Abstract
Clear cell meningiomas are an uncommon subtype of meningioma rarely seen in infancy. We report a case of clear cell meningioma in an 8-month-old male infant. He presented at the Lagos University Teaching Hospital, Lagos, Nigeria, in 2015 with persistent vomiting, poor feeding and failure to thrive over a four month period. Generalised hypertonia and hyperreflexia were noted on examination. Computed tomography of the brain revealed a huge largely isodense suprasellar mass with a hypodense core. The tumour, which measured 6 × 5 × 4 cm, enhanced non-uniformly with contrast injection and extended to occlude the third ventricle. The patient underwent a bifrontal craniotomy with subtotal tumour excision. Six hours postoperatively, he went into cardiac arrest and could not be resuscitated. A histological diagnosis of clear cell meningioma was made as the tumour cells were immunoreactive to epithelial membrane antigen, S100 protein and vimentin. This case of clear cell meningioma was unusual due to its early occurrence and supratentorial location.
Keywords: Clear Cell Meningioma, Brain Tumor, Central Nervous System Tumors, Infant, Case Report, Nigeria
Clear cell meningiomas are a rare variant of meningioma that generally occur in the cerebellopontine angle and the spine.1 Despite its bland histological appearance, this tumour is classified as a World Health Organisation (WHO) grade II neoplasm due to its aggressive nature and high propensity for recurrence and spinal seeding.2 Although they usually occur in a much younger age group than most other meningiomas, clear cell meningiomas are still rare in infancy.3 This case describes a rare case of meningioma with unusual characteristics, which included a very early age of occurrence and the supratentorial location of the tumour.
Case Report
An 8-month-old male infant was referred to the Lagos University Teaching Hospital, Lagos, Nigeria, in 2015 with persistent vomiting, poor feeding and failure to thrive over a four month period. The vomiting was postprandial and the contents contained recently ingested food. There was no history of loss of consciousness, seizures or fever. The patient’s father reported that the child could not see using his right eye. The pregnancy, delivery and perinatal history had been unremarkable and there was no history of maternal exposure to radiation.
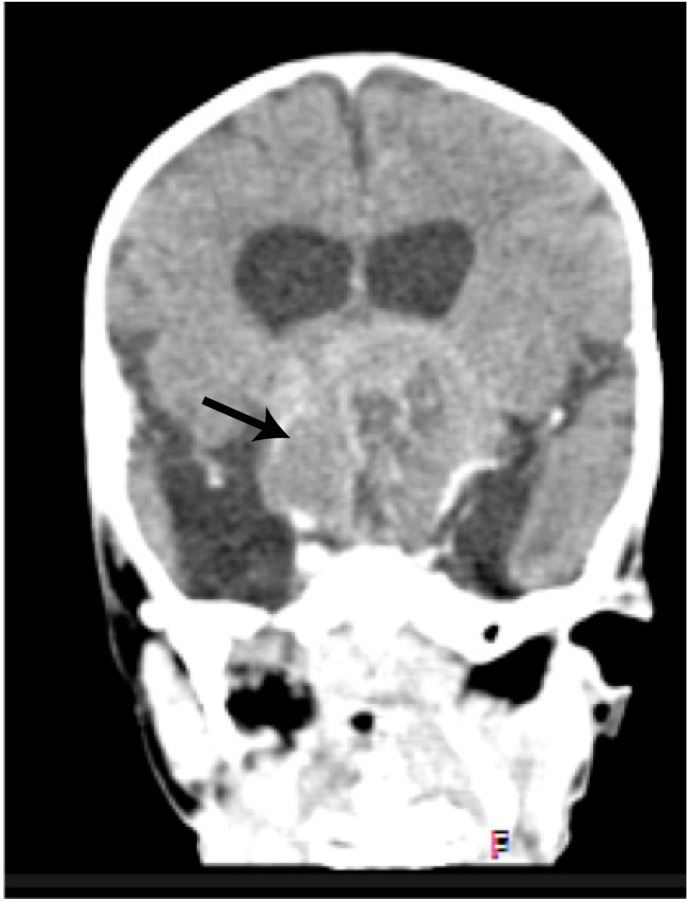
On examination, the child was fully conscious and undernourished, weighing 6 kg (60% of his expected weight). He was not pale, cyanosed or dehydrated. His pupils measured 3 mm and were reactive bilaterally; however, a fundoscopic examination revealed bilateral optic atrophy. Generalised hypertonia and hyperreflexia were also noted. A computed tomography scan of the brain revealed a huge largely isodense suprasellar mass with a hypodense core. The mass measured 6 × 5 × 4 cm, enhanced non-uniformly with contrast injection and extended superiorly to efface the third ventricle [Figure 1]. A bifrontal craniotomy was performed. Intraoperatively, the tumour contained areas which felt hard and gritty to the touch, while other areas were soft and jelly-like in consistency. It was adherent to the optic nerves bilaterally and the optic chiasm and was successfully separated from the left optic nerve and the optic chiasm during surgery. However, attempts to separate the tumour from the right optic nerve proved unsuccessful, resulting in subtotal excision of the tumour. The patient was transfused with 480 mL of blood intraoperatively. He was transferred postoperatively to the Intensive Care Unit where he subsequently developed hyperthermia (temperature: >40 °C) and tachycardia (pulse rate range: 180–240 beats per minute). Six hours following the operation, the patient went into cardiac arrest and unfortunately could not be resuscitated.
Figure 1:
Brain computed tomography scan showing an isodense suparasellar mass (arrow) in an 8-month-old infant with a suprasellar clear cell meningioma.
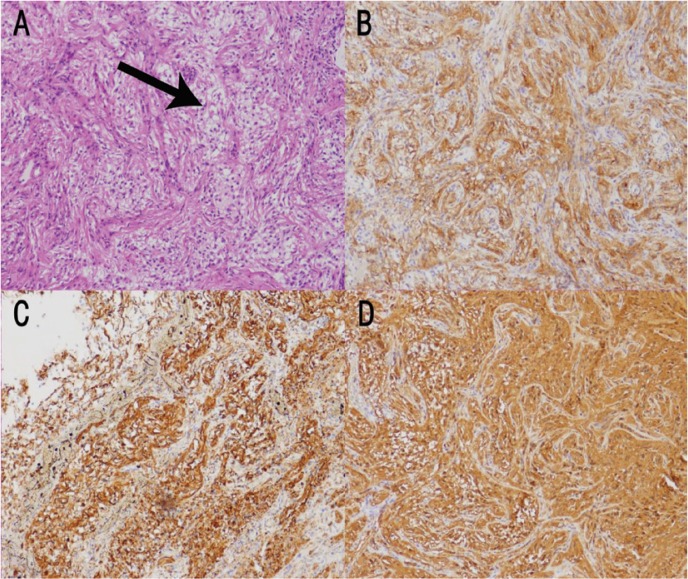
Histopathological assessment of the tumour revealed proliferating meningothelial cells, many of which had clear cytoplasm within a densely fibrotic stroma. The cells formed a vague whorled pattern in some foci and had a bland cytological appearance. Mitoses were scanty and areas of cystic degeneration and vascular congestion were seen [Figure 2A]. The tumour cells showed immunoreactivity to epithelial membrane antigen (EMA), vimentin and S100 protein [Figures 2B–D]. A diagnosis of clear cell meningioma was made.
Figure 2A–D:
Photomicrographs of (A) a haematoxylin and eosin stain at ×1,000 magnification showing meningothelial cells with clear cytoplasm within a fibrotic stroma (arrow) and (B) epithelial membrane antigen stain at ×1,000 magnification, (C) vimentin stain at ×1,000 magnification and (D) S100 stain at ×1,000 magnification showing immunoreactivity.
Discussion
Like other meningiomas, clear cell meningiomas are tumours of meningothelial cells, which are normally scattered in the arachnoid membranes throughout the neuraxis but have their highest concentration at the tips of the arachnoid granulations, where they are called arachnoid cap cells.4 In clear cell meningiomas, the meningothelial cells accumulate glycogen which results in a clear appearance.2 Clear cell meningiomas are rare tumours that account for 0.2–0.8% of all meningiomas and thus few cases have been reported in the literature.5 Clear cell meningiomas, as with other meningiomas, show a slight female predominance.1
The current case was unusual in view of the very early age of tumour occurrence and the supratentorial location of the tumour. Clear cell meningiomas are more commonly seen in younger children and adolescents.3,5,6 In a study of 14 patients ranging from 9 to 82 years old, the mean age of occurrence was 29 years.6 In another study of nine cases diagnosed over an eight year period, the median age of occurrence was 26 years.5 These are much lower than the usual ages of occurrence of other types of meningioma, which have been reported variously to be during the fourth, fifth, sixth and ninth decades in Lagos, South Africa, Egypt and the USA, respectively.7–10 The patient in the current case presented at eight months of age, which is an unusually young age of occurrence for clear cell meningiomas. There are only a few reports of this tumour occurring in infancy; among these, most tumours were located in the intraspinal compartment.11,12 In general, most clear cell meningiomas have an infratentorial location.1 However, in the present case, the tumour was located in the suprasellar region; this location accounted for only 4.3% of meningiomas reported in a previous study conducted at the Lagos University Teaching Hospital.7 Other rare tumour locations that have been reported include the foramen magnum and the fourth ventricle.6,13
The histological differential diagnosis of primary central nervous system tumours with a clear cell morphology includes clear cell meningiomas, neurocytomas, oligodendrogliomas, ependymomas and haemangioblastomas.14 Clear cell meningiomas are characterised histologically by the presence of polygonal cells with clear glycogen-rich cytoplasm, often in no particular pattern, within a densely fibrotic stroma.2 Whorl formation is vague and psammoma bodies are not usually seen.2 The tumour cells are usually immunoreactive to EMA, S100 protein and vimentin—as was the case for the current patient— and are usually negative for synaptophysin, glial fibrillary acidic protein, cytokeratins and desmin.1 In ultrastructural studies, the clear cell meningioma cells should have intercellular junctions, interdigitating processes and intermediate vimentin filaments.14 Unlike other WHO grade II meningiomas, which tend to have a mitotic count greater than four per 10 high-power fields, clear cell meningiomas often have low mitotic activity; moreover, mitosis has been shown to be of no value in predicting the aggressiveness of the neoplasm.1,2,6 Jain et al. found that the MIB-1 labelling index of clear cell meningiomas ranged from 2–12%.5 Deb et al. reported a MIB-1 labelling index of <1% in a case of recurrent clear cell meningioma.1
Proliferating cell nuclear antigen proliferative indices, percentage S-phase determination and DNA ploidy have been linked with aggressiveness in clear cell meningiomas.6,13 Closer follow-up is therefore required for these cases. Furthermore, germline SMARCE 1 (SWItch/sucrose non-fermentable-related matrix-associated actin-dependent regulator of chromatin subfamily E member 1) mutations have been linked with spinal and cranial clear cell meningiomas.15,16 Smith et al. identified SMARCE 1 mutations and loss of SMARCE 1 proteins in patients and paraffin-embedded tissue blocks of spinal and cranial clear cell meningioma cases.15 The treatment of choice for clear cell meningiomas is total surgical resection, with radiotherapy and chemotherapy being reserved for recurrent cases.1 Juratli et al. observed increasing overexpression of epidermal growth factor, platelet-derived growth factor and vascular endothelial growth factor receptors with each recurrent tumour; receptor-targeted therapy was therefore recommended for such tumours.17
Conclusion
This report described an 8-month-old infant with clear cell meningioma diagnosed postoperatively by histopathological assessment. Both the early presentation at infancy and supratentorial location of the tumour were unusual features; most cases occur in younger children or adolescents and the tumours usually have an infratentorial location. The optimal treatment for this rare subtype of meningioma is total surgical resection, with radiotherapy, chemotherapy and receptor-targeted therapy being reserved for recurrent cases.
References
- 1.Deb P, Datta SG. An unusual case of clear cell meningioma. J Cancer Res Ther. 2009;5:324–7. doi: 10.4103/0973-1482.59902. [DOI] [PubMed] [Google Scholar]
- 2.Perry A, Louis DN, Scheithauer BW, Budka H, von Deimling A. Meningeal tumours. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, editors. WHO Classification of Tumours of the Central Nervous System. 4th ed. Lyon, France: International Agency for Research on Cancer Press; 2007. pp. 163–86. [Google Scholar]
- 3.Kumar R, Das KK, Jaiswal AK, Mehrotra A, Sahu RN, Srivastava AK, et al. Clear cell meningioma in a child: A case report and review of literature. Asian J Neurosurg. 2015;10:53. doi: 10.4103/1793-5482.151520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brat DJ. Overview of central nervous system anatomy and histology. In: Prayson R, editor. Neuropathology. 2nd ed. Philadelphia, Pennsylvania, USA: Saunders; 2011. pp. 1–39. [Google Scholar]
- 5.Jain D, Sharma MC, Sarkar C, Suri V, Garg A, Singh M, et al. Clear cell meningioma, an uncommon variant of meningioma: A clinicopathologic study of nine cases. J Neurooncol. 2007;81:315–21. doi: 10.1007/s11060-006-9237-7. [DOI] [PubMed] [Google Scholar]
- 6.Zorludemir S, Scheithauer BW, Hirose T, Van Houten C, Miller G, Meyer FB. Clear cell meningioma: A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol. 1995;19:493–505. doi: 10.1097/00000478-199505000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Anunobi CC, Ikeri NZ. Primary central nervous system tumours in children and adolescents in LUTH, Lagos, Nigeria. Niger Med Pract. 2015;68:39–44. [Google Scholar]
- 8.Ibebuike K, Ouma J, Gopal R. Meningiomas among intracranial neoplasms in Johannesburg, South Africa: Prevalence, clinical observations and review of the literature. Afr Health Sci. 2013;13:118–21. doi: 10.4314/ahs.v13i1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zalata KR, El-Tantawy DA, Abdel-Aziz A, Ibraheim AW, Halaka AH, Gawish HH, et al. Frequency of central nervous system tumours in delta region, Egypt. Indian J Pathol Microbiol. 2011;54:299–306. doi: 10.4103/0377-4929.81607. [DOI] [PubMed] [Google Scholar]
- 10.Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: Primary brain and central nervous system tumours diagnosed in the United States in 2005–2009. Neuro Oncol. 2012;14:1–49. doi: 10.1093/neuonc/nos218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu PI, Liu GC, Tsai KB, Lin CL, Hsu JS. Intraspinal clear-cell meningioma: Case report and review of literature. Surg Neurol. 2005;63:285–8. doi: 10.1016/j.surneu.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Park HC, Sohn MJ, Kim EY, Han HS, Park HS. Spinal clear cell meningioma presented with progressive paraparesis in infancy. Childs Nerv Syst. 2000;16:607–10. doi: 10.1007/PL00007302. [DOI] [PubMed] [Google Scholar]
- 13.Pimentel J, Fernandes A, Pinto AE, Fonseca I, Moura Nunes JF, Lobo Antunes J. Clear cell meningioma variant and clinical aggressiveness. Clin Neuropathol. 1998;17:141–6. [PubMed] [Google Scholar]
- 14.Camelo-Piragua S. Clear cell tumours of the central nervous system: A case-based review. Arch Pathol Lab Med. 2012;136:915–26. doi: 10.5858/arpa.2012-0216-CR. [DOI] [PubMed] [Google Scholar]
- 15.Smith MJ, Wallace AJ, Bennett C, Hasselblatt M, Elert-Dobkowska E, Evans LT, et al. Germline SMARCE1 mutations predispose to both spinal and cranial clear cell meningiomas. J Pathol. 2014;234:436–40. doi: 10.1002/path.4427. [DOI] [PubMed] [Google Scholar]
- 16.Evans LT, Van Hoff J, Hickey WF, Smith MJ, Evans DG, Newman WG, et al. SMARCE1 mutations in pediatric clear cell meningioma: Case report. J Neurosurg Pediatr. 2015;16:296–300. doi: 10.3171/2015.3.PEDS14417. [DOI] [PubMed] [Google Scholar]
- 17.Juratli TA, Geiger KD, Weigel P, von der Hagen M, Daubner D, Pinzer T, et al. A five year-old child with clear cell petro-clival meningioma: Case report with clinical and histopathological long-term follow-up. Childs Nerv Syst. 2015;31:2193–8. doi: 10.1007/s00381-015-2782-7. [DOI] [PubMed] [Google Scholar]