Abstract
Introduction
Though preventing recurrent violent injury is an important component of a public health approach to interpersonal violence, and a common focus of violence intervention programs, the true incidence of recurrent violent injury is unknown. Prior studies have reported recurrence rates from 0.8% to 44%, and risk factors for recurrence are not well established.
Methods
We used a statewide, all-payer database to perform a retrospective cohort study of emergency department visits for injury due to interpersonal violence in Florida, following patients injured in 2010 for recurrence through 2012. We assessed risk factors for recurrence with multivariable logistic regression and estimated time to recurrence with the Kaplan-Meier method. We tabulated hospital charges and costs for index and recurrent visits.
Results
Of 53,908 patients presenting for violent injury in 2010, 11.1% had a recurrent violent injury during the study period. Trauma centers treated 31.8%, including 55.9% of severe injuries. Among recurrers, 58.9% went to a different hospital for their second injury. Low income, homelessness, Medicaid or uninsurance, and Black race were associated with increased odds of recurrence. Patients with visits for mental and behavioral health and unintentional injury also had increased odds of recurrence. Index injuries accounted for $105 million in costs, and recurrent injuries accounted for another $25.3 million.
Conclusions
Recurrent violent injury is a common and costly phenomenon, and effective violence prevention programs are needed. Prevention must include the non-trauma centers where many patients seek care.
Keywords: recurrent violent injury, injury epidemiology
1. Introduction
Interpersonal violence caused 16,671 deaths, 140,343 hospitalizations, and 1,615,995 emergency department visits in the US in 2010, for a cumulative $8.5 billion in medical costs.1 Violence is increasingly understood as a public health issue with a broad impact on individual and community health.2 Recurrent injury is a promising target for prevention, as prior injury is a predictor of future violent injury3 and death.4–6 Hospital-based violence intervention programs show promising results with in reducing re-injury and costs by using an initial injury visit to initiate prevention,7,8 but appropriately scaling and distributing violence prevention resources requires a more accurate understanding of the incidence, risk factors, and impact of recurrent violent injury.
Although recurrent violent injury has been studied since the 1980s, prior studies have tracked recurrent visits limited to an individual trauma center,7,9–16 a particular intervention or cohort study,17–19 or a local area,3,20,21 and many have combined results for both violent and nonviolent injuries. Most report a rate of recurrence of 10–25% over 2–5 years.10–15,20,22–24 At the population level, one study showed a 0.8% incidence of recurrence over six years in San Diego County,25 and another found a 2.0% incidence in Nevada over five years.26 These two studies included both violent and nonviolent injuries, and were limited to severely injured patients. A prospective cohort study in Detroit showed a 44% rate of recurrence and a 20% rate of death within five years for violently injured individuals.3 A population-based study in Philadelphia that included both violently and nonviolently injured patients showed a 14% rate of recurrent injury over 4 years.21 A recent, prospective cohort study of violently injured youth in Flint, Michigan that incorporated the full range of injury severity found a 37% recurrence rate within 2 years.27 Past studies have reported costs of recurrent violent injuries in small cohorts,7,8 but not population-level costs. Although many injured patients are treated in non-trauma center hospitals,28 these institutions’ role in violence prevention is not established.
Understanding the health and economic impacts of recurrent violent injury at a population level is critical for clinicians to identify and intervene with high-risk individuals, and for the health care system to allocate violence prevention resources appropriately. To this end, we performed a retrospective cohort study of all ED visits for injury resulting from interpersonal violence in a large U.S state to provide a comprehensive assessment of the incidence of recurrent violent injury, the site of care and acute care costs of these injuries, and demographic and clinical factors associated with risk of recurrence.
2. Methods
2.1 Study design and data source
We conducted a retrospective cohort study of all patients presenting to an ED or admitted to a hospital in Florida in 2010 for injuries due to interpersonal violence, and followed these patients for recurrence through the end of 2012. We used data from The Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) State Emergency Department Database (SEDD) includes all ED discharges. The State Inpatient Database (SID) includes all hospital admissions. Combined, these two databases include all ED visits to nonfederal hospitals. This analysis utilizes the HCUP revisit variables visitlink and daystoevent, which allows tracking of individual patients across years and hospitals.29,30 We include data from Florida from 1/2010-12/2012, as Florida collects relevant risk factors; is one of eight states to report person identifiers;31 and has robust revisit variables, with >95% verified.32 Based on prior studies,20,26 we expected three years to capture most recurrences, while being short enough for trauma centers and violence prevention programs to feasibly replicate. This study was deemed exempt by the University of Pennsylvania Institutional Review Board.
2.2 Population
We identified all patients presenting for violent injury to a Florida hospital, excluding out-of-state residents. Visits missing revisit variables were excluded from the analysis as recurrence could not be assessed. We used HCUP Clinical Classification Software (CCS) to identify all visits with an ICD-9 diagnosis code associated with injury, excluding poisonings and complications of medical treatment or devices, (Summarizing 2,721 ICD-9 codes into CCS codes 225–236, 239, 240 and 244; see Supplementary Table),33 and an external cause-of-injury code (E-code) indicating interpersonal violence as the cause, as classified by the CDC.34 Injuries due to intimate partner violence were included. Florida has mandated e-coding in hospital discharge data since 1997 and in emergency department discharge data since 2005,35 and over 95% of Florida inpatient and ED discharges with an injury diagnosis include an e-code.36,37 E-codes have been validated 95% accurate with respect to injury intent, compared to chart review.38
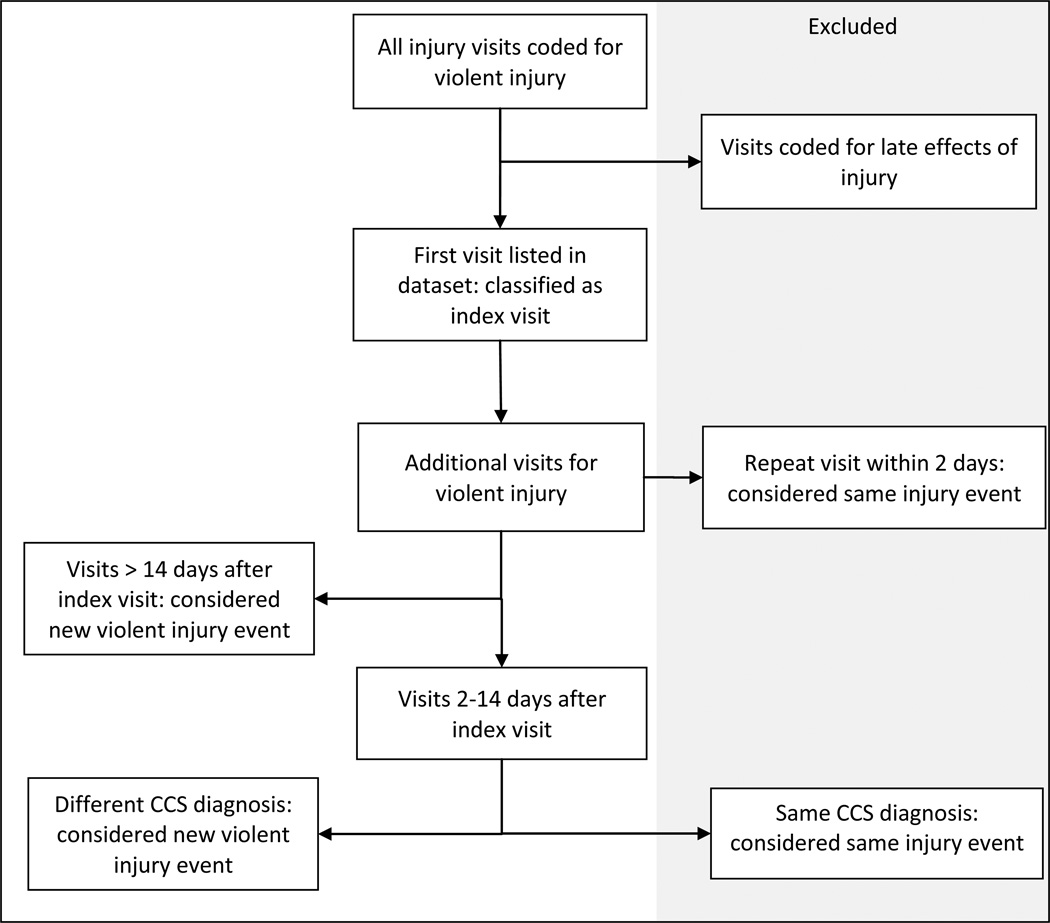
Index visits were limited to those occurring in 2010 in order to allow a minimum of 2 years of follow-up after the index injury. To ensure at least two years of follow-up, we excluded patients who died from their index injury, and patients who had no documented recurrence but whose death was recorded in the dataset within two years. Patients who died of a recurrent injury were included as recurrers. The SID and SEDD cannot be linked to any other dataset, including death certificate data, so out-of-hospital deaths could not be included, nor could injuries not leading to ED or hospital treatment. To identify recurrent injuries stemming from separate episodes of violence, rather than revisits for continuing care, we excluded visits coded as late effects or complications of injury. Because a visit occurring soon after an injury might not be coded as a late effect, even if the patient had already sought care, we further classified visits as new violent injury events according to both time between visits and injury diagnoses (see Figure 1).
Figure 1.
Injury Event Determination
2.3 Measurements
The primary outcome was recurrence. Patients were classified as recurrers if they had at least one visit for a new violent injury subsequent to their index violent injury visit. Demographic explanatory variables included age, sex, race/ethnicity, homelessness, urban vs. rural location, median income of home zip code, and insurance type. Injury-related covariates included diagnosis and mechanism. Injury severity score (ISS) was calculated from ICD-9 diagnosis codes using validated methodology.39,40 Patients were classified as to whether their index injury resulted in hospital admission, and whether they had a visit for an alcohol-related disorder, substance use, mental illness, or unintentional injury at any point in the study period.
2.4 Statistical Analysis
Bivariate analyses were performed on demographics, injury characteristics, and occurrence of visits for comorbid disease. Categorical variables were assessed using χ2 tests, and continuous variables were assessed using t-tests. Differences in demographic and clinical characteristics between recurrers and non-recurrers were estimated using multivariable logistic regression. Multiple imputation was performed on missing data using the remaining covariates.41 To identify the relevance of a population-based as opposed to registr-based studies, we identified severe recurrent injuries as those that would have beene included in the state trauma registry: injuries resulting in death or hospital admission, excluding isolated skeletal injuries.42 We performed a secondary analysis to identify risk factors for severe recurrence. To assess the relevance of a state-wide vs. single-center study, we tracked whether recurrers sought care for a second injury at the same or at a different hospital and whether they were treated at a designated trauma center. We calculated the proportion of recurrence for injured patients residing in each Florida zip code and mapped these results using using ArcGIS (Esri Inc., Redlands, CA; 2015). All other analyses used Stata (Version 14, StataCorp. College Station, TX; 2015).
2.5 Survival analysis
The Kaplan-Meier method was used to estimate time to recurrence, including all patients presenting for violent injury between 2010 and 2012 and accounting for differences in follow-up time. For patients who did not recur or die, time under observation was given as maximum time under observation. Time to recurrence for severe vs. mild recurrences was compared using the log-rank test.
2.6 Cost analysis
We assessed the total hospital charges and costs for violent injury for the cohort of patients with an index injury in 2010. The SID and SEDD report total hospital charges for each visit. These charges were summed for all violent injury visits in 2010–2012 for this population, and separated by ED treat-and-release visits, including observation stays, and inpatient admissions. Charges associated with the index injury were grouped, as were charges associated with any subsequent violent injuries, including charges for multiple visits related to a single injury. To estimate costs, we multiplied charges by the hospital-specific cost-to-charge ratios provided by HCUP, which are based on all-payer, inpatient costs. Combining validated techniques,43 where no hospital-specific ratio was available, the HCUP group average ratio based on hospital category was substituted. When neither was available, the state average was used.
3. Results
There were 54,178 individuals who presented for violent injuries in the first year of the study period. One hundred fifteen died of their initial injuries, and 155 died at another hospital visit within two years, without being re-injured, leaving 53,908 patients for analysis. Among survivors, 11.1% (5,967/53,908) recurred, with 5.6% (336) classified as severe. Just 2.2% (1,192/53,908) had multiple recurrences. Overall, 31.3% of non-recurrers and 33.3% of recurrers went to a trauma center. Of severe injuries, 55.9% of index injuries and 52.0% of recurrent injuries were treated in trauma centers.
3.1 Characteristics of study subjects
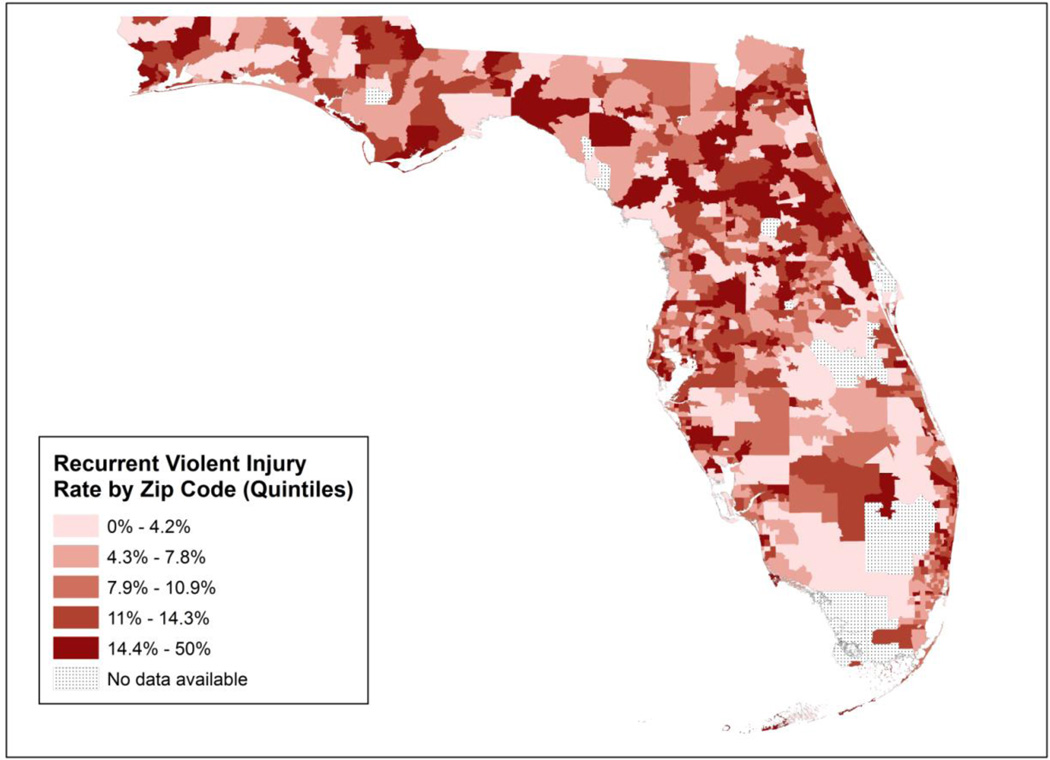
Demographic and clinical characteristics from the index visit for recurrers and non-recurrers are shown in Table 1. Demographics of recurrers were as follows: mean age was 33 years, 61.8% (n= 3,687) were male, 57.5% (n=3,410) were white; 76.7% (n=4,307) lived in a zip code with median income below the national median; and 88.4% (n=5,071) lived in an urban area. The vast majority of injuries were mild: ISS was < 9 in 94.3% of non-recurrers and 95.2% of recurrers, and 0.3% (115/53,908) of index injuries and 0.2% (11/5,967) of second injuries resulted in death. More than 90% of injuries were blunt for both recurrers and non-recurrers, and the most common mechanism was struck (with or without a weapon). Only 2.5% of non-recurrers and 1.5% of recurrers had gunshot wounds. ED utilization was high: the mean total number of ED and hospital visits per patient was 8 for recurrers (IQR 5–16) and 3 for non-recurrers (IQR 1–6) over the 3-year time period, although recurrent violent injury accounted for an average of only 1 of these additional visits. Figure 2 shows recurrence rates for violently injured individuals by zip code of residence.
Table 1.
Patient Characteristics at First Visit for Violent Injury, 2010
| Non-Recurrers N=47,941 |
Recurrers N=5,967 |
P value | |
|---|---|---|---|
| Race | N (%) | N (%) | <0.001 |
| White | 24,911 (52.3) | 3,410 (57.5) | |
| Black | 15,375 (32.3) | 1,912 (32.2) | |
| Hispanic | 6,333 (13.3) | 524 (8.8) | |
| Asian/Pacific Islander | 260 (0.6) | 16 (0.3) | |
| Native American | 63 (0.1) | 13 (0.2) | |
| Other | 685 (1.4) | 61 (1.0) | |
| Female | 17,564 (36.6) | 2,280 (38.2) | 0.017 |
| Age | <0.001 | ||
| <18 | 5,824 (12.2) | 529 (8.9) | |
| 18–34 | 24,862 (51.9) | 3,070 (51.5) | |
| 35–54 | 14,146 (29.5) | 2,070 (34.7) | |
| ≥55 | 3,109 (6.5) | 298 (5.0) | |
| Insurance type | <0.001 | ||
| Private | 7,638 (15.9) | 426 (7.1) | |
| Medicare | 2,634 (5.5) | 375 (6.3) | |
| Medicaid | 11,381 (23.7) | 1,700 (28.5) | |
| Uninsured/other | 26,288 (54.8) | 3,466 (58.1) | |
| Zip code median income below the national median | 33,387 (72.0) | 4,307 (76.7) | <0.001 |
| Homeless | 516 (1.1) | 198 (3.3) | <0.001 |
| Urban location | 41,131 (87.1) | 5,071 (88.4) | 0.005 |
| Injury type | <0.001 | ||
| Head injury | 6,557 (13.7) | 805 (13.5) | |
| Spinal cord injury | 21 (0.04) | 2 (0.03) | |
| Internal injury | 751 (1.6) | 65 (1.1) | |
| Musculoskeletal injury | 6,898 (14.4) | 934 (15.7) | |
| Open wound | 12,618 (26.3) | 1,431 (24.0) | |
| Superficial injury | 14,988 (31.3) | 1,994 (33.4) | |
| Other | 6,108 (12.7) | 736 (12.3 | |
| Mechanism | <0.001 | ||
| Gunshot wound | 1,180 (2.5) | 92 (1.5) | |
| Stab wound | 3,007 (6.3) | 365 (6.1) | |
| Struck by or against | 24,824 (51.8) | 3,075 (51.5) | |
| Other or multiple | 18,924 (39.5) | 2,435 (40.8) | |
| Admitted to the hospital at index injury | 3,428 (7.2) | 363 (6.1) | 0.002 |
| Index presentation to trauma center | 15,110 (31.5) | 1,994 (33.4) | 0.003 |
| Injury Severity Score | 0.022 | ||
| <9 | 45,218 (94.3) | 5,680 (95.2) | |
| 9–15 | 2,109 (4.4) | 224 (3.8) | |
| >15 | 614 (1.3) | 63 (1.1) | |
| Other visits | |||
| Mental health | 5,240 (10.9) | 1,588 (26.6) | <0.001 |
| Substance use | 1,864 (3.9) | 641 (10.7) | <0.001 |
| Alcohol abuse | 2,064 (4.3) | 977 (16.4) | <0.001 |
| Unintentional injury | 15,619 (32.6) | 3,416 (57.3) | <0.001 |
T test. All others χ2 test.
Figure 2.
Geographic Distribution of Recurrent Violent Injury, Florida, 2010–2012
3.2 Risk factors for recurrence
Multivariable logistic regression results identifying risk factors for recurrence and severe recurrence are presented in Table 2. Patients living in low-income areas had 20% increased odds of recurrence, but equal odds of severe recurrence. Medicare patients had 1.7 times increased odds compared to privately insured patients. Patients with Medicaid or no insurance had approximately double the odds of recurrence, and increased odds of severe recurrence. Compared to white patients, Black patients had 10% higher odds of any recurrence, but 40% higher odds of severe recurrence. Hispanic patients had 30% lower odds of recurrence. Men and women had equal odds of any recurrence, but women had 70% lower odds of severe recurrence. Rural residence was associated with 10% lower odds of recurrence, though nearly 90% of patients lived in urban areas. Compared to patients aged 18–35, those under 18 and over 55 had lower odds of any recurrence, while those age 35–54 had 60% higher odds of severe recurrence.
Table 2.
Multivariable Logistic Regression Results: Risk Factors for Recurrent Violent Injury and Severe Recurrent Violent Injury
| Any Recurrence | Severe Recurrence | |||
|---|---|---|---|---|
| Odds Ratio (95% confidence interval) |
p-Value | Odds Ratio (95% confidence interval) |
p-Value | |
| Race | ||||
| White | 1 | Reference | ||
| Black | 1.1 (1.0–1.2) | 0.009 | 1.4 (1.1–1.8) | 0.018 |
| Hispanic | 0.7 (0.6–0.8) | <0.001 | ||
| Asian/Pacific Islander | 0.7 (0.4–1.1) | 0.104 | ||
| Native American | 1.7 (0.9–3.2) | 0.109 | ||
| Other | 0.9 (0.7–1.1) | 0.287 | ||
| Female | 1 (0.9–1.0) | 0.509 | 0.3 (0.2–0.5) | <0.001 |
| Age | ||||
| <18 | 0.7 (0.7–0.8) | <0.001 | 0.6 (0.3–1.1) | 0.073 |
| 18–34 | 1 | Reference | 1 | Reference |
| 35–54 | 1 (0.9–1.0) | 0.345 | 1.6 (1.2–2.1) | 0.001 |
| ≥55 | 0.7 (0.6–0.8) | <0.001 | 1.5 (0.9–2.4) | 0.087 |
| Insurance type | ||||
| Private | 1 | Reference | ||
| Medicare | 1.6 (1.4–1.9) | <0.001 | ||
| Medicaid | 2.1 (1.9–2.4) | <0.001 | 1.5 (1.0–2.4) | 0.061 |
| Uninsured/other | 1.9 (1.7–2.1) | <0.001 | 1.8 (1.2–2.6) | 0.003 |
| Zip code median income below | ||||
| national median | 1.2 (1.1–1.3) | <0.001 | 1.3 (1.0–1.9) | 0.085 |
| Homeless | 1.8 (1.4–2.1) | <0.001 | ||
| Rural residence | 0.9 (0.8–0.9) | 0.001 | ||
| Injury severity score | ||||
| <9 | 1 | Reference | ||
| 9–15 | 1.0 (0.8–1.1) | 0.618 | ||
| >15 | 0.9 (0.6–1.2) | 0.321 | ||
| Admitted to the hospital at index injury |
0.9 (0.8–1.0) | 0.066 | 1.5 (1.0–2.2) | 0.023 |
| Index presentation to trauma center | 1 (1.0–1.1) | 0.226 | 1.3 (1.0–1.6) | 0.072 |
| Mechanism of Injury | ||||
| Gunshot wound | 0.8 (0.6–1.0) | 0.020 | ||
| Stab wound | 1.0 (0.9–1.2) | 0.621 | ||
| Struck by or against | 1 | Reference | ||
| Other or multiple | 1.0 (1.0–1.1) | 0.688 | ||
| Other visits | ||||
| Mental health | 1.8 (1.7–2.0) | <0.001 | 1.8 (1.3–2.4) | <0.001 |
| Substance use | 1.6 (1.4–1.7) | <0.001 | ||
| Alcohol abuse | 2.6 (2.4–2.9) | <0.001 | 2.7 (1.9–3.7) | <0.001 |
| Unintentional injury | 2.2 (2.0–2.3) | <0.001 | 1.7 (1.3–2.1) | <0.001 |
Homeless patients had 60% increased odds of any recurrence, but no significant increase in severe recurrences. Concomitant visits for mental illness, alcohol abuse, and unintentional injury were associated with increased odds of any recurrence and severe recurrence. Visits for substance use were associated with recurrence, but not severe recurrence. Patients admitted to the hospital for their index injury had equal odds of any recurrence, but 50% higher odds of severe recurrence. Injury severity score was not an independent predictor of recurrence, nor was initial trauma center treatment. However, patients with gunshot wounds had 20% reduced odds of recurrence compared to other mechanisms of injury. Of patients who recurred within the study period, median time-to-recurrence was 307 days, with no significant difference between severe and non-severe recurrers (p value for the log rank test = 0.1204).
3.3 Charges and costs
Hospital charges and costs are summarized in Table 3. Overall, violent injury accounted for $596 million in charges and $131 million in costs for patients with an index injury in 2010. Index visits accounted for $105 million and recurrent visits for $25.3 million in costs. Overall, 58.9% of recurrers presented to a different hospital for their second injury. Women, Black patients, rural residents, and those age ≥35 were more likely to return to the same hospital. Odds of returning to the same hospital decreased with time between injuries, and in patients with mental health visits.
Table 3.
2010–2012 Hospital Charges and Costs for All Violent Injury Visits of Patients with an Index Visit in 2010
| N | Median charges | Total charges | Median cost | Total costs | |
|---|---|---|---|---|---|
| Visits for Index | |||||
| Injuries | |||||
| ED discharges* | 52,748 | $2,655 | $227 million | $577 | $48.1 million |
| Admissions | 4,662 | $32,914 | $252 million | $7,239 | $ 57.3 million |
| Total | 58,661 | $3,040 | $479 million | $674 | $105 million |
| Visits for | |||||
| Recurrent | |||||
| Injuries | |||||
| ED discharges* | 9,836 | $3,164 | $49.7 million | $690 | $10.5 million |
| Admissions | 1,244 | $31,816 | $66.9 million | $6,875 | $14.9 million |
| Total | 11,110 | $3,835 | $117 million | $860 | $25.3 million |
| Grand total | 68,490 | $3,161 | $596 million | $699 | $131 million |
Observation stays included with ED discharges
3.4 Missing data
We excluded 24,869 visits (12.5%) for intentional injury from 2010–2012 that lacked the visitlink identifier. These patients were more likely to be Hispanic, male, or homeless, and to live in low income or urban areas. These visits more often resulted in death (1.8 vs. 0.2%) or hospital admission. Injury diagnoses were similar, but excluded visits were more often due to penetrating mechanism (16.9 vs. 7.4%). Regarding other missing data, race, age, income, or rurality was missing for 4% of patients. The regression results reported here reflect imputed values, but results and standard errors were similar when performed without imputation.
4. Discussion
In the first state-wide analysis of all ED and hospital stays for violent injury, we found that 11.1% of violently injured patients presented to the ED with another violent injury within 2–3 years, and 5.6% of these recurrences were severe. These patients’ recurrent violent injuries accounted for 9,836 ED visits, 1,244 hospitalizations, and $25.3 million in direct costs, a substantial burden on injured individuals and the healthcare system. The majority of visits were to non-trauma centers, consistent with past studies.44 As most hospital-based violence intervention programs are at trauma centers, this suggests new opportunities for prevention.45 We identified key predictors of recurrence, including urban location; low income home zip code; public insurance or no insurance; homelessness; and visits for behavioral health or unintentional injury.
By using a state-wide, all-payer database, we followed patients regardless of where they sought care. This provides a major advantage over single-institution studies, as we saw that 58.9% of patients presented to a new hospital for their second injury, and 68.5% initially presented to non-trauma centers, in keeping with a Los Angeles survey which found that 42% of recurrently injured patients had previously sought care elsewhere.20 Moreover, as shown in Figure 2, rates of recurrence varied across the state, with multiple areas of high and low rates. Our findings can serve as a baseline for interventions aimed at reducing recurrence. Our results also point to the opportunity for a comprehensive approach to preventing recurrent violent injury: by intervening in community hospitals as well as trauma centers; by studying how to identify high-risk patients at their non-injury visits; and by harnessing the potential of housing stability and behavioral health treatment to promote safety. Patients who present for an initial violent injury with the risk factors we identify could be directed to detailed assessment or intervention by emergency department protocol or by a flag in the electronic medical record. Hospital-based violence intervention programs that provider wrap-around social and psychological support to injured patients have shown promise.8,46–48 However, these programs have primarily targeted youth violence, and expanded strategies may be needed to reach the older segment of the violently injured population.
Our analysis supports past findings and expands upon them. Nearly all authors have found increased risk of recurrent injury among those living in poverty,13,15,16,18,49,50 and those with limited insurance.13,16,18,50 While many prior studies have identified increased risk in Black compared to white patients,13,16,18,23,25,50 we found that Black patients had minimally higher overall recurrence (OR 1.1), but a substantial increase in severe recurrence (OR 1.4). Furthermore, while only 15.2% of the state population was Black in 2010,51 nearly 1/3 of both recurrers and non-recurrers were Black, consistent with national trends.52 In 2010, 22.5% of the population of Florida was Hispanic,51 indicating relatively low rates of violent injury in this population, as Hispanics made up only 13.3% of nonrecurrers and 8.8% of recurrers. Moreover, we found that Hispanic patients had lower risk of recurrence than non-Hispanic Black and white patients. This trend was seen but was nonsignificant in one prior single-center study.16 Contrary to some studies,26,50 young age was not a risk factor for recurrence here, and older age appeared to increase odds of severe recurrence. However, compared to the state population median age of 40.7 years, violently injured individuals were younger overall.
Women were the minority of violently injured patients, and were underrepresented compared to a state female population of 51.1%,53 but in contrast to most literature,14,16,21,23,25,26,54 we found similar recurrence rates for women and men. This may represent the large proportion of minor injuries included here, as men did have a higher rate of severe recurrence. These findings support Madden et al.’s suggestion that demographics alone do not identify those patients at greatest risk for recurrence.10 Patients with gunshot wounds had lower odds of recurrence. This may reflect greater severity of injury not fully captured elsewhere in our model that led to longer time to recovery, postponing risk of reinjury. Conversely, studies have shown elevated mortality risk after recovery from firearm injury, which may have lowered our measured recurrence rate.4,5
Several studies have found increased risk for recurrent trauma associated with alcohol and substance abuse,3,49,50,55 along with an opportunity for intervention.9,18 Our findings support efforts to incorporate alcohol and substance abuse screening and treatment into trauma care, as recommended by the American College of Surgeons Committee on Trauma.9,56 Few studies have investigated mental health comorbidity, but our results are consistent with evidence that mental illness increases risk of recurrence,13,49 and that trauma increases risk of mental health challenges,57 and with the efforts of violence intervention initiatives to incorporate behavioral health care.8,58–60 Homelessness was rare in all groups, but the homeless are nonetheless substantially overrepresented at 1.1% of nonrecurrers and 3.3% of recurrers, compared to < 0.01% of the state population.61 More than half of recurrers had visits for unintentional injury. The only study that, to our knowledge, investigated this relationship found increased risk of violence in unintentionally injured patients.23 These injury visits may represent additional opportunities for ED and trauma clinicians to intervene in these patients’ trajectory.
4.1 Limitations
We acknowledge several limitations to this study. In this retrospective analysis of administrative data, information is necessarily limited, and causal inference cannot be drawn. Injuries may have been miscoded as intentional or unintentional, and patients’ identities may have been mis-registered. We could not account for injuries treated out-of-state. Because the SID and SEDD cannot be linked to any other data source, including death certificate data, out-of-hospital deaths, including those caused by recurrent injury, could not be captured. Because these databases do not include outpatient providers, we cannot account either for injuries not treated in an ED or hospital, or for injured patients’ use of outpatient care for other health needs. Important opportunities to intervene with patients to prevent recurrent injuries may exist in the outpatient setting, and deserve further investigation. Although these deaths are significant in that they represent the most severe potential outcome of recurrent violent injury, we expect that the impact of excluding them to be small. Approximately 20% of deaths in Florida occur in the hospital, implying an additional 1080 deaths in this population.62 Accounting for these deaths as all recurrers would raise the rate of recurrence to 13.1%. Accounting for all these deaths as non-recurrers censored for inadequate follow-up would increase the recurrence rate to 11.3%. Likewise, the CDC reported 794 assault-related, out-of-hospital deaths occurring in Florida from 2010 through 2012.63 If all of these deaths occurred in recurrers not otherwise captured in our analysis, this would raise the recurrence rate to 12.5%. It is not possible to determine the impact of out-of-hospital deaths on our assessment of risk factors for recurrence.
It was challenging to determine whether each visit was related to a separate injury event, and visits may have been misclassified as new as opposed to related to the same injury event. Using a restricted time period necessarily underestimated recurrence, both because later recurrences could not be captured, and because the index injury we identify may not have been a patient’s true, lifetime, first injury. Studies have consistently found recurrences beginning within one month after initial injury, and a Cunningham et al. identified the first 6 months after injury as the highest risk time period in youth, in part due to high risk for retaliatory violence in the immediate post-injury period.27,64 One study found that 82% of recurrences occurred within two years,26 but recurrences have been reported for up to 30 years.20 We expect that our three-year time frame captured the majority of recurrences, while remaining short enough that a violence prevention program could feasibly follow patients for a similar time period. Early presentation may itself indicate high risk, leading to more recurrences, but we did not discern any substantive differences between patients whose index injury occurred early as opposed to late in the study period. We defined severe injuries in keeping with Florida trauma registry criteria, but these criteria are subjective, and many others could have been used. We excluded visits lacking revisit variables, which may have biased our results. Lastly, our cost data were estimated using cost-to-charge ratios derived for inpatient stays,65 and the results for ED visits may be less reliable.
5. Conclusions
Recurrent violent injury is a common and costly phenomenon, with an incidence of 11.1% within 2–3 years in this state-wide analysis. Two-thirds of violently injured patients, including half of those with severe injuries, present to non-trauma centers. Effective violence prevention programs that collaborate with all hospitals are needed to prevent recurrent injury. The homeless and those with behavioral health needs are at high risk for recurrent injury and stand to benefit from focused prevention efforts.
Supplementary Material
Acknowledgments
No specific funding support was obtained for this research, but the first author was supported by a training grant from the National Heart, Lung and Blood Institute, T32 HL-98054-6.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presentation: Poster presentation, the 2016 Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma, January 12–16, 2016, San Antonio, TX.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Author Contributions: EJK had full access to the data and takes responsibility for the integrity and accuracy of the analysis. EJK and KLR are responsible for data acquisition. EJK and MKD are responsible for the concept and data analysis. EJK drafted the manuscript. All authors contributed to critical review of the manuscript.
Contributor Information
Elinore Kaufman, Department of Surgery, New York-Presbyterian Hospital Weill Cornell Medical Center, New York, NY, USA.
Kristin Rising, Department of Emergency Medicine, Thomas Jefferson University, Philadelphia, PA, USA.
Douglas J. Wiebe, Associate Professor of Epidemiology, Department of Biostatistics and Epidemiology, University of Pennsylvania, Philadelphia, PA, USA.
David J. Ebler, Division of Acute Care Surgery, University of Florida College of Medicine Jacksonville, Jacksonville, FL, USA.
Marie L. Crandall, Director of Research, Department of Surgery, University of Florida College of Medicine Jacksonville, Jacksonville, FL, USA.
M. Kit Delgado, Department of Emergency Medicine and Biostatistics and Epidemiology, University of Pennsylvania, Philadelphia, PA, USA.
References
- 1.US Centers for Disease Control and Prevention. [accessed 12.10.14];Web-based Injury Statistics Query and Reporting System. http://www.cdc.gov/injury/wisqars/index.html.
- 2.Dahlberg LL, Mercy JA. The History of Violence as a public health issue. AMA Vitual Mentor. 2009;11(2):167–172. doi: 10.1001/virtualmentor.2009.11.2.mhst1-0902. [DOI] [PubMed] [Google Scholar]
- 3.Sims DW, Bivians BA. Urban trauma: a chronic recurrent disease. J Trauma Injury Infect Crit Care. 1988;28(7):940–946. [PubMed] [Google Scholar]
- 4.Fahimi J, Larimer E, Hamud-Ahmed W, Anderson E, Schnorr D, Yen I, Alter HJ. Long-term mortality of patients surviving firearm violence. Inj Prev. 2015 doi: 10.1136/injuryprev-2015-041710. [DOI] [PubMed] [Google Scholar]
- 5.Rowhani-Rahbar A, Zatzick D, Wang J, Mills BM, Simonetti JA, Fan MD, et al. Firearm-Related Hospitalization and Risk for Subsequent Violent Injury, Death, or Crime Perpetration. Ann Int Med. 2015;162(7):492–500. doi: 10.7326/M14-2362. [DOI] [PubMed] [Google Scholar]
- 6.Caputo ND, Shields CP, Ochoa C, Matarlo J, Leber M, Madlinger R, et al. Violent and fatal youth trauma: is there a missed opportunity? West J Emerg Med. 2012;13(2):146–150. doi: 10.5811/westjem.2011.6.6765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chong VE, Smith R, Garcia A, Lee WS, Ashley L, Marks A, et al. Hospital-centered violence intervention programs: a cost-effectiveness analysis. Am J Surg. 2014;209(4):597–603. doi: 10.1016/j.amjsurg.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Purtle J, Dicker R, Cooper C, Corbin T, Greene MB, Marks A, et al. Hospital-based violence intervention programs save lives and money. J Trauma Acute Care Surg. 2013;75(2):331–333. doi: 10.1097/TA.0b013e318294f518. [DOI] [PubMed] [Google Scholar]
- 9.Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surgery. 1999;230(4):473–483. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madden C, Garrett JM, Cole TB, Runge JW, Porter CQ. The urban epidemiology of recurrent injury: beyond age, race, and gender stereotypes. Acad Emerg Med. 1997;4(8):772–775. doi: 10.1111/j.1553-2712.1997.tb03782.x. [DOI] [PubMed] [Google Scholar]
- 11.Dixon SD, Como JJ, Banerjee A, Claridge JA. Trauma recidivists: surprisingly better outcomes than initially injured trauma patients. Am J Surg. 2013;207:423–431. doi: 10.1016/j.amjsurg.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrissey TB, Byrds CR, Deitch EA. The incidence of recurrent penetrating trauma in an urban trauma center. J Trauma Injury Infect Crit Care. 1991;31(11):1536–1538. doi: 10.1097/00005373-199111000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Buss TF, Abdu R. Repeat victims of violence in an urban trauma center. Violence Vict. 1995;10(3):183–194. [PubMed] [Google Scholar]
- 14.McCoy AM, Como JJ, Greene G, Laskey SL, Claridge JA. A novel prospective approach to evaluate trauma recidivism: the concept of the past trauma history. J Trauma Acute Care Surg. 2013;75(1):116–121. doi: 10.1097/TA.0b013e31829231b7. [DOI] [PubMed] [Google Scholar]
- 15.Goins WA, Thompson J, Simpkins C. Recurrent intentional injury. J Natl Med Assoc. 1992;84(5):431–435. [PMC free article] [PubMed] [Google Scholar]
- 16.Chong VE, Lee WS, Victorino GP. Neighborhood socioeconomic status is associated with violent reinjury. J Surg Res. 2015;199(1):177–182. doi: 10.1016/j.jss.2015.03.086. [DOI] [PubMed] [Google Scholar]
- 17.Hankin A, Wei S, Foreman J, Houry D. Screening for violence risk factors identifies young adults at risk for return emergency department visit for injury. West J Emerg Med. 2014;15(5):609–614. doi: 10.5811/westjem.2014.4.21275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rivara FP, Koepsell TD, Jurkovich GJ, Gurney JG, Soderberg R. The effects of alcohol abuse on readmission for trauma. JAMA. 1993;270(16):1962–1964. [PubMed] [Google Scholar]
- 19.Juillard C, Smith R, Anaya N, Garcia A, Kahn JG, Dicker R. Saving lives and saving money: Hospital-based violence intervention is cost-effective. J Trauma Acute Care Surg. 2015;78(2):252–258. doi: 10.1097/TA.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy F, Brown JR, Brown KA. Geographic and temporal patterns of recurrent intentional injury in south-central Los Angeles. J Natl Med Assoc. 1996;88(9):970–972. [PMC free article] [PubMed] [Google Scholar]
- 21.Schwarz DF, Grisso JA, Miles CG, Holmes JH, Wishner AR, Sutton RL. A longitudinal study of injury morbidity in an African-American population. JAMA. 1994;271(10):755–760. [PubMed] [Google Scholar]
- 22.Griffin RL, Davis GC, Levitan EB, MacLennan PA, Redden DT, McGwin G. The effect of previous traumatic injury on homicide risk. J Forensic Sci. 2014;59(4):986–990. doi: 10.1111/1556-4029.12416. [DOI] [PubMed] [Google Scholar]
- 23.Litacker D. Preventing recurring injuries from violence: the risk of assault among Cleveland youth after hospitalization. Am J Pub Health. 1996;86(11):1633–1636. doi: 10.2105/ajph.86.11.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brooke BS, Efron DT, Chang DC, Haut ER, Cornwell EE. Patterns and outcomes among penetrating trauma recidivists: it only gets worse. J Trauma. 2006;61(1) doi: 10.1097/01.ta.0000224143.15498.bb. [DOI] [PubMed] [Google Scholar]
- 25.Hedges BE, Dimsdale JE, Hoyt DB. Characteristics of repeat trauma patients, San Diego County. Am J Pub Health. 1995;85(7):1008–1010. doi: 10.2105/ajph.85.7.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufmann CR, Branas CC, Brawley ML. A population-based study of trauma recidivism. J Trauma. 1998;45(2):325–332. doi: 10.1097/00005373-199808000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham RM, Carter PM, Ranney M, Newton M, Woodman W, Zimmerman M, Walton MA. Violent Reinjury and Mortality Among Youth Seeking Emergency Department Care for Assault-Related Injury. JAMA Pediatr. 2015;169:e96–e104. doi: 10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nathens AB, Jurkovich GJ, MacKenzie EJ, Rivara FP. A resource-based assessment of trauma care in the United States. J Trauma. 2004;56:173–178. doi: 10.1097/01.TA.0000056159.65396.7C. [DOI] [PubMed] [Google Scholar]
- 29.Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues when Studying Readmissions and Revisits Using Hospital Adminstrative Data. HCUP Methods Series Report #. 2011:2011–2001. [Google Scholar]
- 30.Agency for Healthcare Research and Quality. [accessed 5.1.15];Healthcare Cost and Utilization Project (HCUP) http://www.hcup-us.ahrq.gov. [PubMed]
- 31.Agency for Healthcare Research and Quality. [accessed 15.8.15];Data Element Availability Map: HCUP Revisit Variables. https://www.hcup-us.ahrq.gov/maps/revisit.jsp.
- 32.Rising KL, Victor TW, Hollander JE, Carr BG. Patient returns to the emergency department: the time-to-return curve. Acad Emerg Med. 2014;21(8):864–871. doi: 10.1111/acem.12442. [DOI] [PubMed] [Google Scholar]
- 33.Agency for Healthcare Research and Quality. [accessed 14.5.15];Clinical Classifications Software (CCS) for ICD-9-CM. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp#pubs.
- 34.US Centers for Disease Control and Prevention. Recommended Framework for Presenting Injury Mortality Data. MMWR. 1997;46(RR-14):1–33. [PubMed] [Google Scholar]
- 35.US Centers for Disease Control and Prevention. Strategies to improve external cause-of-injury coding in state-based hospital discharge and emergency department data systems. [accessed 25.2.16];MMWR Recom Rep. 2008 57(RR01):1–15. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5701a1.htm. [PubMed] [Google Scholar]
- 36.The Trust for America’s Health. The Facts Hurt: a State-By-State Injury Prevention Policy Report. Washington, DC: 2013. [Google Scholar]
- 37.Barrett M, Steiner C. Addendum to Healthcare Cost and Utilization Project (HCUP) E Code Evaluation Report (Updated for 2009) [accessed 25.2.16];HCUP Methods Series Report # 2004-06. ONLINE November 1, 2011. U.S. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- 38.LeMier M, Cummings P, West TA. Accuracy of external cause of injury codes reported in Washington State hospital discharge records. Inj Prevn. 2001;7:334–338. doi: 10.1136/ip.7.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clark DE, Osler T, Hahn DR. [accessed 20.7.15];ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. https://ideas.repec.org/c/boc/bocode/s457028.html.
- 40.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj Prev. 2015;21(5):325–330. doi: 10.1136/injuryprev-2014-041524. [DOI] [PubMed] [Google Scholar]
- 41.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 42.National Trauma Data Bank. [accessed 18.11.15];Florida State Information. http://www.ntdsdictionary.org/ntdbParticipants/stateInformation/florida.html;
- 43.Yu T-C, Zhou H. Evaluation of techniques for handling missing cost-to-charge ratios in the USA Nationwide Inpatient Sample: a simulation study. J Comp Effect Res. 2015;4:473–483. doi: 10.2217/cer.15.28. [DOI] [PubMed] [Google Scholar]
- 44.MacKenzie EJ, Steinwachs DM, Ramzy AI. Evaluating performance of statewide regionalized systems of trauma care. J Trauma. 1990;30(6):681–688. doi: 10.1097/00005373-199006000-00005. [DOI] [PubMed] [Google Scholar]
- 45. [accessed 16.9.15];National Network of Hospital-Based Violence Intervention Programs. http://nnhvip.org/network-membership/
- 46.Karraker N, Cunningham R, Becker M, Fein JA, Knox LM. Violence Is Preventable: A Best Practices Guide for Launching & Sustaining a Hospital-Based Program to Break the Cycle of Violence. Chicago, IL: Youth ALIVE!; 2011. [Google Scholar]
- 47.Cunningham R, Knox L, Fein JA, Harrison S, Frisch K, Walton M, et al. Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009;53:490–500. doi: 10.1016/j.annemergmed.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 48.Shibru D, Zahnd E, Becker M, Bekaert N, Calhoun D, Victorino GP. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689. doi: 10.1016/j.jamcollsurg.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 49.Smeltzer SC, Redeker NS. A framework of trauma and trauma recidivism in adolescents and young adults. J Trauma Nurs. 1995;2:93–99. doi: 10.1097/00043860-199510000-00016. [DOI] [PubMed] [Google Scholar]
- 50.Cooper C, Eslinger D, Nash D, al-Zawahri J, Stolley P. Repeat victims of violence: report of a large concurrent case-control study. Arch Surg. 2000;135(7):837–843. doi: 10.1001/archsurg.135.7.837. [DOI] [PubMed] [Google Scholar]
- 51.United States Census Bureau. [accessed 9.2.15]; http://www.census.gov.
- 52.Kalesan B, Vasan S, Mobily ME, Keiser O, Fagan JA, Galea S. State-specific, racial and ethnic heterogeneity in trends of firearm-related fatality rates in the USA from 2000 to 2010. BMJ Open. 2014;4:1–9. doi: 10.1136/bmjopen-2014-005628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.U.S. Census Bureau. 2010 Census of Population and Housing, Population and Housing Unit Counts, CPH-2–11, Florida U.S. Washington, DC: Government Printing Office; 2012. [Google Scholar]
- 54.Greenberg M, Schneider D. Violence in American cities: Young black males in the answer, but what was the question? Soc Sci Med. 1994;39(2):179–187. doi: 10.1016/0277-9536(94)90326-3. [DOI] [PubMed] [Google Scholar]
- 55.Claassen CA, Larkin GL, Hodges G, Field C. Criminal correlates of injury-related emergency department recidivism. J Emerg Med. 2007;32(2):141–147. doi: 10.1016/j.jemermed.2006.05.041. [DOI] [PubMed] [Google Scholar]
- 56.American College of Surgeons Committee on Trauma. Resources for Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2014. [Google Scholar]
- 57.Richmond TS, Kauder D, Strumpf N, Meredith T. Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatric Ssoc. 2002;50:215–222. doi: 10.1046/j.1532-5415.2002.50051.x. [DOI] [PubMed] [Google Scholar]
- 58.Cheng TL, Haynie D, Brenner RA, Wright JL. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: results of a randomized trial. Pediatrics. 2008;122:938–946. doi: 10.1542/peds.2007-2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carr BG, Wiebe DJ, Richmond TS, Cheney R, Branas CC. A randomised controlled feasibility trial of alcohol consumption and the ability to appropriately use a firearm. Inj Prev. 2009;15(6):409–412. doi: 10.1136/ip.2008.020768. [DOI] [PubMed] [Google Scholar]
- 60.Rich JA, Grey CM. Pathways to recurrent trauma among young Black men: traumatic stress, substance use, and the “code of the street”. Am J Pub Health. 2005;95(5):816–824. doi: 10.2105/AJPH.2004.044560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.U.S. Census Bureau. 2010 Census Special Reports, the Emergency and Transitional Shelter Population: 2010, C2010SR-02, U.S. Washington, DC: Government Printing Office; 2012. [Google Scholar]
- 62.Dartmouth Atlas of Healthcare: Percent of Deaths Occurring in Hospital. [accessed 25.8.15]; http://www.dartmouthatlas.org/data/table.aspx?ind=15.
- 63.U.S. Centers for Disease Control and Prevention. Compressed Mortality File 1999–2013 on CDC WONDER Online Database. [accessed 2.4.15];Compressed Mortality File 1999–2013 20;2S. 2014 http://wonder.cdc.gov/cmf-icd10.html.
- 64.Wiebe DJ, Blackstone MM, Mollen CJ, Culyba AJ, Fein JA. Self-reported Violence-related Outcomes for Adolescents Within Eight Weeks of Emergency Department Treatment for Assault Injury. J Adol Health. 2011;49:440–442. doi: 10.1016/j.jadohealth.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Agency for Healthcare Research and Quality. Cost-to-Charge Ratio Files. [accessed 25.2.15];Healthcare Cost and Utilization Project (HCUP) 2014 www.hcup-us.ahrq.gov/db/state/costtocharge.jsp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.