Abstract
Purpose
Improving dyspnea and exercise performance are goals of COPD therapy. We tested the hypothesis that air current applied to the face would lessen dyspnea and improve exercise performance in moderate-severe COPD patients.
Methods
We recruited 10 COPD patients (5 men, age 62 ± 6 years, FEV1 0.93 ± 0.11 L (34 ± 3 % predicted), TLC 107 ± 6 %, RV 172 ± 18 %) naïve to the study hypothesis. Each patient was randomized in a crossover fashion to lower extremity ergometry at constant submaximal workload with a 12-diameter fan directed at the patients face or exposed leg. Each patients’ studies were separated by at least 1 week. Inspiratory capacity and Borg dyspnea score were measured every 2 min and at maximal exercise.
Results
Total exercise time was longer when the fan was directed to the face (14.3 ± 12 vs. 9.4 ± 7.6 min, face vs. leg, respectively, p = 0.03). Inspiratory capacity tended to be greater with the fan directed to the face (1.4 (0.6–3.25) vs. 1.26 (0.56–2.89) L, p = 0.06). There was a reduction in dynamic hyperinflation, as reflected by higher IRV area in the fan on face group (553 ± 562 a.u. vs. 328 ± 319 a.u., p = 0.047). There was a significant improvement in the Borg dyspnea score at maximal exercise (5.0 (0–10) vs. 6.5 (0–10), p = 0.03), despite exercising for 34 % longer with the fan directed to the face.
Conclusions
Air current applied to the face improves exercise performance in COPD. Possible mechanisms include an alteration in breathing pattern that diminishes development of dynamic hyperinflation or to a change in perception of breathlessness.
Keywords: COPD, Dynamic hyperinflation, Emphysema, Exercise physiology
Introduction
Chronic obstructive pulmonary disease (COPD) is the 3rd leading cause of death in the United States and further increases in the prevalence and mortality is expected in the coming decades [1]. Progressive dyspnea and exercise intolerance are often the reasons patients seek medical consultation [2]. Patients with COPD have an expiratory flow limitation that leads to air trapping and hyperinflation, both of which cause dyspnea. Dynamic hyperinflation is one of the major causes of exercise limitation in COPD patients [3]. As the end-inspiratory lung volume approaches total lung capacity during exercise, the inspiratory capacity decreases, dyspnea develops, and the subject stops exercising [3, 4].
Improving dyspnea and exercise performance are primary goals of COPD therapy, and there are many pharmacologic and non-pharmacologic methods of achieving these goals. These methods vary in the degree of cost and invasiveness. Medications such as tiotropium and salmeterol have been shown to improve exercise by delaying the development of dynamic hyperinflation [5, 6]. Oxygen and heliox have also been shown to improve exercise performance by reducing dynamic hyperinflation [7, 8]. Non-pharmacologic methods such as lung volume reduction surgery or bullectomy also improve dyspnea and exercise intolerance by improving dynamic hyperinflation [9, 10]. Patients often seek relief from dyspnea by blowing air toward their face with use of a fan or sitting in front of an open window. In fact, the use of fans has previously been suggested as a method of treating dyspnea [11]. Schwartzstein et al. have shown that an air current applied to the face of normal subjects resulted in less dyspnea while breathing against a resistive load during hypercapnic challenge [12]. Also, we have shown that normal subjects breathing against a resistive load with air current directed to their face were able to perform more inspiratory muscle work due to a change in respiratory muscle recruitment [13].
We hypothesized that air blown to the face of COPD patients would reduce dyspnea and improve exercise performance. We designed a randomized crossover study, where patients exercised with an air current directed toward their face or leg. Specifically, we wanted to study the effect of the air current on exercise time, dyspnea, and breathing pattern during exercise, and the development of dynamic hyperinflation. Some of the results of this study has been previously reported in the form of an abstract [14].
Methods and Materials
Patient Selection
Patients between 50- and 80-years old with COPD [2] and ≥10 pack-years smoking history were recruited from the outpatient pulmonary clinic at Temple University. Patients with recent COPD exacerbation (≤3 months) or a clinical history of cardiovascular or peripheral vascular disease were excluded. The Institutional Review Board approved the study and the patients signed an informed consent prior to participation.
Pulmonary Function Testing
All patients underwent spirometry and lung volumes according to ATS standards [15], and the reference for normals was that of Morris and Polgar [16]. The post bronchodilator FEV1 was reported as percent predicted.
Air Current
An air current provided by a standard 12-inch house fan (Windmere; Miami Lakes, FL) on medium speed placed 24 inches laterally from the patient's exposed leg (control) or face while performing constant workload exercise. Peak air flow was 840 Ft/min as measured by an anenmometer (Kurz Instruments, Monterey, CA). The order of fan placement was random and patients were naïve to study hypothesis.
Study Design
Patients first performed symptom limited maximal incremental cardiopulmonary exercise test (CPET) on a cycle ergometer (Viasys, San Diego, CA). During exercise, metabolic and respiratory parameters were recorded breath to breath (Vmax; Yorba Linda, CA) and reported as 20-s averages. Modified Borg score scale [17] was used every 2 min to assess dyspnea. Following 5 min warm-up and 3 min of unloaded pedaling, the patients exercised using either a 5 or 10 watt/min ramp depending on their maximal voluntary ventilation. If patients used supplemental oxygen at home, then patients exercised while breathing 30 % FiO2 using an oxygen blender (Bird, Palm Springs, CA). One week later, patients performed constant workload exercise on the cycle ergometer at a workload at 75 % of max workload obtained on maximal CPET (n = 3), but because patients were stopping exercise prematurely, the constant workload was decreased to 50 % of max for the remainder of the patients (n = 7). Patients returned one week later to perform a second constant workload exercise study at the same constant workload, but with fan directed toward the opposite site.
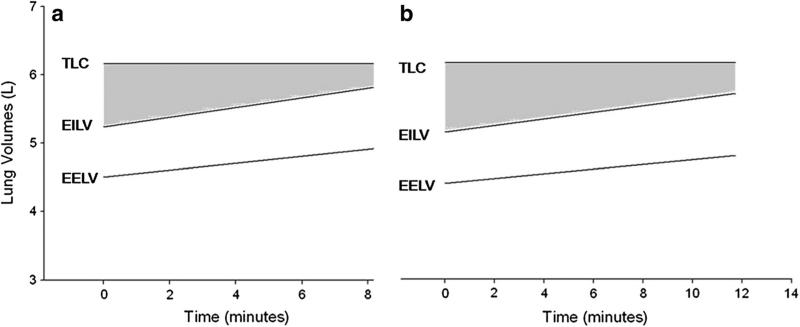
Measurement of Dynamic Lung Volumes
In order to measure end-expiratory lung volume (EELV) during exercise, the inspiratory capacity (IC) was measured every two minutes during exercise [3]. Patients were instructed in performance of the IC maneuver prior to exercise, and three IC measurements were taken during the baseline phase of CPET. The baseline IC reported is the mean of these three measurements. Because TLC does not change during exercise [18, 19], EELV can be calculated by subtracting IC from TLC. The end-inspiratory lung volume (EILV) is calculated by adding VT to the EELV. The inspiratory reserve volume (IRV) is calculated by subtracting the EILV from the TLC. When plotted against time, the IRV area can be calculated by calculating the area of a trapezoid.
The base is represented by the IRV at the beginning of exercise, the top by the IRV at the end of exercise, and the height is the exercise time. Greater IRV area represents less DH..
Statistical Analysis
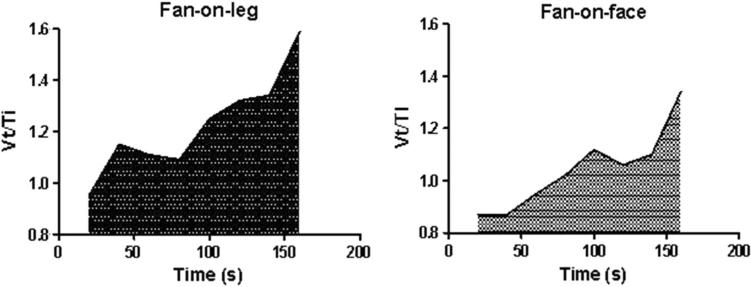
All data are reported as mean ± SD unless otherwise noted. Non-parametric data were presented as median (range). A two-way ANOVA with repeated measures analysis was used to compare Borg scores and inspiratory capacity during exercise over time. Data were analyzed using paired t tests or, when the data were non-parametric, Wilcoxon-matched pairs signed rank test. The area under the curve was calculated using GraphPad Prism 5 (La Jolla, CA) for each parameter for the shorter exercise time of the two CPETs in order to match exercise isotimes (Fig. 1).
Fig. 1.
Area under the curve (AUC). A representative patient showing the AUC for the parameter VT/Ti. AUC was calculated over the exercise isotime (160 s in this example) and is expressed as arbitrary units (a.u.)
Results
Demographics
Ten patients (five men) with a mean age of 62 ± 6 years participated in the study and all subjects completed the study (Table 1). These patients had severe obstructive disease by ATS criteria with significant air trapping [20]. Four of the patients used oxygen during exercise, and no patient had a significant decrease in their oxygenation (defined as a fall in SpO2 of at least 4 %) during exercise.
Table 1.
Demographics and Functional Characteristics
| Age (years) (n = 10) | 62 ± 6 |
| FEV1 (L) (n = 10) | 0.93 ± 0.11 |
| FEV1 % predicted (n = 10) | 34 ± 3 |
| TLC % predicted (n = 9) | 107 ± 6 |
| RV % predicted (n = 9) | 172 ± 18 |
| RV/TLC % (n = 9) | 59 ± 3 |
| Sex | 5 men |
FEV1 forced expiratory volume in 1 s; TLC total lung capacity; RV residual volume
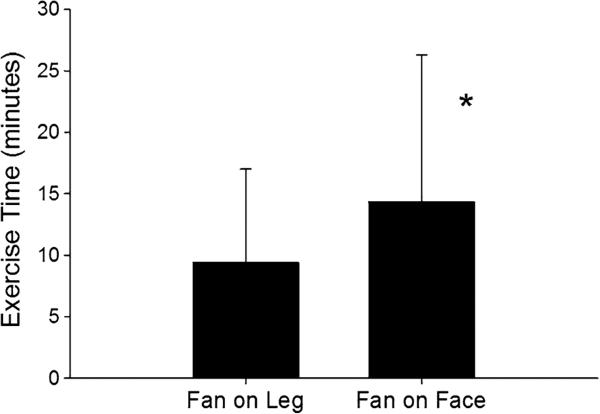
Exercise Time and Dyspnea
Exercise was performed at a mean of 28.2 ± 18.8 watts. Patients exercised 34 % longer (14.3 ± 12 vs. 9.4 ± 7.6 min; p = 0.03) with the air current applied to the face as compared to the leg (Fig. 2). Despite exercising for a significantly longer duration, subjects had lower Borg dyspnea scores (5.0 (0–10) vs. 6.5 (0–10); p = 0.03) during max exercise with the fan directed toward the face.
Fig. 2.
Exercise time. Patients exercised 34 % longer with the air current directed to the face as compared to the leg. Data bars are mean ± standard deviation. *p<0.05, fan directed to fan compared to fan directed to legs
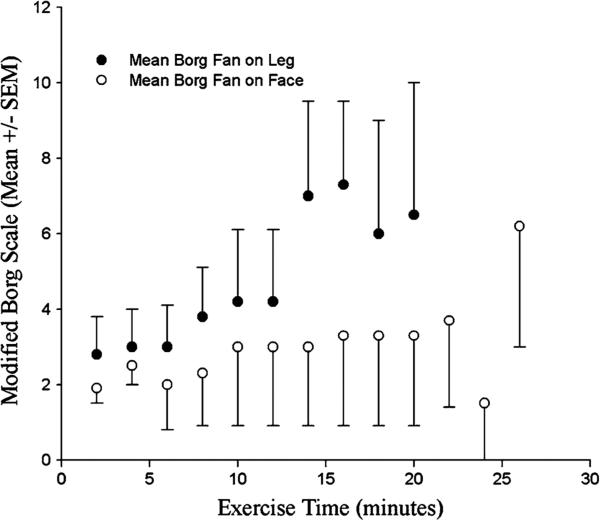
They also had lower Borg dyspnea scores with the fan on the face at each recorded time point during exercise (Fig. 3).
Fig. 3.
Borg scores during exercise. Filled circle air current directed to the face. Open circle air current directed to the leg. Data are mean ± standard error of the mean. *p≤0.05, fan directed to fan compared to fan directed to legs
Breathing Pattern
The breathing pattern was analyzed by comparing the area under the curve, as shown in Fig. 1. There was no significant difference between VO2, respiratory rate (f), tidal volume (Vt), minute ventilation, or f/Vt ratio with the fan directed toward the face or the leg. The area under the curve for the inspiratory time (Ti) (Table 2) was significantly lower (p = 0.04) with the fan directed toward the face.
Table 2.
Breathing pattern (n = 10) expressed as the area under the curve (arbitrary units (a.u.))
| Fan on leg | Fan on face | p value | |
|---|---|---|---|
| VO2 (a.u.) | 179.2 (72.1, 619.4) | 165.7 (64.3, 640.0) | 0.19 |
| RR (a.u.) | 7640.4 (4095.5, 24,708.1) | 7710.2 (3877.8, 25,072.6) | 0.13 |
| Vt (a.u.) | 10,598.9 (5155.0, 29,352.2) | 10,063.4 (5172.3, 49,171.7) | 0.38 |
| VE (a.u.) | 7790.0 (3183.5, 20,765.3) | 7595.6 (2555.8, 20,849.2) | 0.23 |
| Ti (a.u.) | 238.3 (118.0, 731.6) | 233.3 (132.4, 751.2) | 0.04 |
| Te (a.u.) | 478.9 (236.7, 1418.1) | 506.0 (241.3, 1491.3) | 0.19 |
| VT/Ti (a.u.) | 342.7 (167.4, 1170.3) | 347.0 (143.3, 1104.8) | 0.05 |
| VT/Te (a.u.) | 220.0 (80.0, 544.2) | 208.1 (62.6, 550.3) | 0.19 |
| f/VT (a.u.) | 10,600.3 (5155.9, 29,352.1) | 10,063.2 (5172.0, 30,513.8) | 0.31 |
| Borg (a.u.) | 6.5 (0–10) | 5.0 (0–10) | 0.03 |
| IC (L) | 1.26 (0.56–2.89) | 1.4 (0.6–3.25) | 0.06 |
Data are presented as median (range)
VO2 oxygen uptake, RR respiratory rate; Vt tidal volume; VE minute ventilation, Ti inspiratory time; Te expiratory time; Vt/Ti inspiratory flow rate; Vt/Te expiratory flow rate; f/Vt respiratory rate/tidal volume, IC inspiratory capacity
Dynamic Hyperinflation
The inspiratory capacity throughout exercise was higher with the fan directed toward the face (1.45 ± 0.4 vs 1.37 ± 0.4 L; p = 0.06) suggesting that there was less dynamic hyperinflation with air blown on the face. Nine of the ten patients had static lung volumes measured, which allowed the calculation of the IRV area. The IRV area was significantly greater when the fan was directed toward the face (553 ± 562 a.u. vs. 328 ± 319 a.u.; p = 0.047) showing that there was less dynamic hyperinflation (Fig. 4a and b).
Fig. 4.
Inspiratory reserve area (IRV) with fan on leg (a) compared to fan on face( b). The IRV area was significantly greater with the fan on the face (see text for details). The shaded area represents the IRV
Heart Rate/Blood Pressure
To explore the diving reflex as a potential mechanism for improved exercise performance, heart rate and blood pressure were analyzed. When measured at metabolic isotime (75 %VCO2max), there was no difference in HR between fan on face and fan on leg (111.9 ± 15.2 vs. 113 ± 12.9; p = 0.76). There was also no difference between fan on face and fan on leg in change in systolic BP from the start to the end of exercise (46.8 ± 17.7 vs. 53.8 ± 21.8; p = 0.42) or change in mean arterial pressure (23.3 ± 11.7 vs. 26.6 ± 13.1; p = 0.58).
Discussion
COPD patients were able to exercise 34 % longer during constant workload (50–75 % max) lower extremity ergometry with a fan blowing air onto the face compared to the exposed leg. Not only did patients exercise longer, but they also had less dynamic hyperinflation and less dyspnea with the fan directed toward the face.
Possible mechanisms for this observation may be related to the diving reflex, stimulation of the trigeminal nerve leading to alterations in the perception of dyspnea, or to diminished dynamic hyperinflation. The diving reflex is defined as an oxygen-conserving decrease in heart rate that is due to an increase in cardiac parasympathetic nerve activity and peripheral vasoconstriction triggered by the cessation of respiration and stimulation of facial cold receptors [21]. An experiment by Mukhtar et al. demonstrated that either breath holding or facial immersion in water is necessary for the full diving reflex [22]. However, other investigators have shown that facial cooling without immersion, with [23] or without [24] breath holding, may induce a similar reflex, with reductions in heart rate and increases in blood pressure and tidal volume. However, in our current study, we did not observe a lower heart rate, a higher blood pressure, or higher tidal volumes during exercise with an air current directed toward the face making the diving reflex seem less likely. This is possibly because there was no facial immersion, no breath holding, and lack of adequate facial cooling for the diving reflex to occur in our study.
An alternate mechanism may be an altered perception of breathlessness. Schwartzstein et al. have shown that an air current applied to the face of normal subjects resulted in less dyspnea while breathing against a resistive load during hypercapnic challenge [12]. They theorized that afferent information that results from stimulation of receptors in the trigeminal nerve distribution is projected to the sensory cortex and alters perception of breathlessness. In our current study, we showed that COPD patients exercising with the fan on their face had lower Borg dyspnea scores at all time points as well as at maximum exercise, despite exercising for a significantly longer time. The lower Borg dyspnea scores may be reflective of trigeminal nerve stimulation from the fan current.
We were able to show that there was significantly less dynamic hyperinflation, which likely explains why patients were able to exercise longer. During exercise, the EELV rises in patients with COPD until the inspiratory reserve volume reaches a critical point. Our patients were able to exercise longer prior to reaching their critical IRV with the fan directed toward their face and this likely explains why they were able to exercise longer. We believe that the air current directed to the face stimulates the trigeminal nerve thus altering the patient's perception of dyspnea, which alters the patient's breathing pattern. This would allow patients to breathe slower resulting in less dynamic hyperinflation. There was a shorter inspiratory time and a trend toward a longer expiratory time and a lower f/Vt ratio during exercise in our patients that may become significant with a larger number of patients. The change in breathing pattern as an explanation for improved exercise performance is also supported by the fact that we have shown normal subjects breathing against a resistive load with air current directed to their face were able to perform more inspiratory muscle work due to a change in respiratory muscle recruitment [13].
An air current applied toward the subject's face results in exercise performance improvement that is equivalent to other pharmacologic and non-pharmacologic approaches to improve exercise performance in COPD. However, the cost associated with the use of a fan is dramatically lower compared to the other interventions (Table 3).
Table 3.
Comparison of fan on face to other modalities of exercise performance improvement in COPD
| Degree of exercise improvement (%) | Cost | |
|---|---|---|
| Heliox | 30 | $59,808/year |
| Oxygen | 30–45 | $4800/year |
| Tiotropium | 20 | $3600/year |
| LVRS | 25 | $71,515 first year cost [25] |
| Fan | 34 | $12 |
LVRS lung volume reduction surgery
There are some limitations to our current study. The small number of patients limited our ability to determine the exact mechanism of lowered dynamic hyperinflation. However, despite this we were able to show our primary endpoints of improved exercise time and less dynamic hyperinflation. Another potential limitation was the fact that a minority of the patients performed constant workload exercise at 75 % of the maximal workload, while the majority exercised at 50 % of the maximal workload. This was necessary because at 75 % of the maximal workload, our severe COPD patients were unable to exercise long enough. We believe that this is a minor limitation because the majority of the patients exercised at 50 % of the maximal workload, and all patients exercised at the same constant workload with the fan directed to the face and the leg. Also some of the patients exercised with oxygen, while others did not. We decided to have patients that use oxygen at home to exercise with it so that hypoxemia did not limit their exercise performance. Whether or not patients exercised with oxygen or not was the same for the air current directed toward the face or the leg. It is possible that there was a differential cooling of body temperature in the two groups. Although we did not measure body temperature, it is unlikely that a fan with the same current applied to different body parts would lead to a significantly different body temperature.
Conclusions
An air current directed toward the face resulted in a 34 % improvement in exercise performance in patients with COPD. The exercise improvement is likely related to reduced dynamic hyperinflation and is comparable to other pharmacologic and non-pharmacologic modalities that improve exercise performance in COPD but at a significantly lower cost. An air current directed toward the face is a cost-effective way to relieve dyspnea and improve exercise performance in patients with COPD.
Acknowledgments
Supported in part by the National Institute of General Medical Sciences of the National Institutes of Health under award number U54 GM104940 (MRL).
Footnotes
Compliance with Ethical Standards
Conflict of interest None of the authors have any real or apparent conflicts of interests related to this work to disclose. No professional writing assistance was used for this manuscript.
References
- 1.Kochanek KD, Xu J, Murphy SL, et al. Deaths: preliminary data for 2009. Natl Vital Stat Rep. 2011;59:1–51. [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global strategy for the diagnosis, management, and prevention of COPD. 2008 http://goldcopd.com.
- 3.O'Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(5):770–777. doi: 10.1164/ajrccm.164.5.2012122. [DOI] [PubMed] [Google Scholar]
- 4.O'Donnell DE, Hamilton AL, Webb KA. Sensory-mechanical relationships during high-intensity, constant-work-rate exercise in COPD. J Appl Physiol. 2006;101(4):1025–1035. doi: 10.1152/japplphysiol.01470.2005. [DOI] [PubMed] [Google Scholar]
- 5.O'Donnell DE, Fluge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respir J. 2004;23(6):832–840. doi: 10.1183/09031936.04.00116004. [DOI] [PubMed] [Google Scholar]
- 6.O'Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J. 2004;24(1):86–94. doi: 10.1183/09031936.04.00072703. [DOI] [PubMed] [Google Scholar]
- 7.O'Donnell DE, D'Arsigny C, Webb KA. Effects of hyperoxia on ventilatory limitation during exercise in advanced chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(4):892–898. doi: 10.1164/ajrccm.163.4.2007026. [DOI] [PubMed] [Google Scholar]
- 8.Palange P, Valli G, Onorati P, et al. Effect of heliox on lung dynamic hyperinflation, dyspnea, and exercise endurance capacity in COPD patients. J Appl Physiol. 2004;97(5):1637–1642. doi: 10.1152/japplphysiol.01207.2003. [DOI] [PubMed] [Google Scholar]
- 9.Martinez FJ, de Oca MM, Whyte RI, et al. Lung-volume reduction improves dyspnea, dynamic hyperinflation, and respiratory muscle function. Am J Respir Crit Care Med. 1997;155(6):1984–1990. doi: 10.1164/ajrccm.155.6.9196106. [DOI] [PubMed] [Google Scholar]
- 10.O'Donnell DE, Webb KA, Bertley JC, et al. Mechanisms of relief of exertional breathlessness following unilateral bullectomy and lung volume reduction surgery in emphysema. Chest. 1996;110(1):18–27. doi: 10.1378/chest.110.1.18. [DOI] [PubMed] [Google Scholar]
- 11.Galbraith S, Fagan P, Perkins P, et al. Does the use of a handheld fan improve chronic dyspnea? A randomized, controlled, crossover trial. J Pain Symptom Manag. 2010;39(5):831–838. doi: 10.1016/j.jpainsymman.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Schwartzstein RM, Lahive K, Pope A, et al. Cold facial stimulation reduces breathlessness induced in normal subjects. Am Rev Respir Dis. 1987;136(1):58–61. doi: 10.1164/ajrccm/136.1.58. [DOI] [PubMed] [Google Scholar]
- 13.Solomon BR, Travaline JM, Criner GJ. Impact of air current applied to the face on inspiratory task performance in normal subjects [abstract]. Am J Respir Crit Care. 2003;167:A414. [Google Scholar]
- 14.Marchetti N, Travaline JM, Criner GJ. Air current applied to the face of COPD patients enhances leg ergometry performance. Am J Respir Crit Care. 2004;169:A773. [Google Scholar]
- 15.Anonymous American thoracic society Standardization of spirometry: 1994 update. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 16.Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- 17.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 18.Stubbing DG, Pengelly LD, Morse JL, Jones NL. Pulmonary mechanics during exercise in subjects with chronic airflow obstruction. J Appl Physiol. 1980;49(3):511–515. doi: 10.1152/jappl.1980.49.3.511. [DOI] [PubMed] [Google Scholar]
- 19.Stubbing DG, Pengelly LD, Morse JL, Jones NL. Pulmonary mechanics during exercise in normal males. J Appl Physiol. 1980;49(3):506–510. doi: 10.1152/jappl.1980.49.3.506. [DOI] [PubMed] [Google Scholar]
- 20.Celli BR, MacNee W, ATS, ERS Task Force Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–946. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 21.Foster GE, Sheel AW. The human diving response, its function, and its control. Scand J Med Sci Sports. 2005;15(1):3–12. doi: 10.1111/j.1600-0838.2005.00440.x. [DOI] [PubMed] [Google Scholar]
- 22.Mukhtar MR, Patrick JM. Ventilatory drive during face immersion in man. J Physiol. 1986;370:13–24. doi: 10.1113/jphysiol.1986.sp015919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paulev PE, Pokorski M, Honda Y, et al. Facial cold receptors and the survival reflex ‘‘diving bradycardia” in man. Jpn J Physiol. 1990;40(5):701–712. doi: 10.2170/jjphysiol.40.701. [DOI] [PubMed] [Google Scholar]
- 24.Argacha JF, Xhaet O, Gujic M, et al. Facial cooling and peripheral chemoreflex mechanisms in humans. Acta Physiol (Oxf) 2008;194(2):161–170. doi: 10.1111/j.1748-1716.2008.01876.x. [DOI] [PubMed] [Google Scholar]
- 25.National Emphysema Treatment Trial Research Group Cost effectiveness of lung volume reduction surgery for patients with severe emphysema. NEJM. 2003;348(21):2092–2102. doi: 10.1056/NEJMsa030448. [DOI] [PubMed] [Google Scholar]