Abstract
Developmental prosopagnosia has received increased attention in recent years, but as yet has no confirmed genetic or structural markers. It is not certain whether this condition reflects simply the low-end of the spectrum of normal face recognition, an ‘under-development’, or a pathologic failure to develop such mechanisms, a ‘mal-development’. This difference in views creates challenges for the diagnosis of developmental prosopagnosia by behavioural criteria alone, which also vary substantially between studies, with secondary effects on issues such as determining its prevalence. After review of the literature and the problems inherent to diagnoses based solely on behavioural data, we propose as a starting discussion point a set of two primary and four secondary criteria for the diagnosis of developmental prosopagnosia.
Keywords: face recognition, diagnosis, perception, development, prosopagnosia
The definition of developmental prosopagnosia is deceptively simple: a life-long difficulty in recognizing or learning to recognize faces. When the disorder is severe it leads to anecdotes that stand apart from typical human experience: failures to recognize one’s own image in the mirror, mistaking siblings who change their hairstyle for strangers, and an inordinate reliance on voice to identify people, when for most people voices are far inferior to faces as cues to identity (Barsics & Bredart, 2012). Most would agree that subjects who describe such experiences likely have an anomalous mechanism for face recognition. However, operationalizing these impressions and translating the definition into diagnostic criteria has challenges and complexities that cannot be denied.
How is it currently done? Not surprisingly, but no less unfortunate for that, this varies considerably between studies, as can be seen in an illustrative sample of reports spanning recent years (Table 1). Some document the inability to identify famous faces by name, others poor short-term familiarity with recently viewed faces. Some include impaired discrimination between faces, although the ability to do this is no guarantee that one can recognize faces. Some require subjects to complain of problems with face recognition in daily life, and some formalize this with a questionnaire and use this in lieu of behavioural testing. Some studies require meeting only one or two of these various criteria, while others insist on fulfillment of several. Even when the same test is applied, the criterion for diagnosis varies: with the Cambridge Face Memory Test, there are studies that use 1.7 standard deviations, 2 standard deviations, or a set numerical score.
Table 1. Diagnostic criteria for developmental prosopagnosia in various studies.
| STUDY | HISTORY (SELF-REPORT) |
BEHAVIOURAL TESTING |
||||||
|---|---|---|---|---|---|---|---|---|
| Citation | family | Life-long | Daily | familiarity for faces |
famous face identification |
face discrimination |
||
|
|
||||||||
| (Towler, Parketny, & Eimer, 2015) | × | × | and both of | CFMT [2], old/new | and | × | ||
| (Parketny, Towler, & Eimer, 2015) | × | × | and both of | CFMT [2], old/new | and | × | ||
| (Yovel & Duchaine, 2006) | × | × | and both | CMFT [2], old/new | and | × | ||
| (Bate, et al., 2014) | × | and | CFMT [2] | and | × | |||
| (Song, et al., 2015) | × | and | CFMT [Crawford] | and | × | |||
| (Garrido, et al., 2009)] | × | and | CMFT [Crawford] | and | × | |||
| (Duchaine & Nakayama, 2005) | × | and 3 of | OIT, old/new (×2) | or | × | |||
| (Harris et al, 2005) | × | and 1 of | old/new (×2) | and | × | |||
| (Minnebusch, et al, 2007) | × | and | WRMT | and all of | X (×2), caricatures | |||
| (Yardley, et al., 2008) | × | × | and | CFMT {44} | ||||
| (Liu, et al., 2015) | × | × | and both of | CFMT [2], WRMT | ||||
| (DeGutis, et al., 2014) | × | and | CFMT [1.7] | |||||
| (Duchaine & Nakayama, 2004) | × | and 2 of | OIT, old/new (×2) | |||||
| (de Haan et al, 1999) | × | × | and | famous | and | × | ||
| (Zhang, Liu, & Xu, 2015) | × | × | and | × | ||||
| (Le Grand, et al., 2006) | × | × | and 1 of | X (×2) | ||||
| (Grueter, et al., 2007) | × | × | ||||||
| (Kennerknecht, et al., 2006)] | × | × | ||||||
| (Kennerknecht, et al., 2008) | × | |||||||
| (Sha, et al, 2015) | CFMT | |||||||
| (Burns et al, 2014) | CFMT [2] | and | × | |||||
| (Burns, et al., 2014) | and | × | matching | |||||
| (Righart & de Gelder, 2007) | BFRT, matching RT | |||||||
CMFT = Cambridge Face Memory Test; WRMT = Warrington Recognition Memory Test; BFRT = Benton Face Recognition Test; OIT = One-in-Ten
famous = yes/no familiarity judgement of famous face
(×2) = 2 similar or idential versions of a test given.
[n] = CFMT standard deviation criterion
{n} = CFMT score criterion
[Crawford] = score must differ by Crawford’s t-statistic
Some of the difficulties created by this diagnostic heterogeneity will be discussed later. However, a more fundamental issue with behavioural tests and questionnaires is the diagnostic inference they afford. All of these instruments claim to indicate a problem when a subject’s score falls below a certain criterion. The crux is what we can infer when that happens.
The normative and the pathologic view
To reflect upon this, we must consider one of the key issues about this diagnosis: its pathogenetic implication. First of all, as with any human ability, face recognition skills vary in the normal population (Bowles, et al., 2009; Wilmer, et al., 2010; Zhu, et al., 2010), and the results of any test of these skills will reflect that variability. Thus there will be both those who never forget a face, the super-recognizers (Russell, Duchaine, & Nakayama, 2009), and those who are bad with faces. These are quantitative rather than qualitative differences. Nevertheless, should we consider those on the less-skilled end of this spectrum to have developmental prosopagnosia?
Most would suggest not. Accepting this view means attaching a label to a segment of the normal population, creating a discrete category where there is only continuous variation. This is exactly the concern of those who see the medicalization of normal traits as an insidious sociologic problem (Conrad, 1992). Rather, an alternate view is to see developmental prosopagnosia as a distinct entity, the product not of weaker than average development, but of development gone wrong. In statistical terms, this should result in a population that is not just the tail end of the bell curve, but its own separate cluster in performance space.
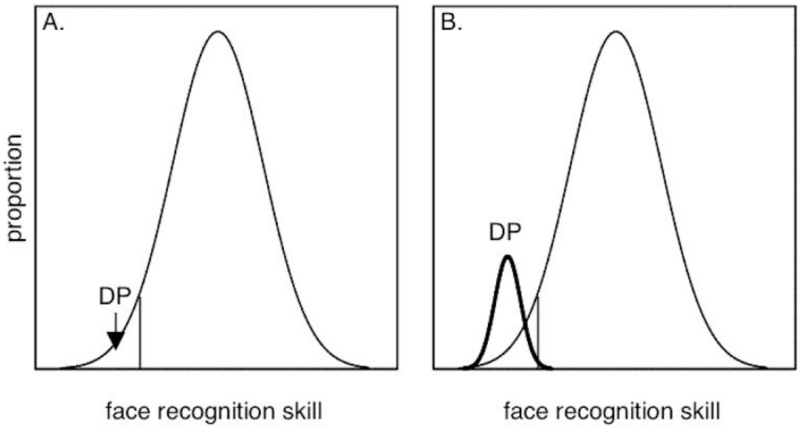
We can call these two different views the normative and the pathologic view (Figure 1). In the normative view, developmental prosopagnosia is a statistical phenomenon, the deficient end of a normal distribution that has reduced but not aberrant face processing. In the pathologic view, it is a distinct population created by a failure of normal face processes to develop. While the pathologic view seems most consistent with the concepts most researchers hold about developmental prosopagnosia - consider, for example, the speculations about genetic mutations (Gruter, Gruter, & Carbon, 2008) and neural migration errors (Susilo & Duchaine, 2013) - it creates a diagnostic challenge. After all, this view does not deny that the normal distribution of face processing skills includes individuals who are less adept at face recognition. However, it does assert that there is a difference between those who are just ‘bad at faces’, the tail end of the normal population’s distribution, and those who have developmental prosopagnosia, an anomalous subgroup. Hence a challenge for the pathologic view is to distinguish between those bad at faces and those with developmental prosopagnosia. This is not a problem for the normative view, because in that view those who are bad with faces are precisely those with developmental prosopagnosia.
Figure 1.
Two views of developmental prosopagnosia. The graphs plot hypothetical proportions of subjects in the population as a function of their face recognition skill, which increases along the x-axis. A. The normative view. Face recognition is a continuous, normally distributed ability in the population, and those with developmental prosopagnosia (DP) are those on the low-end of this spectrum. B. The pathologic view. In addition to this normally distributed ability, there is a discrete population of developmental prosopagnosia subjects (bold curve, labeled DP) with different face processing mechanisms. These overlap with the low end of the distribution of the normal population.
Failure to keep these different concepts clear can lead to some interesting conclusions. For example, there is the claim that the prevalence of developmental prosopagnosia in the general population is around 2 to 3%, which is echoed in the introduction to many research papers (e.g. DeGutis, Cohan, & Nakayama, 2014; Rivolta, Schmalzl, Coltheart, & Palermo, 2010; Tree & Wilkie, 2010; Yardley, McDermott, Pisarski, Duchaine, & Nakayama, 2008) and reviews (Gruter, et al., 2008; Susilo & Duchaine, 2013). Where did this number come from? Initial work derived this from screening questionnaires in relatively large groups of high school or medical students, followed by semi-structured interviews (Kennerknecht, et al., 2006; Kennerknecht, Ho, & Wong, 2008; Kennerknecht, Plumpe, Edwards, & Raman, 2007). However, many find interview-based diagnoses unsettling, particularly when no criteria are given for establishing or rejecting the diagnosis in the screened subjects. Thus, although it was claimed that the conclusions derived from interviews and the results of face recognition tests were congruent in another, smaller sample (Grueter, et al., 2007; Kennerknecht, et al., 2008), others have insisted that it would be ‘essential’ to confirm interview-based diagnoses with testing (Duchaine, 2008). Following this, a study derived a similar prevalence estimate of 2 to 2.9% for developmental prosopagnosia by determining how many subjects in a relatively unselected sample scored more than two standard deviations below the mean on the Cambridge Face Memory or Cambridge Face Perception Tests (Bowles, et al., 2009). But of course, that is exactly what the statistical concept of two standard deviations implies, that the normal variation of ability in a population will result in the scores of 2.5% of people falling below this limit. While this claim of a prevalence of 2.5% is therefore tautologic - one could create any prevalence desired just by changing the diagnostic criterion for abnormal performance from 2 standard deviations to some other value - such an exercise also suggests a normative view. Indeed, the data in Figure 5 of (Bowles, et al., 2009) suggests a broad normally distributed function for scores of the Cambridge Face Memory Test, without any specific indication that low-scoring subjects form a distinct group.
Other aids to diagnosis
Frankly, if one subscribes to the pathologic view, there is no way that one can statistically infer from the fact that someone falls below a performance criterion on any behavioural test of face recognition that they have developmental prosopagnosia rather than being ‘bad with faces’. Hence the challenge is to find some other characteristic that will separate the developmental prosopagnosic from the person bad at faces.
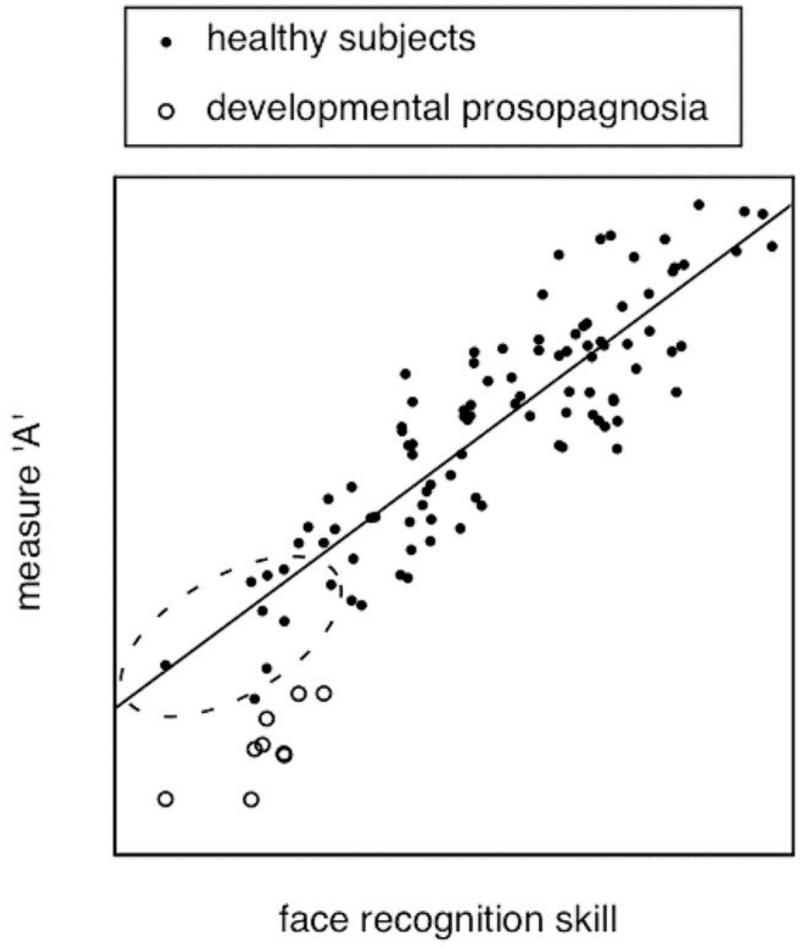
Are there markers in perceptual performance that could potentially segregate developmental prosopagnosic subjects from normal subjects who are bad with faces, markers that can show a discontinuity between these groups rather than a spectrum of ability? There are numerous candidate observations: lack of a face-inversion effect (Behrmann, Avidan, Marotta, & Kimchi, 2005), lack of holistic processing (Avidan, Tanzer, & Behrmann, 2011), paradoxically better processing of the mouth than the eye region (DeGutis, Cohan, Mercado, Wilmer, & Nakayama, 2012), anomalous scanning of faces (Schwarzer, et al., 2007), and so on. The terms ‘lack of’ and ‘anomalous’ might suggest discrete phenomena, but sometimes the results show reduced rather than absent effects (for review see DeGutis, et al., 2012). Furthermore, all of these effects are measured with continuous variables such as accuracy and reaction time, and what is required is evidence that the performance of developmental prosopagnosic subjects stands apart from normal variability on these measures. For example, one possibility would be if, for a given level of face recognition ability, developmental prosopagnosic subjects had scores on a measure that were clearly different from that predicted from the variation in performance of the normal population (Figure 2). However, the individual differences in face-related measures in the healthy population and how these co-vary with normal face recognition skills are only just beginning to be studied (Degutis, Mercado, Wilmer, & Rosenblatt, 2013; DeGutis, Wilmer, Mercado, & Cohan, 2013). Caution is also required with some of these observations: it may be that certain anomalous phenomena could reflect adaptive strategies that any subject who struggles with face processing – including those just bad at faces - might use.
Figure 2.
A hypothetical qualitative difference in perceptual performance that might distinguish developmental prosopagnosia from those bad at faces. Suppose that there is some perceptual measure A that is a linear function of face recognition skill in the normal population, so that those on the low end of the normal distribution still follow this linear function. If the developmental prosopagnosic subjects performed worse on measure A than predicted by the linear relationship in healthy subjects, then they would occupy a part of this performance space that was distinct from that containing those simply bad at faces (the dashed oval).
Could heredity be a marker of developmental prosopagnosia? There are subjects who report parents and siblings with similar difficulties (Kennerknecht, et al., 2006; Kennerknecht, et al., 2008), and there are well-studied families in whom developmental prosopagnosia appears to be inherited in an autosomal dominant fashion (Grueter, et al., 2007; Lee, Duchaine, Wilson, & Nakayama, 2010). However, this cannot guarantee that one is dealing with an inborn error and not just normal variation. Nowhere is it written that the hereditary tendencies of normal perceptual skills or memory capacity are any less than those of other human qualities such as tallness, athletic ability or general intelligence, for example. A man who is bad with faces may have a child who takes after his father, without this necessarily implying that they both have a developmental disorder. Indeed, recent studies of twins show a strong hereditary element to face perception and face recognition skills in the normal population (Wilmer, et al., 2010; Zhu, et al., 2010). Conversely, lack of a familial component does not exclude aberrant development of face recognition due to embryonic environmental factors or de novo mutations.
Of course things are more straightforward for acquired prosopagnosia. For one, subjects realize that their poor face recognition is a discontinuity from their pre-morbid ability: something happened, outside of their prior normal experience. More importantly, most have lesions on neuroimaging that provide a plausible pathologic corollary to and basis for their perceptual complaints. In fact, in the absence of such discrete structural changes, the diagnosis has to be subject to doubt. At this time, there are no similar structural anomalies that can provide similar reassurance for the diagnosis of developmental prosopagnosia.
Naturally these diagnostic issues with developmental prosopagnosia are familiar to neuropsychologists and psychiatrists, who often deal with conditions with as yet no genetic, biochemical or neuroimaging markers. When one is limited to behavioral observations to define a condition, there is an understandable insistence on rigorous adherence to lists of diagnostic criteria (consider the Diagnostic and Statistical Manual of Mental Disorders). This is not necessarily how biology works, but a reflection of the needs of scientific communication. How can we ensure that two groups of subjects studied by two different investigators in disparate parts of the globe have the same condition? How can we know that the mechanistic discoveries made with one group apply to another group, or that a treatment for one will also work for the second? Lacking other markers, one strives for homogeneity of the behavioural phenotype. Once genetic or structural markers are found, though, everything changes. Often this is followed by a revision of the behavioural criteria, typically with both a widening of the range of possible phenotypes and also a reporting of mimicking conditions that meet the previous behavioural criteria but have a different pathologic basis. Thus genetic or structural homogeneity replaces behavioural homogeneity as the grounds for clarity in diagnosis.
Concluding remarks
Faced with these challenges, what are we to do? Others have recently grappled with this, and their suggestions are worth reviewing (Dalrymple & Palermo, 2016). We agree with them that objective confirmation of poor familiarity for faces on two or more tests seems prudent (Table 2). Most common in recent years has been the Cambridge Face Memory Test (Duchaine & Nakayama, 2006), which probes the ability to become familiar with recently viewed faces, along with a test of famous face familiarity or identification1 (Table 1). Statistical cut-offs are always somewhat empiric, but again some uniformity across the field is desirable. The use of appropriate single-subject statistics is important and establishing 95% prediction limits (Whitmore, 1986) or using Crawford’s T-test (Crawford & Howell, 1998) seems reasonable, as discussed recently (Dalrymple & Palermo, 2016). However, the consistency of having poor scores on more than one test simply indicates that these are not likely chance occurrences. They still do not discriminate between the subject who is simply at the low end of the normal distribution and the one with aberrant development. Subjective observations of poor face recognition impacting daily life seem a reasonable requirement, with or without the use of a questionnaire. However, one has to admit that a) this will exclude the occasional subject with developmental prosopagnosia who has not yet realized that their experience with faces is anomalous (thus this may not be a useful criterion to apply in studies of children) and b) there is no logical reason why healthy subjects who are bad at faces may not have similar complaints.
Table 2.
Proposed diagnostic criteria for developmental prosopagnosia
|
Beyond the point of establishing the existence of a problem with face recognition, there is the equally important task of confirming that there is not another explanation for this difficulty, which we propose for discussion as a suggested secondary diagnostic criteria. First, the use of visual and neuropsychologic tests to exclude more general problems of perception or memory severe enough to account for poor face recognition is standard in work on acquired prosopagnosia, and this should be the same for developmental prosopagnosia. For basic visual functions, adequate visual acuity and sufficient preservation of the central visual field would be a minimum. Some reports have gone further and measured contrast sensitivity, contour detection, judgments of orientation, size and length (Bate, et al., 2014; Behrmann, et al., 2005) but one can discuss whether this extra effort is necessary. (Impaired curvature perception was reported in one atypical case (Kosslyn, Hamilton, & Bernstein, 1995) though this finding was later questioned (Barton, Cherkasova, Press, Intriligator, & O’Connor, 2003)). Neuropsychological tests should exclude general visual agnosia by confirming that subjects can recognize objects at a basic category level (e.g. faces, cars, trees), though difficulty distinguishing between specific items in other categories (e.g. which face, which car, which tree) should not be grounds for exclusion, given ongoing debates about whether the prosopagnosic deficit is face-specific (Barton & Corrow, 2016). Detailed screening of memory can be done, but a statistically significant discrepancy between good short-term memory for words and poor familiarity for faces on the Warrington Recognition Memory test (Warrington, 1984) may serve a similar purpose (Corrow, et al., 2016; Liu, Corrow, Pancaroglu, Duchaine, & Barton, 2015).
Second, subjects should have intact familiarity for names and voices. If they cannot, they have a multi-modal problem with person recognition (Gainotti, 2013). This could be a syndrome in which a face recognition deficit that is no different from that in developmental prosopagnosia is clustered with a number of other independent recognition defects in other modalities, but it could also be a disorder due to damage to some overarching amodal process, in which case the mechanism underlying impaired face recognition would be quite different. Without knowing which is true one should at least document person recognition in other modalities and consider whether the data suggest grounds for exclusion on the basis that the subject actually has a different cognitive problem and diagnosis. Currently this documentation is usually done only by subjective report. However, testing for name familiarity is relatively simple (Barton, Cherkasova, & O’Connor, 2001). Testing voice familiarity is more of a challenge, given that there are no standard tests and that people are generally poorer at voice recognition than face recognition. Nevertheless, some prosopagnosic studies have used tests of discrimination and short-term familiarity for recently heard voices, with the disconcerting finding that people’s opinions about their ability to recognize voices is not always accurate (Hills, Pancaroglu, Duchaine, & Barton, 2015; Liu, et al., 2015).
Third, one should exclude other neurologic conditions that are associated with impaired face recognition. When the recognition problem is present from an early age, this means mainly autism spectrum disorders, for which the Autism Questionnaire is a reasonable screening tool (Baron-Cohen, Wheelwright, Skinner, Martin, & Clubley, 2001).
Finally, the need to exclude structural lesions with neuroimaging may be debated – particularly as this incurs a considerable expense - but some studies have done so (Avidan, Hasson, Malach, & Behrmann, 2005; Behrmann, et al., 2005; Duchaine, 2008; Liu, et al., 2015). Face recognition difficulties from early acquired lesions can mimic developmental prosopagnosia and the mixing of the two may confuse the field (Barton, Cherkasova, Press, Intriligator, & O’Connor, 2003). Without more imaging data to clarify the incidence of early acquired lesions among subjects who would otherwise be diagnosed as having developmental prosopagnosia, it is difficult to comment upon how serious a confound lack of imaging introduces to this field of study.
It must be acknowledged that, even if all these criteria are met, one could still be dealing with a subject who is just bad with faces. Accepting this means accepting a source of heterogeneity in research on developmental prosopagnosia that stems from diagnostic uncertainty, and conflicting results and failures to replicate effects may reflect this heterogeneity rather than variability from technical or methodological differences. This source of noise in the field will not be resolved until better and more discrete markers of the condition are found, either among perceptual effects, genetic mutations, or subtle structural anomalies. And if none of these surface? We may then have to face the possibility that the pathologic view is wrong, that maybe there is no maldevelopment, only under-development. In which case, developmental prosopagnosia is just being bad with faces. This would not necessarily invalidate this condition as a field of research, but the difference in concept would have an impact on the way we approach its study, in searching for its genetic and structural origins, for example, and how we interpret the results of such study.
Highlights.
This commentary focuses on ambiguities in concepts about developmental prosopagnosia.
Is this condition merely the low end of normal or a product of aberrant development?
How is this reflected in our diagnostic criteria, which vary between studies?
A set of primary and secondary diagnostic criteria is proposed for discussion.
Acknowledgements
Brad Duchaine participated in helpful discussions about this manuscript. JB is supported by a Canada Research Chair and the Marianne Koerner Chair in Brain Diseases. SC is supported by National Eye Institute of the National Institutes of Health under award number F32 EY023479-02 and the Loan Repayment Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Identification or naming may be a step too far. One can have a semantic deficit or anomia in which the subject has intact face familiarity but cannot name or provide biographical data about the person. Nevertheless, if the subject does not recognize a face as familiar, it is unlikely that they will then identify the face by name or other information.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Avidan G, Hasson U, Malach R, Behrmann M. Detailed exploration of face-related processing in congenital prosopagnosia: 1. functional neuroimaging findings. J Cogn Neurosci. 2005;17:1150–1167. doi: 10.1162/0898929054475145. [DOI] [PubMed] [Google Scholar]
- Avidan G, Tanzer M, Behrmann M. Impaired holistic processing in congenital prosopagnosia. Neuropsychologia. 2011;49:2541–2552. doi: 10.1016/j.neuropsychologia.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31:5–17. doi: 10.1023/a:1005653411471. [DOI] [PubMed] [Google Scholar]
- Barsics C, Bredart S. Recalling semantic information about newly learned faces and voices. Memory. 2012;20:527–534. doi: 10.1080/09658211.2012.683012. [DOI] [PubMed] [Google Scholar]
- Barton J, Cherkasova M, O’Connor M. Covert recognition in acquired and developmental prosopagnosia. Neurology. 2001;57:1161–1167. doi: 10.1212/wnl.57.7.1161. [DOI] [PubMed] [Google Scholar]
- Barton J, Cherkasova M, Press D, Intriligator J, O’Connor M. Developmental prosopagnosia: a study of three patients. Brain and Cognition. 2003;51:12–30. doi: 10.1016/s0278-2626(02)00516-x. [DOI] [PubMed] [Google Scholar]
- Barton JJ, Cherkasova MV, Press DZ, Intriligator JM, O’Connor M. Developmental prosopagnosia: a study of three patients. Brain Cogn. 2003;51:12–30. doi: 10.1016/s0278-2626(02)00516-x. [DOI] [PubMed] [Google Scholar]
- Barton JJ, Corrow SL. Selectivity in acquired prosopagnosia: The segregation of divergent and convergent operations. Neuropsychologia. 2016;83:76–87. doi: 10.1016/j.neuropsychologia.2015.09.015. [DOI] [PubMed] [Google Scholar]
- Bate S, Cook SJ, Duchaine B, Tree JJ, Burns EJ, Hodgson TL. Intranasal inhalation of oxytocin improves face processing in developmental prosopagnosia. Cortex. 2014;50:55–63. doi: 10.1016/j.cortex.2013.08.006. [DOI] [PubMed] [Google Scholar]
- Behrmann M, Avidan G, Marotta JJ, Kimchi R. Detailed exploration of face-related processing in congenital prosopagnosia: 1. Behavioral findings. J Cogn Neurosci. 2005;17:1130–1149. doi: 10.1162/0898929054475154. [DOI] [PubMed] [Google Scholar]
- Bowles DC, McKone E, Dawel A, Duchaine B, Palermo R, Schmalzl L, Rivolta D, Wilson CE, Yovel G. Diagnosing prosopagnosia: effects of ageing, sex, and participant-stimulus ethnic match on the Cambridge Face Memory Test and Cambridge Face Perception Test. Cogn Neuropsychol. 2009;26:423–455. doi: 10.1080/02643290903343149. [DOI] [PubMed] [Google Scholar]
- Burns EJ, Tree JJ, Weidemann CT. Recognition memory in developmental prosopagnosia: electrophysiological evidence for abnormal routes to face recognition. Front Hum Neurosci. 2014;8:622. doi: 10.3389/fnhum.2014.00622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad P. Medicalization and Social-Control. Annual Review of Sociology. 1992;18:209–232. [Google Scholar]
- Corrow JC, Corrow SL, Lee E, Pancaroglu R, Burles F, Duchaine B, Iaria G, Barton JJ. Getting lost: Topographic skills in acquired and developmental prosopagnosia. Cortex. 2016;76:89–103. doi: 10.1016/j.cortex.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford JR, Howell DC. Comparing an individual’s test score against norms derived from small samples. The Clinical Neuropsychologist. 1998;12:482–486. [Google Scholar]
- Dalrymple KA, Palermo R. Guidelines for studying developmental prosopagnosia in adults and children. Wiley Interdiscip Rev Cogn Sci. 2016;7:73–87. doi: 10.1002/wcs.1374. [DOI] [PubMed] [Google Scholar]
- De Haan EH. A familial factor in the development of face recognition deficits. J Clin Exp Neuropsychol. 1999;21:312–315. doi: 10.1076/jcen.21.3.312.917. [DOI] [PubMed] [Google Scholar]
- DeGutis J, Cohan S, Mercado RJ, Wilmer J, Nakayama K. Holistic processing of the mouth but not the eyes in developmental prosopagnosia. Cogn Neuropsychol. 2012;29:419–446. doi: 10.1080/02643294.2012.754745. [DOI] [PubMed] [Google Scholar]
- DeGutis J, Cohan S, Nakayama K. Holistic face training enhances face processing in developmental prosopagnosia. Brain. 2014;137:1781–1798. doi: 10.1093/brain/awu062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degutis J, Mercado RJ, Wilmer J, Rosenblatt A. Individual differences in holistic processing predict the own-race advantage in recognition memory. PLoS One. 2013;8:e58253. doi: 10.1371/journal.pone.0058253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGutis J, Wilmer J, Mercado RJ, Cohan S. Using regression to measure holistic face processing reveals a strong link with face recognition ability. Cognition. 2013;126:87–100. doi: 10.1016/j.cognition.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Duchaine B. Comment on prevalence of hereditary prosopagnosia (HPA) in Hong Kong Chinese population. Am J Med Genet A. 2008;146A:2860–2862. doi: 10.1002/ajmg.a.32548. [DOI] [PubMed] [Google Scholar]
- Duchaine B, Nakayama K. Dissociations of face and object recognition in developmental prosopagnosia. J Cogn Neurosci. 2005;17:249–261. doi: 10.1162/0898929053124857. [DOI] [PubMed] [Google Scholar]
- Duchaine B, Nakayama K. The Cambridge Face Memory Test: results for neurologically intact individuals and an investigation of its validity using inverted face stimuli and prosopagnosic participants. Neuropsychologia. 2006;44:576–585. doi: 10.1016/j.neuropsychologia.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Duchaine BC, Nakayama K. Developmental prosopagnosia and the Benton Facial Recognition Test. Neurology. 2004;62:1219–1220. doi: 10.1212/01.wnl.0000118297.03161.b3. [DOI] [PubMed] [Google Scholar]
- Gainotti G. Is the right anterior temporal variant of prosopagnosia a form of ‘associative prosopagnosia’ or a form of ‘multimodal person recognition disorder’? Neuropsychol Rev. 2013;23:99–110. doi: 10.1007/s11065-013-9232-7. [DOI] [PubMed] [Google Scholar]
- Garrido L, Furl N, Draganski B, Weiskopf N, Stevens J, Tan GC, Driver J, Dolan RJ, Duchaine B. Voxel-based morphometry reveals reduced grey matter volume in the temporal cortex of developmental prosopagnosics. Brain. 2009;132:3443–3455. doi: 10.1093/brain/awp271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grueter M, Grueter T, Bell V, Horst J, Laskowski W, Sperling K, Halligan PW, Ellis HD, Kennerknecht I. Hereditary prosopagnosia: the first case series. Cortex. 2007;43:734–749. doi: 10.1016/s0010-9452(08)70502-1. [DOI] [PubMed] [Google Scholar]
- Gruter T, Gruter M, Carbon CC. Neural and genetic foundations of face recognition and prosopagnosia. J Neuropsychol. 2008;2:79–97. doi: 10.1348/174866407x231001. [DOI] [PubMed] [Google Scholar]
- Harris AM, Duchaine BC, Nakayama K. Normal and abnormal face selectivity of the M170 response in developmental prosopagnosics. Neuropsychologia. 2005;43:2125–2136. doi: 10.1016/j.neuropsychologia.2005.03.017. [DOI] [PubMed] [Google Scholar]
- Hills CS, Pancaroglu R, Duchaine B, Barton JJ. Word and text processing in acquired prosopagnosia. Ann Neurol. 2015;78:258–271. doi: 10.1002/ana.24437. [DOI] [PubMed] [Google Scholar]
- Kennerknecht I, Grueter T, Welling B, Wentzek S, Horst J, Edwards S, Grueter M. First report of prevalence of non-syndromic hereditary prosopagnosia (HPA) Am J Med Genet A. 2006;140:1617–1622. doi: 10.1002/ajmg.a.31343. [DOI] [PubMed] [Google Scholar]
- Kennerknecht I, Ho NY, Wong VC. Prevalence of hereditary prosopagnosia (HPA) in Hong Kong Chinese population. Am J Med Genet A. 2008;146A:2863–2870. doi: 10.1002/ajmg.a.32552. [DOI] [PubMed] [Google Scholar]
- Kennerknecht I, Plumpe N, Edwards S, Raman R. Hereditary prosopagnosia (HPA): the first report outside the Caucasian population. J Hum Genet. 2007;52:230–236. doi: 10.1007/s10038-006-0101-6. [DOI] [PubMed] [Google Scholar]
- Kosslyn S, Hamilton S, Bernstein J. The perception of curvature can be selectively disrupted in prosopagnosia. Brain Cognition. 1995;27:36–58. doi: 10.1006/brcg.1995.1003. [DOI] [PubMed] [Google Scholar]
- Le Grand R, Cooper PA, Mondloch CJ, Lewis TL, Sagiv N, de Gelder B, Maurer D. What aspects of face processing are impaired in developmental prosopagnosia? Brain Cogn. 2006;61:139–158. doi: 10.1016/j.bandc.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Lee Y, Duchaine B, Wilson HR, Nakayama K. Three cases of developmental prosopagnosia from one family: detailed neuropsychological and psychophysical investigation of face processing. Cortex. 2010;46:949–964. doi: 10.1016/j.cortex.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Liu RR, Corrow SL, Pancaroglu R, Duchaine B, Barton JJ. The processing of voice identity in developmental prosopagnosia. Cortex. 2015;71:390–397. doi: 10.1016/j.cortex.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnebusch DA, Suchan B, Ramon M, Daum I. Event-related potentials reflect heterogeneity of developmental prosopagnosia. Eur J Neurosci. 2007;25:2234–2247. doi: 10.1111/j.1460-9568.2007.05451.x. [DOI] [PubMed] [Google Scholar]
- Parketny J, Towler J, Eimer M. The activation of visual face memory and explicit face recognition are delayed in developmental prosopagnosia. Neuropsychologia. 2015;75:538–547. doi: 10.1016/j.neuropsychologia.2015.07.009. [DOI] [PubMed] [Google Scholar]
- Righart R, de Gelder B. Impaired face and body perception in developmental prosopagnosia. Proc Natl Acad Sci U S A. 2007;104:17234–17238. doi: 10.1073/pnas.0707753104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivolta D, Schmalzl L, Coltheart M, Palermo R. Semantic information can facilitate covert face recognition in congenital prosopagnosia. J Clin Exp Neuropsychol. 2010;32:1002–1016. doi: 10.1080/13803391003662710. [DOI] [PubMed] [Google Scholar]
- Russell R, Duchaine B, Nakayama K. Super-recognizers: people with extraordinary face recognition ability. Psychon Bull Rev. 2009;16:252–257. doi: 10.3758/PBR.16.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer G, Huber S, Gruter M, Gruter T, Gross C, Hipfel M, Kennerknecht I. Gaze behaviour in hereditary prosopagnosia. Psychol Res. 2007;71:583–590. doi: 10.1007/s00426-006-0068-0. [DOI] [PubMed] [Google Scholar]
- Shah P, Gaule A, Gaigg SB, Bird G, Cook R. Probing short-term face memory in developmental prosopagnosia. Cortex. 2015;64:115–122. doi: 10.1016/j.cortex.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Song S, Garrido L, Nagy Z, Mohammadi S, Steel A, Driver J, Dolan RJ, Duchaine B, Furl N. Local but not long-range microstructural differences of the ventral temporal cortex in developmental prosopagnosia. Neuropsychologia. 2015;78:195–206. doi: 10.1016/j.neuropsychologia.2015.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susilo T, Duchaine B. Advances in developmental prosopagnosia research. Curr Opin Neurobiol. 2013;23:423–429. doi: 10.1016/j.conb.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Towler J, Parketny J, Eimer M. Perceptual face processing in developmental prosopagnosia is not sensitive to the canonical location of face parts. Cortex. 2015 doi: 10.1016/j.cortex.2015.10.018. [DOI] [PubMed] [Google Scholar]
- Tree JJ, Wilkie J. Face and object imagery in congenital prosopagnosia: a case series. Cortex. 2010;46:1189–1198. doi: 10.1016/j.cortex.2010.03.005. [DOI] [PubMed] [Google Scholar]
- Warrington E. Warrington Recognition Memory Test. Western Psychological Services; Los Angeles: 1984. [Google Scholar]
- Whitmore G. Prediction limits for a univariate normal observation. The American Statistician. 1986;40:141–143. [Google Scholar]
- Wilmer JB, Germine L, Chabris CF, Chatterjee G, Williams M, Loken E, Nakayama K, Duchaine B. Human face recognition ability is specific and highly heritable. Proc Natl Acad Sci U S A. 2010;107:5238–5241. doi: 10.1073/pnas.0913053107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardley L, McDermott L, Pisarski S, Duchaine B, Nakayama K. Psychosocial consequences of developmental prosopagnosia: a problem of recognition. J Psychosom Res. 2008;65:445–451. doi: 10.1016/j.jpsychores.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Yovel G, Duchaine B. Specialized face perception mechanisms extract both part and spacing information: evidence from developmental prosopagnosia. J Cogn Neurosci. 2006;18:580–593. doi: 10.1162/jocn.2006.18.4.580. [DOI] [PubMed] [Google Scholar]
- Zhang J, Liu J, Xu Y. Neural decoding reveals impaired face configural processing in the right fusiform face area of individuals with developmental prosopagnosia. J Neurosci. 2015;35:1539–1548. doi: 10.1523/JNEUROSCI.2646-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Q, Song Y, Hu S, Li X, Tian M, Zhen Z, Dong Q, Kanwisher N, Liu J. Heritability of the specific cognitive ability of face perception. Curr Biol. 2010;20:137–142. doi: 10.1016/j.cub.2009.11.067. [DOI] [PubMed] [Google Scholar]