Abstract
The present study examined whether the presence of comorbid ODD differentially moderated the outcome of two Behavioral Parent Training (BPT) programs in a sample of preschoolers with ADHD: One designed specifically for ADHD (NFPP: New Forest Parenting Programme) and one designed primarily for ODD (HNC: Helping the Noncompliant Child). In a secondary analysis, 130 parents and their 3–4 year-old children diagnosed with ADHD were assigned to one of the two programs. 44.6 % of the children also met criteria for ODD. Significant interactions between treatment conditions (NFPP vs. HNC) and child ODD diagnosis (presence vs. absence) indicated that based on some parent and teacher reports, HNC was more effective with disruptive behaviors than NFPP but only when children had a comorbid diagnosis. Further, based on teacher report, NFPP was more effective with these behaviors when children had a diagnosis of only ADHD whereas HNC was equally effective across ADHD only and comorbid ODD diagnoses. Comorbidity profile did not interact with treatment program when parent or teacher reported ADHD symptoms served as the outcome. Implications for clinical interventions are discussed and directions for future work are provided.
Keywords: Parent management training, Attention-deficit/hyperactivity disorder, Oppositional defiant disorder, Moderation, Preschool children
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by inconsistent attention, excessive activity and impulsive behaviors (Nigg and Barkley 2014). It is already prevalent in the preschool years (e.g., Lavigne et al. 2009; National Center for Health Statistics, 2011–2012). Although there are cultural, regional, and country differences in prevalence (see Nigg and Barkley 2014), ADHD has been identified as one of the most prevalent disorders among preschoolers in multiple countries (e.g., Lavigne et al. 2009; Wichstrøm et al. 2012). Individuals who are identified at a young age often continue to manifest symptoms across development and other externalizing behavior problems often emerge (Barkley et al. 2004; Lavigne et al. 1998; Riddle et al. 2013): A developmental profile strongly predictive of health economic burden across the lifespan (Chorozoglou et al. 2015). Given this, early detection and intervention are critical (e.g., Sonuga-Barke and Halperin 2010; Sonuga-Barke et al. 2011). The recommended initial intervention for preschool-aged children diagnosed with ADHD is behavioral parent training (BPT) (Charach et al. 2013; Novotney 2015; Rajwan et al. 2012) which positively affects a range of outcomes (for reviews, see Charach et al. 2013; Mulqueen et al. 2013).
Adverse developmental outcomes appear to be more pronounced for children who present with a comorbid Oppositional Defiant Disorder (ODD) (Angold et al. 1999). The DSM-5 describes ODD as “a pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least 6 months” (American Psychiatric Association, APA 2013, p. 462). However, there has been no comparison of the value of different BPT programs specifically for those preschoolers with both ADHD and ODD. The current study aims to address this question by comparing the extent to which comorbid ODD moderates the effects of two programs—one designed specifically for ADHD (New Forest Parenting Programme [NFPP]; Sonuga-Barke et al. 2006) and one designed primarily for ODD (Helping the Noncompliant Child [HNC]; Forehand and McMahon 1981; McMahon and Forehand 2003).
HNC and NFPP
Hanf developed the original Behavioral Parent Training (BPT) program for preschool-aged children in the 1960s to address oppositional behaviors, including child noncompliance and aggression (see Reitman and McMahon 2013). Since then, a number of programs labeled as Hanf-based interventions (McMahon and Forehand 2003, p. 24) have emerged, notably “Parent-Child Interaction Therapy” (PCIT; Eyberg and Boggs 1998), “Incredible Years” (IY; Webster-Stratton 2000), “Defiant Children” (DC; Barkley 1997), and “Helping the Noncompliant Child” (HNC; Forehand and McMahon 1981; McMahon and Forehand 2003). Each of these programs is primarily delivered in a clinic setting, focuses on enhancing the parent-child relationship, utilizes disciplinary skills to reduce oppositional behavior, and has been shown to be effective for children presenting with ODD (e.g., see Eyberg et al. 2008, for a review).
The efficacy of the foregoing Hanf programs also has been examined in children primarily diagnosed with ADHD. Both Van Den Hoofdakker et al. (2007) and Webster-Stratton et al. (2011) found that, relative to a control condition, a Hanf-based BPT reduced parent-reported oppositional behaviors (i.e., ODD symptoms) when implemented in a sample of children primarily diagnosed with ADHD. However, the former study failed to find a reduction in parent reported ADHD symptoms and the latter study failed to find a reduction in any school disruptive and ADHD behaviors. Such findings have led other investigators to utilize different BPT interventions to address preschoolers’ ADHD symptoms.
The New Forest Parenting Programme (NFPP) is one such program considered to be a potentially effective intervention for young children diagnosed with ADHD. In addition to the aspects targeted by Hanf-based BPT interventions, the New Forest Parenting Programme (NFPP) was designed to target a preschool child’s self-regulation abilities—deficits that putatively underlie ADHD symptoms (Sonuga-Barke et al. 2006). However unlike Hanf-based programs, which are delivered in a clinic setting, NFPP uses the family’s home environment as a context for the teaching of these elements (Sonuga-Barke et al. 2006). These distinctive activities are primarily taught through the use of specific games; for example, memory and attention are targeted through the “I spy” game (e.g., “I spy something blue”) (Sonuga-Barke et al. 2006). Accordingly, Thompson et al. (2009) described the NFPP approach as incorporating “constructive parenting” as the “parent acts as an ‘engine’ for the development of their child’s self-regulatory and self control” skills (p. 606). NFPP is distinctive in its claim that it systematically targets ADHD processes; therefore, this program is expected to “have a greater, more wide-ranging impact on preschool ADHD symptoms than standard BPT” (Abikoff et al. 2015, p. 619). In terms of similarities to Hanf-based programs, NFPP targets the parent-child relationship and to some extent also draws on standard behavioral principles to reduce child noncompliance and oppositional behaviors (Sonuga-Barke et al. 2006). Although, given the other foci, a smaller proportion of time is taken up with these elements.
The efficacy of the NFPP has been evaluated in several randomized controlled trials. When delivered by trained nurse therapists in a community sample of 3-year old children with ADHD symptoms, parents who participated reported a significant reduction in their children’s ADHD and ODD symptoms (Sonuga-Barke et al. 2001). In contrast, a subsequent study implemented in routine primary care settings was unable to replicate the initial results (Sonuga-Barke et al. 2004). However, when a revised version of the NFPP was tested, reductions in both ADHD and ODD symptoms were noted again and sustained at a 7-week follow-up assessment (Thompson et al. 2009). School behavior was not examined in these three investigations.
A recent randomized controlled trial contrasted NFPP with a Hanf-based program—the HNC program—to probe treatment efficacy of each intervention in reducing ADHD symptoms, and secondarily oppositional behaviors, in preschoolaged children diagnosed with ADHD (Abikoff et al. 2015). This investigation included a waitlist (WL) control group and a multi-informant, multi-method assessment (i.e., parent, clinician, and teacher reports, laboratory measures of sustained attention and delay of gratification). Findings indicated that, relative to the control group, children in both active treatment conditions showed a significant reduction at post-treatment in both inattention and hyperactivity/impulsivity symptoms and one of two disruptive behaviors (i.e., defiance; NFPP was not different from WL for parent-reported child physical aggression) when parent (but not teacher) report was utilized. Clinician ratings, based on parent input, confirmed the parent reports of reductions in ADHD symptoms. The two treatment groups did not differ significantly from controls in sustained attention and ability to delay at post treatment. NFPP and HNC did not differ from each other at post-treatment on any outcome measures and gains were maintained at a 7-month follow-up for symptoms of inattention, defiance, and physical aggression but not hyperactivity/impulsivity symptoms.
The findings from Abikoff et al. (2015) suggest that a program designed for ADHD and a program designed for oppositional behaviors are both effective with preschool children diagnosed with ADHD based on parent, but not teacher, report. As Abikoff et al. (2015) noted, because parents (unlike teachers) were actively involved as treatment agents in NFPP and HNC, the significant improvements reported by parents may reflect rater bias effects. If so, these treatment allegiance biases presumably should have resulted in a general halo effect that influenced parent ratings similarly in both treatment groups, regardless of the children’s characteristics. However, to the extent that an overall halo effect was not operative, it allows us to address a question of clinical significance; namely, whether these BPT approaches work equally well for ADHD preschoolers with and without comorbid ODD. This question is the primary focus of this study.
Moderation of Treatment Response
Although BPT has generally been found to effectively change child behaviors (Eyberg et al. 2008), effect sizes have often been small to moderate and heterogeneous outcomes sometimes have emerged across studies (see Lundahl et al. 2006, for a review). To account for such results, researchers have begun to examine baseline variables to ascertain for whom and under what conditions BPT is effective (i.e., moderation). As Beauchaine et al. (2005) have noted, moderators “differentially predict outcome across treatment conditions” (p. 372). Identifying moderators of treatment outcomes is important for several reasons; among other things, such information can inform clinical work. The ultimate goal is to tailor interventions, such as BPT, to clients’ specific needs to increase effectiveness of the treatment.
Because BPT was originally developed to address child oppositional behaviors (see Forehand et al. 2013), most of the extant work on moderators of BPT has focused on children presenting with ODD symptoms rather than ADHD symptoms (see Lundahl et al. 2006 for a review of BPT studies with child ODD symptoms). This body of work suggests that, relative to children with non-clinical levels of ODD symptoms, those with clinical levels decrease more from pre- to post-treatment (Lundahl et al.). With one exception, the role of ODD symptoms alone (i.e., not combined with other symptoms or disorders) as a moderator of treatment response for children with ADHD has not been examined.1
Webster-Stratton et al. (2013) recently examined seven moderators of BPT treatment response at a 1-year follow-up in a sample of preschool-aged children diagnosed with ADHD. The intervention consisted of a combined Hanf-based BPT (i.e., the Incredible Years program) and a child-directed intervention. Baseline ODD symptom severity was the only variable that moderated BPT effectiveness: Two of seven measures of child oppositional behavior and none of the five measures of child ADHD symptoms were moderated. For the two significant interactions (mother reported Conners oppositional and father reported number of problems on Eyberg), children with higher levels of ODD symptoms at baseline improved more than those with low levels. This finding is not surprising as the former group had more room for improvement than the latter group. Although examining only one intervention rather than the differential impact of ODD symptoms across multiple interventions (Beauchaine et al. 2005), conclusions drawn from this study align with Lundahl et al.’s (2006) meta-analytic findings with children referred primarily for ODD. Taken together, these results suggest that a child’s initial level of ODD symptoms might serve to moderate changes in oppositional behavior, but not ADHD symptoms, when young ADHD children and their parents undergo treatment with a Hanf-based BPT program.
The Current Study
Building on the work of Webster-Stratton et al. (2013) and the Lundahl et al. (2006) review, the current study examined whether a comorbid diagnosis of ODD differentially impacts the outcome of programs designed for ADHD (NFPP) versus oppositional behaviors (HNC) in preschool children diagnosed with ADHD. We conceptualized moderation according to Beauchaine et al. (2005): A baseline variable that differentially predicts outcome across multiple treatment groups. Research to date has not examined the differential impact of a child’s baseline ODD diagnosis on multiple interventions when a child has been diagnosed with ADHD. We used a diagnosis of ODD, rather than a symptom count, as the moderator based in part on Lundahl et al.’s findings (i.e., clinical vs. non-clinical levels of ODD moderate child outcomes) and in part to inform clinical work about BPT interventions when children have comorbid diagnoses.
In the primary outcome study (Abikoff et al. 2015), parents, but not teachers, reported reductions in ADHD symptoms and disruptive behaviors with both parenting programs. However, the role of an ODD comorbid diagnosis was not considered. We hypothesized that an ODD diagnosis would differentially impact the outcome of HNC and NFPP in the following ways. First, for children with a comorbid diagnosis (ADHD + ODD), HNC would be associated with less disruptive behaviors (i.e., defiance and physical aggression) post-treatment than NFPP as the former program was specifically designed to reduce such symptoms. In contrast, when there was not a comorbid diagnosis of ODD, we hypothesized NFPP would reduce ADHD symptoms more than HNC as it was designed for these types of symptoms. We reasoned that NFPP would be most effective when oppositional defiant behaviors were not present at a clinical level to impede the intervention of targeting ADHD processes. We examined both parent and teacher report. As teachers were blind informants, they served as reporters who were not influenced by potential bias effects. We also examined outcomes at both post-treatment and 7-month follow-up in order to ascertain if differential effects were more pronounced immediately after treatment or after parents had an opportunity to use the skills for a period of time. Finally, we explicated interactions not only by contrasting NFPP and HNC when children had only an ADHD diagnosis and when they had a comorbid diagnosis (i.e., between intervention comparison) but also by examining whether each treatment was more effective with a single (i.e., ADHD) versus comorbid (i.e., ADHD + ODD) diagnosis (i.e., within intervention comparison).
Method
Complete details of the Methods are available in Abikoff et al. (2015) and the online Appendix accompanying that study.
Site
The study was conducted at New York University (NYU) Langone Medical Center between March 2008 and December 2012. NYU and New York City Department of Education institutional review boards approved the study. Parents provided signed informed consent.
Design
In a three-group parallel design, children were randomly assigned to (a) NFPP, (b) HNC, or (c) waitlist (see Abikoff et al. 2015, for details). The first two groups were the focus of the current study as the differential impact of NFPP and HNC relative to the waitlist group was examined in the primary outcome study. These two groups were assessed at pre-treatment (PRE), post-treatment (POST), and follow-up (FU) 6.8 months later.
Participants
Participants were 130 boys and girls (ages 3.0–4.11 years of age) attending a preschool, daycare or nursery school at least 2 and-a-half days a week. Inclusion criteria included: the primary caretaker was fluent in English; and the child had to have an IQ > 70 and a diagnosis of ADHD (DSM-IV, APA, 1994). The diagnosis was based on the Diagnostic Interview Schedule for Children-Parent Report Version 4 (Shaffer et al. 1998), modified Young Child Version (DISC-IV-YC) (Lucas et al. 1998), confirmed by clinical evaluation conducted by a psychologist with the child and parent. Reasons for exclusion included current medication or behavioral treatment for ADHD; a diagnosis of pervasive developmental disorder, psychosis, or posttraumatic stress disorder; history of sexual or physical abuse; or any other psychiatric or medical condition judged to contraindicate participation.
Recruitment and Sample Size Determination
Recruitment relied on referrals from preschools, daycares, nursery schools, community resources (clinics, physicians, and agencies), parent mailings, newspaper ads, and website postings. The sample size was selected to allow at least 80 % power for two-sided tests with significance level 0.05. The planned sample size allowed detecting group differences of magnitude Cohen’s d = 0.51–0.55 (depending on dropout rate).
Measures
Child ODD Diagnosis
A DSM (4th ed.; DSM-IV; American Psychiatric Association 1994) diagnosis of ODD was derived from the Diagnostic Interview Schedule for Children-Parent Report Version 4 (Shaffer et al. 1998), modified Young Child Version (DISC-IV; Lucas et al. 1998), and confirmed by clinical evaluation conducted by a psychologist.
ADHD Symptoms
This outcome was assessed by parent and teacher ADHD ratings on the Conners’ Rating Scales. The Parent and Teacher Rating Scale-Revised (CPRS-R; Conners et al. 1998), which has been validated with samples that include preschool age children, provides two subscale scores: Hyperactivity/Impulsivity (H/I) and Inattention (IN). The scale has adequate psychometric properties (e.g., Conners et al. 1998). The alpha coefficients for the H/I and IN sub-scales ranged from 0.81 to 0.92 (average of 0.87) for pre, post, and FU assessments in the current sample.
Physical Aggression and Defiant Behaviors
These outcomes were assessed with the parent and teacher completed preschool version of the New York Parent and Teacher Rating Scales (NYRS, Brotman et al. 2008). The scale has Defiance and Physical Aggression subscales. The scales have adequate psychometric properties (e.g., Brotman et al. 2008; Collette et al. 2003; Miller et al. 1995). The alpha coefficients for the Defiance and Physical Aggression subscales across reporters ranged from 0.77 to 0.96 (average of 0.92) for pre, post, and FU assessments in the current sample.
Interventions
New Forest Parenting Programme (NFPP; Thompson et al. 2009)
The NFPP is a manualized intervention for preschoolers with ADHD, involves 8 weekly 1-to-1.5-h sessions, and is delivered in the family home by trained clinicians. NFPP focuses on key issues related to a child with ADHD’s self-regulation ability, and relies on the parent as the primary agent of change. While it shares a number of features with standard BPT (e.g., targets the defiant behaviors through changing the parent-child relationship), it has a number of distinctive features. First, NFPP educates parents to alter their views of ADHD, avoid blaming their child for ADHD symptoms, and increase parental tolerance with the ultimate goal of improving the quality of the parent-child relationship. Second, NFPP directly aims to improve four elements of constructive parenting: (i) Scoping– learning how to observe their child’s current level of competencies so as to promote realistic expectations and performance goals for their child regarding self-control, attention, and memory; (ii) Extending – establishing new goals based on their child’s performance and progress; (iii) Scaffolding– using game-like activities to facilitate their child’s skills development and goal achievement; and (iv) Consolidation—promoting their child’s skill use across settings and situations to facilitate generalization.
Helping the Noncompliant Child (HNC; McMahon and Forehand 2003)
HNC is a manualized BPT intervention for treating young children with noncompliance and oppositional problems. The individualized, clinic-based treatment is delivered by therapists with the parent and child jointly in each session. The clinical provision of HNC typically averages 8–10 intervention sessions (McMahon and Forehand 2003). To ensure that NFPP and HNC were equated for length and amount of therapist contact, HNC was delivered in 8 weekly sessions, lasting approximately 1 h. HNC was provided according to the details specified in the McMahon and Forehand (2003) treatment manual, except that meeting behavioral criteria for advancement from one parenting skill to the next was not required.
The program includes two phases. Phase I focuses on differential attention. Parents are taught how to attend to, describe, and verbally reward their child’s appropriate behavior to the child and to ignore their child’s minor, inappropriate attention-seeking behaviors. Phase II focuses on increasing child compliance. Parents learn to use clear and simple instructions and to provide positive attention and verbal rewards for compliance and time-out for noncompliance.
Treatment Delivery
Therapists (n = 5) were clinical psychologists with at least 2 years of behavior therapy experience with children and families. To control for possible therapist effects, each therapist provided both treatments (see Abikoff et al. 2015, for therapist training, supervision, and treatment fidelity procedures).
Data Analytic Plan
Mplus 6.0 software (Muthén and Muthén 2010) was used to conduct regression analyses with two between-subject factors, treatment program (NFPP vs. HNC) and child ODD diagnosis (presence vs. absence), their interaction, and baseline of the outcome variable serving as the covariate. Outcome measures consisted of parent and teacher ratings of child inattention, hyperactivity/impulsivity, defiance, and physical aggression, both at POST and at FU. As examination of the differential role of ODD diagnosis in moderating the outcomes of two intervention programs (NFPP and HNC) was the purpose of this study, the interaction between these two variables was of interest in the analyses. We examine both between intervention comparisons when a comorbid diagnosis was absent (NFPP vs. HNC) and present (NFPP vs. HNC) and within intervention comparisons (NFPP or HNC) across ADHD only and ADHD plus ODD diagnosis. To account for missing data and non-normality in outcomes, full information maximum likelihood estimation with robust standard errors was used for inclusion of all available data.
Results
Sample
The parents and children who participated in the NFPP (n = 67) and HNC (n = 63) interventions, but not the waitlist control (n = 34), served as participants in this study. Eight dropped out from NFPP (11.9 %) and four from HNC (6.3 %) but all were included in analyses. [See Abikoff et al. (2015) for participant flow chart (CONSORT diagram)].
The study sample was 74.6 % male, 68.3 % White, 14.6 % Black, 9.8 % Asian, and 7.3 % other; 26.9 % of participants were Hispanic. Children’s mean IQ was 102.3 (± 14.2). DSM-IVADHD subtype diagnoses were 50.8 % Combined, 33.8 % Hyperactive/Impulsive, and 14.6 % Inattentive; 44.6 % had a diagnosis of oppositional-defiant disorder. Regarding educational status, 73 % of mothers and 60.5 % of fathers were college graduates. The primary caregivers and informants were predominantly mothers (94 %). No child started medication from PRE to POST. At FU, three children in NFPP and three in HNC were reported to have started medication. There were no significant treatment program group differences on any demographic and clinical variables. Specific details regarding attendance (which was high), contamination across treatments (low), and treatment fidelity (high) are reported in Abikoff et al. (2015).
Primary Analyses
Descriptive statistics for main outcomes for each treatment condition by timepoint and comorbidity status are depicted in Table 1. Although not included in analyses, the means and standard deviations for the waitlist control group (n = 34) are also presented for the two times they were assessed (baseline and post). The standardized estimates and 95 % confidence intervals for all models at POST and at FU are presented in Table 2.
Table 1.
Means and standard deviations of study outcomes by time point and by comorbidity status
| Baseline – M(SD)
|
Post – M (SD)
|
Follow-up – M(SD)
|
||||
|---|---|---|---|---|---|---|
| ODD− | ODD+ | ODD− | ODD+ | ODD− | ODD+ | |
| Parent-reported Defiance | ||||||
| NFPP | 13.8 (7.6) | 22.0 (8.2) | 9.1 (4.3) | 15.0 (7.8) | 10.8 (6.7) | 15.7 (7.6) |
| HNC | 14.1 (6.9) | 23.0 (7.3) | 9.7 (6.8) | 12.3 (6.7) | 11.0 (7.8) | 14.1 (9.7) |
| WL | 15.8 (11) | 24.7 (6.3) | 16.2 (8.1) | 23.3 (9.4) | – | – |
| Teacher-reported Defiance | ||||||
| NFPP | 14.6 (9.9) | 23.8 (11) | 10.6 (7.2) | 17.3 (10) | 6.5 (7.0) | 16.3 (12) |
| HNC | 14.0 (10) | 21.8 (12) | 13.9 (10) | 15.8 (10) | 8.6 (8.2) | 10.4 (10) |
| WL | 16.9 (11) | 18.4 (10) | 12.1 (10) | 15.1 (12) | – | – |
| Parent-reported Aggression | ||||||
| NFPP | 1.4 (1.6) | 4.4 (3.6) | 1.25 (1.3) | 3.3 (3.4) | 1.1 (1.2) | 1.8 (2.2) |
| HNC | 1.8 (3.5) | 4.9 (4.4) | 1.4 (2.7) | 2.1 (2.1) | 1.7 (2.1) | 2.2 (2.0) |
| WL | 3.2 (5.0) | 5.4 (4.3) | 3.3 (4.2) | 4.7 (3.9) | – | – |
| Teacher-reported Aggression | ||||||
| NFPP | 2.4 (3.4) | 6.5 (5.2) | 1.5 (2.1) | 4.8 (4.4) | .5 (1.0) | 4.8 (5.1) |
| HNC | 2.8 (3.6) | 5.8 (5.2) | 2.4 (3.4) | 3.3 (3.8) | 1.8 (3.7) | 2.2 (4.1) |
| WL | 5.3 (5.7) | 2.4 (3.0) | 2.5 (3.3) | 2.3 (2.7) | – | – |
| Parent-reported IN | ||||||
| NFPP | 14.6 (8.8) | 17.2 (6.9) | 11.7 (7.2) | 13.1 (7.0) | 13.0 (9.5) | 12.9 (7.5) |
| HNC | 15.1 (6.7) | 15.7 (7.0) | 10.0 (6.7) | 10.1 (7.7) | 11.3 (6.4) | 9.3 (6.3) |
| WL | 18.5 (7.8) | 18.3 (8.2) | 17.7 (7.2) | 18.4 (8.4) | – | – |
| Teacher-reported IN | ||||||
| NFPP | 7.1 (4.7) | 6.8 (3.6) | 5.1 (3.8) | 4.6 (4.3) | 4.1 (5.7) | 3.6 (4.0) |
| HNC | 6.6 (4.7) | 7.6 (4.5) | 5.3 (5.8) | 5.2 (4.3) | 2.9 (2.2) | 5.8 (7.1) |
| WL | 4.8 (3.3) | 9.0 (7.7) | 4.3 (3.7) | 6.6 (5.4) | – | – |
| Parent-reported HI | ||||||
| NFPP | 17.9 (6.0) | 19.3 (5.2) | 12.8 (6.5) | 13.1 (6.1) | 14.6 (6.6) | 14.4 (5.7) |
| HNC | 19.9 (4.1) | 19.0 (4.5) | 11.6 (5.1) | 12.1 (5.1) | 13.0 (6.0) | 12.4 (6.2) |
| WL | 19.5 (5.1) | 21.4 (7.3) | 17.8 (6.3) | 21.2 (6.7) | – | – |
| Teacher-reported HI | ||||||
| NFPP | 15.0 (4.9) | 16.2 (4.2) | 11.8 (5.4) | 12.3 (5.5) | 8.1 (4.3) | 10.8 (6.4) |
| HNC | 15.6 (4.5) | 15.1 (5.1) | 13.3 (5.1) | 12.0 (4.9) | 10.3 (5.6) | 8.3 (6.2) |
| WL | 16.3 (4.2) | 15.3 (6.3) | 12.5 (6.0) | 13.3 (6.5) | – | – |
ODD Oppositional Defiant Disorder (0 = absent; 1 = present), IN Inattention, HI Hyperactive/Impulsive
Table 2.
Regression analyses conducted using Mplus with maximum likelihood estimation with robust standard errors for four outcomes at post-treatment and follow-up
| Parent Report
|
Teacher Report
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post
|
Follow-up
|
Post
|
Follow-up
|
|||||||||
| β | 95 % CI | p | β | 95 % CI | p | β | 95 % CI | p | β | 95 % CI | p | |
| DV: NYRS Defiance | ||||||||||||
| Baseline DV | 0.64 | 0.52–0.77 | 0.000 | 0.57 | 0.50–0.70 | 0.000 | 0.79 | 0.71–0.87 | 0.000 | 0.35 | 0.15–0.55 | 0.001 |
| Treatment Program | −0.10 | −0.23–0.03 | 0.121 | −0.03 | −0.20–0.15 | 0.763 | −0.16 | −0.29 – −0.04 | 0.011 | −0.10 | −0.28–0.09 | 0.317 |
| ODD | −0.13 | −0.28–0.02 | 0.100 | −0.05 | −0.29–0.18 | 0.654 | −0.11 | −0.26–0.04 | 0.147 | −0.01 | −0.23–0.21 | 0.911 |
| Interaction | 0.26 | 0.08–0.43 | 0.005 | 0.10 | −0.17–0.36 | 0.473 | 0.13 | −0.04–0.30 | 0.127 | 0.28 | −0.01–0.58 | 0.057 |
| DV: NYRS Aggression | ||||||||||||
| Baseline DV | 0.49 | 0.31–0.67 | 0.000 | 0.43 | 0.18–0.68 | 0.001 | 0.71 | 0.59–0.83 | 0.000 | 0.32 | 0.10–0.54 | 0.004 |
| Treatment Program | 0.02 | −0.12–0.15 | 0.820 | −0.01 | −0.20–0.19 | 0.944 | −0.12 | −0.25–0.01 | 0.057 | −0.10 | −0.25–0.05 | 0.182 |
| ODD | −0.05 | −0.25–0.14 | 0.596 | 0.01 | −0.25–0.28 | 0.924 | −0.09 | −0.24–0.06 | 0.225 | −0.05 | −0.29–0.19 | 0.672 |
| Interaction | 0.21 | 0.03–0.40 | 0.021 | −0.03 | −0.33–0.27 | 0.833 | 0.24 | 0.04–0.24 | 0.017 | 0.36 | 0.08–0.64 | 0.013 |
| DV: CRS IN | ||||||||||||
| Baseline DV | 0.53 | 0.41–0.66 | 0.000 | 0.47 | 0.32–0.62 | 0.000 | 0.70 | 0.60–0.80 | 0.000 | 0.17 | 0.01–0.32 | 0.035 |
| Treatment Program | 0.03 | −0.12–0.24 | 0.758 | 0.11 | −0.11–0.33 | 0.329 | −0.08 | −0.27–0.11 | 0.426 | 0.02 | −0.21–0.25 | 0.888 |
| ODD | −0.06 | −0.30–0.20 | 0.623 | −0.14 | −0.34–0.06 | 0.156 | −0.08 | −0.28–0.11 | 0.398 | 0.20 | −0.04–0.43 | 0.104 |
| Interaction | 0.11 | −0.17–0.38 | 0.460 | 0.05 | −0.21–0.30 | 0.717 | 0.06 | −0.17–0.30 | 0.610 | −0.17 | −0.44–0.11 | 0.227 |
| DV: CRS HI | ||||||||||||
| Baseline DV | 0.58 | 0.46–0.70 | 0.000 | 0.47 | 0.31–0.62 | 0.000 | 0.60 | 0.48–0.72 | 0.000 | 0.23 | 0.07–0.40 | 0.005 |
| Treatment Program | 0.19 | −0.02–0.41 | 0.076 | 0.20 | −0.02–0.41 | 0.077 | −0.08 | −0.27–0.12 | 0.454 | −0.18 | −0.40–0.04 | 0.105 |
| ODD | 0.10 | −0.10–0.31 | 0.316 | −0.01 | −0.25–0.24 | 0.941 | −0.09 | −0.29–0.11 | 0.361 | −0.13 | −0.41–0.15 | 0.354 |
| Interaction | −0.15 | −0.43–0.12 | 0.277 | −0.08 | −0.40–0.21 | 0.586 | 0.06 | −0.18–0.06 | 0.624 | 0.28 | −0.02–0.57 | 0.065 |
N = 130; Treatment Program is coded such that 0 = HNC and 1 = NFPP; ODD Oppositional Defiant Disorder (0 = absent; 1 = present); Interaction = Treatment Program × ODD; NPRS New York Rating Scale, CRS Conners’ Rating Scale, IN Inattention, HI Hyperactive/Impulsive
Parent Outcomes
A treatment program by child ODD diagnosis interaction emerged for both parent-reported defiance and physical aggression at POST. Figures 1a and b illustrate the form of the interactions by depicting the regression lines of the relation between diagnostic status and defiance (Fig. 1a) and physical aggression (Fig. 1b) separately for each treatment group (Hayes 2013). The metric of the Yaxis in all figures is change from baseline. Probing the interactions and testing simple slopes (Hayes 2013) indicated that the conditional effect of treatment condition (NFPP vs. HNC) on defiance and physical aggression symptoms was significant for children with ODD (p < 0.05) but not significant for children without ODD (p > 0.10) for both measures of disruptive behavior at POST. When there was a comorbid ODD diagnosis, HNC was associated with less disruptive behavior than NFPP. For within intervention comparisons, none of the slopes of the lines was significant. The interaction of ODD status and treatment condition was not significant at FU on parent ratings of defiance and physical aggression. In addition, child ODD status did not moderate treatment outcome for ADHD symptoms at POST nor for any of the outcomes at FU.2
Fig. 1.
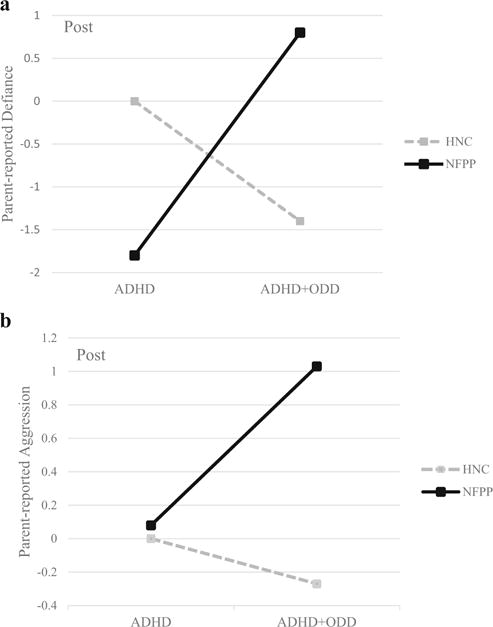
a Interaction of ODD diagnosis (presence vs. absence) by treatment program (NFPP vs. HNC) for parent-reported child defiance at POST. b Interaction of ODD diagnosis (presence vs. absence) by treatment program (NFPP vs. HNC) for parent-reported child physical aggression at POST
Teacher Outcomes
In regard to teacher-reported outcomes, a significant treatment program by child ODD diagnosis interaction emerged for physical aggression at POST and FU and approached significance (p = 0.057) for defiance at FU. Figures 2a, b, and c illustrate the form of the interactions by depicting the regression lines of the relation between diagnostic status and defiance at FU (Fig. 2a), physical aggression at POST (Fig. 2b), and physical aggression at FU (Fig. 2c) separately for each treatment group (Hayes 2013). Probing the interaction and testing simple slopes (Hayes 2013), between intervention comparisons indicated the conditional effect of treatment condition (NFPP vs. HNC) for teacher-reported physical aggression at follow-up was significant for children with ODD (p < 0.05) but not significant for children without ODD (p > 0.10). When there was a comorbid ODD diagnosis, HNC was associated with less physical aggression than NFPP. For within intervention comparisons, for all three teacher reported interactions, the slope of the NFPP across child comorbidity status was significant (ps < 0.05) and the HNC slope was non-significant (p > 0.10) suggesting NFPP, but not HNC, had differential effectiveness for children with and without ODD comorbid diagnoses. Lastly, congruent with parent-reported models, child ODD status did not moderate treatment outcome for ADHD symptoms at POST or FU.3
Fig. 2.
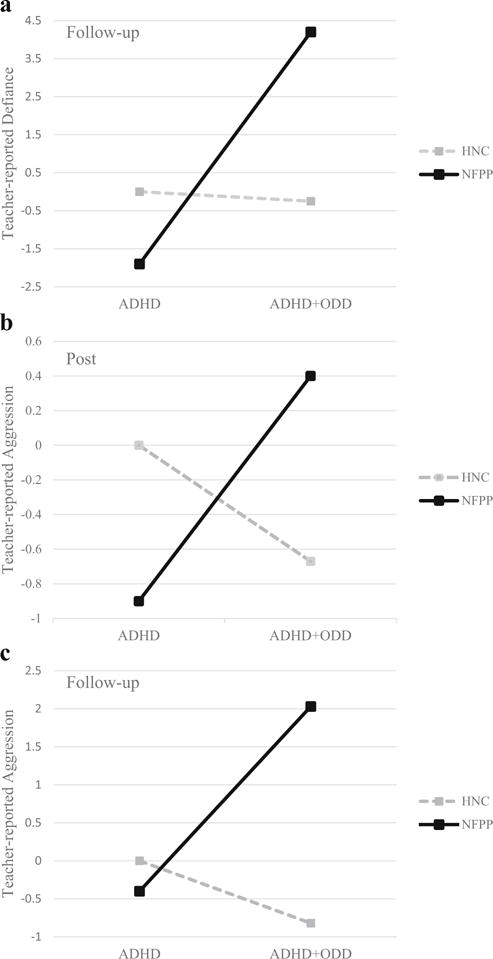
a Interaction of ODD diagnosis (presence vs. absence) by treatment program (NFPP vs. HNC) for teacher-reported child defiance at FU. b Interaction of ODD diagnosis (presence vs. absence) by treatment program (NFPP vs. HNC) for teacher-reported child aggression at POST. c Interaction of ODD diagnosis (presence vs. absence) by treatment program (NFPP vs. HNC) for teacher-reported child aggression at FU
Discussion
The primary outcome study revealed that NFPP and HNC are both effective at posttreatment in reducing ADHD symptoms and disruptive behaviors for preschool-age children diagnosed with ADHD (Abikoff et al. 2015) based on parent report. For most outcomes, both differed from a waitlist control group at post-treatment, and gains were maintained at a 7-month follow-up. In the current secondary analysis study, when children had a comorbid ODD diagnosis, parents and, to some extent, teachers reported fewer disruptive behaviors following HNC than NFPP. Further, NFPP, but not HNC, was differentially effective for children with and without a comorbid diagnosis. For ADHD symptom outcomes, HNC and NFPP were equivalent regardless of whether or not the child had comorbid ODD. These results refine conclusions drawn from the primary outcome study (Abikoff et al. 2015) as they indicate that for select populations, in this case children with comorbid ODD, differential findings emerge for some outcomes across intervention programs.
The results for parent report for disruptive behaviors are congruent with the theoretical underpinnings of the two examined BPT programs. HNC and other Hanf-based interventions were specifically developed to reduce child oppositional behaviors, including defiant and aggressive behaviors. HNC consists of teaching parents a limited number of skills (five) through a structured approach for each session: Homework review, didactics, modeling, role playing with the therapist, practice with the child with and without therapist feedback, and homework assignment. In contrast, although NFPP includes components that resemble Hanf-based BPT (e.g., strengthening the parent-child relationship and addressing noncompliance), these represent secondary goals of the intervention (Thompson et al. 2009) and less time in therapy is focused on these components. NFPP primarily targets preschool children’s self-regulation abilities in an effort to address ADHD symptoms of inattention and impulsivity (Sonuga-Barke et al. 2006), educates caregivers about ADHD symptoms (Abikoff et al. 2015), and includes discussing a number of parenting strategies (e.g., soliciting attention and eye contact, importance of praise, voice control, avoiding threats, quiet time, reminders, limit setting). Modeling, role playing, and practice with child, while occurring, are not the focus of sessions like in HNC. Thus, the two parenting programs differ not only whether the focus is on ODD or ADHD but also on what skills are taught, the number of skills taught, and the teaching method. Given the differences in treatment of HNC and NFPP, it is not surprising that a child’s specific comorbidity profile (i.e., ADHD vs AHDD + ODD) differentially impacted the two treatment programs when disruptive behaviors served as the treatment outcome. Our findings suggest that, as we initially proposed, oppositional behavior may impede the effectiveness of NFPP. A program specifically designed for these behaviors (e.g., HNC), which teaches a limited set of parenting skills through a structured learning approach, may be necessary when there is a comorbid ODD diagnosis.
For teacher reported outcome measures, the form of significant interactions was consistent with parent reported outcomes (see Figs. 1 and 2). HNC and NFPP were equivalent for children without ODD, and HNC received some support for being more effective for children with comorbid ODD. The most consistent finding with teacher reported outcomes was that HNC was equally effective for children with and without comorbid ODD whereas NFPP was differentially effective such that teachers reported higher levels of disruptive behaviors when the child had comorbid ODD. Although significant interactions only emerged at post-treatment for parent reported outcomes, significant interactions also emerged at follow-up for teacher reported outcomes, indicating differential effectiveness across time for the two interventions depending on comorbidity profile. As teachers were blind to treatment condition, these long-term differential effects have important clinical implications, which are noted below.
Regarding the second research hypothesis, we had expected that, among preschoolers who did not have a comorbid diagnosis of ODD, those assigned to NFPP would manifest a larger reduction in the ADHD symptoms at post-treatment compared to children assigned to HNC. This hypothesis was based on the premise that NFPP, which focused on ADHD, would be more effective when not impeded by clinical levels of ODD symptoms. An interaction did not emerge for either inattention or hyperactivity/impulsivity for parent or teacher report, suggesting that HNC and NFPP achieved comparable levels of gains when used to treat these ADHD symptoms. It is important to note that both programs were effective in reducing ADHD symptoms in the original study (Abikoff et al. 2015).
Taken together, our results inform clinical interventions. They point to the importance of completing a comprehensive intake evaluation prior to planning and delivering treatments to children and their families. When working with preschool children with ADHD, a particular focus should be placed on determining whether a child has a comorbid diagnosis of ODD. Our results suggest that Hanf-based programs, such as HNC, can be particularly effective in remediating the disruptive behaviors of preschool-age children diagnosed with both ADHD and ODD. As support for HNC emerged across parents and teachers (who were blind raters), at home and in preschool, and, for teacher ratings, at follow-up, the findings are especially noteworthy. In contrast to disruptive behaviors, the current study suggests that, for ADHD symptoms, neither a Hanf-based program (HNC) nor a program designed specifically for ADHD (NFPP) is moderated by an ODD diagnosis. If the only treatment target is ADHD symptomatology (i.e., inattention and hyperactivity/impulsivity), then the presence or absence of an ODD diagnosis does not appear relevant for selecting one of these intervention programs.
Some of the limitations (e.g., educated parents, interventions limited to eight sessions) and strengths (e.g., clinical sample of ADHD preschoolers, high treatment fidelity and integrity) of the present investigation have been detailed in the primary study (Abikoff et al. 2015) and will not be reiterated here. Specific to the current study, the primary study was powered to detect group differences, not interactions. All moderation effect sizes of the significant interactions (f2 range = 0.01–0.07; medium to large effect sizes) were above the average effect size reported in the literature for tests of moderation (f2 = 0.009; Aguinis et al. 2005). Although our sample size was relatively large, as with most treatment outcome studies, we were underpowered to detect small interaction effect sizes. Finally, there is the issue of rater bias. The inclusion of teacher reports reduces concern about this bias. Furthermore, even if rater bias was present, it did not operate universally as there was differential improvement based on children’s ODD diagnostic status.
Although ODD represents the most common co-occurring diagnosis for children with ADHD (Angold et al. 1999), it is by no means the only potential moderator (see Lundahl et al. 2006). As such, future research should examine whether other moderators, such as parental symptoms or diagnoses (e.g., ADHD) (see Wang et al. 2014), and demographic variables (e.g., child age, family SES), differentially impact BPT programs with parents of ADHD children. Such knowledge could help tailor treatments to individuals’ specific needs, thereby optimizing intervention effects.
In conclusion, results support the recommendation that treatment outcome research identify for whom and under conditions treatment is effective (e.g., Kraemer et al. 2002, 2006; Owens et al. 2003). The ultimate goal of these refined analyses is to help ensure that mental health treatments are delivered both effectively and efficiently to young children and their families.
Acknowledgments
Funding This research was supported by NIMH grant 5R01MH074556 to the last author, NIMH grant R01MH100377 to the first author and NICHD grant F31HD082858 to the second author. The content is solely the responsibility of the authors and does not necessarily represent he official views of the National Institutes of Health.
Footnotes
Jensen et al. (2007) and van den Hoofdakker et al. (2010) examined child comorbidity as a moderator but did not examine ODD individually.
Clinician ratings of ADHD symptoms were included in the primary outcome study (Abikoff et al. 2015). We did not include them as outcomes in the current study as they were based on parent interviews and, thus, overlapped with parental report of child symptoms. We did examine clinician ratings and, as expected, they yielded the same outcome as parent ratings of Inattention and Hyperactivity/Impulsivity.
In exploratory analyses, we examined the marginally significant teacher reported Hyperactive/Impulsive interaction at follow-up. Neither the between treatment nor the within treatment comparison was significant.
Conflicts of Interest J.P., V.D.P, and H.B.A. have no conflict of interest to report. R.F. and N.L. receive royalties from the book ‘Parenting the Strong Willed Child.’ R.F. receives royalties from ‘Helping the Noncompliant Child’ (HNC). E.S.B. declares the following competing interests during the last three years: fees for speaking, consultancy, research funding and conference support from Shire; speaker fees from Janssen Cilag, Medice & Obtech, consultancy support from Neurotech Solutions, book royalties from OUP and Jessica Kingsley; conference support from Shire; grants awarded from MRC, ESRC, Wellcome Trust, Solent NHS Trust, European Union, Child Health Research Foundation New Zealand, NIHR, Nuffield Foundation, Fonds Wetenschappelijk Onderzoek-Vlaanderen (FWO).
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in.
References
- Abikoff HB, Thompson M, Laver-Bradbury C, Long N, Forehand RL, Brotman LM, Sonuga-Barke E. Parent training for preschool ADHD: A randomized controlled trial of specialized and generic programs. Journal of Child Psychology and Psychiatry. 2015;56:618–631. doi: 10.1111/jcpp.12346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguinis H, Beaty JC, Boik RJ, Pierce CA. Effect size and power in assessing moderating effects of categorical variables using multiple regression: A 30-year review. Journal of Applied Psychology. 2005;90:94–107. doi: 10.1037/0021-9010.90.1.94. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, D.C: 1994. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 5th. Arlington: 2013. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Barkley RA. Defiant children: A clinician’s manual for assessment and parent training. 2nd. New York: Guilford; 1997. [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: antisocial activities and drug use. Journal of Child Psychology and Psychiatry. 2004;45:195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: a latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Kamboukos D, Theise R. Symptom-specific measures for disorders usually first diagnosed in infancy, childhood, or adolescence. In: Rush AJ, First MB, Blacker D, editors. Handbook of psychiatric measures. 2nd. Washington, DC: American Psychiatric Publishing, Inc; 2008. pp. 309–342. [Google Scholar]
- Charach A, Carson P, Fox S, Ali MU, Beckett J, Lim CG. Interventions for preschool children at high risk for ADHD: A comparative effectiveness review. Pediatrics. 2013;131:1–21. doi: 10.1542/peds.2012-0974. [DOI] [PubMed] [Google Scholar]
- Chorozoglou M, Smith E, Koerting J, Thompson MJ, Sayal K, Sonuga-Barke EJS. Preschool hyperactivity is associated with long-term economic burden: evidence from a longitudinal health economic analysis of costs incurred across childhood, adolescence and young adulthood. Journal of Child Psychology and Psychiatry. 2015;56:966–975. doi: 10.1111/jcpp.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collette BR, Ohan JL, Myers KM. Ten-year review of rating scales. VI: Scales assessing externalizing behaviors. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1143–1170. doi: 10.1097/00004583-200310000-00006. [DOI] [PubMed] [Google Scholar]
- Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners’ parent rating scale (CPRS-R): factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology. 1998;26:257–268. doi: 10.1023/a:1022602400621. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Boggs SR. Parent-child interaction therapy: A psychosocial intervention for the treatment of young conduct-disordered children. Hoboken: John Wiley & Sons Inc; 1998. [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Forehand RL, McMahon RJ. Helping the noncompliant child: A clinician’s guide to parent training. New York: Guilford Press; 1981. [Google Scholar]
- Forehand R, Jones DJ, Parent J. Behavioral parenting interventions for child disruptive behaviors and anxiety: What’s different and what’s the same. Clinical Psychology Review. 2013;33:133–145. doi: 10.1016/j.cpr.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill LL, et al. 3-year follow-up of the NIMH MTA study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: clinical, research, and policy importance. JAMA. 2006;296:1286–1289. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: I. Stability of diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1246–1254. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child & Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Lucas C, Fisher P, Luby J. Young-child DISC-IV research draft: diagnostic interview schedule for children. New York: Columbia University, Division of Child Psychiatry; 1998. (Joy and William Ruane Center to Identify and Treat Mood Disorders). [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: moderators and follow-up effects. Clinical Psychology Review. 2006;26:86–104. doi: 10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Forehand R. Helping the noncompliant child: Family-based treatment for oppositional behavior. 2nd. New York: Guilford; 2003. [Google Scholar]
- Miller LS, Klein RG, Piacentini J, Abikoff H, Shah MR, Samoilov A, et al. The New York teacher rating scale for disruptive and antisocial behavior. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:359–370. doi: 10.1097/00004583-199503000-00022. [DOI] [PubMed] [Google Scholar]
- Mulqueen JM, Bartley CA, Bloch MH. Meta-analysis: parental interventions for preschool ADHD. Journal of Attention Disorders. 2013;17:1–7. doi: 10.1177/1087054713504135. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide: Statistical analysis with latent variables 2010 [Google Scholar]
- National Center for Health Statistics: The National Survey of Children’s Health (NSCH) The public file and documentation. Hyattville, MD: US Department of Health and Human Services; 2011–2012. [Google Scholar]
- Nigg JT, Barkley RA. Attention-deficit/hyperactivity disorder. In: Mash EJ, Barkley RA, editors. Child psychopathology. 3rd. New York: Guilford; 2014. pp. 75–143. [Google Scholar]
- Novotney A. Behavioral therapy is recommended as the first line of treatment for very young children. So why is medication use rising among this group? Monitor on Psychology. 2015;46:66–67. [Google Scholar]
- Owens EB, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, et al. Which treatment for whom for ADHD? moderators of treatment response in the MTA. Journal of Consulting and Clinical Psychology. 2003;71:540–552. doi: 10.1037/0022-006x.71.3.540. [DOI] [PubMed] [Google Scholar]
- Rajwan E, Chacko A, Moeller M. Nonpharmacological interventions for preschool ADHD: state of the evidence and implications for practice. Professional Psychology: Research and Practice. 2012;43:520–526. [Google Scholar]
- Reitman D, McMahon RJ. Constance “Connie” Hanf (1917–2002): the mentor and the model. Cognitive and Behavioral Practice. 2013;20:106–116. [Google Scholar]
- Riddle MA, Yershova K, Lazzaretto D, Paykina N, Yenokyan G, Greenhill L, et al. The preschool attention-deficit/hyperactivity disorder treatment study (PATS) 6-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:264–278. doi: 10.1016/j.jaac.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C. NIMH DISC-IV diagnostic interview schedule for children, parent-informant. New York: Columbia University; 1998. [Google Scholar]
- Sonuga-Barke EJ, Halperin JM. Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: potential targets for early intervention? Journal of Child Psychology and Psychiatry. 2010;51:368–389. doi: 10.1111/j.1469-7610.2009.02195.x. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJ, Daley D, Thompson M, Laver-Bradbury C, Weeks A. Parent-based therapies for preschool attention deficit/hyperactivity disorder: A randomized, controlled trial with a community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:402–408. doi: 10.1097/00004583-200104000-00008. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Thompson M, Daley D, Laver-Bradbury C. Parent training for pre-school attention-deficit/hyperactivity disorder: Is it effective as part of routine primary care? British Journal of Clinical Psychology. 2004;43:449–457. doi: 10.1348/0144665042388973. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJ, Thompson M, Abikoff H, Klein R, Brotman LM. Nonpharmacological interventions for preschoolers with ADHD: the case for specialized parent training. Infants & Young Children. 2006;19:142–153. [Google Scholar]
- Sonuga-Barke EJ, Koerting J, Smith E, McCann DC, Thompson M. Early detection and intervention for attention-deficit/hyperactivity disorder. Expert Review of Neurotherapeutics. 2011;11:557–563. doi: 10.1586/ern.11.39. [DOI] [PubMed] [Google Scholar]
- Thompson MJ, Laver-Bradbury C, Ayres M, Le Poidevin E, Mead S, Dodds C, et al. A small-scale randomized controlled trial of the revised new Forest parenting programme for preschoolers with attention deficit hyperactivity disorder. European Child & Adolescent Psychiatry. 2009;18:605–616. doi: 10.1007/s00787-009-0020-0. [DOI] [PubMed] [Google Scholar]
- Van Den Hoofdakker BJ, Van der Veen-Mulders L, Sytema S, Emmelkamp PM, Minderaa RB, Nauta MH. Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1263–1271. doi: 10.1097/chi.0b013e3181354bc2. [DOI] [PubMed] [Google Scholar]
- Van Den Hoofdakker BJ, Nauta MH, van der Veen-Mulders L, Sytema S, Emmelkamp PM, Minderaa RB, et al. Behavioral parent training as an adjunct to routine care in children with attention-deficit/hyperactivity disorder: moderators of treatment response. Journal of Pediatric Psychology. 2010;35:317–326. doi: 10.1093/jpepsy/jsp060. [DOI] [PubMed] [Google Scholar]
- Wang CH, Mazursky-Horowitz H, Chronis-Tuscano A. Delivering evidence-based treatments for child attention-deficit/hyperactivity disorder (ADHD) in the context of parental ADHD. Current Psychiatry Reports. 2014;16:1–8. doi: 10.1007/s11920-014-0474-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C. “The Incredible Years training series” bulletin. Washington, DC: U.S. Department of Justice and Delinquency Prevention; 2000. [Google Scholar]
- Webster-Stratton C, Reid MJ, Beauchaine T. Combining parent and child training for young children with ADHD. Journal of Clinical Child & Adolescent Psychology. 2011;40:191–203. doi: 10.1080/15374416.2011.546044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, Beauchaine TP. One-year follow-up of combined parent and child intervention for young children with ADHD. Journal of Clinical Child & Adolescent Psychology. 2013;42:251–261. doi: 10.1080/15374416.2012.723263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichstrøm L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH. Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry. 2012;53:695–705. doi: 10.1111/j.1469-7610.2011.02514.x. [DOI] [PubMed] [Google Scholar]


