Abstract
Cross-sectional studies have shown an association between better patient experiences and health outcomes. However, the direction of causality remains unclear. Our prospective study seeks to determine whether better initial patient experiences predict subsequent retention in HIV care. We enrolled patients new to an HIV clinic in Houston, Texas, from August 26, 2013 to November 18, 2013. The patients’ overall experience with the HIV provider was based on six items; overall experience with the HIV clinic was based on five items. We measured subsequent retention over the first 6 months and entire first year of HIV care. Analyses included 140 patients. Sixty-one percent were non-Hispanic black, 41 % were diagnosed with HIV within the last 3 months, and 36 % had a CD4 cell count <200. Thirty three percent were totally satisfied with their initial HIV provider experience and 32 % were totally satisfied with their initial HIV clinic experience. Retention was 68 % over the first 6 months and 51 % over the first year. Satisfaction with the HIV provider at the initial visit significantly predicted 6-month retention in care (aOR = 3.56, p = 0.006). Similar results were found for satisfaction with the HIV clinic (aOR = 4.67, p = 0.002). Neither of the patient experience measures at the initial visit predicted 12-month retention. Patients with better initial care experiences have significantly greater retention in HIV care. The effect of better initial care experiences was limited in duration. Consistently improving patient care experiences, not only at baseline but also on subsequent visits, may be a way to increase retention in HIV care.
Keywords: Patient satisfaction, Patient experience, HIV infection, Retention in care, Prospective studies
Background
Even though potent HIV medicines exist, many patients do not get regular HIV care. Poor retention in HIV care predicts worse health outcomes. The National HIV/AIDS Strategy aims to increase the percentage of HIV diagnosed persons who are retained in HIV care from 50.9 % in 2010 to 90 % by 2020 [1]. However, retention in HIV care is a relatively young field and few evidence-based interventions exist to guide improvements [2]. To date, interventions to improve retention in HIV care have generally focused on difficult-to-modify factors, such as intensive case management to address unmet needs and behavioral skills building to change patient-related factors [3]. These interventions are resource intensive and dissemination has been limited. These data underscore the need to identify drivers of retention in HIV care that are modifiable, feasible, and low cost.
The Institute of Medicine cites patient-centered care as one of six quality aims [4]. Patient experience, an integral component of patient-centered care, is an innovative approach to enhancing value in health care delivery and improving retention in HIV care. In our previous study of 489 HIV primary care patients, we found that better patient experiences positively correlated with retention in HIV care and adherence to HAART [5]. Better patient experiences have also been associated with less switching behavior with providers and insurance plans [6–8].
Although promising, these data are cross-sectional and subject to a number of biases, including non-response and sampling biases and inconclusive causal inference. Do better patient experiences result in greater retention in HIV care? Or do patients retained in HIV care feel better and thus rate their experiences highly? Moreover, do patients with negative experiences drop out of care and become unavailable for study? To move the field forward, prospective studies are needed. Health care organizations have the power to monitor and influence patient experiences. If prospective studies show that patients with better care experiences have greater retention in HIV care, health care organizations could potentially retain more HIV patients in care by improving the care experience. Such efforts may be impactful independent of patient-related factors.
To address this question, we enrolled patients new to an HIV clinic over the first year. We were specifically interested in new patients, because they allow the study of patient experience from all patients entering HIV care at the clinic, before patients have the opportunity to miss subsequent visits, and thus eliminating survivor bias. New patients also may be most impressionable [9]. They have not yet formed strong impressions of the provider or clinic nor have they established strong behavioral patterns of retention. Thus, the quality of initial care experiences may have a greater effect on outcomes like retention in care.
We conducted a prospective cohort study of patients entering care for HIV at a single clinic in a major metropolitan area. We hypothesized that patients with better initial care experiences will have greater retention in HIV care in the first 6 months and entire year of care.
Methods
Study Population
We enrolled patients establishing HIV primary care at Thomas Street Health Center in Houston, Texas, between August 26 and November 18, 2013. Eligible patients were 18 years or older and HIV infected, and had never completed an HIV provider appointment at Thomas Street Health Center. Although new to the HIV clinic, patients were not necessarily newly diagnosed or naïve to antiretroviral therapy. Exclusion criteria consisted of: (1) mental or physical inability to give consent or complete a survey, (2) inability to complete the survey in English or Spanish, or (3) active incarceration.
Data Collection
We recruited consecutive eligible patients on the day they attended their first HIV provider visit. Research staff administered a baseline patient experience survey immediately after the first HIV provider visit to assess patient experience and measure potential confounders and covariates. In a prior study of patients at this clinic, 28 % had inadequate health literacy [10]. Thus, we offered to read the survey questions to most patients, especially if they appeared hesitant or uncomfortable. Mode of survey administration was coded as interviewer-administered if staff helped the patient complete the survey by reading the questions; it was coded as self-administered if the patient did not require such assistance. Survey data were double-entered into a database, compared and discrepancies reconciled.
Description of Clinic
Patients new to Thomas Street Health Center complete an intake visit. At this visit, a nurse takes a brief history and orders initial labs and a chest X-ray, which are generally obtained that same day. The nurse then typically schedules the first HIV provider visit to occur within 2 weeks. While patients may also be scheduled appointments with the case manager, social worker, and other staff, those appointments are not necessary to receive an appointment with an HIV provider or for the provider to prescribe HIV medicines. HIV providers are defined as clinicians who can prescribe HIV medicines. In all cases, providers were physicians. Subsequent provider visits are typically with the same provider. All patients in this study had to have completed an intake visit and the first HIV provider visit. Retention in care is based on completed provider visits subsequent to the first HIV provider visit (Table 1).
Table 1.
Baseline characteristics of participants at Thomas Street Health Center in Houston, Texas (N = 140)
| Characteristics | |
|---|---|
| Age, years [mean (±SD)] | 39 (±12) |
| Gender [n (%)] | |
| Male | 95 (68 %) |
| Female | 43 (31 %) |
| Transgender | 2 (1 %) |
| Race ethnicity [n (%)] | |
| Non-Hispanic black | 86 (61 %) |
| Hispanic | 32 (23 %) |
| Non-Hispanic white | 19 (14 %) |
| Other | 3 (2 %) |
| Survey administered [n (%)] | |
| In Spanish | 17 (12 %) |
| By in-person interviewera | 44 (32 %) |
| Education [n (%)] | |
| Some high school or less | 43 (31 %) |
| High school graduate or equivalent | 39 (28 %) |
| Some college or higher | 58 (41 %) |
| Income, per year [n (%)]b | |
| ≤$10 K | 82 (62 %) |
| >$10 and ≤30 K | 39 (30 %) |
| >$30 K | 11 (8 %) |
| Alcohol screen, positive (%) | 67 (48 %) |
| Drug use in past 30 days (%) | 27 (19 %) |
| HIV risk factor (%) | |
| IVDA | 11 (8 %) |
| MSM, no IVDA | 51 (36 %) |
| Heterosexual sex, no IVDA | 75 (54 %) |
| Other | 3 (2 %) |
| Time from HIV diagnosis (%) | |
| ≤3 months | 57 (41 %) |
| 3 months–1 year | 9 (6 %) |
| 1–5 years | 26 (19 %) |
| 5–10 years | 13 (9 %) |
| >10 years | 35 (25 %) |
| Naïve to HIV care | 66 (47 %) |
| CD4 cell count <200 | 50 (36 %) |
| HIV RNA <20 copies (%)a | 27 (19 %) |
Data on mode of survey administration were missing for two participants
Data on income were missing for eight participants
Measures
Retention in HIV Care
We measured retention in care over 6- and 12-month time periods. Retention was operationalized as a dichotomous variable (retained or not retained). For the 6-month time period, retained was defined as having completed at least one HIV provider visit between 1 and 180 days after the first provider visit. For the 12-month time period, retention was defined as having completed at least one HIV provider visit between 1 and 180 days after the first provider visit and at least one additional visit at 181–365 days.
Overall Experience with the HIV Provider and Clinic
Similar to the widely used Consumer Assessment of Healthcare Providers and Systems (CAHPS®) survey, patient experience with the HIV provider and the clinic were measured with separate multi-item constructs (see Table 2) [11]. Experience with the HIV provider was measured by a battery of six items rated by patients (Cronbach’s alpha = 0.868), while experience with the HIV clinic was measured by a battery of five items (Cronbach’s alpha = 0.844). Item responses were transformed to a 0–100 scale and averaged to create a composite index of patients’ overall experience with the HIV provider and the clinic.
Table 2.
Patient experience items and response distributions at baseline (by percent)
| Items | Scale | Response values |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| % below | ||||||||||||
| Overall evaluation of the HIV provider | ||||||||||||
| 1. Overall, how satisfied or dissatisfied are you with your HIV provider? | 1–7a | 1 | 1 | 1 | 4 | 4 | 25 | 64 | ||||
| 2. All things considered, how much do you trust your HIV provider? | 1–10b | 0 | 0 | 1 | 1 | 1 | 1 | 7 | 16 | 12 | 61 | |
| 3. Overall, how do you feel about your HIV provider? | 1–7c | 1 | 2 | 0 | 6 | 14 | 31 | 46 | ||||
| 4. Would you recommend your HIV provider to other patients with HIV? | 1–5d | 1 | 1 | 5 | 23 | 69 | ||||||
| 5. If you could stay with the same HIV provider or switch to another HIV provider at this clinic, would you stay or switch? |
1–5e | 1 | 2 | 11 | 21 | 64 | ||||||
| 6. Using any number from 0 to 10, where 0 is the worst HIV provider possible and 10 is the best HIV provider possible, what number would you use to rate this provider? |
0–10 | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 9 | 13 | 16 | 59 |
| Overall evaluation of the HIV clinic | ||||||||||||
| 7. Overall, how satisfied or dissatisfied are you with the care you got at this clinic? | 1–7a | 0 | 0 | 0 | 2 | 9 | 25 | 64 | ||||
| 8. Overall, how do you feel about the care you got at this clinic? | 1–7c | 0 | 0 | 1 | 4 | 17 | 33 | 45 | ||||
| 9. Would you recommend this clinic to other patients with HIV? | 1–5d | 1 | 1 | 3 | 24 | 71 | ||||||
| 10. If you could stay or switch to another HIV clinic in this area at the same cost, would you stay or switch? |
1–5e | 0 | 3 | 11 | 21 | 65 | ||||||
| 11. Using any number from 0 to 10, where 0 is the worst clinic possible and 10 is the best clinic possible, what number would you use to rate this clinic? |
0–10 | 0 | 0 | 0 | 0 | 1 | 1 | 3 | 6 | 15 | 20 | 54 |
1 = Completely dissatisfied, 2 = mostly dissatisfied; 3 = somewhat dissatisfied, 4 = mixed feelings, 5 = somewhat satisfied, 6 = mostly satisfied, 7 = completely satisfied
1 = I do not trust my HIV provider → 10 = I trust my HIV provider completely
1 = Terrible, 2 = unhappy, 3 = mostly dissatisfied, 4 = mixed, 5 = mostly satisfied, 6 = pleased, 7 = wonderful
1 = Definitely no, 2 = probably no, 3 = not sure, 4 = probably yes, 5 = definitely yes
1 = Definitely switch, 2 = probably switch, 3 = not sure, 4 = probably stay, 5 = definitely stay
The patient experience items shown in Table 2 were adapted from validated survey items. Items 3 and 8 were based on the Delightful–Terrible Scale, which has high validity across a wide spectrum of life experiences [12]. Items 1, 2 and 7 were adapted from the Primary Care Assessment Survey [13]. Items 4, 6, 9 and 11 were adapted from the CAHPS® survey [11]. Item 5 and 10 were developed for and validated in our prior study [14].
For purposes of this analysis, the patient experience scores for the HIV provider and clinic were classified into two categories: (1) totally satisfied [score of 100, i.e. selecting the most positive rating scale response (top box score) for all items in the multi-item construct], and (2) less than totally satisfied. This classification was chosen based on findings in the marketing literature that customer loyalty requires very high levels of customer satisfaction, since even “merely satisfied” customers are more likely to switch products or services given a choice [15].
Other Measures
To describe the patient population and control for potential confounding factors, we collected survey data on gender, race, ethnicity, education, income, insurance, HIV risk factors, time from HIV diagnosis, antiretroviral use, naivety to HIV care, health status (physical and mental) [16], and co-morbid conditions. We reviewed the electronic medical record to obtain data on age, CD4 cell count and HIV RNA, and to corroborate self-reported antiretroviral use.
Validated scales were used to assess contextual factors highly prevalent among patients with HIV and which have been associated with lower retention in care, including homelessness [17, 18], depression [19], alcohol use [20], drug use (excluding marijuana) [21], and tangible social support [22].
We adapted and validated a 5-item retention-specific Self-efficacy Scale to assess patients’ confidence in carrying out behaviors related to HIV appointment adherence. Patients were asked, “How confident are you that you can: (1) Keep all your HIV appointments even when getting to the clinic is a major hassle; (2) Call and make an appointment to see the HIV doctor; (3) Arrange other things in your life to get to your HIV appointment; (4) Arrange transportation to get to the HIV clinic; and (5) Continue with your treatment even when your feel discouraged about your health. Responses ranged from 0 (not at all confident) to 3 (very confident). Items 1 and 5 were adapted from the HIV Treatment Adherence Self-efficacy Scale [23]. Items 2–4 were adapted from the Self-efficacy in Mammography Scale [24]. Responses were averaged to create a composite measure of retention-specific self-efficacy (Cronbach’s alpha = 0.858).
Finally, we adapted a validated a 3-item health-specific social support scale, based on items from the Medication-Specific Social Support Scale [25]. Patients were asked, “Please indicate how often people may have helped you in the various ways described during the past 3 months: (1) Reminded you to keep your clinic appointments; (2) Reminded you to take your medicines; (3) Called you specifically to ask how you were doing with your health.” Responses ranged from 0 (never) to 4 (very often). The scale’s Cronbach’s alpha was 0.851.
Statistical Analysis
We examined the reliability of our multi-item scales. We computed Pearson correlations between the constituent items in each scale. The internal consistency reliability of the scales was assessed with Cronbach’s Coefficient Alpha. All scales achieved satisfactory reliability (>0.70).
To evaluate the differences in patient characteristics between those who were and were not retained in HIV care, χ2 and paired t-tests were calculated. We also estimated logistic regression models of retention in HIV care, using initial patient experiences with both providers and clinics as the predictor variables. The patient experience variables were dichotomized based on whether a top box score was given by the patient. Patient characteristics were included in the regression model as controls of potential confounders if their bivariate correlations for both the retention measures reached a significance level of p < 0.10.
Statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC) and SPSS version 22 (IBM Corp, Armonk, NY). The Institutional Review Board for Baylor College of Medicine and Affiliated Hospitals approved this study. Participants gave written informed consent.
Results
Study Population
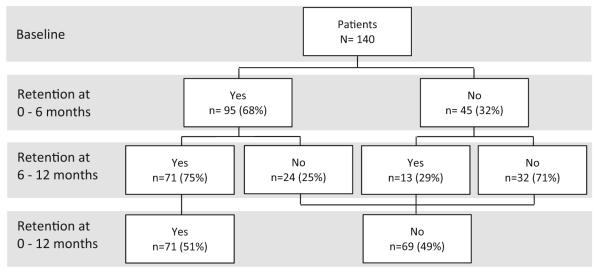
A total of 146 new patients enrolled in the study (Fig. 1). Participants who enrolled in the study were not significantly different from those who did not enroll, in terms of age, race, ethnicity, and sex (data not shown). The participation rate among eligible patients was 84 % (146/173). Six patients completed the baseline experience survey but were excluded from analyses (see Fig. 1 footnote).
Fig. 1.
Flow diagram. aThree patients subsequently moved out of town, one patient was incarcerated during the follow-up period, one patient was referred to Thomas Street Health Center for oncology care only and continued to receive HIV primary care elsewhere, and one patient transferred HIV care to Thomas Street Health Center but was not new to the HIV provider (provider also sees patients at another facility)
Baseline patient characteristics are shown in Table 1. The majority of the enrolled patients were non-Hispanic black (61 %) and the predominant HIV risk factor was unprotected heterosexual intercourse (54 %). A total of 41 % were diagnosed with HIV within the last 3 months, 36 % had a CD4 cell count <200 and almost half (47 %) were naïve to HIV care, defined as never having seen an HIV provider at any other clinic. Twenty-five percent were diagnosed with HIV for >10 years and 19 % had an undetectable HIV viral load (<20 copies) at entry to the clinic.
Item Nonresponse
For the patient experience survey, 59 % of participants had no missing items, and 99 % had a missing item rate of <5 %. Rates of nonresponse for individual items were low, ranging from 0 to 6 %.
Overall Experience with the HIV Provider and Clinic
Patients were highly satisfied with their experiences with both providers and the clinic; response distributions of each item rated are shown in Table 2. A total of 33 % were totally satisfied with their initial HIV provider experience, selecting the most positive response (i.e. top box score) for all six HIV provider items. The provider experience index, calculated by averaging these six items, yielded a median score was 94.4 out of a maximum possible score of 100. Results for the HIV clinic are similar; 32 % were totally satisfied with their initial HIV clinic experience, selecting the most positive response for all five HIV clinic items. The clinic experience index created by averaging these five items yielded a median score of 93.3.
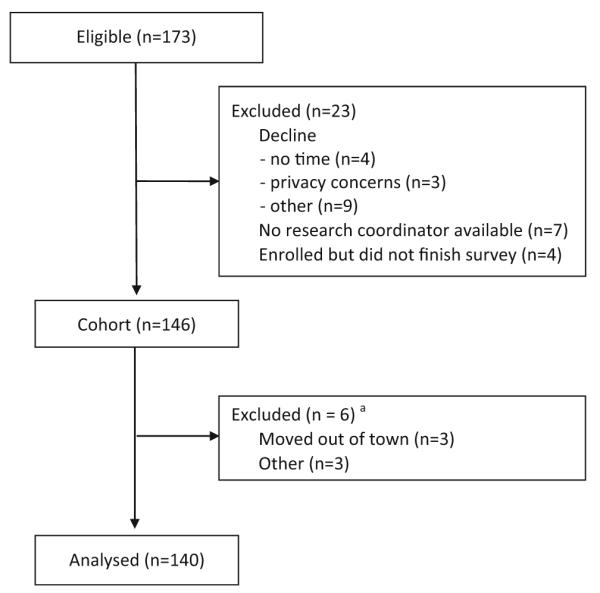
Retention in HIV Care
As shown in Fig. 2, 68 % of patients (95 out of 140) returned for at least one visit within the first 6 months. For the 12-month time period, 51 % of patients (71 out of 140) had returned for at least one visit in the first 6 months and at least one additional visit in the latter 6 months, and were thus considered retained in care over the entire first year of care. Among patients retained at 6 months, the average number of visits was two; among those retained at 12 months, the average was three visits.
Fig. 2.
Flow diagram—retention in care
Relationship Between Patient Characteristics and Retention in HIV Care
The associations between patient characteristics and retention in care are shown in Table 3. Significant associations with both 6- and 12-month retention were observed for (1) being naïve to HIV care at enrollment in study, (2) having a Spanish language preference for the survey, (3) in-person interviewer-administration rather than self-administration of the patient experience survey, and (4) baseline CD4 cell count <200. Time from HIV diagnosis correlated highly with being naïve to HIV care (r = −0.713, p < 0.001), and we chose the latter as a control variable.
Table 3.
Patient characteristics by retention in HIV care at 0–6 and 0–12 months
| Baseline characteristics | Retention at 0–6 months |
p | Retention at 0–12 months |
p | ||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||
| Age, years (mean) | 40 | 37 | 0.180 | 41 | 37 | 0.038 |
| Gender (%) | ||||||
| Male | 65 | 35 | 0.268 | 47 | 53 | 0.242 |
| Female | 74 | 26 | 58 | 42 | ||
| Race/ethnicity (%) | ||||||
| Non-Hispanic Black | 69 | 31 | 0.893 | 49 | 51 | 0.766 |
| Hispanic | 69 | 31 | 56 | 44 | ||
| Non-Hispanic White | 63 | 37 | 53 | 47 | ||
| Survey administered in Spanish (%) | ||||||
| Yes | 88 | 12 | 0.093 | 76 | 24 | 0.036 |
| No | 65 | 35 | 47 | 53 | ||
| Survey admin by interviewer in-person (%) | ||||||
| Yes | 79 | 21 | 0.037 | 68 | 32 | 0.003 |
| No | 62 | 38 | 42 | 58 | ||
| Education (%) | ||||||
| Some high school or less | 77 | 23 | 0.299 | 60 | 40 | 0.073 |
| High school graduate or equivalent | 62 | 39 | 36 | 64 | ||
| Some college or higher | 66 | 35 | 53 | 47 | ||
| Income (%) | ||||||
| ≤ $10 K | 67 | 33 | 0.899 | 54 | 46 | 0.683 |
| > $10 K | 66 | 34 | 50 | 50 | ||
| Depression screen, positive (%) | ||||||
| Yes | 75 | 25 | 0.202 | 57 | 43 | 0.271 |
| No | 64 | 36 | 47 | 53 | ||
| Alcohol screen, positive (%) | ||||||
| Yes | 61 | 39 | 0.106 | 48 | 52 | 0.503 |
| No | 74 | 26 | 53 | 47 | ||
| Drug use in past 30 days (%) | ||||||
| Yes | 56 | 44 | 0.128 | 44 | 56 | 0.468 |
| No | 71 | 29 | 52 | 48 | ||
| HIV risk factor (%) | ||||||
| IVDA | 55 | 45 | 0.233 | 45 | 55 | 0.833 |
| MSM, no IVDA | 61 | 39 | 47 | 53 | ||
| Heterosexual sex, no IVDA | 75 | 25 | 53 | 47 | ||
| Time from HIV dx, years (%) | ||||||
| ≤3 months | 81 | 19 | 0.025 | 67 | 33 | 0.007 |
| 3 months–5 year | 57 | 43 | 37 | 63 | ||
| >5 years | 60 | 40 | 42 | 58 | ||
| Naïve to HIV care (%) | ||||||
| Yes | 80 | 20 | 0.003 | 68 | 32 | <0.001 |
| No | 57 | 43 | 35 | 65 | ||
| CD4 cell count (%) | ||||||
| <200 | 84 | 16 | 0.002 | 68 | 32 | 0.002 |
| >200 | 59 | 41 | 41 | 59 | ||
| HIV RNA copies <20 copies (%) | ||||||
| Yes | 56 | 44 | 0.128 | 37 | 63 | 0.114 |
| No | 71 | 29 | 54 | 46 | ||
| Physical health | 44 | 47 | 0.255 | 44 | 46 | 0.162 |
| Mental health | 44 | 45 | 0.664 | 43 | 45 | 0.516 |
| Tangle social support | 55 | 62 | 0.289 | 56 | 59 | 0.693 |
| Health-specific social support | 51 | 52 | 0.887 | 49 | 54 | 0.475 |
| Retention-specific self-efficacy | 87 | 88 | 0.921 | 87 | 88 | 0.827 |
| Co-morbid conditions | 1.2 | 1.2 | 0.964 | 1.3 | 1.0 | 0.163 |
Relationship Between Patient Experiences and Retention in HIV Care
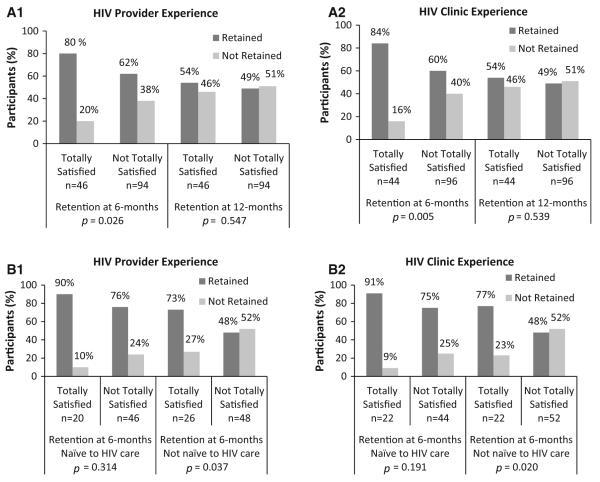
Bivariate analysis indicated that patient experiences were significantly associated with retention in care in the first 6 months (Fig. 3a). Patients who were totally satisfied with the HIV provider on the initial visit were significantly more likely to be retained at 6 months than those who were not totally satisfied (80 vs 62 %, p = 0.026). Similarly, patients totally satisfied with the HIV clinic were significantly more likely to have been retained at 6 months than those not totally satisfied (84 vs 60 %, p = 0.005). However, neither patient experience variable was significantly associated with retention in care at 12 months (54 vs 49 %, p = 0.547 for overall satisfaction with HIV provider; 54 vs 49 %, p = 0.539 for overall satisfaction with HIV clinic).
Fig. 3.
Initial HIV provider and clinic experiences and subsequent retention in HIV care for a total population, b patients either naïve or non-naïve to HIV care
Additional bivariate analyses were conducted to assess if the relationship between initial patient experience and subsequent retention in HIV care differs among those who are and are not naïve to HIV care (Fig. 3b). In the sub-population of patients not naïve HIV care, patients who were totally satisfied on the initial visit were significantly more likely to be retained at 6 months than those who were not totally satisfied (73 vs 48 %, p = 0.037 for overall satisfaction with HIV provider; 77 vs 48 %, p = 0.020 for overall satisfaction with HIV clinic). Bivariate analyses restricted to patients who are naïve to HIV care also indicated that patient experiences were associated with retention in HIV care at 6-months, although these associations did not reach statistical significance (90 vs 76 %, p = 0.314 for overall satisfaction with HIV provider; 91 vs 75 %, p = 0.191 for overall satisfaction with HIV clinic).
Logistic regression was conducted to assess whether patients’ experiences at the initial visit predicted their subsequent retention in care, while controlling for potential confounding variables. Table 4 shows the logistic regression models predicting retention for provider and clinic satisfaction. Results are shown with and without the inclusion of the four patient characteristics variables noted above as statistical controls of potential confounders. Satisfaction with HIV provider at the initial visit was a significant predictor of 6-month retention in care after controlling for the potential confounders (model 1: aOR = 3.56, p = 0.006). Similarly, satisfaction with the HIV clinic at the initial visit was a significant predictor of 6-month retention in care (model 2: aOR = 4.67, p = 0.002). For 12-month retention, neither of the patient experience measures at the initial visit predicts retention over a 12 month period (model 3: aOR = 1.59, p = 0.259 for provider satisfaction; model 4: aOR = 1.40, p = 0.413 for clinic satisfaction).
Table 4.
Bivariate and multivariate analyses—associations between initial patient experiences and retention in HIV care (N = 140)
| Bivariate |
Multivariatea |
|||||
|---|---|---|---|---|---|---|
| OR | 95 % CI | p | OR | 95 % CI | p | |
| Retention at 0–6 months | ||||||
| Model 1 | ||||||
| Index of HIV provider experience | 2.55 | 1.10–5.90 | 0.029 | 3.56 | 1.44–8.84 | 0.006 |
| Model 2 | ||||||
| Index of HIV clinic experience | 3.46 | 1.40–8.57 | 0.007 | 4.67 | 1.76–12.44 | 0.002 |
| Retention at 0–12 months | ||||||
| Model 3 | ||||||
| Index of HIV provider experience | 1.24 | 0.61–2.52 | 0.548 | 1.59 | 0.71–3.57 | 0.259 |
| Model 4 | ||||||
| Index of HIV clinic experience | 1.25 | 0.61–2.56 | 0.540 | 1.40 | 0.63–3.13 | 0.413 |
Patient experience was operationalized as a dichotomous variable and measured as the proportion of patients with an experience score of 100
OR odds ratio, CI confidence interval
Controlling for being naïve to HIV care on enrollment into study, Spanish language preference, interviewer mode of survey administration, and baseline CD4 cell count <200
Discussion
In our prospective cohort study of 140 patients new to an HIV clinic, patients with better initial care experiences had greater retention in HIV care. However, the effect of better initial care experiences was limited to the initial 6-month period of care at the clinic. These associations persisted even after controlling for potential confounders.
Our data support the contention that there is a short-term relationship between the quality of initial care experiences and the subsequent retention of patients in HIV care. However, the effects of patient experience appear to be limited in duration. The study does not provide evidence of a longer-term, i.e. 12-month effect, of initial patient experiences. It is possible that alternative drivers of retention intercede after the provider and clinic effects wear off, causing null findings. In other words, better experience at one time point may only carry one so far in increasing retention at a much later date. For example, patients’ motivation to keep appointments after an initial visit to a new provider and clinic (whether newly diagnosed or re-engaging in care) may diminish as other life priorities take precedence. We suspect it may also take better patient experiences at both the outset as well as in subsequent visits for longer term retention to also be high. Better patient experiences at baseline alone may have a beneficial short-term effect, but it may be the combination of repeated better patient experiences over the first year that is needed to have an effect on 12-month retention. Limited sample size and power must also be acknowledged in not finding longer-term effect of initial care experiences.
Better initial patient experiences were associated with retention in HIV care in the first 6-month period, regardless of whether a patient was naïve or not naïve to HIV care. Although the trends were similar for both populations, it only reached statistical significance in patients not naïve to HIV care. The lack of significance for those naïve to HIV care could have been due to lack of power (e.g. there were only two patients who were totally satisfied and not retained at 6 months, for both HIV provider and clinic experiences). Still, the data supports our hypothesis that patients’ initial experience with a new clinic, even among patients who have had prior experience with HIV care, whether good or bad, influences subsequent retention. We suspect that patients who have prior experience may be better able to judge the care they receive because they have a base of experience for assessing that care. Interventions targeting patient experience could potentially help both populations.
Our research and findings are promising. Based on these results, larger and more definitive studies are warranted. Future studies should include a multi-wave longitudinal assessment of patient experience to quantify how patient experiences change over time as care progresses, and identify the key factors behind any changes.
Potential interventions for improving the patient’s experience with the provider include those that incorporate audit feedback and/or feedback coupled with communication skills training. In a classic study by Cope et al., internal medicine residents receiving an audit feedback session with the program director had significantly improved patient experience scores than those who did not [26]. In a recent randomized controlled trial by Tulsky et al., oncologists completed a 1 h computer program that included training on communication skills and tailored feedback based on previously recorded conversations with patients [27]. Patients seen by oncologists in the intervention arm reported significantly greater trust in the provider than those seen by providers in the control arm. Randomized controlled intervention studies like these are needed to inform evidence-based strategies to improve patient experiences. Without evidence based interventions, there is the risk of misdirected interventions to improve patient experiences, e.g. administrative mandates to improve elements of care that do not significantly drive the patient care experience, such as renovating hospital cafeterias and providing free valet parking [14, 28, 29]. Intervention studies are also needed to see the extent to which improved patient experiences raise outcomes such as retention in HIV care.
This study has a number of important methodological strengths. To our knowledge, this is the first prospective cohort study in any disease process examining the temporal relationship between initial care experiences and subsequent health outcomes, and doing so by using the patient as the unit of analysis, as opposed to aggregate data at the care organization level. The study is notable for using psychometrically rigorous measures of patient experience. The study is also unique in including only patients who are new to an HIV clinic, reducing opportunities for selection bias. Lastly, our study includes a large number of Black and Hispanic patients, a population disproportionally affected by HIV yet underrepresented in many studies.
As in any investigation, this study has certain limitations. We conducted this study at a public HIV clinic, and the findings may not generalize to other settings. In addition, our sample size may have been too small to detect significant relationships between initial patient experience and retention in care over 12 months, even if a significant relationship were to exist.
Conclusions
Retention in HIV care is a critical challenge to maximizing the benefits of effective antiretroviral therapy. Our study suggests that better patient experiences may be an important modifiable health systems level factor in keeping patients in HIV care. The findings, if confirmed in a larger, definitive prospective study, suggest that patient experience may be a new tool in improving retention in HIV care. Such a tool would also align with the National HIV/AIDS Strategy’s goal to develop models of care that are patient-centered and take into account patients’ needs and preferences [1].
Acknowledgments
We thank Drs. Daniel M. Musher and Richard L. Street for their critical review of an earlier draft of this manuscript. This study was supported by a supplement to the National Institutes of Health—funded Baylor College of Medicine—University of Texas Houston Center for AIDS Research (Grant Number P30AI036211), supplemental funds to the District of Columbia Developmental Center for AIDS Research (Grant Number 5P30AI087714), the facilities and resources of the Houston VA Center for Innovations in Quality, Effectiveness and Safety (HFP90-020), and the facilities and resources of Harris Health System.
Footnotes
Disclaimer The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Compliance with Ethical Standards
Conflict of interest All authors report no conflict of interest.
References
- 1.White House Office of National AIDS Policy [Accessed 5 Jan 2016];National HIV/AIDS strategy for the United States: updated to 2020. https://www.aids.gov/federal-resources/national-hiv-aids-strategy/overview.
- 2.Centers for Disease Control and Prevention [Accessed 5 Jan 2016];Compendium of evidence-based interventions and best practices for HIV prevention. http://www.cdc.gov/hiv/prevention/research/compendium/lrc/index.html.
- 3.Giordano TP. Retention in HIV care: what the clinician needs to know. Top Antivir Med. 2011;19(1):12–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine (IOM) Crossing the quality chasm: a new health system for the 21st century. National Academy Press; Washington: 2001. [PubMed] [Google Scholar]
- 5.Dang BN, Westbrook RA, Black WC, Rodriguez-Barradas MC, Giordano TP. Examining the link between patient satisfaction and adherence to HIV care: a structural equation model. PLoS One. 2013;8(1):e54729. doi: 10.1371/journal.pone.0054729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marquis MS. Patient satisfaction and change in medical care provider: a longitudinal study. Med Care. 1983;21(8):821–9. doi: 10.1097/00005650-198308000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Ware JE, Jr, Davies AR. Behavioral consequences of consumer dissatisfaction with medical care. Eval Program Plan. 1983;6(3–4):291–7. doi: 10.1016/0149-7189(83)90009-5. [DOI] [PubMed] [Google Scholar]
- 8.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician’s practice. J Fam Pract. 2001;50(2):130–6. [PubMed] [Google Scholar]
- 9.Gardner LI, Marks G, Craw JA, et al. A low-effort, clinic-wide intervention improves attendance for HIV primary care. Clin Infect Dis. 2012;55(8):1124–34. doi: 10.1093/cid/cis623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayben JK, Kramer JR, Kallen MA, Franzini L, Lairson DR, Giordano TP. Predictors of delayed HIV diagnosis in a recently diagnosed cohort. AIDS Patient Care STDS. 2007;21(3):195–204. doi: 10.1089/apc.2006.0097. [DOI] [PubMed] [Google Scholar]
- 11.Consumer Assessment of Healthcare Providers and Systems (CAHPS) CAHPS clinician & group visit survey. Agency for Healthcare Research and Quality; Rockville: 2011. [Google Scholar]
- 12.Andrews F, Crandall R. The validity of measures of self-reported wellbeing. Soc Indic Res. 1978;3:1–19. [Google Scholar]
- 13.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Dang BN, Westbrook RA, Rodriguez-Barradas MC, Giordano TP. Identifying drivers of overall satisfaction in patients receiving HIV primary care: a cross-sectional study. PLoS One. 2012;7(8):e42980. doi: 10.1371/journal.pone.0042980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones TO, Sasser EWJ. Why satisfied customers defect. Harvard business review. J Manag Eng. 1995;12:11. [Google Scholar]
- 16.Ware J, Kosinki M, Dewey J, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-TM health survey. Quality Metric Incorporated; Lincoln: 2001. [Google Scholar]
- 17.Link B, Phelan J, Bresnahan M, Stueve A, Moore R, Susser E. Lifetime and five-year prevalence of homelessness in the United States: new evidence on an old debate. Am J Orthopsychiatr. 1995;65(3):347–54. doi: 10.1037/h0079653. [DOI] [PubMed] [Google Scholar]
- 18.Center for Disease Control and Prevention (CDC) Behavioral risk factor surveillance system survey questionnaire. Center for Disease Control and Prevention; Atlanta: 2011. [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 20.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24(7):783–8. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The Addiction Severity Index at 25: origins, contributions and transitions. Am J Addict. 2006;15(2):113–24. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 22.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 23.Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) J Behav Med. 2007;30(5):359–70. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Champion V, Skinner CS, Menon U. Development of a self-efficacy scale for mammography. Res Nurs Health. 2005;28(4):329–36. doi: 10.1002/nur.20088. [DOI] [PubMed] [Google Scholar]
- 25.Lehavot K, Huh D, Walters KL, King KM, Andrasik MP, Simoni JM. Buffering effects of general and medication-specific social support on the association between substance use and HIV medication adherence. AIDS Patient Care STDs. 2011;25(3):181–9. doi: 10.1089/apc.2010.0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cope DW, Linn LS, Leake BD, Barrett PA. Modification of residents’ behavior by preceptor feedback of patient satisfaction. J Gen Intern Med. 1986;1(6):394–8. doi: 10.1007/BF02596425. [DOI] [PubMed] [Google Scholar]
- 27.Tulsky JA, Arnold RM, Alexander SC, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593–601. doi: 10.1059/0003-4819-155-9-201111010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–8. [PubMed] [Google Scholar]
- 29.Glickman SW, Boulding W, Manary M, et al. Patient satisfaction and its relationship with clinical quality and inpatient mortality in acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3(2):188–95. doi: 10.1161/CIRCOUTCOMES.109.900597. [DOI] [PubMed] [Google Scholar]