Abstract
Toxoplasma gondii is a protozoan with worldwide distribution and in spite of increasing information about its biology, treatment of toxoplasmosis is restricted to a few drugs and unfortunately using of each of drugs is associated with significant side effects in patients. This study was designed to evaluate the efficacy of cromolyn sodium and ketotifen as alternative drugs for the treatment of toxoplasmosis. In vitro; in case group, concentrations of 1, 5, 10 and 15 µg/ml of ketotifen and cromolyn sodium were added to RPMI medium containing peritoneal macrophages. After 1 h incubation and adding tachyzoites to medium, efficacy rate of these drugs in entrance inhibition of Toxoplasma tachyzoites into macrophages were evaluated after 30 and 60 min. In vivo; case groups received ketotifen and cromolyn sodium with different concentrations at various times. Control groups received none of drugs. We found that in vitro; after 60 min the best efficacy of these drugs in inhibition of cell entrance of Toxoplasma was observed at 15 µg/ml (78.9 ± 1.70 and 91.97 ± 0.37 %, respectively) (P < 0.05). In vivo; after 60 min ketotifen at 2 mg/kg in 3 h before tachyzoite injection (69.83 ± 2.25 %), and cromolyn sodium, at 10 mg/kg in 6 h before tachyzoite injection (80.47 ± 2/49 %) had the best effect on inhibition of Toxoplasma entry into the cells (P < 0.05). Our findings show that ketotifen and cromolyn sodium are suitable drugs for entrance inhibition of tachyzoites into nucleated cells in vitro and in vivo.
Keywords: Toxoplasma gondii, Ketotifen, Cromolyn sodium, Entrance inhibition, Nucleated cells, Mouse
Introduction
Toxoplasmosis is a zoonotic disease caused by an obligate intracellular protozoan, Toxoplasma gondii (T. gondii). Human beings become infected with T. gondii mainly by ingesting contaminated undercooked meat, food or water (Ho-Yen and Joss 1992; Dubey 2008).
Toxoplasmosis is considered as an opportunistic infection with a worldwide distribution and is mainly subclinical in immunocompetent people. Nevertheless, in congenitally infected children and immunocompromised persons such as human immunodeficiency virus-infected individuals, organ transplant recipients and cancer patients, infection causes high rates of morbidity and mortality (Ambroise-Thomas and Pelloux 1993).
Treatment of toxoplasmosis in at risk individuals such as infants and immunocompromised patients because of the severity of drugs side effects and infection recurrent is difficult (Serranti et al. 2011). Clinical toxoplasmosis has been treated by blocking folate metabolism with a combination of antifolates (such as pyrimethamine) and sulfonamides. This strategy is highly effective in healthy individuals. In spite of increasing information about Toxoplasma biology, treatment of toxoplasmosis is restricted to a few drugs and unfortunately using of each of drugs is associated with significant side effects in patients (Araujo and Remington 1992; Petersen 2007; Iaccheri et al. 2008). Frequent development of allergic reactions to sulfonamides often precludes continuous administration of these drugs, and pyrimethamine alone is insufficient to prevent relapse (Araujo and Remington 1992; Van der Ven et al. 1996). Therefore, it seems that investigation on alternative drugs is necessary.
Research on drugs to inhibit T. gondii may reasonably include agents that affect the parasites complex cytoskeleton (Nichols and Chiappino 1987). This parasite is highly motile and actively invades host cells. Replication occurs by endodyogeny, a process needs the assembly of daughter parasites within a cytoskeletal framework inside the mother cell. The cytoskeleton probably plays an important role in motility, invasion, and endodyogeny (Morisaki et al. 1995). Disruption of any of these essential functions might be expected to kill or inhibit the parasite.
Penetration enhancing factor (PEF) after discharge from the Toxoplasma tachyzoite rhoptry, attached to surface of nucleated cells receptors, called actin, laminin and collagen. T. gondii enters host cells via endocytosis after binding to cell surface molecules. In most cells, microfilament structure is formed by actin polymers and myosin, and plays an important role in bringing micro pseudopods (Kasper and Mineo 1994; Weiss and Kim 2004). It is known that the cell membrane stabilizing drugs, change the resistance of the cell membrane with interference to microfilament functional and blocking the actin gel (Ryning and Remington 1978; D’Angelo et al. 2009). The goal of our study was to survey whether the drugs stabilizing cell membrane such as cromolyn sodium and ketotifen, are able to inhibit T. gondii pentrance into nucleated cells in vitro and in vivo.
Materials and methods
Toxoplasma tachyzoites
In vitro and in vivo studies were performed with the virulent RH strain of Toxoplasma which maintained in mice (6–8 weeks of age) by subsequent passage every 3–4 days. For each experiment, tachyzoites were harvested from the peritoneal cavities of infected mice using phosphate-buffered saline (PBS) supplemented with penicillin (100 U/ml), and streptomycin (100 µg/ml) (Dadimoghaddam et al. 2014).
Macrophage monolayer
For the preparation of peritoneal macrophages the sterile PBS (pH 7.2), injected into the peritoneal cavity of mice and then aspirated. Subsequently harvested macrophages (1 × 105/ml) were seeded in 24-well plates containing a glass cover slip. After plating and incubation at 37 °C for 1 h, non-adherent cells and the supernatants were removed. Then, for in vitro and in vivo assays, macrophages were incubated at 37 °C in a 5 % CO2 atmosphere for up to 24 h, in RPMI-1640 culture medium (Cortez et al. 2008).
In vitro studies
Ketotifen and cromolyn sodium were dissolved in PBS and used at the concentrations of 1, 5, 10 and 15 µg/ml. In case groups, before infection, monolayer macrophages in RPMI medium were incubated (1 h, at 37 °C) with various drug concentrations. After that, the wells of the plate were seeded with 4 × 105 tachyzoites and incubated for 30 and 60 min at 37 °C. Control group received only PBS and RPMI.
Thereafter, for evaluation of efficacy rate of different concentrations of drugs in entrance inhibition of Toxoplasma tachyzoites into macrophages in 30 and 60, the number of tachyzoites entrance into the macrophage cells was counted under a light microscope with Giemsa staining. Inhibition rate of tachyzoites entry into nucleated cells was obtained according to the following formula:
For each concentration of the drug, counting of tachyzoites was done in triplicate in random adjacent microscopic fields. The data were recorded and compared with the control group. The Mann–Whitney U test was used for statistical analysis.
In vivo studies
Inhibition activity of ketotifen and cromolyn sodium against tachyzoites entry was evaluated by intraperitoneal (i.p.) inoculation to Balb/c mice. Eight treatment groups were used for drugs: four groups of mice (n = 4) pretreated with ketotifen 1 and 2 mg/kg, i.p. at 30 and 60 min prior to exposure of tachyzoite, and four groups pretreated with cromolyn sodium 5 and 10 mg/kg, i.p. at 30 and 60 min prior to exposure of tachyzoite. The control group (n = 4) received only the tachyzoites in PBS.
Afterward, 4 × 105 tachyzoites were injected i.p. to mice, and after 60 min mice peritoneal exudates containing tachyzoites and nucleated cells were aspirated. Then entry inhibition evaluated under a light microscope with Giemsa staining. The project underwent ethical review and was given approval by the Ethics Committee of Mazandaran University of Medical Sciences.
Results
In vitro
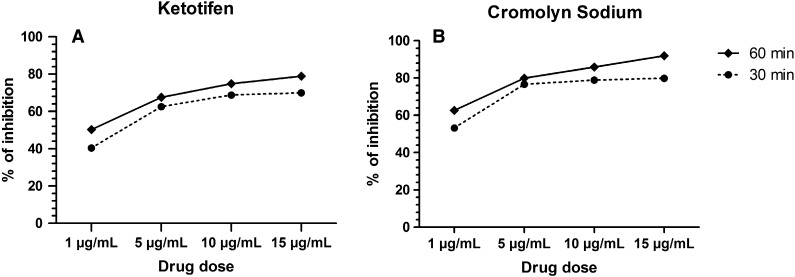
According to the in vitro experiments, different concentrations of ketotifen and cromolyn sodium at 30 and 60 min, showed a dose dependent inhibition of Toxoplasma entry into the cells (Fig. 1). So that after 30 min of ketotifen application, the highest entrance inhibition of Toxoplasma tachyzoites were seen at 10 and 15 µg/ml concentrations with an average 68.81 ± 1.08 and 69.92 ± 0.7 %, respectively. Due to the proximity effect of these doses, and no statistically significant difference (P > 0.05), lower drug concentration (10 µg/ml) is appropriate. After 60 min, the greatest amount of inhibition was observed at 15 µg/ml concentration (78.9 ± 1.70 %) (P < 0.05) (Fig. 1a).
Fig. 1.
Inhibition rate of different concentrations of ketotifen (a) and cromolyn sodium (b) in Toxoplasma gondii entrance into host cells after 30 and 60 min, in vitro
The consequences of the evaluation of cromolyn sodium, similar results were obtained. According to Fig. 1b, the mean inhibition of cromolyn sodium, increased with increasing concentration at both 30 and 60 min. So that at 30 min, the highest entry inhibition of Toxoplasma tachyzoites with an average 78.81 ± 2.06 and 79.91 ± 1.37 % was observed at 10 and 15 µg/ml concentrations of cromolyn sodium, respectively; with no statistically significant difference (P > 0.05); hence like ketotifen, lower drug concentration (10 µg/ml) is appropriate.
After 60 min, the highest amount of inhibition was seen at 15 µg/ml (91.97 ± 0.37 %) (P < 0.05).
In vivo
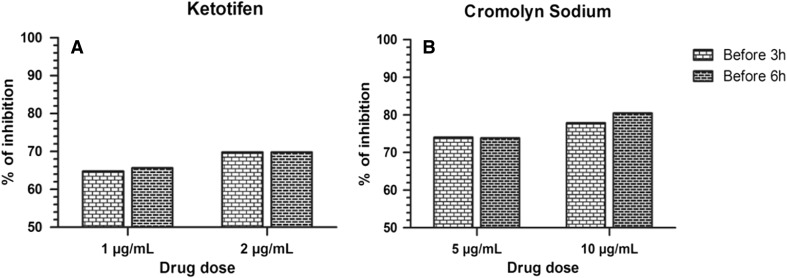
In this study, inhibitions of Toxoplasma tachyzoite entry into nucleated cells using ketotifen and cromolyn sodium were also examined in vivo. The effect of ketotifen on tachyzoite entry, at concentrations of 1 and 2 mg/kg at 6 and 3 h before tachyzoites injection and evaluation after 60 min showed with increasing concentration of ketotifen, the number of intracellular tachyzoites decreased (P < 0.05) (Fig. 2a).
Fig. 2.
Inhibition rate of different concentrations of ketotifen (a) and cromolyn sodium (b) in Toxoplasma gondii entrance into host cells at 6 and 3 h before tachyzoites injection, in vivo
According to Fig. 2b, the results of the in vivo study at 5 and 10 mg/kg concentrations of cromolyn sodium at 6 and 3 h before tachyzoites injection and their assessment after 60 min showed that the inhibitory effect was dose dependent and the best effect of inhibition of Toxoplasma tachyzoites entry into the cells was seen at concentration of 10 mg/kg of cromolyn sodium at 6 h before tachyzoite injection (80.47 ± 2.49) (P < 0.05).
Discussion
This survey was carried out to determine the effect rate of ketotifen and cromolyn sodium on entry inhibition of T. gondii into nucleated cells, in vitro and in vivo. It is taken to relieve a blocked or runny nose caused by allergic rhinitis. These drugs stabilize cell membrane and inhibit parasite entry into the host cells. In this study, ketotifen and cromolyn sodium in vitro (10 µg/ml) and in vivo (2 and 10 µg/ml, respectively) by stabilizing of cell membrane, showed the highest entrance inhibition of T. gondii into cells. When T. gondii enters both phagocytes and cells not generally considered phagocytic, micropseudopods are frequently seen partially enveloping this organism as it gains an intracellular position (Kasper and Mineo 1994; Morisaki et al. 1995). The importance of contractile proteins in the formation of these pseudopods and the interaction of their subunits results in actin filament gelation, which can be prevented by cromolyn sodium and ketotifen, support the hypothesis that microfilaments are the most likely subcellular site of cromolyn sodium and ketotifen action in the prevention of T. gondii entry. Cromolyn sodium and ketotifen might render the cell membrane resistant to the parasites efforts to gain an intracellular position. The cytoskeleton is suspected to play an important role in motility, invasion and endodyogeny (Morisaki et al. 1995). Thus, disruption in the mentioned functions may be effective in inhibition of parasite. Ryning and Remington (1978) have shown that cytochalasin D inhibits the entry of T. gondii into peritoneal macrophages and bladder tumor cells followed a dose related but did not prevent attachment. Microfilaments are likely candidates for this common site of action in preventing entry of T. gondii into cells. These sub cellular structures are contractile proteins composed of actin and myosin polymers, which are present in most mammalian cells (Clarke and Spudich 1977). The subunits of these proteins, namely, actin and actomyosin, appear to be the major binding sites for cytochalasin D (Ryning and Remington 1978).
Nam et al. (1993) showed that fetal bovine serum (FBS) factor inhibits the penetration of T. gondii into host cells. The FBS factors might participate to neutralize materials secreted or intervene between receptor-ligand binding through sterically rather than functionally. Stokkermans et al. (1996) have described that dinitroaniline herbicides inhibit T. gondii replication. Dinitroaniline has long been known to interfere with tubulin polymerization in plants (Morejohn et al. 1987). Trifluralin also binds to Leishmania tubulin and inhibits polymerization of subpellicular microtubules (Chan et al. 1991). In Plasmodium, Trifluralins bind to fragments of the subpellicular microtubules of gametocytes also inhibit erythrocytic stages and exflagellation of gametocytes (Nath et al. 1994; Kaidoh et al. 1995). They presume that T. gondii microtubules also interact with dinitroaniline.
Previously Parshikov et al. (2005) has been reported the antiplasmodial activities of artemisinin. D’Angelo et al. (2009) demonstrate that C-10 unsaturated, carba-linked (oxo-linked) derivatives of artemisinins can be effective in the inhibition of infection by T. gondii. This inhibition occurs at more than one step in the parasites lytic cycle. They have also documented that treatment of extracellular tachyzoites with these new derivatives resulted in an inhibition of parasite invasion.
Conclusion
To establish whether either one or both mechanisms are operative render, it requires to develop methods to differentiate between the effect of cromolyn sodium and ketotifen on the host cell membrane and the effect of cromolyn sodium and ketotifen on T. gondii itself. In this study, the inhibitory effects of ketotifen and cromolyn sodium on entrance of T. gondii tachyzoites into macrophages and other nucleated cells show that these drugs can be introduced as effective agents to inhibit the entry and invasion of T. gondii tachyzoites, into the cells.
Acknowledgments
We acknowledge the financial support of Grant No. 91-234 from the Mazandaran University of Medical Science, Iran.
Conflict of interest
The authors have no conflicts of interest regarding the content of this article.
References
- Ambroise-Thomas P, Pelloux H. Toxoplasmosis—congenital and in immunocompromised patients: a parallel. Parasitol Today. 1993;9:61–63. doi: 10.1016/0169-4758(93)90038-H. [DOI] [PubMed] [Google Scholar]
- Araujo FG, Remington JS. Recent advances in the search for new drugs for treatment of toxoplasmosis. Int J Antimicrob Agents. 1992;1:153–164. doi: 10.1016/0924-8579(92)90002-9. [DOI] [PubMed] [Google Scholar]
- Chan MMY, Triemer RE, Fong D. Effect of the anti-microtubule drug oryzalin on growth and differentiation of the parasitic protozoan Leishmania mexicana. Differentiation. 1991;46:15–21. doi: 10.1111/j.1432-0436.1991.tb00861.x. [DOI] [PubMed] [Google Scholar]
- Clarke M, Spudich JA. Non muscle contractile proteins: the role of actin and myosin in cell motility and shape determination. Annu Rev Biochem. 1977;46:797–822. doi: 10.1146/annurev.bi.46.070177.004053. [DOI] [PubMed] [Google Scholar]
- Cortez E, Stumbo AC, Saldanha-Gama R, et al. Immunolocalization of an osteopontin-like protein in dense granules of Toxoplasma gondii tachyzoites and its association with the parasitophorous vacuole. Micron. 2008;39:25–31. doi: 10.1016/j.micron.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Dadimoghaddam Y, Daryani A, Sharif M, Ahmadpour E, Hossienikhah Z. Tissue tropism and parasite burden of Toxoplasma gondii RH strain in experimentally infected mice. Asian Pac J Trop Med. 2014;7(7):521–524. doi: 10.1016/S1995-7645(14)60087-0. [DOI] [PubMed] [Google Scholar]
- D’Angelo JG, Bordon C, Posner GH, Yolken R, Jones-Brando L. Artemisinin derivatives inhibit Toxoplasmagondii in vitro at multiple steps in the lytic cycle. J Antimicrob Chemother. 2009;63:146–150. doi: 10.1093/jac/dkn451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey JP. The history of Toxoplasma gondii the first 100 years. J Eukaryot Microbiol. 2008;55:467–475. doi: 10.1111/j.1550-7408.2008.00345.x. [DOI] [PubMed] [Google Scholar]
- Ho-Yen DO, Joss AWL. Human toxoplasmosis. New York: Oxford University Press; 1992. [Google Scholar]
- Iaccheri B, Fiore T, Papadaki T, et al. Adverse drug reactions to treatments for ocular toxoplasmosis: a retrospective chart review. Clin Ther. 2008;30:2069–2074. doi: 10.1016/j.clinthera.2008.10.021. [DOI] [PubMed] [Google Scholar]
- Kaidoh T, Nath J, Fujioka H, et al. Effect and localization of trifluralin in Plasmodiumfalciparum gametocytes: an electron microscopic study. J Eukaryot Microbiol. 1995;42:61–64. doi: 10.1111/j.1550-7408.1995.tb01540.x. [DOI] [PubMed] [Google Scholar]
- Kasper LH, Mineo JR. Attachment and invasion of host cells by Toxoplasma gondii. Parasitol Today. 1994;10:184–188. doi: 10.1016/0169-4758(94)90026-4. [DOI] [PubMed] [Google Scholar]
- Morejohn LC, Bureau TE, Mole-Bajer J, et al. Oryzalin, a dinitroaniline herbicide, binds to plant tubulin and inhibits microtubule polymerization in vitro. Planta. 1987;172:252–264. doi: 10.1007/BF00394595. [DOI] [PubMed] [Google Scholar]
- Morisaki JH, Heuser JE, Sibley LD. Invasion of Toxoplasma gondii occurs by active penetration of the host cell. J Cell Sci. 1995;108:2457–2464. doi: 10.1242/jcs.108.6.2457. [DOI] [PubMed] [Google Scholar]
- Nam HW, Kim DJ, Park SK, et al. Inhibition of entry of Toxoplasma gondii into MDCK cells by fetal bovine serum. Korean J Parasitol. 1993;31:379–382. doi: 10.3347/kjp.1993.31.4.379. [DOI] [PubMed] [Google Scholar]
- Nath J, Okoye V, Schneider I (1994) Anti-malarial effects of the anti-tubulin herbicide trifluralin: studies with Plasmodium falciparum. DTIC document
- Nichols BA, Chiappino ML. Cytoskeleton of Toxoplasma gondii. J Eukaryot Microbiol. 1987;34:217–226. doi: 10.1111/j.1550-7408.1987.tb03162.x. [DOI] [PubMed] [Google Scholar]
- Parshikov IA, Miriyala B, Muraleedharan KM, et al. Biocatalysis of the antimalarial artemisinin by Mucor ramannianus strains. Pharm Biol. 2005;43:579–582. doi: 10.1080/13880200500301597. [DOI] [Google Scholar]
- Petersen E. Toxoplasmosis. Semin Fetal Neonatal Med. 2007;12:214–223. doi: 10.1016/j.siny.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Ryning FW, Remington JS. Effect of cytochalasin D on Toxoplasma gondii cell entry. Infect Immun. 1978;20:739–743. doi: 10.1128/iai.20.3.739-743.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serranti D, Buonsenso D, Valentini P. Congenital toxoplasmosis treatment. Eur Rev Med Pharmacol Sci. 2011;15:193–198. [PubMed] [Google Scholar]
- Stokkermans TJW, Schwartzman JD, Keenan K, et al. Inhibition of Toxoplasma gondii replication by dinitroaniline herbicides. Exp Parasitol. 1996;84:355–370. doi: 10.1006/expr.1996.0124. [DOI] [PubMed] [Google Scholar]
- Van der Ven AJAM, Schoondermark-van de Ven EME, Camps W, et al. Anti-Toxoplasma effect of pyrimethamine, trimethoprim and sulphonamides alone and in combination: implications for therapy. J Antimicrob Chemother. 1996;38:75–80. doi: 10.1093/jac/38.1.75. [DOI] [PubMed] [Google Scholar]
- Weiss LM, Kim K. Toxoplasma gondii: the model apicomplexan. Perspectives and methods. London: Academic Press; 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]