To the Editor—Barlam and colleagues recently published a comprehensive and evidence-based primer on implementing an antibiotic stewardship program [1]. We read with particular interest the section describing the limited role of education as an intervention to reduce inappropriate antibiotic use. Many of the interventions aimed at heath professionals have been time-limited and conducted via individual sessions. Although successful in the short term, they resulted in nonsustainable improvements in prescribing behaviors [2]. There has been increasing interest in targeting trainees before antibiotic prescribing behaviors become fixed [3]. However, few programs have been developed specifically for health profession learners [4]. Similar to more advanced practitioners, the few educational strategies that have been employed in these early learners have been limited to individual classes or modules. We describe below one approach to medical student education on antibiotic stewardship.
We developed a comprehensive learning experience throughout the second to fourth years of medical school. Our curriculum utilized the concept of spiral learning, where the same material or concept is revisited frequently, but with increasing complexity [5]. In spiral learning, previous learning is not only reinforced but also deepened, so that mastery is more efficiently obtained.
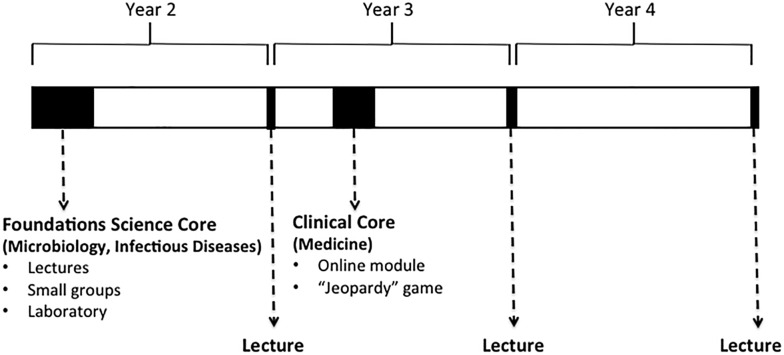
We initiated an antibiotic stewardship curriculum in 2013 at the University of California, San Francisco School of Medicine (Figure 1). The second year component included (1) purposeful integration of stewardship themes throughout the foundations science microbiology block (integrates microbiology, infectious diseases, and pharmacology), and (2) a 2-hour, interprofessional, case-based small group activity for medical and pharmacy students on antibiotic stewardship. During the third year of medical school we developed (1) an interactive case-based 1-hour didactic session emphasizing responsible antibiotic use immediately prior to start of clerkships, and (2) during the medicine clerkship, an online module on common infections and antimicrobial use, followed by an interactive “Jeopardy”-style chief resident–taught game. During the fourth year of medical school we delivered 2 sessions (2 hours and 1.5 hours) on common infections and responsible antimicrobial use immediately before the start of the fourth year and 1 week before graduation. We also developed and disseminated antibiotic cards for medical students to use on the wards starting in the third year.
Figure 1.
Mapping of a longitudinal medical school antimicrobial stewardship curriculum during a 4-year medical school.
We queried students about their attitudes regarding prescribing patterns and antibiotic stewardship. By the middle of second year, 99.6% believed that antibiotic resistance is a major public health problem, and that overprescribing of antibiotics is a major cause of antibiotic resistance. Prior to graduation, 88% felt at least moderately prepared to initiate empiric antibiotics and when and how to narrow the spectrum of coverage. Eighty-eight percent felt very or extremely satisfied with the education they received on antibiotic stewardship during medical school. We agree with Barlam and colleagues that didactic education cannot be used as a stand-alone intervention in antimicrobial stewardship programs [1], but argue that a multimodal and longitudinal approach could increase impact.
Educational strategies that incorporate spiral learning may enhance the role of education in stewardship. Methodical inclusion in a longitudinal undergraduate medical education curriculum should be linked to future activities proposed in graduate medical education and existing efforts that already target health professionals.
Notes
Disclaimer. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health (NIH).
Financial support. This work was supported by the Endowed Chair funds from the Academy of Medical Educators and from the Department of Medicine, University of California, San Francisco (UCSF). This project was also supported by the National Center for Advancing Translational Sciences (CTSI), NIH, through UCSF-CTSI grant number UL1 TR000004.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Barlam TF, Cosgrove SE, Abbo LM et al. . Executive summary: implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016; 62:1197–202. [DOI] [PubMed] [Google Scholar]
- 2.Landgren FT, Harvey KJ, Mashford ML, Moulds RF, Guthrie B, Hemming M. Changing antibiotic prescribing by educational marketing. Med J Aust 1988; 149:595–9. [DOI] [PubMed] [Google Scholar]
- 3.Abbo LM, Cosgrove SE, Pottinger PS et al. . Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis 2013; 57:631–8. [DOI] [PubMed] [Google Scholar]
- 4.Luther VP, Ohl CA, Hicks LA. Antimicrobial stewardship education for medical students. Clin Infect Dis 2013; 57:1366. [DOI] [PubMed] [Google Scholar]
- 5.Harden RM, Davis MH, Crosby JR. The new Dundee medical curriculum: a whole that is greater than the sum of the parts. Med Educ 1997; 31:264–71. [DOI] [PubMed] [Google Scholar]