the whole device onto the femoral shaft.
Figure 1.
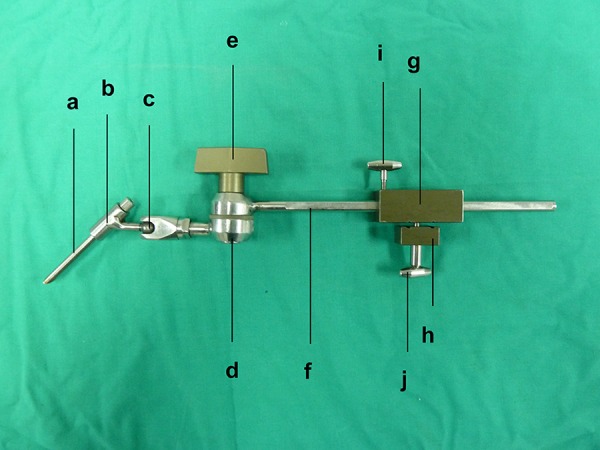
Picture of the guidewire aiming device: (a) interior sleeve; (b) exterior sleeve; (c) ball and socket joint; (d) hinge joint; (e) large T-shaped bolt; (f) rod; (g) large splint; (h) small splint; (i) small T-shaped bolt 1; (j) small T-shaped bolt 2.
Surgical procedures
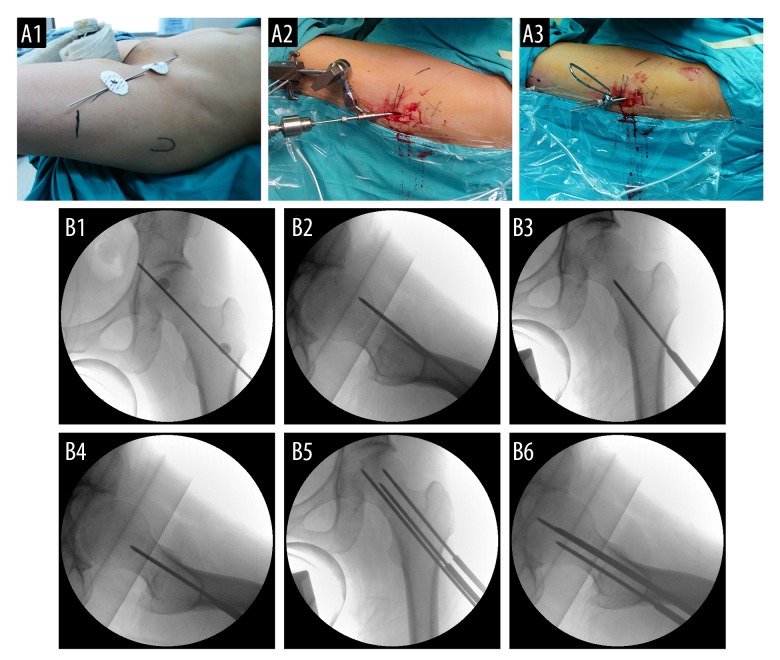
After general anesthesia, closed reduction was performed by traction bed and confirmed by fluoroscopic imaging. A Kirschner wire was placed on the front of hip and located at the central axis of the femoral neck in anteroposterior fluoroscopy image (Figure 2A1, 2B1). Lines were marked on the skin for locating. With general sterilization and draping, a 3-cm straight lateral incision was made over the proximal-lateral part of the femur, and a Kirschner wire was inserted along the anterior cortex of femoral neck through the incision manually. Fluoroscopic imaging was performed to ensure that the Kirschner wire was parallel to the central axis of the femoral neck on anteroposterior imaging and lay immediately anterior to the cortex of the femoral neck on lateral imaging (Figure 2B2). The Kirschner wire can then visually present the collodiaphyseal angle and the anteverted angle of the femoral neck.
Figure 2.
Pictures and radiographs showing appliance of the aiming device in femoral neck fracture (A1); Placement of the Kirschner wire for locating; (A2) Insert the first guidewire into femoral neck through the interior sleeve of the aiming device; (A3) Insert the rest of the guidewires into the femoral neck by parallel aiming device; (B1) Anteroposterior plain radiograph of the Kirschner wire placed on the front of hip for locating; (B2) Lateral plain radiograph of the Kirschner wire inserted to the front of the femoral neck; (B3) Anteroposterior plain radiograph of the first guidewire inserted into the femoral neck through the interior sleeve of the aiming device; (B4) Lateral plain radiograph of the first guidewire inserted into femoral neck through the interior sleeve of the aiming device; (B5) Anteroposterior plain radiograph of the other guidewires inserted into the femoral neck by parallel aiming device; (B6) Lateral plain radiograph of the other guidewires inserted into the femoral neck by parallel aiming device.
For patients in the novel device group, 2 Steinmann wires were laterally drilled into the femoral shaft through the fastening component, and small T-shaped bolt 2 was locked to fasten the device onto the femoral shaft. Then, an appropriate interior sleeve was inserted into the incision through the exterior sleeve. As the guidewire would be inserted into the femoral neck through the interior sleeve, the interior sleeve acts as the marker determining the entry point and direction for the guidewire. Next, we adjusted the position and the direction of the interior sleeve according to the Kirschner wire placed before, and locked the small T-shaped bolt 1 and the large T blot to fixate the interior sleeve securely (Figuere 2A2). Fluoroscopic imaging was used to ensure the appropriate position and direction of the interior sleeve. Then, the first guidewire was inserted as a reference guidewire through the interior sleeve into the femoral neck (Figure 2B3, 2B4). The Kirschner wire and the device were then removed, and the parallel aiming device in DePuy suitcase was applied to help inserting the other 2 guidewires according to the first guidewire (Figure 2A3). Fluoroscopic imaging was utilized to confirm the appropriate position and depth of the guidewires (Figure 2B5, 2B6). Next, 3 cannulated screws were implanted along the guidewires. The fixation was ensured by fluoroscopic imaging.
For patients in the conventional technique group, operations were performed as usual. Generally, surgeons inserted the first guidewire into the femoral neck according to the Kirschner wire, relying on their experience. Then, fluoroscopic imaging was used to check the direction and position of the guidewire. If the direction or position was not appropriate, partial or total removal of the inserted guidewire may be required to make adjustment. When the appropriate direction and position of the first guidewire was obtained, the subsequent procedure was performed the same as in the novel device group.
Outcome evaluation
Operative time and intraoperative blood loss were recorded during each operation to evaluate the efficacy of the novel device. Operative time referred to the total duration from the incision-making to closing. Intraoperative blood loss referred to the total volume of the blood loss during the operation.
To evaluate the accuracy of the guidewire insertion, the frequency of drilling attempts was recorded during each operation, and, the direction and position of the cannulated screws were measured on the postoperative radiographs. The frequency of drilling attempts refers to the total drilling times of the first guidewire. The insertion of the guiding Kirchner wire, which was placed along but not into the femoral neck cortex, was not included in the frequency. The fixation direction was evaluated by measuring the angles between the first cannulated screw and the central axis of the femoral neck on anteroposterior and lateral view radiographs. Generally, the guidewires were in an inverted triangle configuration with 1 guidewire inserted close to the calcar femorale to ensure the stability of the fixation. The fixation position was evaluated by measuring the distance between the medial calcar femorale rim and the bottom cannulated screw on anteroposterior view radiographs.
Ethics statement
All the procedures in this study were approved by the Ethics Committee of Shanghai Sixth People’s Hospital. The trial was registered in ChiCTR (trial registration number ChiCTR-ICR-15007334). The authors confirm that all ongoing and related trials for this intervention are registered. Patient selection was performed upon admission, and written informed consent was obtained from all individuals included in this study. The study conforms to the CONSORT statement (www.consort-statement.org).
Statistical analysis
Data were analyzed using the IBM SPSS Statistics Version 22.0 (SPSS Inc., Chicago, Illinois, USA). Data are presented as mean ± standard deviation or numbers, as appropriate. The independent-samples Students’ t-test was performed to analyze continuous data. Sex and fracture types were analyzed using the chi-squared test. The total frequency of guidewire drilling was analyzed using the Mann-Whitney U test. P value less than 0.05 was considered statistically significant.
Results
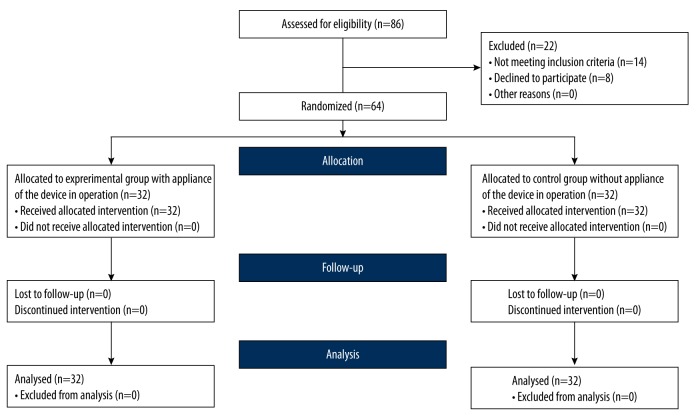
Between January 2010 and June 2012, 86 patients with femoral neck fracture were considered to be included in this trial. Of these, 14 were found to not fulfil the inclusion criteria, and 8 declined to participate in the trial (Figure 3). Sixty-four eligible patients were randomized to the 2 groups.
Figure 3.
CONSORT flow diagram. The flow diagram displays the progress of all participants through the trial.
General information of patients in the novel device group and the conventional technique group is provided in Table 1. There was no statistically significant difference of age, sex, fracture patterns, or interval from injury to surgery between the groups.
Table 1.
General information of the patients treated by both groups.
| The novel device group | The conventional technique group | p value | |
|---|---|---|---|
| Age (years, mean ±SD) | 40.81±10.15 | 44.06±7.77 | 0.155 |
| Sex (male: female) | 20:12 | 19:13 | 0.799 |
| Fracture patterns (Garden type I:II:III) | 3:16:13 | 2:19:11 | 0.767 |
| Injury-to-surgery interval (hours, mean ±SD) | 37.00±10.66 | 41.84±11.33 | 0.083 |
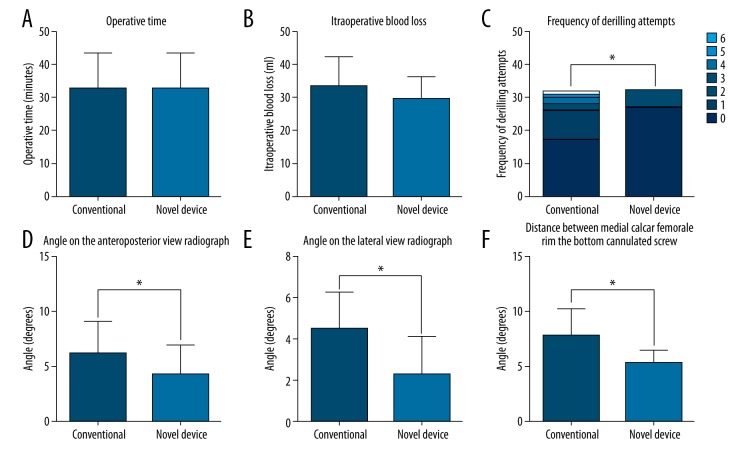
The mean operative time was 32.78±10.58 min in the conventional technique group and 31.81±11.23 min in the novel device group (Figure 4A). The mean intraoperative blood loss was 33.28±8.85 mL in the conventional technique group and 29.63±6.54 mL in the novel device group (Figure 4B). Application of the novel device did not influence the operative time or intraoperative blood loss (P=0.724 and 0.065, respectively).
Figure 4.
Outcome measurement for participants in the Experimental group and Control group. * p<0.05 between the 2 groups.
In the conventional technique group, the frequency of drilling attempts was 1 time in 17 patients (53.13%), 2 times in 9 patients (28.13%), 3 times in 2 patients (6.25%), 4 times in 2 patients (6.25%), 5 times in 1 patient (3.13%), and 6 times in 1 patient (3.13%). In the novel device group, the frequency of drilling attempts was 1 time in 27 patients (84.38%) and 2 times in 5 patients (15.63%). The novel device reduced the frequency of drilling attempts significantly (P=0.004, Figure 4C). The mean angle between the first cannulated screw and the central axis of the femoral neck on the anteroposterior view radiographs was 6.14±2.99 degrees in the conventional technique group and 4.30±2.62 degrees in the novel device group (Figure 4D). The mean angle between the first cannulated screw and the central axis of the femoral neck on the lateral view radiographs was 4.49±1.79 degrees in the conventional technique group and 2.88±1.23 degrees in the novel device group (Figure 4E). The mean distance between medial calcar femorale rim and the bottom cannulated screw was 7.76±2.50 mm in the conventional technique group and 5.35±1.13 mm in the novel device group (Figure 4F). The differences in angles and distance between the groups were significant (P=0.011, P<0.001, P<0.001, respectively). The patients in both groups all successfully obtained fracture union during 1-year follow-up.
Discussion
Appropriate placement of guidewires is crucial for treating femoral neck fractures with cannulated screws. However, it is not easy to insert the guidewire at the right position and drill straight along in the right direction. When the position or the direction of a guidewire is unsatisfactory, multiple drilling attempts may be required to make adjustment. However, it is not easy for surgeons to make accurate adjustment for the guidewire. When encountering the drilling track, the guidewire may possibly slide along it, which would make a failed adjustment. In addition, repeated drillings might weaken the bone and even lead to subtrochanteric fractures [13]. Therefore, numerous surgical techniques have been introduced to aid in accurate guidewire insertion. Tai et al. demonstrated that using a cannulated screw as the drill guide and sleeve was time-saving and easy to perform [14]. However, the guiding cannulated screw could not be fixated securely. Therefore, appropriate position and direction of the guidewire could not be guaranteed. Computer-assisted navigation system is another technique applied in the field of orthopedic surgery. It is believed to have the potential to improve the precision of guidewire insertion. However, previous studies demonstrated that the navigation system increases the radiation and operative time [15–19]. Additionally, the navigation system is expensive and complicated. The cost of purchasing of the system and the training of a skilled manipulator would further increase the cost to patients.
Our novel aiming device has the following advantages in design: Firstly, the position-adjusting part is highly adjustable for the aiming component in proximodistal and anteroposterior position, and the direction-adjusting part can freely rotate to adjust the aiming component according to the collodiaphyseal angle and anteverted angle. Secondly, the aiming component can be easily locked by a small bolt when appropriate position and direction are obtained. Thirdly, the structure and mechanism of the device make it simple and easy to use.
In clinical practice, we found that our aiming device assists in improving operation quality and reducing intraoperative injury. In fact, the pre-located Kirschner wire allows the initial judgment for the surgeons about the entry points, collodiaphyseal angle, and anteverted angle, which increases the accuracy of guidewire drilling. This method is seemingly credible, but in practice the surgeon still cannot appropriately drill the first guidewire because there may be errors in judging the position and direction. Our aiming device, shown in fluoroscopy, was marked by the interior sleeve, which was displayed together with the femoral head and femoral neck in the same view. For aiming the device, the tip of the interior sleeve was considered as the entry point and the extended axis of the interior sleeve as the entry path. By making adjustments of the interior sleeve corresponding to collodiaphyseal angle and anteverted angle, the position and direction of the first guidewire can be assured. An appropriate first guidewire insertion can lay a good foundation for the second and third guidewires to enhance the fixation quality. In this study, the angle between the first cannulated screw and the femoral neck axis in both coronal plane and sagittal plane, and the distance between the bottom cannulated screw and the medial calcar femorale rim, were all significantly different between the novel device group and the conventional technique group (P<0.05). These results indicate that the accuracy of guidewire inserting was enhanced by the novel aiming device. In addition, the aiming device reduces the frequency of guidewire drilling because it can accurately adjust the position and direction before drilling attempts. The frequency of guidewire drilling was significantly different in both groups (P<0.05). Although the 2 Steinmann wires drilled into the femur increase additional injury, no significant difference was found regarding intraoperative blood loss between the groups (P>0.05). This indicates that use of this aiming device did not cause more bleeding during the operation. Moreover, sutures for the small incisions made for Steinmann wires were not required, and the incisions heal soon with only a slight scar.
Since more surgical procedures were added in the novel device group, the operative time might have been extended. But the result shows that there was no significant difference in operative time between the groups (P>0.05). Despite the added procedures, the aiming device effectively avoids invalid drilling. That may be the reason why it does not extend the operative time.
This device could help to improve operation quality and lead to less injury. However, to further raise the efficiency, the surgeons should master a few skills to better apply this technique. Firstly, the line labeled on the anterior hip joint should be exposed during draping. Care must be taken to avoid over-stretching the skin in film dressing. These details could ensure the accurate location of the Kirschner wire inserted into the anterior of femoral neck. Secondly, the incision should be located approximately 1.5 cm posterior to the lateral thigh axis. If the incision is made more to the front, the sleeve placement and guidewire insertion tend to be quite difficult due to greater uplifting tension from the posterior soft tissues. If the incision is positioned over-posteriorly, using the placed Kirschner wire as a locator is even harder because the pressure pushing down from the fascia lata and soft tissue tend to be greater. Thirdly, the strength-compressing order of cannulated screws has nothing to do with the guidewire insertion order. The order of cannulated screws mainly depends on the fracture situation.
Conclusions
We developed a novel guidewire aiming device to assist surgeons in inserting cannulated screw guidewires accurately in femoral neck fracture operations. The aiming device possesses advantages of simple structure and flexible use. The results demonstrate that this novel device can enhance the accuracy of inserting cannulated screw guidewires, without increasing operative time and iatrogenic injury. Therefore, the aiming device is suitable for clinical application and deserves to be generalized.
Acknowledgements
We would like to acknowledge the contribution of the Shanghai Libang Medical Equipment Co. for the manufacture of instruments used in this study.
Footnotes
Source of support: This work was funded by Shanghai Municipal Commission of Health and Family Planning (Grant No. 2007040)
References
- 1.Dy CJ, McCollister KE, Lubarsky DA, Lane JM. An economic evaluation of a systems-based strategy to expedite surgical treatment of hip fractures. J Bone Joint Surg Am. 2011;93(14):1326–34. doi: 10.2106/JBJS.I.01132. [DOI] [PubMed] [Google Scholar]
- 2.Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am. 2008;90(10):2254–66. [PubMed] [Google Scholar]
- 3.Parker MJ. The management of intracapsular fractures of the proximal femur. J Bone Joint Surg Br. 2000;82(7):937–41. doi: 10.1302/0301-620x.82b7.11595. [DOI] [PubMed] [Google Scholar]
- 4.Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236–42. doi: 10.1097/TA.0b013e3181c428ce. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein J, Ahn J. In brief: fractures in brief: femoral neck fractures. Clin Orthop Relat Res. 2010;468(6):1713–15. doi: 10.1007/s11999-010-1295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seyfettinoglu F, Ersan O, Kovalak E, et al. Fixation of femoral neck fractures with three screws: results and complications. Acta Orthop Traumatol Turc. 2011;45(1):6–13. doi: 10.3944/AOTT.2011.2434. [DOI] [PubMed] [Google Scholar]
- 7.Huang HK, Su YP, Chen CM, et al. Displaced femoral neck fractures in young adults treated with closed reduction and internal fixation. Orthopedics. 2010;33(12):873. doi: 10.3928/01477447-20101021-15. [DOI] [PubMed] [Google Scholar]
- 8.Haidukewych GJ, Rothwell WS, Jacofsky DJ, et al. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004;86-A(8):1711–16. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A(9):1673–81. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Selvan VT, Oakley MJ, Rangan A, Al-Lami MK. Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: a biomechanical study. Injury. 2004;35(2):136–41. doi: 10.1016/s0020-1383(03)00059-7. [DOI] [PubMed] [Google Scholar]
- 11.Wu CC. Using biomechanics to improve the surgical technique for internal fixation of intracapsular femoral neck fractures. Chang Gung Med J. 2010;33(3):241–51. [PubMed] [Google Scholar]
- 12.Zdero R, Keast-Butler O, Schemitsch EH. A biomechanical comparison of two triple-screw methods for femoral neck fracture fixation in a synthetic bone model. J Trauma. 2010;69(6):1537–44. doi: 10.1097/TA.0b013e3181efb1d1. [DOI] [PubMed] [Google Scholar]
- 13.Lindequist S, Tornkvist H. Quality of reduction and cortical screw support in femoral neck fractures. An analysis of 72 fractures with a new computerized measuring method. J Orthop Trauma. 1995;9(3):215–21. doi: 10.1097/00005131-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Tai TW, Lien FC, Lee PY, et al. Using a cannulated screw as a drill guide and sleeve: A simple technique for multiple-screw fixation for intracapsular femoral neck fracture. Orthopedics. 2010;33(8) doi: 10.3928/01477447-20100625-05. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Yun C, Hu L, et al. DEA-based efficiency evaluation of a novel robotic system for femoral neck surgery. Int J Med Robot. 2009;5(2):207–12. doi: 10.1002/rcs.252. [DOI] [PubMed] [Google Scholar]
- 16.Muller MC, Belei P, De La Fuente M, et al. Evaluation of a fluoroscopy-based navigation system enabling a virtual radiation-free preview of X-ray images for placement of cannulated hip screws. A cadaver study. Comput Aided Surg. 2011;16(1):22–31. doi: 10.3109/10929088.2010.542694. [DOI] [PubMed] [Google Scholar]
- 17.Muller MC, Belei P, Pennekamp PH, et al. Three-dimensional computer-assisted navigation for the placement of cannulated hip screws. A pilot study. Int Orthop. 2012;36(7):1463–69. doi: 10.1007/s00264-012-1496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang JQ, Zhao CP, Su YG, et al. Computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures: a comparison of bi-planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin Med J. 2011;124(23):3906–11. [PubMed] [Google Scholar]
- 19.Nousiainen MT, Omoto DM, Zingg PO, Weil YA, et al. Training femoral neck screw insertion skills to surgical trainees: Computer-assisted surgery versus conventional fluoroscopic technique. J Orthop Trauma. 2013;27(2):87–92. doi: 10.1097/BOT.0b013e3182604b49. [DOI] [PubMed] [Google Scholar]