Abstract
Background
Hypertension is a common chronic disease among older adults, and is associated with medical complications and mortality. This study aimed to examine the effects of social network characteristics on the prevalence, awareness, and control of hypertension among older adults.
Methods
The Korean Social Life, Health, and Aging Project (KSHAP) interviewed 814 ≥ 60-year-old residents and their spouses from a rural township between December 2011 and March 2012 (response rate: 95%). We evaluated the data from 595 participants. Multivariate logistic regression models were used to assess the effects of network characteristics on hypertension.
Results
We observed strong sex-specific network effects on the prevalence, awareness, and control of hypertension. Among older women, network density was associated with hypertension awareness [odds ratio (OR): 2.63, 95% confidence interval (CI): 1.03–5.37] and control (OR: 1.72; 95% CI: 0.94–3.13). Among older men, large networks were associated with a lower prevalence of hypertension (OR: 0.75; 95% CI: 0.58–0.96). Compared to older women, older men with coarse networks exhibited better hypertension awareness (OR: 0.37; 95% CI: 0.14–0.95) and control (OR: 0.42; 95% CI: 0.19–0.91). Network size interacted with density for hypertension control (P = 0.051), with controlled hypertension being associated with large and course networks.
Conclusions
A large network was associated with a lower risk for hypertension, and a coarse network was associated with hypertension awareness and control among older men. Older women with dense networks were most likely to exhibit hypertension awareness and control.
Keywords: Hypertension management, Sex difference, Social density, Social network
1. Introduction
Hypertension is one of the most common chronic diseases among older adults, and its prevalence has increased with the growing population of older adults.[1] In South Korea, 30% of the adult population (> 30 years old) had hypertension in 2013, and approximately 28% of the adult population had hypertension in 2005.[2] Furthermore, approximately 58.6% of older Korean adults have hypertension, and this rate is much higher than the rate among 30–37-year-old adults (9.7%) or 40–59-year-old adults (27.7%).[2]
Hypertension awareness, control, and prevention are important considerations for addressing this disease. In South Korea, 84.8% of individuals with hypertension are aware that they have high blood pressure, with 83.2% of individuals receiving antihypertensive medications and 57.4% of individuals having controlled hypertension.[2] However, despite > 80% of older adults with hypertension being aware of their condition and receiving medication for hypertension, 50% of seniors have uncontrolled hypertension. Therefore, greater efforts are needed to promote hypertension awareness and control, as this condition can cause medical complications and death.[3],[4]
It is difficult to control an individual's blood pressure, and previous studies have focused on the importance of early detection,[5] medical treatment,[6]–[8] and management of patients' diet and exercise.[9] In addition, recent studies have started to concentrate on the effects of social factors on hypertension management, such as the patient-doctor relationship,[10] or social support from families and friends.[11]–[13] These relationships can help promote coping behaviors, provide information, and promote emotional stability.[14] Several studies have also revealed that social interventions are much more effective than simply focusing on individual risk factors, which has new implications for public health policy at the national level.[15]
Although numerous studies have examined social relationships, only a few studies have investigated the association between social networks and hypertension.[16]–[18] Therefore, this study aimed to investigate the effects of social network characteristics (e.g., size and density) on the prevalence, awareness, and control of hypertension among older adults. In particular, we focused on the sex-specific effects of social network characteristics on hypertension.
2. Methods
2.1. Study sample
This study used data from the Korean Social Life, Health, and Aging Project (KSHAP). The KSHAP study was designed to examine the entire population of ≥ 60-year-old adults and their spouses in Township K, which is located on Ganghwa Island, Korea. Township K is a typical rural Korean community, with ten Ris (the smallest administrative unit in Korea) in one Myeon (township). The total population of Township K in January 2013 was 1864 individuals from 871 families. The KSHAP study identified 860 older adults and their spouses. Approximately 67% of the respondents were working, and 88% of the respondents actively farmed.[19]
Between December 2011 and March 2012, the KSHAP study completed a face-to-face population-based survey that included 814 of the 860 older adults and their spouses who were living in Township K (response rate: 95%). The interviews were performed in the respondents' homes or at community centers, with an average duration of 48 min. All KSHAP participants were invited to health examinations, and 698 people (85.7% of the KSHAP participants; 81.1% of the target population) completed health examinations at a public health center (n = 533) or at their homes (n = 165).[19],[20] The KSHAP study's design was approved by the institutional review board of Yonsei University (YUIRB-2011-012-01).
Analyses for the present study were restricted to 595 respondents, after excluding respondents with insufficient information regarding blood pressure (n = 116), body mass index (BMI, n = 30), education (n = 8), blood pressure check-ups (n = 6), social support from family or friends (n = 11), or participants who had zero (n = 5) or one (n = 43) social network member.
2.2. Prevalence, awareness, and control of hypertension
The prevalence, awareness, and control of hypertension were measured using self-reporting and blood pressure measurements. Resting systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured at least twice, using the oscilloscopic method and an automatic sphygmomanometer (Carescape Dinamap V100; GE Healthcare, Milwaukee, WI). Before each measurement, all participants rested for ≥ 5 min in a seated position, and the cuff size was adapted to their right upper arm. If the first and second SBP and/or DBP measurements varied by ≥ 10 mmHg, additional measurements were performed, and the average of the last two measurements was used for the analysis.[21]
Hypertension was defined as an average SBP of ≥ 140 mmHg, an average DBP of ≥ 90 mmHg, and/or a self-reported clinical diagnosis of hypertension. Hypertension awareness was defined as a self-reported clinical diagnosis of hypertension among participants who were found to have hypertension at the health examination. Among the participants with hypertension, hypertension control was defined as an SBP of < 140 mmHg and a DBP of < 90 mmHg. Respondents were classified as not having hypertension if they did not report a clinical diagnosis of hypertension and exhibited normal blood pressure at the health examination.[22]
2.3. Social network characteristics
To collect egocentric network data, the KSHAP adopted a module that was similar to the module that was used in the National Social Life, Health, and Aging Project. The network module allowed each respondent to identify several members of their personal network, and to provide information regarding these people and their relationships.[23] The KSHAP interviewers asked the respondents to list up to five social network members with whom they had discussed important topics during the last 12 months and a spouse, if applicable (a maximum of 6 members, with a possible range of 0–6 members).[19] However, we excluded respondents who had any zero or one network member, as we aimed to obtain information regarding the relationships among the network members. Thus, the networks in the present study had 2–6 members.
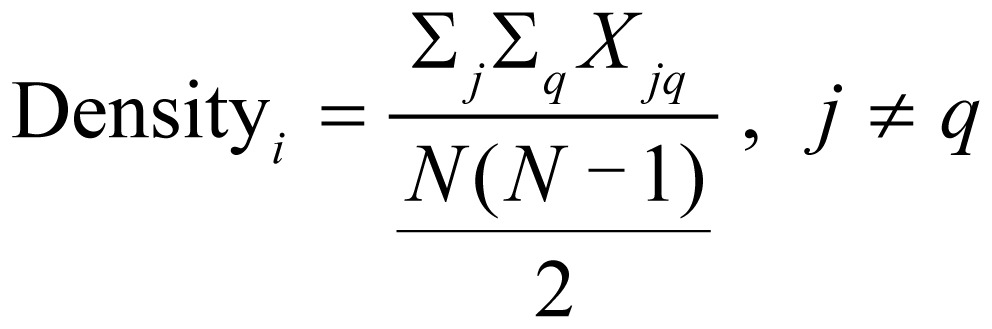 |
Density was used to address the relationships within a network, and was defined as the number of relationships that existed among the members of an individual's social network, as a proportion of the total possible number of relationships.[24],[25] Density was calculated using the following formula, with ‘i’ indicating a respondent, ‘j’ and ‘q’ indicating network members, ‘xjq’ indicating the relationship between ‘j’ and ‘q’, and ‘N’ indicating the total number of people in the network.
To evaluate density, each respondent was asked the following question: “How often does (network member 1) talk to (network member 2)?” The responses were measured on an eight-point scale that ranged from “every day” to “less than once per year.” We assumed that a relationship existed between the two network members if the respondent reported that they “have spoken to each other at least once per week.” Next, density was evaluated as a binary variable based on the average score. A coarse network was defined as a density that was lower than the mean score, and a dense network was defined as a density that was above the mean score. This is because highly dense networks exhibit members who are highly interconnected and provide cohesive, strong, and effective support systems.[26]
2.4. Other measurements
Three indicators of health-related behaviors were included in the analysis: cigarette smoking, alcohol consumption, and blood pressure monitoring. These health-related behaviors are typically included in the recommended lifestyle changes for individuals who are diagnosed with hypertension. Participants were classified as cigarette smokers if they answered that they “currently smoke cigarettes.” Participants were classified as consuming alcohol if they answered that they “currently drink alcohol”. Participants were classified as regularly checking their blood pressure if they answered that they check their blood pressure “at least once per month”. In addition, we considered BMI because obesity can cause hypertension, and participants were classified as having a BMI of < 23.0 kg/m2 or ≥ 23.0 kg/m2. We also accounted for diagnoses of other health problems, such as diabetes, that might influence hypertension awareness and management.
The multivariate regression analyses were adjusted for social support from family or friends. Instrumental support from family or friends was measured by asking how often the participant relied on family or friends for help if they had a practical problem. Emotional support from family or friends was also measured by asking how often the participant expressed their worries to their family members or friends. Instrumental and/or emotional support was considered present if the participant indicated that they “occasionally” or “frequently” sought support. We also controlled for socio-demographic characteristics, such as age, current working status, and education level.
2.5. Statistical analysis
Serial multivariate logistic regression models were constructed to identify factors that were associated with the prevalence, awareness, and control of hypertension. The first model included age, current working status, education level, BMI, cigarette smoking, alcohol consumption, diabetes, blood pressure check-ups, and social network characteristics. In addition to these factors, the second model included the interaction term between network size and density. Statistical analyses were performed separately for men and women, and the results were presented as odds ratios (ORs) and 95% confidence intervals (95% CIs). Two-sided P-values of < 0.05 were considered statistically significant. All analyses were performed using STATA software (version 12.0; College Station, TX).
3. Results
3.1. Participant characteristics
Hypertension was observed in 394 participants (66.2%), which included 156 men and 238 women. Among the individuals with hypertension, 41 men (26.3%) and 49 women (20.6%) were unaware of their hypertension, while 115 men and 189 women had been diagnosed with hypertension. Uncontrolled hypertension was observed in 84 men (53.8%) and 129 women (54.2%), and controlled hypertension was observed in 72 men and 109 women (Table 1).
Table 1. Characteristics of the 595 participants.
| Variables | Men (n = 250) | Women (n = 345) | ||
| Hypertension present | ||||
| No | 94 (37.6%) | 107 (31.1%) | ||
| Yes | 156 (62.4%) | 238 (68.9%) | ||
| Awareness of hypertension | ||||
| Unaware | 41 (26.3%) | 49 (20.6%) | ||
| Aware | 115 (73.7%) | 189 (79.4%) | ||
| Control of hypertension | ||||
| Uncontrolled | 84 (53.8%) | 129 (54.2%) | ||
| Controlled | 72 (46.2%) | 109 (45.8%) | ||
| Age, yrs | 71.9 ± 6.5 | 70.6 ± 7.8 | ||
| Currently working | 198 (79.2%) | 221 (64.1%) | ||
| Education | ||||
| None | 33 (13.2%) | 144 (41.7%) | ||
| ≤ 6 yrs | 114 (45.6%) | 144 (41.7%) | ||
| > 6 yrs | 103 (41.2%) | 57 (16.5%) | ||
| Body mass index | ||||
| < 23.0 kg/m2 | 108 (43.2%) | 121 (35.1%) | ||
| ≥ 23.0 kg/m2 | 142 (56.8%) | 224 (64.9%) | ||
| Diagnosed diabetes | 52 (20.8%) | 58 (16.5%) | ||
| Current smoker | 70 (28.0%) | 8 (2.3%) | ||
| Alcohol consumption | 148 (59.2%) | 59 (17.1%) | ||
| Blood pressure check-up at least once per month | 150 (60.0%) | 213 (61.7%) | ||
| Instrumental support | ||||
| From family | 141 (43.6%) | 246 (71.3%) | ||
| From friends | 88 (35.2%) | 138 (40.0%) | ||
| Emotional support | ||||
| From family | 191 (76.4%) | 288 (83.5%) | ||
| From friends | 160 (64.0%) | 224 (64.9%) | ||
| No. of individuals in social network | 3.50 ± 1.14 | 3.16 ± 1.11 | ||
| Density | ||||
| Coarse network | 93 (37.2%) | 146 (42.3%) | ||
| Dense network | 157 (62.8%) | 199 (57.8%) | ||
Data are expressed as mean ± SD or n (%).
3.2. Risk for hypertension
Table 2 showed the results for the risk for hypertension among older men according to their socio-demographic, health, and social network characteristics. Among older men, hypertension was associated with a high BMI (OR: 1.88, 95% CI: 1.04–3.39) and consuming alcohol (OR: 2.08, 95% CI: 1.16–3.76). Compared to participants without hypertension, participants with hypertension were more likely to have a small social network (OR: 0.75, 95% CI: 0.58–0.96).
Table 2. Factors associated with hypertension prevalence and awareness.
| Hypertension prevalence (n = 595) |
Hypertension awareness (n = 394) |
||||||||||||||
| Men (n = 250) |
Women (n = 345) |
Men (n = 156) |
Women (n = 238) |
||||||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||||
| Age, yrs | 1.05 | (1.00–1.10) | 0.050 | 1.10 | (1.06–1.16) | < 0.001 | 1.05 | (0.98–1.14) | 0.167 | 1.05 | (0.99–1.13) | 0.116 | |||
| Currently working | 1.27 | (0.62–2.61) | 0.520 | 0.60 | (0.35–1.04) | 0.070 | 2.21 | (0.67–7.29) | 0.193 | 0.55 | (0.23–1.27) | 0.159 | |||
| Education (reference: none) | |||||||||||||||
| ≤ 6 yrs | 1.01 | (0.42–2.44) | 0.982 | 1.68 | (0.84–3.14) | 0.106 | 0.59 | (0.13–2.61) | 0.96 | (0.37–2.47) | 0.925 | ||||
| > 6 yrs | 1.43 | (0.57–3.63) | 0.448 | 1.18 | (0.45–2.78) | 0.699 | 0.57 | (0.12–2.68) | 0.479 | 1.80 | (0.41–7.97) | 0.437 | |||
| Body mass index | |||||||||||||||
| < 23.0 kg/m2 | |||||||||||||||
| ≥ 23.0 kg/m2 | 1.88 | (1.04–3.39) | 0.036 | 2.12 | (1.26–3.57) | 0.005 | 0.84 | (0.31–2.26) | 0.735 | 1.54 | (0.68–3.49) | 0.298 | |||
| Current smoker | 0.69 | (0.37–1.29) | 0.247 | 0.64 | (0.23–1.81) | 0.402 | |||||||||
| Alcohol consumption | 2.08 | (1.16–3.76) | 0.015 | 0.47 | (0.25–0.86) | 0.017 | 0.85 | (0.32–2.25) | 0.736 | 0.58 | (0.21–1.62) | 0.298 | |||
| Blood pressure check-up atleast once per month | 8.25 | (3.15–21.6) | < 0.001 | 11.57 | (5.00–26.8) | < 0.001 | |||||||||
| Diagnosed diabetes | 0.83 | (0.40–1.72) | 0.616 | 1.44 | (0.71–2.73) | 0.310 | 4.96 | (1.21–20.4) | 0.026 | 3.53 | (0.89–14.0) | 0.078 | |||
| Instrumental support from family | 1.37 | (0.66–2.88) | 0.399 | 1.35 | (0.67–2.73) | 0.409 | 2.29 | (0.67–7.77) | 0.184 | 6.08 | (2.01–18.41) | 0.001 | |||
| Instrumental support from friends | 0.73 | (0.37–1.46) | 0.378 | 0.91 | (0.49–1.70) | 0.782 | 2.13 | (0.65–6.98) | 0.211 | 0.70 | (0.26–1.92) | 0.493 | |||
| Emotional support from family | 0.73 | (0.30–1.78) | 0.484 | 0.40 | (0.16–1.02) | 0.054 | 0.84 | (0.21–3.32) | 0.800 | 0.29 | (0.07–1.11) | 0.070 | |||
| Emotional support from friends | 0.57 | (0.28–1.19) | 0.136 | 1.22 | (0.62–2.38) | 0.576 | 0.68 | (0.24–1.95) | 0.471 | 0.75 | (0.25–2.25) | 0.612 | |||
| No. of individuals in social network | 0.75 | (0.58–0.96) | 0.020 | 1.00 | (0.78–1.28) | 0.998 | 0.84 | (0.56–1.26) | 0.392 | 0.89 | (0.62–1.29) | 0.537 | |||
| Density | 0.90 | (0.50–1.64) | 0.738 | 0.84 | (0.49–1.46) | 0.545 | 0.37 | (0.14–0.95) | 0.039 | 2.36 | (1.03–5.37) | 0.042 | |||
Among older women, hypertension was associated with older age (OR: 1.10, 95% CI: 1.06–1.16) and a BMI of ≥ 23 kg/m2 (OR: 2.12, 95% CI: 1.26–3.57). Consuming alcohol was associated with a reduced risk for hypertension (OR: 0.47, 95% CI: 0.25–0.86). The risk for hypertension was not significantly associated with education level, diabetes, emotional support, instrumental support, network size, or network density.
3.3. Hypertension awareness
Older men with diabetes were more likely to be aware of their hypertension (OR: 4.96, 95% CI: 1.21–20.35). In addition, older men who checked their blood pressure at least once per month were more likely to be aware of their hypertension (OR: 8.25, 95% CI: 3.15–21.62). Older men with dense networks were less likely to be aware of their hypertension (OR: 0.37, 95% CI: 0.14–0.95), Table 2.
Among older women, checking blood pressure at least once per month was associated with hypertension awareness (OR: 11.57, 95% CI: 5.00–26.77). Instrumental support from friends was positively associated with hypertension awareness (OR: 6.08, 95% CI: 2.01–18.41). Older women with a dense network were more likely to be aware of their hypertension (OR: 2.36, 95% CI: 1.03–5.37), Table 2.
3.4. Hypertension control
Table 3 presented the results of logistic regression analyses examining the association of socio-demographic, health, and social network characteristics and hypertension control. Older men who checked their blood pressure at least once per month were more likely to maintain blood pressure control (OR: 6.18, 95% CI: 2.44–15.7). Instrumental support from friends was positively associated with hypertension control (OR: 3.02, 95% CI: 1.09–8.35), and network density significantly affected hypertension control (OR: 0.42, 95% CI: 0.19–0.91). Older men with a coarse network were more likely to have controlled hypertension. In model 2, the interaction term for network size and density also indicated that the association between network size and controlled hypertension varied according to network density (P = 0.051).
Table 3. Factors associated with hypertension control.
| Men (n = 156) |
Women (n = 238) |
||||||||||||
| Model 1 |
Model 2 |
Model 1 |
Model 2 |
||||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Age, yrs | 1.01 | (0.94–1.07) | 0.855 | 1.01 | (0.94–1.07) | 0.856 | 1.01 | (0.96–1.06) | 0.693 | 1.01 | (0.96–1.06) | 0.662 | |
| Currently working | 1.62 | (0.66–4.00) | 0.294 | 1.57 | (0.63–3.92) | 0.329 | 1.28 | (0.69–2.37) | 0.440 | 1.28 | (0.69–2.38) | 0.434 | |
| Education (reference: none) | |||||||||||||
| ≤ 6 yrs | 0.58 | (0.18–1.82) | 0.346 | 0.55 | (0.17–1.74) | 0.306 | 1.64 | (0.84–3.20) | 0.150 | 1.64 | (0.84–3.20) | 0.150 | |
| > 6 yrs | 0.45 | (0.14–1.51) | 0.197 | 0.46 | (0.14–1.57) | 0.216 | 2.81 | (0.96–8.23) | 0.060 | 2.81 | (0.96–8.24) | 0.060 | |
| Body mass index | |||||||||||||
| < 23.0 kg/m2 | |||||||||||||
| ≥ 23.0 kg/m2 | 0.72 | (0.32–1.64) | 0.438 | 0.73 | (0.32–1.68) | 0.454 | 1.12 | (0.61–2.05) | 0.715 | 1.11 | (0.61–2.03) | 0.735 | |
| Current smoker | 0.66 | (0.27–1.65) | 0.376 | 0.67 | (0.26–1.67) | 0.386 | |||||||
| Alcohol consumption | 0.52 | (0.23–1.19) | 0.119 | 0.49 | (0.21–1.13) | 0.092 | 1.41 | (0.65–3.04) | 0.385 | 1.41 | (0.65–3.05) | 0.384 | |
| Blood pressure check-up at least once per month | 6.18 | (2.44–15.7) | < 0.001 | 6.77 | (2.61–17.52) | < 0.001 | 2.26 | (1.18–4.32) | 0.014 | 2.23 | (1.16–4.29) | 0.016 | |
| Diagnosed diabetes | 1.98 | (0.39–2.48) | 0.962 | 1.13 | (0.43–2.98) | 0.798 | 0.96 | (0.46–2.01) | 0.919 | 0.98 | (0.47–2.05) | 0.953 | |
| Instrumental support from family | 0.96 | (0.33–2.77) | 0.935 | 0.82 | (0.28–2.40) | 0.710 | 1.20 | (0.52–2.77) | 0.664 | 1.20 | (0.52–2.75) | 0.673 | |
| Instrumental support from friends | 3.01 | (1.09–8.35) | 0.034 | 2.73 | (0.96–7.75) | 0.059 | 1.42 | (0.71–2.83) | 0.324 | 1.39 | (0.70–2.79) | 0.351 | |
| Emotional support from family | 0.70 | (0.22–2.22) | 0.541 | 0.81 | (0.25–2.64) | 0.731 | 0.53 | (0.20–1.44) | 0.213 | 0.53 | (0.20–1.44) | 0.214 | |
| Emotional support from friends | 0.87 | (0.36–2.14) | 0.766 | 1.05 | (0.42–2.64) | 0.918 | 0.85 | (0.40–1.80) | 0.675 | 0.87 | (0.41–1.84) | 0.710 | |
| [1] No. of individuals in social network | 1.14 | (0.81–1.62) | 0.457 | 1.90 | (1.00–3.61) | 0.050 | 1.02 | (0.78–1.32) | 0.911 | 0.92 | (0.63–1.36) | 0.690 | |
| [2] Density | 0.42 | (0.19–0.91) | 0.027 | 5.77 | (0.38–87.2) | 0.206 | 1.72 | (0.94–3.13) | 0.077 | 0.99 | (0.17–5.77) | 0.995 | |
| [1] × [2] | 0.46 | (0.21–1.00) | 0.051 | 1.18 | (0.71–1.98) | 0.518 | |||||||
Older women who checked their blood pressure at least once per month were more likely to have controlled hypertension (OR: 2.23, 95% CI: 1.16–4.29). The number of individuals in the discussion network was not significantly related to hypertension control. However, older women with a dense network were more likely to have controlled hypertension at the 90% significance level (OR: 1.72, 90% CI: 0.94–3.13).
In supplemental analyses, hypertension control was defined as an average SBP of < 130 mmHg and an average SBP < 80 mmHg for the respondents who reported that they had been diagnosed with diabetes. The results are not included in the tables presented here but could be found in online data Table S1.
Table S1. Factors associated with hypertension control1) among older adults.
| Men (n = 156) |
Women (n = 238) |
||||||||||||
| Model 1 |
Model 2 |
Model 1 |
Model 1 |
||||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Age, yrs | 1.00 | (0.94–1.07) | 0.975 | 1.00 | (0.93–1.07) | 0.958 | 1.01 | (0.96–1.06) | 0.740 | 1.01 | (0.96–1.06) | 0.704 | |
| Currently working | 1.81 | (0.72–4.54) | 0.205 | 1.77 | (0.70–4.48) | 0.228 | 1.32 | (0.70–2.48) | 0.397 | 1.32 | (0.70–2.49) | 0.391 | |
| Education (reference: none) | . | . | |||||||||||
| ≤ 6 years | 0.61 | (0.20–1.90) | 0.394 | 0.60 | (0.19–1.89) | 0.384 | 1.74 | (0.87–3.49) | 0.115 | 1.74 | (0.87–3.49) | 0.116 | |
| > 6 years | 0.48 | (0.15–1.59) | 0.229 | 0.52 | (0.15–1.74) | 0.285 | 2.70 | (0.91–8.03) | 0.075 | 2.70 | (0.90–8.08) | 0.075 | |
| Body mass index | |||||||||||||
| < 23.0 kg/m2 | |||||||||||||
| ≥ 23.0 kg/m2 | 0.82 | (0.36–1.87) | 0.643 | 0.86 | (0.37–1.98) | 0.722 | 0.99 | (0.53–1.83) | 0.974 | 0.98 | (0.53–1.82) | 0.957 | |
| Current smoker | 0.79 | (0.32–1.96) | 0.610 | 0.80 | (0.32–2.03) | 0.642 | |||||||
| Alcohol consumption | 0.43 | (0.19–1.00) | 0.049 | 0.41 | (0.17–0.95) | 0.038 | 1.23 | (0.57–2.67) | 0.598 | 1.23 | (0.57–2.67) | 0.598 | |
| Blood pressure check-up at least once per month | 5.44 | (2.13–13.9) | < 0.001 | 5.83 | (2.26–15.1) | < 0.001 | 2.56 | (1.31–5.02) | 0.006 | 2.54 | (1.29–5.00) | 0.007 | |
| Diagnosed diabetes | 0.45 | (0.17–1.19) | 0.107 | 0.49 | (0.18–1.33) | 0.161 | 0.33# | (0.14–0.76) | 0.009 | 0.33 | (0.15–0.77) | 0.010 | |
| Instrumental support from family | 1.00 | (0.34–2.94) | 0.999 | 0.85 | (0.28–2.55) | 0.771 | 1.15 | (0.49–2.71) | 0.753 | 1.15 | (0.49–2.71) | 0.756 | |
| Instrumental support from friends | 2.79 | (1.02–7.64) | 0.045 | 2.50 | (0.89–6.99) | 0.082 | 1.45 | (0.71–2.96) | 0.306 | 1.42 | (0.70–2.91) | 0.334 | |
| Emotional support from family | 0.59 | (0.18–1.92) | 0.379 | 0.69 | (0.21–2.32) | 0.552 | 0.56 | (0.20–1.56) | 0.269 | 0.56 | (0.20–1.56) | 0.268 | |
| Emotional support from friends | 1.07 | (0.44–2.61) | 0.886 | 1.27 | (0.50–3.19) | 0.617 | 0.93 | (0.43–2.01) | 0.849 | 0.95 | (0.43–2.06) | 0.891 | |
| [1] No. of individuals in social network | 1.09 | (0.77–1.53) | 0.630 | 1.68 | (0.94–3.02) | 0.081 | 1.04 | (0.79–1.35) | 0.790 | 0.94 | (0.63–1.40) | 0.765 | |
| [2] Density | 0.50 | (0.23–1.07) | 0.074 | 5.83 | (0.41–82.2) | 0.192 | 0.69 | (0.91–3.13) | 0.097 | 0.96 | (0.16–5.75) | 0.965 | |
| [1] × [2] | 0.48 | (0.23–1.03) | 0.059 | 1.19 | (0.71–2.00) | 0.512 | |||||||
1)Hypertension control was classified as an average systolic blood pressure of < 140 mmHg and an average diastolic blood pressure of < 90 mmHg (for patients with diabetes: an average systolic blood pressure of < 130 mmHg and an average diastolic blood pressure of <80 mmHg).
4. Discussion
This study investigated the effects of social network characteristics on hypertension management among older Korean adults. We found strong sex-specific network effects on the prevalence, awareness, and control of hypertension. For example, men with a large and coarse network tended to have better hypertension management, and women with a dense network had better hypertension management.
We had anticipated that a large network would reduce the risk for uncontrolled or previously unidentified hypertension, although we only observed this relationship among older men. The effect of network size can be explained through three mechanisms: improving health-related behaviors, maintaining psychological health, and satisfaction with one's life promoting health. As physical and mental capabilities deteriorate with age, health status is related to a willingness to maintain health and to perform positive health-related behaviors. Therefore, social relationships can promote self-esteem and self-confidence among older adults, although different relationships and activities have varied effects on the aging population.[27],[28]
Social network size and density were relevant for hypertension management. In the present study, older men with large and coarse networks exhibited a greater likelihood of having controlled hypertension, compared to men with a small and dense network. This finding indicates that men with a large and coarse network were more likely to personally control their health, compared to men with a highly dense network. We believe that large and coarse networks of individuals from diverse backgrounds might provide older men with better information and greater social prestige. In this context, older men tend to focus on shared activities, rather than relational support from close friendships.[29] Thus, establishing intimate relationships throughout various social network increases pride among men, which would increase motivation to preserve their appearance and health, and might actually improve their health.
Among women, our results indicate that network characteristics also affected hypertension management. Although the social network characteristics were not associated with the prevalence of hypertension, we found that individual characteristics, such as older age and obesity, were risk factors for an increased prevalence of hypertension. Interestingly, the effects of network density on hypertension management among women highlight the sex-specific effects of social network characteristics on hypertension. For example, network density is relevant among older women, regardless of network size, as network density was associated with better hypertension awareness. Older women with a dense network also seemed to have the best hypertension management. Therefore, we believe that older women receive important emotional, instrumental, and information support through dense networks. These results suggest that women likely rely on their social network for emotional, instrumental, and information support.[30] Compared to men, women invest more time and energy in creating intimate interpersonal relationships,[24] and place more emphasis on confiding, reassuring, and talking to the members of their network.[31] Thus, a dense network likely provides a greater positive effect on health among women, compared to the effect among men.
However, this study also has several limitations. First, this study used data from a community-based survey, which are not representative of the entire Korean population. Second, blood pressure was only measured only in the clinical testing, as ambulatory or home blood pressure monitoring was not available. Thus, we could not control for the potential effects of white-coat hypertension or masked hypertension. Third, there is a possibility of reverse causality because of the data's cross-sectional nature (i.e., differences in network types may arise from health status). However, sex-specific differences in the association between social networks and hypertension management still exist in the reverse causal relationship.
The findings of this study indicate that sex-specific characteristics of social networks might be used to help to prevent, detect, and control hypertension among older adults. Therefore, future studies are needed to provide additional sex-specific data regarding hypertension-related behaviors, which can faciliate the development of sex-specific prevention strategies.
Acknowledgments
This study was supported by a grant from the National Research Foundation of Korea (NRF-2014S1A3A2044496). The authors declare that there are no conflicts of interest regarding this study.
References
- 1.Kim HJ, Kim Y, Cho Y, et al. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: Results from the Korea National Health and Nutrition Examination Survey, 1998–2012. Int J Cardiol. 2014;174:64–72. doi: 10.1016/j.ijcard.2014.03.163. [DOI] [PubMed] [Google Scholar]
- 2.Korea health statistics 2013: Korea National Health and Nutritional Examination Survey (KNHANES VI-1) 53–54. Cheongju, South Korea: Korea Centers for Disease Control and Prevention; 2014. pp. 572–579. [Google Scholar]
- 3.Neaton JD, Grimm RH, Prineas RJ, et al. Treatment of mild hypertension study: final results. JAMA. 1993;270:713–724. [PubMed] [Google Scholar]
- 4.Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: Analysis of nationwide data 2003–2012. Int J Cardiol. 2015;184:637–644. doi: 10.1016/j.ijcard.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 5.Marques-Vidal P, Tuomilehto J. Hypertension awareness, treatment and control in the community: is the ‘rule of halves’ still valid? J Hypertens. 1997;11:213–220. doi: 10.1038/sj.jhh.1000426. [DOI] [PubMed] [Google Scholar]
- 6.Group UPDS Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–713. [PMC free article] [PubMed] [Google Scholar]
- 7.Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861–869. doi: 10.1056/NEJMoa011161. [DOI] [PubMed] [Google Scholar]
- 8.Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. The Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 9.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 10.Redwood H. Hypertension, society, and public policy. Eur Heart J Suppl. 2007;9:B13–B18. [Google Scholar]
- 11.Hughes BM, Howard S. Social support reduces resting cardiovascular function in women. Anxiety Stress Coping. 2009;22:537–548. doi: 10.1080/10615800902814614. [DOI] [PubMed] [Google Scholar]
- 12.Li G, Hu H, Dong Z, Arao T. Development of the Chinese Family Support Scale in a Sample of Chinese Patients with Hypertension. PLoS ONE. 2013;8:e85682. doi: 10.1371/journal.pone.0085682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Räikkönen K, Matthews KA, Kuller LH. Trajectory of psychological risk and incident hypertension in middle-aged women. Hypertension. 2001;38:798–802. [PubMed] [Google Scholar]
- 14.Berkman LF. Social network analysis and coronary heart disease. Adv Cardiol. 1981;29:37–49. doi: 10.1159/000406195. [DOI] [PubMed] [Google Scholar]
- 15.de Leon CFM, Glass TA, Berkman LF. Social engagement and disability in a community population of older adults. Am J Epidemiol. 2003;157:633–642. doi: 10.1093/aje/kwg028. [DOI] [PubMed] [Google Scholar]
- 16.Horwitz SM, Prados-Torres A, Singer B, Bruce ML. The influence of psychological and social factors on accuracy of self-reported blood pressure. J Clin Epidemiol. 1997;50:411–418. doi: 10.1016/s0895-4356(96)00427-1. [DOI] [PubMed] [Google Scholar]
- 17.Vogt TM, Mullooly JP, Ernst D, et al. Social networks as predictors of ischemic heart disease, cancer, stroke and hypertension: incidence, survival and mortality. J Clin Epidemiol. 1992;45:659–666. doi: 10.1016/0895-4356(92)90138-d. [DOI] [PubMed] [Google Scholar]
- 18.Cornwell EY, Waite LJ. Social network resources and management of hypertension. J Health Soc Behav. 2012;53:215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Youm Y, Laumann EO, Ferraro KF, et al. Social network properties and self-rated health in later life: comparisons from the Korean social life, health, and aging project and the national social life, health and aging project. Bmc Geriatr. 2014:14. doi: 10.1186/1471-2318-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JM, Lee WJ, Kim HC, et al. The korean social life, health and aging project-health examination cohort. Epidemiol Health. 2014;36:e2014003. doi: 10.4178/epih/e2014003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chu SH, Baek JW, Kim ES, et al. Gender differences in hypertension control among older Korean adults: Korean social life, health, and aging project. J Prev Med Pub Health. 2015;48:38–47. doi: 10.3961/jpmph.14.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xi B, Liang Y, Reilly KH, et al. Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol. 2012;158:326–329. doi: 10.1016/j.ijcard.2012.04.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cornwell B, Schumm LP, Laumann EO, Graber J. Social Networks in the NSHAP Study: rationale, measurement, and preliminary findings. J Gerontol B Psychol Sci Soc Sci. 2009;64(suppl 1):S47–S55. doi: 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hirsch BJ. Psychological dimensions of social networks: A multimethod analysis. Am J Community Psychol. 1979;7:263–277. [Google Scholar]
- 25.Hirsch BJ. Natural support systems and coping with major life changes. American Am J Community Psychol. 1980;8:159–172. [Google Scholar]
- 26.Stokes JP. Predicting satisfaction with social support from social network structure. Am J Community Psychol. 1983;11:141–152. [Google Scholar]
- 27.Longino CF, Kart CS. Explicating activity theory: A formal replication. J Gerontol. 1982;37:713–722. doi: 10.1093/geronj/37.6.713. [DOI] [PubMed] [Google Scholar]
- 28.Menec VH. The relation between everyday activities and successful aging: A 6-year longitudinal study. J Gerontol B Psychol Sci Soc Sci. 2003;58:S74–S82. doi: 10.1093/geronb/58.2.s74. [DOI] [PubMed] [Google Scholar]
- 29.Haines VA, Beggs JJ, Hurlbert JS. Contextualizing Health outcomes: do effects of network structure differ for women and men? Sex Roles. 2008;59:164–175. [Google Scholar]
- 30.Fiori KL, Denckla CA. Social support and mental health in middle-aged men and women a multidimensional approach. J Aging Health. 2012;24:407–438. doi: 10.1177/0898264311425087. [DOI] [PubMed] [Google Scholar]
- 31.Shye D, Mullooly JP, Freeborn DK, Pope CR. Gender differences in the relationship between social network support and mortality: a longitudinal study of an elderly cohort. Soc Sci Med. 1995;41:935–947. doi: 10.1016/0277-9536(94)00404-h. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Factors associated with hypertension control1) among older adults.
| Men (n = 156) |
Women (n = 238) |
||||||||||||
| Model 1 |
Model 2 |
Model 1 |
Model 1 |
||||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Age, yrs | 1.00 | (0.94–1.07) | 0.975 | 1.00 | (0.93–1.07) | 0.958 | 1.01 | (0.96–1.06) | 0.740 | 1.01 | (0.96–1.06) | 0.704 | |
| Currently working | 1.81 | (0.72–4.54) | 0.205 | 1.77 | (0.70–4.48) | 0.228 | 1.32 | (0.70–2.48) | 0.397 | 1.32 | (0.70–2.49) | 0.391 | |
| Education (reference: none) | . | . | |||||||||||
| ≤ 6 years | 0.61 | (0.20–1.90) | 0.394 | 0.60 | (0.19–1.89) | 0.384 | 1.74 | (0.87–3.49) | 0.115 | 1.74 | (0.87–3.49) | 0.116 | |
| > 6 years | 0.48 | (0.15–1.59) | 0.229 | 0.52 | (0.15–1.74) | 0.285 | 2.70 | (0.91–8.03) | 0.075 | 2.70 | (0.90–8.08) | 0.075 | |
| Body mass index | |||||||||||||
| < 23.0 kg/m2 | |||||||||||||
| ≥ 23.0 kg/m2 | 0.82 | (0.36–1.87) | 0.643 | 0.86 | (0.37–1.98) | 0.722 | 0.99 | (0.53–1.83) | 0.974 | 0.98 | (0.53–1.82) | 0.957 | |
| Current smoker | 0.79 | (0.32–1.96) | 0.610 | 0.80 | (0.32–2.03) | 0.642 | |||||||
| Alcohol consumption | 0.43 | (0.19–1.00) | 0.049 | 0.41 | (0.17–0.95) | 0.038 | 1.23 | (0.57–2.67) | 0.598 | 1.23 | (0.57–2.67) | 0.598 | |
| Blood pressure check-up at least once per month | 5.44 | (2.13–13.9) | < 0.001 | 5.83 | (2.26–15.1) | < 0.001 | 2.56 | (1.31–5.02) | 0.006 | 2.54 | (1.29–5.00) | 0.007 | |
| Diagnosed diabetes | 0.45 | (0.17–1.19) | 0.107 | 0.49 | (0.18–1.33) | 0.161 | 0.33# | (0.14–0.76) | 0.009 | 0.33 | (0.15–0.77) | 0.010 | |
| Instrumental support from family | 1.00 | (0.34–2.94) | 0.999 | 0.85 | (0.28–2.55) | 0.771 | 1.15 | (0.49–2.71) | 0.753 | 1.15 | (0.49–2.71) | 0.756 | |
| Instrumental support from friends | 2.79 | (1.02–7.64) | 0.045 | 2.50 | (0.89–6.99) | 0.082 | 1.45 | (0.71–2.96) | 0.306 | 1.42 | (0.70–2.91) | 0.334 | |
| Emotional support from family | 0.59 | (0.18–1.92) | 0.379 | 0.69 | (0.21–2.32) | 0.552 | 0.56 | (0.20–1.56) | 0.269 | 0.56 | (0.20–1.56) | 0.268 | |
| Emotional support from friends | 1.07 | (0.44–2.61) | 0.886 | 1.27 | (0.50–3.19) | 0.617 | 0.93 | (0.43–2.01) | 0.849 | 0.95 | (0.43–2.06) | 0.891 | |
| [1] No. of individuals in social network | 1.09 | (0.77–1.53) | 0.630 | 1.68 | (0.94–3.02) | 0.081 | 1.04 | (0.79–1.35) | 0.790 | 0.94 | (0.63–1.40) | 0.765 | |
| [2] Density | 0.50 | (0.23–1.07) | 0.074 | 5.83 | (0.41–82.2) | 0.192 | 0.69 | (0.91–3.13) | 0.097 | 0.96 | (0.16–5.75) | 0.965 | |
| [1] × [2] | 0.48 | (0.23–1.03) | 0.059 | 1.19 | (0.71–2.00) | 0.512 | |||||||
1)Hypertension control was classified as an average systolic blood pressure of < 140 mmHg and an average diastolic blood pressure of < 90 mmHg (for patients with diabetes: an average systolic blood pressure of < 130 mmHg and an average diastolic blood pressure of <80 mmHg).


