Abstract
Purpose
We evaluated if cortical thickness measures were associated with surgical outcome in patients with non-lesional neocortical epilepsy.
Methods
Twenty-one young patients (age: 2.4–19.7 years) with epilepsy of neocortical origin and normal MRI underwent two-stage epilepsy surgery with subdural EEG monitoring. Cortical thickness was measured on presurgical volumetric MRI using the FreeSurfer software. The prognostic value of hemispheric and lobar/regional cortical thickness measures for 1-year and 2-year post-surgical seizure outcome has been analyzed.
Results
At one-year follow-up, 14 patients (67%) were seizure-free. Hemispheric and frontal lobe cortical thickness showed no/minimal asymmetry in seizure-free patients but thinner cortex ipsilateral to the seizure focus in those with recurrent seizures (p=0.02). More robust differences were found in patients ≥6 years of age (p=0.006 for frontal asymmetries), whose cortical thickness asymmetries remained prognostic for 2-year post-surgical outcome (p=0.007). By using an optimal cutoff threshold based on a receiver operating characteristic analysis, mean hemispheric asymmetry predicted one-year seizure freedom with 93% sensitivity and 71% specificity in the whole group, and with 100% sensitivity and 92% specificity in patients ≥6 years of age.
Conclusion
In patients with neocortical epilepsy and normal MRI, neocortical thinning in the epileptic hemisphere, particularly in frontal cortex, is associated with poor surgical outcome. Although these results require validation in a larger cohort prospectively, these data suggest that presurgical evaluation of cortical thickness may assist in identification of patients at high risk for surgical failure.
Keywords: Epilepsy, epilepsy surgery, frontal lobe, surgical outcome, MRI, cortical thickness
1. INTRODUCTION
Epilepsy surgery is a well-established treatment modality with a relatively high success rate for medically intractable epilepsy. Presence of a focal cortical abnormality on MRI is a good prognostic indicator for epilepsy surgery in such patients: a systematic review and meta-analysis found that the odds of seizure freedom are almost three times higher in the presence of a focal lesion [1]. However, patients who have normal findings on conventional imaging compose a challenging group with a higher rate of surgical failure. In such patients, advanced image acquisition and processing techniques may provide additional localizing and prognostic information during presurgical evaluation [2–5]. Recent software developments, such as FreeSurfer, allow for automated analysis of brain structural features including the measurement of cortical thickness on clinical MRI sequences [6–8]. This approach has previously revealed neocortical thinning in both temporal and extratemporal lobe epilepsy [9–13]. An earlier study of patients with temporal lobe epilepsy demonstrated that cortical thinning in distinct brain regions, even outside the presumed epileptogenic zone, is associated with poor surgical outcome [11]. In a recent study of adults with frontal lobe epilepsy, frontal cortical thinning was associated with poor surgical outcome in those with type I dysplasia [14]. However, the relationship between cortical thickness and surgical outcome has not been evaluated in patients with pediatric neocortical epilepsy and non-localizing conventional MRI. Therefore, in the present study we evaluated the association between cortical thickness and surgical outcome in young patients with neocortical epilepsy associated with non-localizing MRI. The overall goal of this study was to assess the feasibility of cortical thickness as an imaging marker of post-operative seizure risk in this very challenging patient population with no focal abnormalities on clinical MRI. Accurate prognostic markers in such patients could have a strong clinical impact during the presurgical evaluation.
2. MATERIAL AND METHODS
2.1. Subjects
We included 21 young patients (mean age: 9.9 years; range: 2.4–19.7 years) in the study, who fulfilled the following inclusion criteria: (i) medically refractory neocortical epilepsy based on electro-clinical studies; (ii) normal (non-localizing) clinical MRI, (iii) two-stage epilepsy surgery with chronic subdural EEG monitoring at the Children’s Hospital of Michigan (Detroit); (iv) at least 2-year postsurgical follow-up. Detailed clinical, EEG and imaging data of all subjects are presented in Table 1. Comorbidities included clinically significant cognitive/developmental delay (n=8), ADHD/hyperactivity (n=3) and depression (n=1). Five patients had a family history of epilepsy, and none of the patients had a history of febrile seizures or neonatal epilepsy. All patients were on antiepileptic medication in mono- or polytherapy (see details in Table 1). Before surgery, all patients underwent standard presurgical evaluation, as described recently [15]. In brief, all patients were evaluated with scalp ictal/interictal video-EEG, MRI, glucose metabolism positron emission tomography (PET) scans, and neuropsychological assessment. Subsequently, all cases were discussed in a weekly multidisciplinary epilepsy surgery conference where all these modalities were reviewed. Areas showing hypometabolism on PET (present in 18 patients, see details in Table 1) were inspected and no definite MRI abnormalities were found in those areas. At the end of the conference, a consensus was reached pertaining to candidacy for surgery and optimal surgical approach. The actual extent of resection was based on the results from chronic subdural EEG, with electrode coverage including at least some portions of all lobes in the affected hemisphere utilizing up to 128 subdural electrodes. Clinical data and clinically acquired images for these studies were used based on a protocol approved by the Wayne State University Institutional Review Board, and written informed consent was obtained from the patients (if >18 years of age) or from the parents or guardians (for children).
Table 1.
Detailed clinical data of the 21 patients, listed from the youngest to the oldest.
| Pt | Sex | Age at | Seizure type | AED | Scalp EEG focus localization* | FDG-PET focus | Resection | Histopathology | Seizure freedom 1-year | Seizure freedom 2-year | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Onset | MRI | Localization | Localized ictal onset? | Side | Lobe(s) | ||||||||
| 1 | M | 1.5y | 2.4y | ES | CLO,VPA | hemi | no | multilobar | R | ftpo | gliosis | yes | yes |
| 2 | M | 0.5y | 2.5y | CPS,ATON | OXC,LEV,ZON | tpo | yes | multilobar | L | fto | gliosis | yes | yes |
| 3 | F | 0.4y | 3.8y | CPS | TPX,VPA | hemi | no | multilobar | L | tpo | gliosis | no | no |
| 4 | M | 2.4y | 4.9y | CPS | VPA,ZON | frontal | yes | single | L | f | fcdIIA | yes | yes |
| 5 | M | 2.5y | 5.3y | SPS | OXC | parietal | n/a | multilobar | R | p | gliosis | yes | yes |
| 6 | F | 5.3y | 5.7y | CPS,GTCS | TPX | hemi | n/a | single | R | tpo | fcd IA | yes | yes |
| 7 | M | 1.8y | 5.9y | CPS | ZON,FEB,VPA | hemi | no | none | L | fto | gliosis | yes | no |
| 8 | F | 1.8y | 6.0y | ES | LAM | frontal | n/a | none | R | f | gliosis | yes | yes |
| 9 | M | 2.0y | 6.7y | CPS | OXC,LEV,VPA | fp | yes | single | R | fp | gliosis | yes | yes |
| 10 | F | 5.0y | 6.9y | CPS,GTCS | OXC,ZON | tpo | yes | multilobar | L | ftpo | gliosis | no | no |
| 11 | M | 7.6y | 8.1y | SPS | LAM,ZON | nomalEEG | n/a | multilobar | R | f | fcd IA | yes | no |
| 12 | F | 6.6y | 8.9y | SPS | OXC,CLR | ft | yes | multilobar | L | f | fcd IA | yes | yes |
| 13 | F | 4.0y | 10.9y | CPS | LAM,LEV | ft | yes | multilobar | R | fto | mMCD | yes | yes |
| 14 | F | 6.0y | 11.7y | CPS | OXC,LEV | ft | yes | multilobar | R | ft | fcd(t)IBgliosis(f)mMCD | yes | yes |
| 15 | M | 7.5y | 13.6y | CPS | LAM,OXC | temporal | yes | multilobar | L | t | no | no | |
| 16 | F | 0.3y | 13.8y | CPS | LEV,LAM,OXC | tpo | yes | single | R | tpo | gliosis | no | no |
| 17 | F | 9.2y | 15.2y | CPS | OXC | hemi | no | multilobar | R | p | gliosis | no | no |
| 18 | F | 14.0y | 15.5y | SPS | OXC | temporal | yes | single | R | t | gliosis | no | no |
| 19 | F | 2.0y | 16.2y | CPS | KLO,TPX,PHT | hemi | no | single | R | f | gliosis | no | no |
| 20 | F | 0.9y | 17.0y | CPS | LAM,KLO | frontal | yes | none | L | f | gliosis | yes | yes |
| 21 | F | 4.0y | 19.7y | CPS | OXC,LAM,TPX | frontal | yes | multilobar | R | P | gliosis | yes | no |
Abbreviations: Pt: patient; y: year(s); M: male; F: female; hemi: hemispheric; R: right; L: left; f: frontal; t: temporal; p: parietal; o: occipital; fcd: focal cortical dysplasia; mMCD: mild malformation of cortical development; ES: epileptic spams; ATON: atonic seizures; CPS: complex partial seizures; SPS: simple partial seizures; GTCS: generalized tonic-clonic seizures; AED: anti epileptic drugs; CLO: clobazam; VPA: valproic acid; OXC: oxcarbazepine; LEV: levetiracetam; ZON: zonisamide; TPX: topiramate; FEB: felbamate; LAM: lamotrigine; CLR: clorazepate; KLO: klonopin; PHT: phenytoin. n/a: no ictal EEG could be obtained, scalp EEG localization was based on interictal data.
Scalp EEG findings (if localized) and resection were always localized on the same side.
2.2. MRI acquisition
For the clinical epilepsy MR scanning protocol, a 3T GE-Signa scanner (GE Healthcare, Milwaukee, WI) equipped with an 8-channel head coil was utilized to acquire multiple sequences, including axial T1- and T2-weighted, as well as coronal fluid attenuation inversion recovery (FLAIR) images. In addition, a three-dimensional fast-spoiled gradient recalled-echo sequence (FSPGR) was acquired at TR/TE/TI of 9.12/3.66/400 ms, with slice thickness of 1.2 mm, and planar resolution of 0.94×0.94 mm2. MRI acquired within 6 months before the surgery was utilized for cortical thickness measurements. Young children (below age 12 years) were sedated and monitored during the MRI scanning using the pediatric sedation protocol of the Children’s Hospital of Michigan.
2.3. MR image analysis
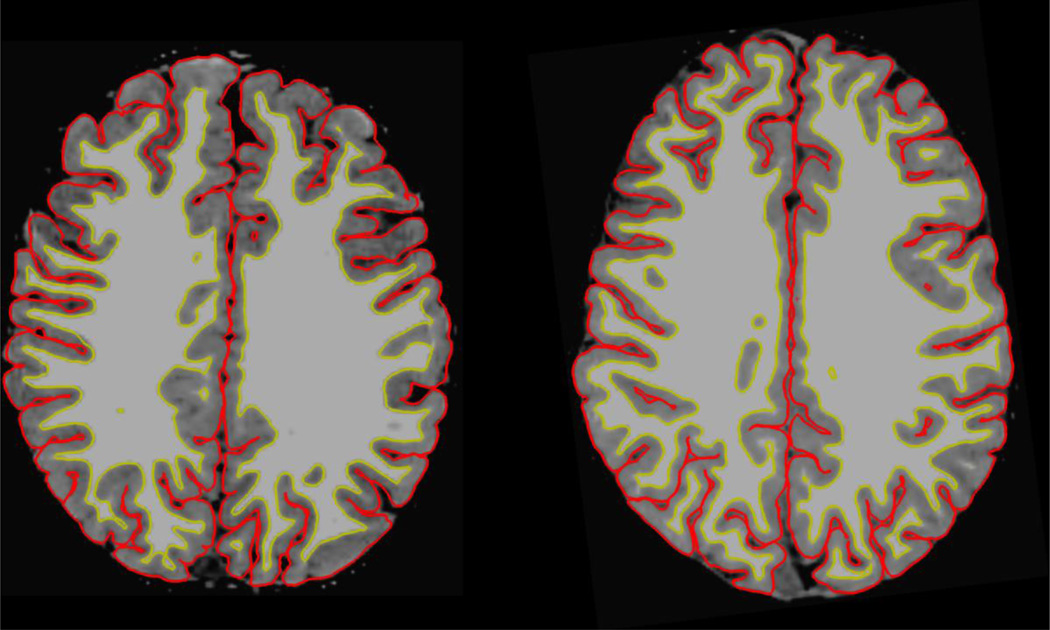
First, the scans were inspected to exclude significant motion or other artifacts. Cortical reconstruction and segmentation (area and volume) were performed using Free Surfer (Version 5.3, http://surfer.nmr.mgh.harvard.edu), as described previously [6–8, 16–19]. In brief, the downstream processing after transferring the FSPGR images to a workstation involved motion correction of volumetric T1-weighted images, removal of non-brain tissue using a hybrid watershed/surface deformation procedure [20], automated Talairach transformation of each subject's native brain, and segmentation of the gray matter–white matter volumetric structures [17]. This was followed by an automated process of inflation of the cortical surface to an average spherical surface to locate both the pial surface and the gray matter–white matter boundary, intensity normalization, and automated topology correction [21]. For each subject, the gray and white matter segmentation (Figure 1) was then inspected and segmentation errors were fixed semi-manually by assigning white matter control points to the affected regions followed by reiteration of the FreeSurfer pipeline from the white matter segmentation checkpoint. After all segmentations passed the quality check, the cerebral cortex of each patient was parcellated into hemispheres, as well as into entire lobes (frontal, parietal, temporal, occipital) and sublobar regions [17], and mean cortical thickness was computed for each of these regions [8]. Cortical thickness asymmetry indices (AIs) were calculated for each of the above regions using the following formula: [(Affected side − Unaffected side) / (Affected side + Unaffected side)* 100], where the side of surgical resection was designated as the affected side.
Figure 1.
Examples of gray and white matter segmentation results of a 2.4-year-old (patient 1#; left) and a 16.2-year old child (patient 19#, right).
2.4. Statistical analysis
First, the patients’ age at the onset of epilepsy, age at MRI acquisition and the duration of epilepsy were correlated with cortical thickness values and AIs using Pearson’s correlations. Unpaired t-tests were used to compare clinical variables (age, age at epilepsy onset, duration of epilepsy) as well as hemispheric and lobar thickness values and AIs between patients who achieved sustained seizure-freedom for at least 1 year vs. those with recurrent seizure(s) before the one-year follow-up mark. This was repeated for 2-year outcome data. The group analysis was also repeated for several subgroups: i. in children 6 years and older, (n=14) where FreeSurfer has been validated before [22]; ii. in patients with no cortical malformation found on histopathology (n=14, all showed non-specific gliosis, Table 1), to exclude the effect of variability of pathology; iii. in patients who had no valproate treatment at the time of the presurgical evaluation (n=16), because of the known effect of this drug on parietal cortical thickness [23]; iv. in subgroups of patients who had frontal, temporal, or parietal lobe involved in the resection. Only eight patients had the occipital lobe included in the resection, thus, this subgroup was not analyzed separately.
In addition, a receiver operating characteristic (ROC) analysis was performed to evaluate the performance of cortical thickness asymmetries to separate the binary outcome variable (seizure-free vs. not seizure-free) at different thickness threshold values. We calculated the area under the curve (AUC), a summary measure reflecting the efficiency of outcome prediction of the cortical thickness parameters. The most accurate cutoff threshold was established, and sensitivity, specificity along with positive predictive values (PPV) were calculated for predicting one-year seizure recurrence. Finally, chi-square tests were used to analyze the relation of one-year outcome with electro-clinical and imaging variables previously found to be significant prognostic factors in neocortical epilepsy surgery in a large study [24], such as (i) localized ictal seizure onset on scalp EEG (ii) focal hypometabolism on FDG-PET, (iii) side of the resection (right vs. left), (iv) unilobar vs. multilobar epileptic focus, and (v) absence of cortical dysplasia on histopathology. Since all of these parameters failed to predict one-year outcome in the present study (p>0.2 in all comparisons), further multivariate analyses were not performed. Statistical assessment was carried out using SPSS 22.0. P-values below 0.05 were considered significant.
3. RESULTS
3.1. Correlation of cortical thickness with age and duration of epilepsy
Both age at MRI and epilepsy duration showed a negative correlation with occipital lobe thickness in both the affected (R=−0.62, p=0.003; R=−0.49, p=0.03, respectively) and unaffected (R=−0.54, p=0.01; R=−0.47, p=0.03, respectively) hemispheres; similar trends were seen in other lobes without reaching statistical significance. In addition, age also showed a negative correlation with hemispheric cortical thickness (R=−0.46, p=0.04). In contrast, lobar and hemispheric cortical thickness AI values were age-independent (p>0.1 in all correlations). Age at epilepsy onset did not correlate with cortical thickness parameters in any brain region. Age, age at epilepsy onset and duration of epilepsy were not significantly different between patients with vs. without 1-year or 2-year seizure freedom, although the 2-year seizure-free group showed a strong trend toward being younger at the time of the MRI than those who had recurrent seizures (7.4 years vs. 11.9 years, p=0.05).
3.2. Association between cortical thickness and epilepsy surgery outcome
3.2.1. Whole group analysis
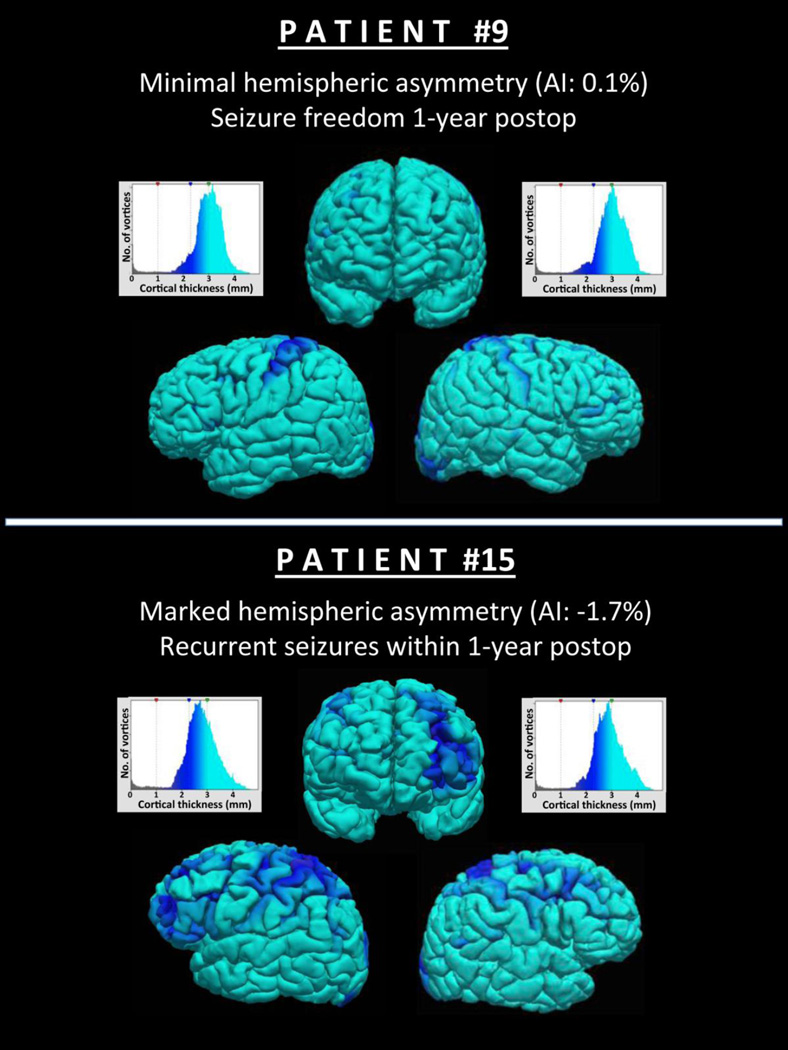
At the one-year follow-up, 14 patients (67%) remained seizure-free. Absolute cortical thickness values of the studied lobes in the affected or unaffected hemisphere did not differ between outcome groups. In contrast, hemispheric and frontal lobe cortical thickness AIs were significantly different among these groups at one-year follow-up (p=0.02), with minimal to no asymmetry in the seizure-free, and lower, often negative, AIs (i.e., greater asymmetry, with lower values on the affected side) in those with seizure recurrence (Table 2, Figure 2). Within the frontal lobe, regions showing a significant group difference included the rostral middle frontal (p=0.018) and lateral orbital cortex (p=0.024), as well as the pars triangular is (p=0.016) (Figure 3).
Table 2.
Comparison of cortical thickness asymmetry index (AI, %) in seizure-free and recurrent seizures (at 1-year follow-up) in the whole group and in three subgroups: children above age 6 years (n=14), children with no cortical dysplasia (only gliosis) on histopathology (n=14), and children who were not treated by valproate (n=16).
| Whole group | Seizure-free (n=14) | Recurrent sz (n=7) | P |
| Hemispheric AI Frontal lobe AI |
0.0±0.7% 0.1±1.9% |
−1.1±1.3% −2.3±2.5% |
0.02 0.02 |
|
Age 6 years and older |
Seizure-free (n=8) | Recurrent sz (n=6) | P |
| Hemispheric AI Frontal lobe AI |
0.1 ±0.5% 0.6±1.4% |
−1.4±1.1% −2.8±2.4% |
0.007 0.006 |
| Gliosis only* | Seizure-free (n=8) | Recurrent sz (n=6) | P |
| Hemispheric AI Frontal lobe AI Parietal lobe AI |
0.4±0.6% 0.4±1.0% 0.4±1.0% |
−1.0±1.4% 2.7±2.7% −2.1 ±2.7% |
0.025 0.029 0.029 |
|
No valproate treatment |
Seizure-free (n=10) | Recurrent sz (n=6) | P |
| Hemispheric AI Frontal lobe AI |
0.04±0.6 0.6±1.2% |
−1.4±1.0% −2.8±2.4% |
0.005 0.002 |
sz: seizures; y=years
no cortical dysplasia on histopathology
Figure 2.
Three-dimensional rendering of MRI-derived brains with cortical thickness values projected to the surface, from a subject with minimal hemispheric cortical thickness asymmetry and seizure freedom one year after epilepsy surgery (patient #9) and from a subject with marked asymmetry and seizure recurrence within 1 year (patient #15). Dark blue represents thinner, whereas light blue represents thicker cortical regions, as indicated by histograms positioned adjacent to their corresponding hemispheres. The y-axis of the histograms shows the number of vortices with the cortical thickness value shown on the x-axis.
Figure 3.
3D inflated cortical surface showing the three frontal regions, where cortical thickness asymmetries predicted 1-year seizure-free outcome. Red: rostral middle frontal; magenta: pars triangular is; yellow: lateral orbital cortex.
At 2-year follow-up, 11 patients (52%) remained seizure-free. Because of the age difference described above, age was included as a co-variate in the group comparisons. In this analysis, frontal cortical thickness AIs showed a trend for a difference between the seizure-free and not seizure-free groups (0.2±2.5% vs. −1.7±2.3%, respectively, p=0.068).
3.2.2. Subgroup analyses
The repeated analysis for 1-year outcome, with only patients age six years and older (n=14, 8 seizure-free) showed similar group differences with lower p-values (p<0.01; Table 2). In addition, in patients with only gliosis on histopathology (n=14, 8 seizure-free) symmetric hemispheric cortical (p=0.025), frontal and parietal (p=0.029 for both) were significant predictors of seizure freedom (Table 2). In patients with no sodium valproate treatment (n=16), both whole brain and frontal cortical AI differences between the 1-year outcome groups were highly significant (p=0.005 and p=0.002, respectively) (Table 2). Subgroup analysis by resection lobes showed that both the mean hemispheric and frontal cortical thickness AIs differed among one-year outcome groups in those with frontal (p=0.005 and p=0.006, respectively), and parietal (p=0.03 and p=0.01, respectively) resections. In those who had temporal lobe resection, only the frontal AI showed a moderate difference according to seizure freedom (p=0.06).
In the 2-year outcome comparisons, both whole brain and frontal cortical thickness AIs predicted seizure-freedom in the non-valproate group (p=0.013 and p=0.003, respectively) and also in patients 6 years and above (p=0.019 and p=0.007, respectively), even after including age as a co-variate.
3.2.3. ROC analysis
On the ROC analysis performed in the whole group, a cut-off value of −0.6% for the hemispheric thickness AI and −1.7% for the frontal cortical thickness AI were identified to be the most accurate for prediction of one-year seizure freedom (hemispheric: p=0.02, AUC = 0.88; frontal: p=0.014, AUC = 0.90). Using the optimal threshold, mean hemispheric AIs predicted surgical outcome with the respective sensitivity and PPV of 93%/83% in the whole population (specificity: 71%). In the subgroup of patients age 6 and older, sensitivity and PPV were 100%, with a specificity of 83% (Table 3).
Table 3.
ROC analysis results for cortical thickness asymmetry indices (AIs) and 1-year outcome prediction
| Region | Cut-off AI | AUC | Sens. | Spec. | PPV | |
|---|---|---|---|---|---|---|
|
Whole population |
Hemispheric Frontal lobe |
−0.6% −1.7% |
78% 79% |
93% 86% |
71% 71% |
83% 71% |
|
Age 6 years and older |
Hemispheric Frontal lobe |
−0.6% −1.7% |
88% 90% |
100% 100% |
83% 83% |
100% 100% |
AUC: area under the curve; Sens.: sensitivity; Spec: specificity; PPV: positive predictive value.
4. DISCUSSION
Our results provide preliminary evidence that cortical thinning in the affected (epileptic) hemisphere and, specifically, in the frontal lobe, relative to the unaffected side, is strongly associated with post-operative seizure recurrence in children with neocortical epilepsy and non-localizing MRI. The studied patient group was heterogeneous in terms of lobar focus location and histopathology, but the observed differences were consistently present in all studied subgroups, regardless of pathology, lobe of resection or valproate treatment. Frontal and hemispheric cortical thickness asymmetries distinguished outcome groups and predicted one-year seizure recurrence with a high positive predictive value, especially for children aged six years and older. The prognostic value of these cortical thickness asymmetries was still present for the 2-year outcome, especially in older children. While the studied subgroups were particularly small, these results suggest that future, prospective studies may include patients with various neocortical foci and underlying etiology and could also address if cortical thickness asymmetries are prognostic in young children.
4.1. Methodologic considerations
Utilization of asymmetries in our study was an integral part of the study design. It served the purpose of excluding inter-individual confounding factors associated with the image processing technique used. Also, the study population included young children; therefore, we did not have an age-matched healthy controls. Even if such controls were available, there could be large inter-individual variations of absolute values of the thickness measures that age matching could not completely counterbalance.
An additional consideration is that acquisition of adequate quality images without a considerable amount of motion artifacts may be difficult in small children and often requires sedation, which is not justified for healthy non-epileptic children. Furthermore, although FreeSurfer cortical thickness measures are close to measures obtained on actual histology [25], motion artifacts can alter MRI-based thickness values even after thorough visual inspection and quality control [26]. Head motion can decrease the measured cortical thickness, which could lead to underestimation of thickness in non-sedated children compared to sedated patients. The use of asymmetry indices improves signal-to-noise ratio by normalization for both developmental differences and measurement errors due to differing amounts of head motion across patients.
The measured cortical asymmetries in our group were small. This is likely explained by the relatively large regions included in the analysis. Previous studies also demonstrated subtle cortical thickness asymmetries in healthy subjects, particularly in young children: in a large cross-sectional study of healthy children and adults (age range: 5–59 years), minimal cortical thickness asymmetries were found in most brain regions of children below age 15, while increased laterality emerged in several clusters in older subjects, especially in adults [27]. Therefore, while the measured asymmetries in our cohort were relatively small, they may have exceeded normal asymmetries, especially in those who had post-operative seizures.
The use of asymmetries also has some inherent limitations. Theoretically, lower values on the affected side (epileptic hemisphere) may occur not only by ipsilateral cortical thinning but also due to higher values (cortical thickening) in the contralateral cortex. However, most previous studies (discussed in detail below) found cortical thinning in various groups with focal epilepsy; contralateral cortical thickening was recently reported in frontal lobe epilepsy associated with type II cortical dysplasia [14], a pathology present only in one of our 21 patients. Therefore, it is unlikely that the observed, prognostic asymmetries were due to contralateral cortical thickening in our patient cohort.
4.2. Pathophysiologic considerations
Despite the heterogeneity of lobar localization of epileptic foci in our patients, cortical thinning in the frontal lobe of the affected hemisphere appears to have the strongest impact on surgery outcome. This finding is rather consistent with the results of a recent study demonstrating that frontal cortical thinning predicts poor surgical outcome in patients with frontal lobe epilepsy associated with type I cortical dysplasia [14]. In the present study, one third of the patients had histologically verified cortical malformation, mostly type I dysplasia or mild malformation of cortical development (see Table 1). In two-thirds of our cases, histopathology revealed no etiology; this could be due to sampling error in some cases, but the lack of MRI abnormalities make the presence of type II dysplasia or other macroscopic lesions unlikely. Additional regional analysis suggested that the frontal lobe findings were mostly driven by three, adjacent prefrontal cortical regions. This frontal localization was different from the medial frontal areas that predicted seizure outcome in the previous, frontal lobe epilepsy study [14], which is likely related to our different patient population.
Cortical thinning in the epileptic brain may be caused by repeated seizures or due to underlying pathology. The latter is supported by a study in children with new-onset focal epilepsy that reported reduced cortical thickness, mostly affecting the frontal lobes [28]. Early onset cortical thinning, predominantly in the left hemisphere, was also observed in children with rolandic epilepsy [29]. Another study, including children with intractable frontal lobe epilepsy, found bilateral cortical thinning in widespread multilobar regions regardless of the laterality of the presumed seizure focus [12]. A longitudinal study of adult patients with pharmacoresistant temporal lobe epilepsy demonstrated progressive cortical thinning in extratemporal regions, including various ipsi- and contralateral areas [30]. The presence of such widespread abnormalities suggests network level changes that could explain the findings of the present study as well.
Beyond the effect of epilepsy, possible mechanisms of cortical thinning include drug effects: e.g., parietal cortex cortical thinning has been reported in valproate users [23]. In our study, however, the group differences of cortical thickness asymmetries remained highly significant when we excluded the valproate users. Another confounding factor could be epilepsy-associated anxiety: a recent study of 25 children with recent-onset epilepsy and anxiety disorder demonstrated thinning in bilateral orbital frontal and prefrontal cortex [31]. Although we did not have detailed neuropsychology data on anxiety, only one patient had clinically diagnosed depression in our cohort. Nevertheless, the effect of chronic anxiety and depression in children with intractable epilepsy needs to be addressed in future studies.
4.3. Potential clinical implications
The results of this study corroborate previous evidence associating neocortical epilepsy and extensive structural cortical changes [9–12]. The present findings also suggest that cortical thickness asymmetries may be used as an objective MRI biomarker to assist in the prediction of epilepsy surgery outcomes in young patients with neocortical epilepsy, where conventional MRI provides no localizing information (which otherwise would be a useful prognostic imaging variable) [24]. Since measurement of hemispheric and cortical thickness utilizes standard MR imaging routinely acquired during presurgical work-up, it could improve cost-efficiency and decrease morbidity secondary to futile invasive efforts while seamlessly incorporated into the current workflow. However, the current study sample was limited and heterogeneous in terms of focus localization. Therefore, the findings will need to be confirmed prospectively in a separate, larger patient population.
In conclusion, these findings indicate that neocortical thinning in the epileptic hemisphere, particularly in the frontal cortex, is associated with poor surgical outcome in patients with neocortical epilepsy and non-localizing MRI. If the findings can be confirmed prospectively in a larger patient group, presurgical evaluation of cortical thickness may assist in identification of patients at high risk for surgical failure.
Highlights.
Decreased ipsilateral cortical thickness predicts post-operative seizures
Cortical thickness asymmetries may predict seizure-free outcome with around 90% accuracy when using an optimized threshold
Cortical thickness asymmetries in the frontal lobe have the strongest prognostic value
Acknowledgments
This study was partially supported by grants from the National Institutes of Health (R01 NS089659 to J.J. and R01 NS064033 to E.A.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: None.
REFERENCES
- 1.Tellez-Zenteno JF, Hernandez Ronquillo L, Moien-Afshari F, Wiebe S. Surgical outcomes in lesional and non-lesional epilepsy: a systematic review and meta-analysis. Epilepsy research. 2010;89(2–3):310–318. doi: 10.1016/j.eplepsyres.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Shah AK, Mittal S. Evaluation of magnetic resonance imaging-negative drug-resistant epilepsy. Ann Indian Acad Neurol. 2014;17(Suppl 1):S80–S88. doi: 10.4103/0972-2327.128667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seo JH, Noh BH, Lee JS, Kim DS, Lee SK, Kim TS, Kim SH, Kang HC, Kim HD. Outcome of surgical treatment in non-lesional intractable childhood epilepsy. Seizure. 2009;18(9):625–629. doi: 10.1016/j.seizure.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Hong KS, Lee SK, Kim JY, Lee DS, Chung CK. Pre-surgical evaluation and surgical outcome of 41 patients with non-lesional neocortical epilepsy. Seizure. 2002;11(3):184–192. doi: 10.1053/seiz.2001.0616. [DOI] [PubMed] [Google Scholar]
- 5.Govindan RM, Asano E, Juhasz C, Jeong JW, Chugani HT. Surface-based laminar analysis of diffusion abnormalities in cortical and white matter layers in neocortical epilepsy. Epilepsia. 2013;54(4):667–677. doi: 10.1111/epi.12129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999;9(2):179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- 7.Fischl B, Sereno MI, Dale AM. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage. 1999;9(2):195–207. doi: 10.1006/nimg.1998.0396. [DOI] [PubMed] [Google Scholar]
- 8.Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci U S A. 2000;97(20):11050–11055. doi: 10.1073/pnas.200033797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin JJ, Salamon N, Lee AD, Dutton RA, Geaga JA, Hayashi KM, Luders E, Toga AW, Engel J, Jr, Thompson PM. Reduced neocortical thickness and complexity mapped in mesial temporal lobe epilepsy with hippocampal sclerosis. Cereb Cortex. 2007;17(9):2007–2018. doi: 10.1093/cercor/bhl109. [DOI] [PubMed] [Google Scholar]
- 10.Mueller SG, Laxer KD, Barakos J, Cheong I, Garcia P, Weiner MW. Widespread neocortical abnormalities in temporal lobe epilepsy with and without mesial sclerosis. Neuroimage. 2009;46(2):353–359. doi: 10.1016/j.neuroimage.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernhardt BC, Bernasconi N, Concha L, Bernasconi A. Cortical thickness analysis in temporal lobe epilepsy: reproducibility and relation to outcome. Neurology. 2010;74(22):1776–1784. doi: 10.1212/WNL.0b013e3181e0f80a. [DOI] [PubMed] [Google Scholar]
- 12.Widjaja E, Mahmoodabadi SZ, Snead OC, 3rd, Almehdar A, Smith ML. Widespread cortical thinning in children with frontal lobe epilepsy. Epilepsia. 2011;52(9):1685–1691. doi: 10.1111/j.1528-1167.2011.03085.x. [DOI] [PubMed] [Google Scholar]
- 13.Kemmotsu N, Girard HM, Bernhardt BC, Bonilha L, Lin JJ, Tecoma ES, Iragui VJ, Hagler DJ, Jr, Halgren E, McDonald CR. MRI analysis in temporal lobe epilepsy: cortical thinning and white matter disruptions are related to side of seizure onset. Epilepsia. 2011;52(12):2257–2266. doi: 10.1111/j.1528-1167.2011.03278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong SJ, Bernhardt BC, Schrader DS, Bernasconi N, Bernasconi A. Whole-brain MRI phenotyping in dysplasia-related frontal lobe epilepsy. Neurology. 2016;86(7):643–650. doi: 10.1212/WNL.0000000000002374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chugani HT, Asano E, Juhasz C, Kumar A, Kupsky WJ, Sood S. "Subtotal" hemispherectomy in children with intractable focal epilepsy. Epilepsia. 2014;55(12):1926–1933. doi: 10.1111/epi.12845. [DOI] [PubMed] [Google Scholar]
- 16.Fischl B, Salat DH, van der Kouwe AJ, Makris N, Segonne F, Quinn BT, Dale AM. Sequence-independent segmentation of magnetic resonance images. Neuroimage. 2004;23(Suppl 1):S69–S84. doi: 10.1016/j.neuroimage.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Fischl B, van der Kouwe A, Destrieux C, Halgren E, Segonne F, Salat DH, Busa E, Seidman LJ, Goldstein J, Kennedy D, Caviness V, Makris N, Rosen B, Dale AM. Automatically parcellating the human cerebral cortex. Cereb Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- 18.Fischl B, Sereno MI, Tootell RB, Dale AM. High-resolution intersubject averaging and a coordinate system for the cortical surface. Hum Brain Mapp. 1999;8(4):272–284. doi: 10.1002/(SICI)1097-0193(1999)8:4<272::AID-HBM10>3.0.CO;2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, van der Kouwe A, Killiany R, Kennedy D, Klaveness S, Montillo A, Makris N, Rosen B, Dale AM. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33(3):341–355. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- 20.Segonne F, Dale AM, Busa E, Glessner M, Salat D, Hahn HK, Fischl B. A hybrid approach to the skull stripping problem in MRI. Neuroimage. 2004;22(3):1060–1075. doi: 10.1016/j.neuroimage.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 21.Segonne F, Pacheco J, Fischl B. Geometrically accurate topology-correction of cortical surfaces using nonseparating loops. IEEE Trans Med Imaging. 2007;26(4):518–529. doi: 10.1109/TMI.2006.887364. [DOI] [PubMed] [Google Scholar]
- 22.Ghosh SS, Kakunoori S, Augustinack J, Nieto-Castanon A, Kovelman I, Gaab N, Christodoulou JA, Triantafyllou C, Gabrieli JD, Fischl B. Evaluating the validity of volume-based and surface-based brain image registration for developmental cognitive neuroscience studies in children 4 to 11 years of age. Neuroimage. 2010;53(1):85–93. doi: 10.1016/j.neuroimage.2010.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pardoe HR, Berg AT, Jackson GD. Sodium valproate use is associated with reduced parietal lobe thickness and brain volume. Neurology. 2013;80(20):1895–1900. doi: 10.1212/WNL.0b013e318292a2e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yun CH, Lee SK, Lee SY, Kim KK, Jeong SW, Chung CK. Prognostic factors in neocortical epilepsy surgery: multivariate analysis. Epilepsia. 2006;47(3):574–579. doi: 10.1111/j.1528-1167.2006.00470.x. [DOI] [PubMed] [Google Scholar]
- 25.Cardinale F, Chinnici G, Bramerio M, Mai R, Sartori I, Cossu M, Lo Russo G, Castana L, Colombo N, Caborni C, De Momi E, Ferrigno G. Validation of FreeSurfer-estimated brain cortical thickness: comparison with histologic measurements. Neuroinformatics. 2014;12(4):535–542. doi: 10.1007/s12021-014-9229-2. [DOI] [PubMed] [Google Scholar]
- 26.Reuter M, Tisdall MD, Qureshi A, Buckner RL, van der Kouwe AJ, Fischl B. Head motion during MRI acquisition reduces gray matter volume and thickness estimates. Neuroimage. 2014;107C:107–115. doi: 10.1016/j.neuroimage.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou D, Lebel C, Evans A, Beaulieu C. Cortical thickness asymmetry from childhood to older adulthood. Neuroimage. 2013;83:66–74. doi: 10.1016/j.neuroimage.2013.06.073. [DOI] [PubMed] [Google Scholar]
- 28.Widjaja E, S ZM, Go C, Raybaud C, Chuang S, Snead OC, Smith ML. Reduced cortical thickness in children with new-onset seizures. AJNR Am J Neuroradiol. 2012;33(4):673–677. doi: 10.3174/ajnr.A2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Overvliet GM, Besseling RM, Jansen JF, van der Kruijs SJ, Vies JS, Hofman PA, Ebus SC, de Louw A, Aldenkamp AP, Backes WH. Early onset of cortical thinning in children with rolandic epilepsy. Neuroimage Clin. 2013;2:434–439. doi: 10.1016/j.nicl.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernhardt BC, Worsley KJ, Kim H, Evans AC, Bernasconi A, Bernasconi N. Longitudinal and cross-sectional analysis of atrophy in pharmacoresistant temporal lobe epilepsy. Neurology. 2009;72(20):1747–1754. doi: 10.1212/01.wnl.0000345969.57574.f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jones JE, Jackson DC, Chambers KL, Dabbs K, Hsu DA, Stafstrom CE, Seidenberg M, Hermann BP. Children with epilepsy and anxiety: Subcortical and cortical differences. Epilepsia. 2015;56(2):283–290. doi: 10.1111/epi.12832. [DOI] [PMC free article] [PubMed] [Google Scholar]