Abstract
Despite suggestions in the literature that depression has serious consequences, few studies have examined specific health and psychosocial outcomes of depression in Black single mothers. The purpose of this study was to estimate paths in a just-identified theoretical model of outcomes of depression for Black single mothers based on theoretical propositions and empirical findings. The model included the variables, depressive cognitions, depressive symptomatology, perceived social support, and positive health practices. Five direct and two indirect hypothesized relationships were estimated using structural equation modeling. A nonprobability sample of convenience of 159 Black single mothers aged 18 to 45 years was recruited for the study. This study used a cross-sectional correlational design. The participants responded in person or via the U.S. mail to the Center for Epidemiologic Studies–Depression scale, the Depressive Cognition Scale, the Personal Resource Questionnaire 85–Part 2, and the Personal Lifestyle Questionnaire. Beta and Gamma path coefficients were statistically significant for four out of five hypothesized direct relationships within the model (p < .01). The direct path between depressive cognitions and positive health practices was not supported (Gamma = −.11, p > .05). The two indirect paths were weak but statistically significant (p < .01). Depressive symptoms and perceived social support were outcomes of depressive cognitions. Positive health practices was not a direct outcome of depressive cognitions. Perceived social support and positive health practices were outcomes of depressive symptoms.
Keywords: structural equation modeling, depression, mental health, Black single mothers
Depression is a serious mental illness that negatively impacts physical health, quality of life, and psychosocial functioning, causing disability and death for some sufferers while increasing morbidity and mortality for others (Lam et al., 2009; Lewinsohn, Seeley, Solomon, & Zeiss, 2000; National Institutes of Mental Health [NIMH], 2009). Black single mothers are a minority population vulnerable to depressive symptoms. Studies have shown that up to 70% of Black single mothers report depressive symptoms consistent with a diagnosis of mild to moderate clinical depression (Hatcher, Rayens, Peden, & Hall, 2008; Kneipp, Welch, Wood, Yucha, & Yarandi, 2007; Siefert, Williams, Finlayson, Delva, & Ismail, 2007), 9 times the rate of depression in the general U.S. population (6.7%; NIMH, 2014). A recent study that tested a theoretical model of depression in Black single mothers has shed light on antecedent variables that explain depression in this population (Atkins, 2015). Although research suggested that depression has negative psychosocial and physical health consequences for multiracial samples of single mothers and their children (Boyd, Zayas, & McKee, 2006; Jackson, Bentler, & Franke, 2008), few studies have examined specific health and psychosocial outcomes of depression in Black single mothers. The purpose of this study was to estimate paths in a just-identified theoretical model of outcomes of depression for Black single mothers based on theoretical propositions and empirical findings. The results of this analysis will provide information that will aide practitioners to improve the health practices and perception of social support for Black single mothers.
Theoretical Model of Outcomes of Depression
Theorists have proposed a relationship between depressive cognitions and depressive symptomatology (Beck, 1967; Zauszniewski, 1995). Depressive cognitions are defined as specific maladaptive cognitive distortions which precede the development of depressive illness or clinical depression (Beck, 1974; Zauszniewski, 1995). These cognitions include feelings of powerlessness, helplessness, purposelessness, worthlessness, loneliness, hopelessness, emptiness, and meaninglessness (Zauszniewski, 1995). In contrast, depressive symptoms include depressed mood, guilt, loss of appetite, sleep disturbances, psychomotor retardation, social withdrawal, self-reproaches, and the desire for self-harm (Radloff, 1977). Theoretically, depressive cognitions are posited to lead to depressive symptoms in adults because, as stated by Robbins (1993), “ … negative thoughts can depress your mood” (p. 2). According to Beck (1967), negative cognitive views about the self, the world, and the future, once activated, dominate a person’s thinking and lead to depressive symptomatology. Abramson, Metalsky, and Alloy (1989) proposed that hopelessness, one of the depressive cognitions, precedes the development of depressive symptomatology which is characterized by lack of energy, psychomotor retardation, lowered self-esteem, and retarded initiations. Essentially, negative cognitions make one vulnerable to depressive symptoms (Alloy, Abramson, Walshaw, & Neeran, 2006), as proposed in the present study.
Studies have shown that depressive cognitions, such as negative thinking, predict depressive symptoms in Black single mothers. Zauszniewski (1997) found a positive correlation (r = .54, p < .001) between depressed cognitions and depressive symptoms in a sample of 160 elderly adults, 42% of whom were African American, who responded to the Depressive Cognition Scale and the Center for Epidemiologic Studies–Depression (CES-D) scale. Peden, Rayens, Hall, and Grant (2004) found a positive correlation (r = .84, p < .0001) between negative thinking and depressive symptoms in a sample of 205 low-income single mothers, who responded to CES-D scale and the Crandell Cognitions Inventory (CCI). Hatcher et al. (2008) found a positive correlation (r = .80, p < .001) between negative thinking and depressive symptoms in a sample of 98 African American single mothers, who responded to the CES-D and the CCI. Based on theory and previous research, the first hypothesis predicted that depressive cognitions will have a direct and positive effect on depressive symptoms in the Black single mothers.
Theorists have proposed a relationship between depression and diminished perception of social support. Perceived social support is conceptualized in the present study as the relational provisions of attachment, social integration, opportunity for nurturance, sense of reliable alliance, and guidance (Weiss, 1974). Klein and Wender (2005) stated that depression leads to social withdrawal, self-isolation, and the belief that others dislike or reject him or her. These feelings make relationships difficult and have the potential to lead to lower levels of perceived social support for depressed individuals. This social withdrawal and self-isolation often leads to perceived loss of social support and resources (Pettit & Joiner, 2006). According to Hammen (2009), depression results in maladaptive ways of construing the self in relation to others and in characteristics that affect the supportiveness of relationship with others. Hence, depression impairs relationships to the point of dissolution and produces behavioral inhibition, shyness, and social withdrawal, all of which can diminish the perception of social support (Hammen, 2009), as proposed in this study.
Studies that have examined the relationship between depressive symptoms and social support in solely Black mothers have found strong support. For example, Coiro (2001) found an inverse correlation (r = −.66, p < .05) between depression and social support in a sample of 173 low-income African American single mothers who responded to the CES-D scale and the questions regarding emotional and instrumental support. Siefert et al. (2007) found an inverse correlation (r = −.49, p < .01) between instrumental social support and depressive symptoms in a sample of 824 low-income African American mothers who responded to the CES-D scale and questions measuring instrumental support.
In more recent studies, moderate to strong support for this relationship has been found in multiethnic samples. An inverse correlation (r = −.41, p < .05) between depression and social support in 336 multiethnic mothers who responded to the Beck Depression Inventory (BDI) and the Social Support Survey (Gjesfield, Greeno, Kim, & Anderson, 2010). Instrumental social support (adjusted odds ratio [AOR] = .93, 95% confidence interval [CI] = [.88, .99], p < .05) and partner social support (AOR = .63, 95% CI = [.55, .73], p < .001) were negatively associated with depression in a sample of multiethnic mothers of young children (Manuel, Martinson, Bledsoe-Mansori, & Bellamy, 2012). Gjesfield et al. argued that the negative thought patterns associated with depressive symptoms could have influenced respondents to underestimate their perception of social support. Another study found a moderate negative relationship between depressive symptoms and social support (r = −.35, p < .05) in 1,383 postpartum mostly married (53.9%) Black mothers, the effects of which was greatly reduced (Gamma = −.08, p < .05) when the effects of social support on depressive symptoms was tested via structural equation modeling (SEM; Giurgescu et al., 2015). The present study will utilize SEM to provide current knowledge to examine the effects of depressive symptoms on social support in a sample of solely single Black mothers or are at heightened risk for depressive symptoms. Based on theory and previous research, the second hypothesis predicted that depressive cognitions will have a direct and negative effect on perceived social support, and the third hypothesis predicted that depressive symptoms will have a direct and negative effect on perceived social support. Furthermore, the fourth hypothesis predicted that depressive cognitions will have an indirect effect on social support through depressive symptoms in Black single mothers.
Theorists have proposed that depression reduces participation in positive health practices. In this study, positive health practices are health behaviors which serve to promote the health of the individual, such as exercise, relaxation, safety, nutrition, avoidance of substance use, and preventive health activities (Brown, Muhlenkamp, Fox, & Osborne, 1983). Billingsley and Billingsley (1987) stated that poor self-care is one of the behavioral outcomes of depression: Individuals who are depressed have poor health maintenance habits, such as lack of exercise and eating well-balanced meals. According to Bandura (2004), personal impediments or obstacles such as depression can decrease a person’s sense of personal efficacy for participating in healthy behaviors. Pender concurs that behavior specific cognitions influence health behaviors (Pender, Murdaugh, & Parsons, 2005). Atkins (2010) additionally explained that depressive cognitions and depressive symptomatology may serve as mental blocks because they are impediments to positive health goal setting, all of which could decrease participation in positive health behaviors. Symptoms of depression “cause decreases in the motivation and drive necessary to engage in health-promoting behaviors” (Atkins, 2010, p. 161).
Moderate empirical support for the relationship between depressive symptoms and health practices has been found in women. These studies, however, are dated and have mainly focused on multiethnic clinical samples and pregnant mothers. Lindgren (2001) found an inverse correlation (r = −.41, p < .05) between depression and health practices in a sample of 252 adult pregnant women who responded to the CES-D scale and the Health Practices Questionnaire (HPQ). Zauszniewski, Chung, Krafcik, and Sousa (2001) found that depressive cognitions had a negate relationship with health practices (r = −.51, p < .001) in a sample of 83 women with type 2 diabetes who responded to the BDI and the Health Promoting Lifestyle Profile. Lindgren (2003) found depressive symptoms had a negative relationship with health practices (B = −.20, p < .05) in a sample of 197 pregnant women who responded to the CES-D scale and the HPQ. These studies used psychometrically sound scales that were measures of multiple health practices. Other studies have found associations between women’s depressive symptoms and single-item measures of specific health practices such as smoking (Siahpush, 2004), and maternal management of child’s preventive health practices (Bartlett et al., 2004; McLennan & Kotelchuck, 2000; Minkovitz et al., 2005) in multiethnic samples. These studies provide moderate support for this relationship in multiethnic samples.
Weak support for the relationship between depressive symptoms and specific health practices has also been found in more recent studies in a sample of multiethnic adults. Depressive symptoms were positively associated with health compromising behaviors such as smoking, binge drinking, risky sexual behaviors, physical inactivity, poor diet, and lack of sleep (B = .12–.20, p < .01) in a sample of multiethnic low-income adults (47% female, 68% African American; Walsh, Senn, & Carey, 2013), and a negative relationship between depressive symptoms and physical activity (r = −.18, p < .01) was found in a multiethnic sample of 542 midlife women (Im, Ham, Chee, & Chee, 2015). The severity of depressive symptoms was associated with increased prevalence of risk behaviors, such as smoking, physical inactivity, and obesity among 18,856 persons with asthma (Strine et al., 2008). Poor health behaviors (i.e., smoking, excessive alcohol consumption, and obesity) were positively associated with risk of depression with a 23% increase in the risk for depression with each successive poor health behavior in a sample of Black and White young adults who responded to the CES-D scale and reported their health behaviors (Boardman & Alexander, 2011).
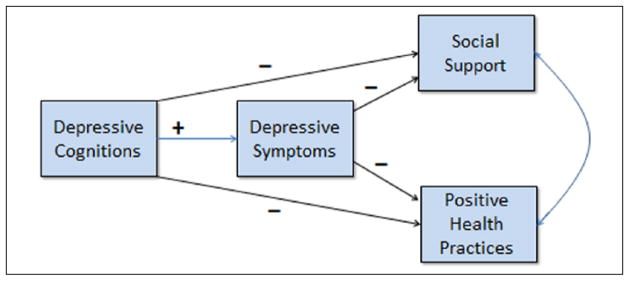
This is the first study to utilize a psychometrically sound measure of a multiple positive health practices to provide current knowledge regarding the nature of the relationship between depressive symptoms and positive health practices in a sample of solely Black single mothers. Based on theory and previous research, the fifth hypothesis predicts that depressive cognitions will have a direct and negative effect on positive health practices and the sixth hypothesis predicts that depressive symptomatology will have a direct and negative effect on positive health practices. Furthermore, the seventh hypothesis predicts that depressive cognitions will have an indirect effect on positive health practices through depressive symptoms in Black single mothers. The proposed model is depicted in Figure 1.
Figure 1.
A priori just-identified recursive model of consequences of depressive cognitions.
Method
Sample
The sample consisted of single mothers between the ages of 18 and 45 years who self-identified as Black. Black single mothers met the following inclusion criteria: (a) never married, widowed, divorced, or separated; and (b) have one or more children living with them. These mothers were physically and mentally able to participate in the study and able to read and comprehend the English language. The sample excluded mothers who were presently receiving psychiatric care or counseling, taking antidepressant medication, pregnant, and who had a child less than 1 year of age.
Sample size for testing the proposed model was based on low to medium correlations between the study variables as found in previously reported empirical findings for relationships in the model, an alpha of .05, and a power of .80 (Cohen, 1988; Tabachnick & Fidell, 2013), and suggested ratio of the number of subjects to the number of free parameters (n = 10) between a 20:1 and 10:1 ratio (Kline, 2005). In this study, a 15:1 ratio was used which yielded a power of .83 and required minimum sample size of 150 subjects (Cohen, 1988).
Instruments
The Depressive Cognition Scale (DCS)
The DCS is an eight-item self-report instrument designed to measure depressive cognitions (Zauszniewski, 1995). Respondents indicate the degree to which particular statements describe their current thoughts on a 6-point summated rating scale. Scores can range from 0 to 40. All eight items on the DCS are worded positively so that higher scores indicate less depressive cognitions. For ease of analysis and interpretation, scores were reversed in this study so that higher scores would indicate more depressive cognitions.
Relative to content validity, 24 items originally were developed based on Erickson’s developmental stages. Five experts in psychiatric nursing evaluated these items and, based on their agreement, narrowed down the final scale to eight items (Zauszniewski, 1995). Evidence of convergent validity was obtained when scores on the DCS correlated positively with scores on the Modified Eriksonian Psychosocial Stage Inventory (MEPSI), a measure of psychosocial attributes (r = .63, p < .05) and the CES-D scale (r = .54, p < .001; Zauszniewski, 1995, 1997) in adults. Concurrent validity was shown when scores on the DCS were negatively related to measures of learned resourcefulness, adaptive functioning, and life satisfaction in African American and European Americans (Zauszniewski, 1997). Factor analysis revealed a unidimensional structure in women including African American women (Zauszniewski, 1997; Zauszniewski, Picot, Debanne, Roberts, & Wykle, 2002). Relative to reliability, adequate coefficient alpha reliabilities ranging from .75 to .92 have been reported for the DCS in adult women, including African American women (Zauszniewski, 1995; Zauszniewski & Bekhet, 2012; Zauszniewski et al., 2002). The alpha coefficient for this sample was .85.
The CES-D scale
The CES-D scale is a 20-item self-report instrument designed to assess current levels of depressive symptoms (Radloff, 1977). Respondents indicate the frequency and duration of which they have experienced certain situations or feelings on a 4-point summated rating scale. A total score was obtained after reversing the scores on four items. The possible range of scores is from 0 to 60, with higher scores indicating more depressive symptomatology.
Relative to content validity, items for the CES-D were selected by Radloff (1977) from previously validated depression scales and the clinical literature. Convergent validity was shown via strong correlations with other measures of depression in adults including African Americans (Caracciolo & Giaquinto, 2002; Radloff, 1977; Wilcox, Field, Prodromidis, & Scafidi, 1998). Evidence of concurrent criterion validity was shown when scores on the CES-D were positively correlated with measures of functional difficulty, psychological distress, physical symptoms of distress, and anxiety, and negatively correlated with measures of spirituality and global health functioning in samples containing African American adults (Gitlin, Hauck, Dennis, & Schulz, 2007; Hann, Winter, & Jacobsen, 1999; Schroevers, Sanderman, van Sonderen, & Ranchor, 2000). Adequate coefficient alpha reliabilities ranging from .83 to .91 have been found for the CES-D in African American mothers (Odom & Vernon-Feagans, 2010; Peden et al., 2004; Siefert et al., 2007). The alpha coefficient for this sample was .91.
The Personal Resource Questionnaire 85–Part 2 (PRQ 85-Part 2)
The PRQ 85-Part 2 (Weinert, 1987) is a 25-item measure of perceived social support as defined conceptually by Weiss (1974). Respondents indicate on a 7-point summated rating scale the degree to which they agree with statements measuring five dimensions of social support. Five negatively worded items were reversed scored. Scores can range from 25 to 175, with higher scores indicating a higher level of perceived social support (Weinert, 1987).
Weinert (1987) established content validity for the PRQ 85-Part 2. Weinert also found a three-factor structure for the PRQ 85-Part 2. Convergent validity was shown when scores for the PRQ 85-Part 2 correlated with the BDI, clinical depression, and the Spielberger Self-Evaluation Questionnaire, a mental health measure (Bai, Chiou, Chang, & Lam, 2008). Adequate coefficient alpha reliabilities ranging from .89 to .93 have been reported in adults including African Americans (Esperat, Feng, Zhang, & Owen, 2007; Willoughby, Kee, & Demi, 2000). The alpha coefficient for this sample was .92.
The Personal Lifestyle Questionnaire (PLQ)
The PLQ is a 24-item self-report scale which measures participation in positive health practices (Muhlenkamp & Brown, 1983). Subjects indicate the extent of their participation in positive health practices on a 4-point summated rating scale ranging from never to almost always. Possible scores range from 24 to 96, with higher scores indicating better health practices.
Items for the PLQ are behaviors or activities consistent with professional literature for self-health care and health protective behaviors (Brown et al., 1983). Convergent validity was shown via significant positive correlations with Pelletier’s Lifestyle Assessment Questionnaire in a sample of adults (Brown et al., 1983). The PLQ has additionally been factor analyzed for adolescents aged 12 to 21 years (Mahon, Yarcheski, & Yarcheski, 2002). Adequate coefficient alpha reliabilities ranging from .74 to .76 were obtained on a sample of adults (Brown et al., 1983). Alpha coefficients of .75 for mothers (Kuster, Badr, Chang, Wuerker, & Benjamin, 2004), .73 for middle-aged adults (McNicholas, 2002), and .85 for adolescents (Mahon, Yarcheski, Yarcheski, & Hanks, 2007) have been reported. The alpha coefficient for this sample was .79.
Data Collection Procedure
The University’s Institutional Review Board (IRB) approved this study. The majority of women were recruited in person from four different sites including a primary care office, a social service agency, a day care center, and a dance school in two inner city communities. The primary investigator approached potential subjects in the waiting areas, screened subjects for inclusion/exclusion criteria, and explained the rights of human subjects. After signing informed consents, all women completed four instrument packets and a demographic data sheet in a quiet area. To increase sample size, a minority of the women were recruited from a larger longitudinal study of depression via the U.S. mail. These women were prescreened by phone to ensure that they met the delimitations for this study before receiving the instrument packets by mail. All participants received US$10.00 for their participation.
Data Analysis
Descriptive statistics were generated via an SPSS computer program and were used to describe demographic characteristics. Pearson correlations were computed between the study variables.
The just-identified model was examined via the LISREL 8 software program (Joreskog & Sorbom, 1993). A bivariate regression analysis was done on the just-identified equation model. A correlated error term for two dependent variables (social support and positive health practices) was used to account for the unhypothesized relationship between them. It was predicted that the model would fit the data perfectly as it is just-identified with 0 df. In structural equation models, path coefficients are either Gammas (between exogenous and endogenous variables) or Betas (between endogenous variables; Joreskog & Sorbom, 1993). Path coefficients and squared multiple correlations, along with direct, indirect, and total effects are obtained in the LISREL program. The path coefficients are identical to maximum likelihood estimates and determine the influence of depressive cognitions (exogenous variables) on depressive symptoms (endogenous variables) and the influence of both on social support and positive health practices (endogenous variables). The language of SEM, which suggests causation, will be used throughout this analysis. However, evidence of causation can never be unquestionably established using SEM (Mason-Hawkes & Holm, 1989). SEM techniques test the plausibility of the hypothesized relationships within the model and are confirmatory, but do not prove causation (Kline, 2005; Tabachnick & Fidell, 2013).
Results
Study Sample
Of the 195 women approached in person to participate in the study, 128 agreed and completed the surveys. Of the 128 who agreed, 122 surveys were usable and the subjects met the inclusion criteria. Of the 52 surveys sent through the U.S. mail, 37 women returned completed surveys and met the inclusion criteria. The final sample consisted of 159 Black single mothers aged 18 to 45 years. The majority of women (90.0%) reported that they were single having never been married, 5.0% were divorced, and 5.0% were separated. Most women reported being head of household (86.7%). Most women also reported having between one to two children (69.8%), while 24.5% had three to four children, 4.4% had five to six children, and the rest gave no response (1.3%; n = 2). The large majority were unemployed 51.6%, while 27.7% worked full-time and 15.7% worked part-time, and the rest gave miscellaneous responses such as being on “maternity leave” and “other” (5.0%; n = 7). Significant mean differences for the main study variables and demographic data were not found based on the data collection method. The participants who participated by mail were initially contacted at the same recruitment sites as those who participated in person. This no doubt helped to prevent significant demographic and characteristic variability between the two samples.
Statistical Analysis
Descriptive statistics for the study variables are presented in Table 1. Pearson correlation coefficients between the study variables are presented in Table 2. All of the correlations between the hypothesized relationships were statistically significant.
Table 1.
Descriptive Statistics for Study Variables.
| Variables | Range | Median | M | SD |
|---|---|---|---|---|
| Depressive cognitions | 0–39 | 4.00 | 5.07 | 5.93 |
| Depressive symptoms | 0–57 | 13.43 | 17.11 | 12.70 |
| Perceived social support | 50–175 | 136.00 | 132.80 | 27.02 |
| Positive health practices | 39–82 | 60.00 | 60.05 | 9.81 |
Table 2.
Correlations Matrix for Study Variables.
| Variables | Depressive cognitions | Depressive symptoms | Positive health practices | Perceived social support |
|---|---|---|---|---|
| Depressive cognitions | 1 | .32* | .19*** | .36* |
| Depressive symptoms | 1 | .30* | .37* | |
| Positive health practices | 1 | .50*** | ||
| Perceived social support | 1 |
p < .01.
p < .05.
Model Testing
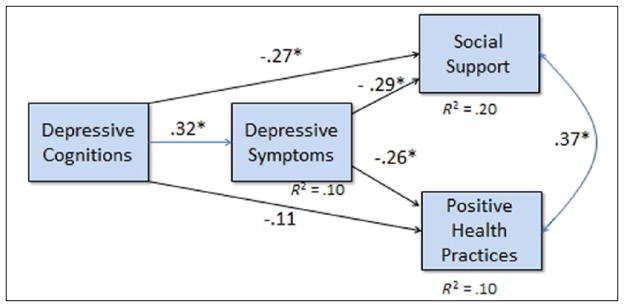
As expected, there was a perfect fit of the model with the data, χ2(0, 159) = .0, p = 1.00. As hypothesized, there was a direct and positive effect of depressive cognitions on depressive symptoms (Gamma = .32, p < .01) and there was a direct and negative effect of depressive cognitions on perceived social support (Gamma = −.27, p < 01). As hypothesized, there was a direct and negative effect of depressive symptoms on perceived social support (Beta = −.29, p < .01). In addition, there was an indirect effect of depressive cognitions on perceived social support through depressive symptoms (B = −.09, p < .01). Although in the predicted negative direction, depressive cognitions did not have a direct effect on positive health practices (Gamma = −.11, ns). Depressive symptoms had a direct and negative effect on positive health practices (Beta = −.26, p < .01). There was an indirect effect of depressive cognitions on positive health practices through depressive symptoms (B = .08, p < .01). The correlated error term between positive health practices and perceived social support was psi = .37, p < .01. The model is presented in Figure 2. The direct, indirect, and total effects are presented in Table 3.
Figure 2.
Empirical results of testing the just-identified model of antecedents and consequences of depression (N = 159).
*p < .01.
Table 3.
Direct, Indirect and Total Effects of Study Variables (N = 159).
| Variables
|
Effects
|
|||
|---|---|---|---|---|
| Dependent | Independent | Direct | Indirect | Total |
| Depressive symptoms | Depressive cognitions | .32** | .00 | .32** |
| Social support | Depressive symptoms | −.29** | .00 | .29** |
| Depressive cognitions | −.27** | −.09* | −.36* | |
| Positive health practices | Depressive symptoms | −.26** | .00 | −.26** |
| Depressive cognitions | .11 | .08* | .19* | |
Note. Indirect effects are estimated statistically as the product of direct effects that comprise them according to the pattern of causation hypothesized in the model. Total effects are the summation of the direct and indirect effects.
p < .01.
p < .001.
Discussion
The just-identified model of depression constructed for Black single mothers predicted five direct hypotheses derived from theoretical propositions and empirical findings and two indirect hypotheses. Four of the five direct hypotheses were supported, and the effect sizes were low to moderate; both of the two indirect hypotheses were supported.
The first hypothesis, derived from theoretical propositions predicting a positive relationship between depressive cognitions and depressive symptoms (Abramson et al., 1989; Beck, 1967; Zauszniewski, 1995), was supported (Gamma = .32, p < .01). However, the path coefficient was weak to moderate, giving modest support for the theoretical relationship between depressive cognitions and depressive symptoms in Black single mothers. Although depressive symptoms were the strongest outcome of depressive cognitions in the model, the strength of the path coefficient was not particularly impressive. Using extant theories, Zauszniewski (1995) synthesized the theoretical basis for the depressive cognitions instrument used in the present study which suggested that depressive cognition is a stable personality characteristic. However, alternative theoretical views of depressive cognitions need to be explored focusing on the nature and pattern of depressive cognitions across nonclinical populations and stages of human development. With a better understanding of the phenomenon, outcomes of depressive cognitions can be more accurately predicted in these populations. Previous researchers have reported strong path coefficients between depressive cognitions and depressive symptoms (Hatcher et al., 2008; Peden et al., 2004); none used SEM to test the relationships as was done in this study, precluding comparison of results across studies (Mason-Hawkes & Holm, 1989). Based on the results of the present study, depressive symptoms are modest manifestations of depressive cognitions, but this finding needs to be replicated in Black single mothers using SEM as well as in other populations. Clinicians should use cognitive behavioral strategies that target the reduction of negative thinking to prevent the progression to clinical depression in Black single mothers.
The second and third hypotheses, derived from theoretical propositions predicting negative relationships of both depressive cognitions (Beta = −.27, p < .01) and depressive symptoms (Gamma = −.29, p < .01) to social support (Hammen, 2009; Klein & Wender, 2005), were supported. The strength of the path coefficient for both relationships was weak to moderate, and both paths give comparable support to the theoretical propositions. Black single mothers who experience depressive phenomena, both cognitions and symptoms, tend to perceive lower levels of social support. These findings are important clinically, especially for depressed individuals who are in need of assistance and social support. This is the first time that the relationship between depressive cognitions and social support has been tested in Black single mothers, thereby providing knowledge about this relationship for this vulnerable sample of women. Similarly, the finding between depressive symptoms and perceived social support adds to the knowledge base for Black single mothers that can be used by clinicians.
The fourth hypothesis inherent in the model, suggesting an indirect relationship between depressive cognitions and social support through depressive symptoms, was weakly supported (B = −.09, p = .05). This finding is not surprising as negative thinking exerts a direct effect on social support (Beta = −.27, p < .01) that is lower, yet nearly equal in magnitude to the direct effect of depressive symptoms on social support (Gamma = −.29, p < .01) in the final model. Hence, in this model, the entire constellation of depressive symptoms plays a small role in explaining the relationship between depressive cognitions and perceived social support by transmitting only a small portion of the causal effects of negative thinking (Kline, 2005; Tabachnick & Fidell, 2013). Nevertheless, these significant findings provide evidence for the mediating role of depressive symptoms in explaining the relationship between depressive cognitions and perceived support. When depressive symptoms are increased due to negative thinking, Black single mothers slightly increase their chances of perceiving less support.
Increasing the perception of support in Black mothers reduces the perception of stress (Giurgescu et al., 2015) that in turn contributes to depressive symptoms (Gruenberg et al., 2015; Hatcher et al., 2008; Odom & Vernon-Feagans, 2010). Clinicians who wish to enhance the perception of support in Black single mothers should take a preventive role by targeting negative thinking which will subsequently reduce depressive symptoms and thereby further enhance perceived support. Interventions to decrease negative thinking have been successful at reducing depressive symptom in low-income single mothers (Peden, Rayens, Hall, & Grant, 2005) and in college women (Peden, Rayens, Hall, & Beebe, 2001).
The fifth and sixth hypotheses were derived from theoretical propositions predicting that depression may serve to reduce participation in positive health practices (Atkins, 2010; Billingsley & Billingsley, 1987; Pender et al., 2005). The fifth hypothesis was not supported suggesting that there is no direct link between depressive cognitions and positive health practices in Black single mothers (Gamma = −.11, p > .05). This finding is not surprising as the negative correlation between these two variables was initially weak (r = .19, p < .05) and thereby disappeared when all included and omitted predictors were held constant via SEM (Kline, 2005). A negative correlation was also found between these two variables by Zauszniewski et al. (2001) in diabetic women (r = −.51, p < .001). However, this more powerful analysis provides more accurate evidence concerning the predictive impact of depressive cognitions on positive health practices. It is clear that depressive cognitions are not powerful enough to interfere with positive health practices and have no direct theoretical implications in relation to positive health practices in Black single mothers.
The sixth hypothesis, however, was supported, indicating a weak to moderate direct and negative link between depressive symptoms and positive health practices (Beta = −.27, p < .01). Looking at the two findings vis-à-vis each other, less participation in positive health practices is an outcome of depressive symptoms as proposed theoretically (Atkins, 2010; Bandura, 2004; Billingsley & Billingsley, 1987). The current findings support those of prior studies that tested this relationship utilizing psychometrically sound scales that measure a variety of health practices (Lindgren, 2001, 2003; Zauszniewski et al., 2001) and those that measured one specific health practice (Im et al., 2015; Walsh et al., 2013) in women. The current findings add to the knowledge base regarding the relationship between depressive symptoms and positive health practices in Black single mothers. Black single mothers who manifest high depressive symptoms need to be monitored in terms of their health practices, such as proper nutrition, exercise, and relaxation, and provided with appropriate counseling and resources.
The seventh hypothesis, proposing an indirect relationship between depressive cognitions and health practices through depressive symptoms, was weakly supported (B = −.08, p < .01). In the absence of a direct effect between depressive cognitions and positive health practices, this small indirect effect is of limited value in explaining the relationships among depressive cognitions, depressive symptoms, and positive health practices in this model.
Limitations
This study used a sample of convenience which is inherently biased. Data collection methods involved personal contact with subjects as well as contact with subjects via the U.S. mail. Although there were no mean differences in the main study variables nor the demographics between those who participated by mail and those who participated in person, these different data collection methods may have influenced the results in some other indeterminate way.
Conclusion
This study estimated paths in a just-identified model constructed from theoretical propositions and previous empirical findings in the literature to provide a better understanding of outcomes of depressive cognitions in Black single mothers, which heretofore had not been examined. Consistent with theory, depressive symptoms and diminished perceived social support are outcomes of depressive cognitions; diminished perceived social support is also an outcome of depressive symptoms. Contrary to theory, decreased participation in positive health practices is not an outcome of depressive cognitions; however, consistent with theory, less participation in positive health practices is an outcome of depressive symptoms. Based on the findings in this study, future research should examine the actual and self-reported health status of Black single mothers who present with significant depressive symptoms. Preventive interventions that target negative thinking will decrease depressive symptoms and enhance the perception of social support in Black single mothers. Research needs to continue on the negative psychosocial and physical consequences of depression in Black single women who are a vulnerable population.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biography
Rahshida L. Atkins, PhD, APN-C, is currently a postdoctoral fellow at the University of Pennsylvania (UPenn) School of Nursing where she is receiving advanced research training to address the health needs of vulnerable families. She received a PhD in nursing from Rutgers, the State University of New Jersey College of Nursing in 2013, where she served as an assistant professor for 1 year prior to coming to UPenn. Her program of research focuses on reducing mental and physical health disparities for vulnerable minority women. She is dedicated to nursing scholarship as she has published her research in premier nursing journals and has presented it nationally raising awareness about the factors influencing the health of vulnerable minority women. In recognition of her dedication to nursing education, scholarship, and research, she has earned numerous awards, including the Veronica Clark-Tasker EOF Alumni Research Award, the Sigma Theta Tau Alpha Tau Chapter Excellence in Research Award, the Robert Wood Johnson Foundation Faculty Preparation Award, and the Sigma Theta Tau International Rising Star Recognition.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;2:358–372. [Google Scholar]
- Alloy LB, Abramson LY, Walshaw PD, Neeren AM. Cognitive vulnerability to unipolar and bipolar mood disorders. Journal of Social and Clinical Psychology. 2006;25:726–754. [Google Scholar]
- Atkins R. Self-efficacy and the promotion of health for depressed single mothers. Mental Health in Family Medicine. 2010;7:155–168. [PMC free article] [PubMed] [Google Scholar]
- Atkins R. Depression in Black single mothers: A test of a theoretical model. Western Journal of Nursing Research. 2015;37:812–830. doi: 10.1177/0193945914528289. [DOI] [PubMed] [Google Scholar]
- Bai Y, Chiou C, Chang Y, Lam H. Correlates of depression in type 2 diabetic elderly patients: A correlational study. International Journal of Nursing Studies. 2008;45:571–579. doi: 10.1016/j.ijnurstu.2006.07.026. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113:229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York, NY: Harper & Row; 1967. [Google Scholar]
- Beck AT. The development of depression: A cognitive model. In: Friedman RE, Katz MM, editors. The psychology of depression: Contemporary theory and research. Washington, DC: Winston-Wiley; 1974. pp. 3–27. [Google Scholar]
- Billingsley ML, Billingsley TH. Depression, the way out: The Benessere Center’s guide to emotional well-being. Shawnee Mission, KS: The Benessere Center; 1987. [Google Scholar]
- Boardman JD, Alexander KB. Stress trajectories, health behaviors, and the mental health of black and white young adults. Social Science & Medicine. 2011;72:1659–1666. doi: 10.1016/j.socscimed.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CR, Zayas LH, McKee DM. Mother-infant interaction, life events and prenatal and postpartum depressive symptoms among urban minority women in primary care. Maternal and Child Health Journal. 2006;10:139–147. doi: 10.1007/s10995-005-0042-2. [DOI] [PubMed] [Google Scholar]
- Brown N, Muhlenkamp A, Fox L, Osborne M. The relationship among health beliefs, health values, and health promotion activity. Western Journal of Nursing Research. 1983;5:155–163. doi: 10.1177/019394598300500205. [DOI] [PubMed] [Google Scholar]
- Caracciolo B, Giaquinto S. Criterion validity of the Center for Epidemiological Studies Depression (CES-D) scale in a sample of rehabilitation inpatients. Journal of Rehabilitation Medicine. 2002;34:221–225. doi: 10.1080/165019702760279215. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Coiro MJ. Depressive symptoms among women receiving welfare. Women & Health. 2001;32:1–23. doi: 10.1300/J013v32n01_01. [DOI] [PubMed] [Google Scholar]
- Esperat C, Feng D, Zhang Y, Owen D. Health behaviors of low-income pregnant minority women. Western Journal of Nursing Research. 2007;29:284–300. doi: 10.1177/0193945906295532. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Hauck WW, Dennis MP, Schulz R. Depressive symptoms in older African-American and White adults with functional difficulties: The role of control strategies. Journal of the American Geriatric Society. 2007;55:1023–1030. doi: 10.1111/j.1532-5415.2007.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giurgescu C, Misra DP, Sealy-Jefferson S, Caldwell CH, Templin TN, Slaughter-Acey JC, Osyp TL. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. Social Science & Medicine. 2015;130:172–180. doi: 10.1016/j.socscimed.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjesfield CD, Greeno CG, Kim KH, Anderson CM. Economic stress, social support, and maternal depression: Is social support deterioration occurring? Social Work Research. 2010;34:135–143. [Google Scholar]
- Gruenberg DA, Wright RJ, Visness CM, Jaffee KF, Bloomberg GR, Cruikshank WW, … Kattan M. Relation between stress and cytokine responses in inner-city mothers. Annals of Allergy, Asthma & Immunology. 2015;115:439–445. doi: 10.1016/j.anai.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen CL. Closing comments and future directions. In: Gotlieb IH, Hammen CL, editors. Handbook of depression. New York, NY: Guilford Press; 2009. pp. 673–679. [Google Scholar]
- Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Journal of Psychosomatic Research. 1999;46:437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Hatcher J, Rayens MK, Peden AR, Hall LA. Predictors of depression for low-income African American single mothers. Journal of Health Disparities Research and Practice. 2008;2:89–110. [Google Scholar]
- Im EO, Ham OK, Chee E, Chee W. Physical activity and depressive symptoms in four ethnic groups of midlife women. Western Journal of Nursing Research. 2015;37:746–766. doi: 10.1177/0193945914537123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson AP, Bentler PM, Franke TM. Low-wage maternal employment and parenting style. Social Work. 2008;53:267–278. doi: 10.1093/sw/53.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joreskog K, Sorbom D. LISREL 8: Structural equation modeling with the SIMPLIS Command Language. Hillsdale, NJ: Lawrence Erlbaum; 1993. [Google Scholar]
- Klein DF, Wender PH. Understanding depression. 2. New York, NY: Oxford University Press; 2005. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford Press; 2005. [Google Scholar]
- Kneipp SM, Welch DP, Wood CE, Yucha CB, Yarandi H. Psychosocial and physiological stress among women leaving welfare. Western Journal of Nursing Research. 2007;29:864–883. doi: 10.1177/0193945906297378. [DOI] [PubMed] [Google Scholar]
- Kuster PA, Badr LK, Chang BL, Wuerker AK, Benjamin AE. Factors influencing health promoting activities of mothers caring for ventilator-assisted children. Journal of Pediatric Nursing. 2004;19:276–287. doi: 10.1016/j.pedn.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Lam CL, Chin WY, Lee PW, Lo YY, Fong DY, Lam TP. Unrecognized psychological problems impair quality of life and increase consultation rates in Chinese elderly patients. International Journal of Geriatric Psychiatry. 2009;24:979–989. doi: 10.1002/gps.2210. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Solomon A, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109:345–351. [PubMed] [Google Scholar]
- Lindgren K. Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Research in Nursing & Health. 2001;24:203–217. doi: 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- Lindgren K. A comparison of pregnancy health practices of women in inner-city and small urban communities. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2003;32:313–321. doi: 10.1177/0884217503253442. [DOI] [PubMed] [Google Scholar]
- Mahon NE, Yarcheski A, Yarcheski TJ. Psychometric evaluation of the Personal Lifestyle Questionnaire for adolescents. Research in Nursing & Health. 2002;25:68–75. doi: 10.1002/nur.10017. [DOI] [PubMed] [Google Scholar]
- Mahon NE, Yarcheski A, Yarcheski TJ, Hanks MM. Mediational models of health practices in early adolescents. Clinical Nursing Research. 2007;16:302–316. doi: 10.1177/1054773807307314. [DOI] [PubMed] [Google Scholar]
- Manuel JI, Martinson ML, Bledsoe-Mansori SE, Bellamy JL. The influence of stress and social support on depressive symptoms in mothers with young children. Social Science & Medicine. 2012;75:2013–2020. doi: 10.1016/j.socscimed.2012.07.034. [DOI] [PubMed] [Google Scholar]
- Mason-Hawkes J, Holm K. Causal modeling: A comparison of path analysis and LISREL. Nursing Research. 1989;38:312–314. [PubMed] [Google Scholar]
- McLennan JD, Kotelchuck M. Parental prevention practices for young children in the context of maternal depression. Pediatrics. 2000;105:1090–1095. doi: 10.1542/peds.105.5.1090. [DOI] [PubMed] [Google Scholar]
- McNicholas LS. Social support and positive health practices. Western Journal of Nursing Research. 2002;24:772–787. doi: 10.1177/019394502237387. [DOI] [PubMed] [Google Scholar]
- Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, Swartz K. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115:306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- Muhlenkamp AF, Brown NJ. The development of an instrument to measure health practices. Paper presented at the American Nurses’ Association Council of Nurse Researchers Conference; Minneapolis, MN. 1983. Jun, [Google Scholar]
- National Institutes of Mental Health. The numbers count: Mental disorders in America. 2009 Retrieved from http://www.lb7.uscourts.gov/documents/12-cv-1072url2.pdf.
- National Institutes of Mental Health. Transforming the understanding and treatment of mental illness. 2014 Retrieved from www.nimh.nih.gov/health/topics/depression/index.shtml.
- Odom EC, Vernon-Feagans L. Buffers of racial discrimination: Links with depression among rural African American mothers. Journal of Marriage and Family. 2010;72:346–359. doi: 10.1111/j.1741-3737.2010.00704.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peden AR, Rayens MK, Hall LA, Beebe LH. Preventing depression in high-risk college women: A report of an 18-month follow-up. Journal of American College Health. 2001;49:299–306. doi: 10.1080/07448480109596316. [DOI] [PubMed] [Google Scholar]
- Peden AR, Rayens MK, Hall LA, Grant E. Negative thinking and the mental health of low-income single mothers. Journal of Nursing Scholarship. 2004;36:337–344. doi: 10.1111/j.1547-5069.2004.04061.x. [DOI] [PubMed] [Google Scholar]
- Peden AR, Rayens MK, Hall LA, Grant E. Testing an intervention to reduce negative thinking, depressive symptoms, and chronic stressors in low-income single mothers. Journal of Nursing Scholarship. 2005;37:268–274. doi: 10.1111/j.1547-5069.2005.00046.x. [DOI] [PubMed] [Google Scholar]
- Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. Upper Saddle River, NJ: Prentice Hall; 2005. [Google Scholar]
- Pettit J, Joiner TE. Chronic depression: Interpersonal sources, therapeutic solutions interpersonal conflict avoidance. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Radloff SL. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. Retrieved from http://proxy.library.upenn.edu:2192/books/11291/006.pdf. [Google Scholar]
- Robbins PR. Understanding depression. Jefferson, NC: McFarland; 1993. [Google Scholar]
- Schroevers MJ, Sanderman RA, van Sonderen E, Ranchor AV. The evaluation of the Center for Epidemiologic Studies Depression (CES-D) scale: Depressed and positive affect in cancer patients and healthy reference subjects. Quality of Life Research. 2000;9:1015–1029. doi: 10.1023/a:1016673003237. [DOI] [PubMed] [Google Scholar]
- Siahpush M. Why is lone-motherhood so strongly associated with smoking? Australian New Zealand Journal of Public Health. 2004;28:37–42. doi: 10.1111/j.1467-842x.2004.tb00630.x. [DOI] [PubMed] [Google Scholar]
- Siefert K, Williams DR, Finlayson TL, Delva J, Ismail AI. Modifiable risk and protective factors for depressive symptoms in low-income African American mothers. American Journal of Orthopsychiatry. 2007;1:113–123. doi: 10.1037/0002-9432.77.1.113. [DOI] [PubMed] [Google Scholar]
- Strine TW, Mokdad AH, Shanta RD, Balluz LS, Berry JT, Gonzalez O. Impact of depression and anxiety on quality of life, healthy behaviors, and asthma control among adults in the United States with asthma. Journal of Asthma. 2008;45:123–133. doi: 10.1080/02770900701840238. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Boston, MA: Pearson; 2013. [Google Scholar]
- Walsh JL, Senn TE, Carey MP. Longitudinal associations between health behaviors and mental health in low-income adults. Translational Behavioral Medicine. 2013;3:104–113. doi: 10.1007/s13142-012-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinert C. A social support measure. Nursing Research. 1987;36:273–277. [PubMed] [Google Scholar]
- Weiss R. The provision of social relationships. In: Zick R, editor. Doing unto others. Englewood Cliffs, NJ: Prentice Hall; 1974. pp. 17–26. [Google Scholar]
- Wilcox H, Field T, Prodromidis M, Scafidi F. Correlations between the BDI and CES-D in a sample of adolescent mothers. Adolescence. 1998;33:565–574. [PubMed] [Google Scholar]
- Willoughby DF, Kee C, Demi A. Women’s psychosocial adjustment to diabetes. Journal of Advanced Nursing. 2000;32:1422–1430. doi: 10.1046/j.1365-2648.2000.01620.x. [DOI] [PubMed] [Google Scholar]
- Zauszniewski JA. Development and testing of a measure of depressive cognition in older adults. Journal of Nursing Measurement. 1995;3:31–41. [PubMed] [Google Scholar]
- Zauszniewski JA. The Depressive Cognition Scale: Further psychometric evaluation. Journal of Nursing Measurement. 1997;5:191–200. [PubMed] [Google Scholar]
- Zauszniewski JA, Bekhet AK. Screening measure for early detection of depressive symptoms: The Depressive Cognition Scale. Western Journal of Nursing Research. 2012;34:230–244. doi: 10.1177/0193945910396731. [DOI] [PubMed] [Google Scholar]
- Zauszniewski JA, Chung C, Krafcik K, Sousa VD. Psychometric testing of the Depressive Cognition Scale in women with type 2 diabetes. Journal of Nursing Measurement. 2001;9:61–72. [PubMed] [Google Scholar]
- Zauszniewski JA, Picot SJF, Debanne SM, Roberts BL, Wykle ML. Psychometric characteristics of the Depressive Cognition Scale in African American women. Journal of Nursing Measurement. 2002;10:83–95. doi: 10.1891/jnum.10.2.83.52557. [DOI] [PubMed] [Google Scholar]