Abstract
Background
Following the adoption of the Millennium Development Goal 4 (MDG 4) in Ghana to reduce under-five mortality by two-thirds between 1990 and 2015, efforts were made towards its attainment. However, impacts and challenges of implemented intervention programs have not been examined to inform implementation of Sustainable Development Goal 3.2 (SDG 3.2) that seeks to end preventable deaths of newborns and children aged under-five. Thus, this study aimed to compare trends in neonatal, infant, and under-five mortality over two decades and to highlight the impacts and challenges of health policies and intervention programs implemented.
Design
Ghana Demographic and Health Survey data (1988–2008) were analyzed using trend analysis. Poisson regression analysis was applied to quantify the incidence rate ratio of the trends. Implemented health policies and intervention programs to reduce childhood mortality in Ghana were reviewed to identify their impact and challenges.
Results
Since 1988, the annual average rate of decline in neonatal, infant, and under-five mortality in Ghana was 0.6, 1.0, and 1.2%, respectively. From 1988 to 1989, neonatal, infant, and under-five mortality declined from 48 to 33 per 1,000, 72 to 58 per 1,000, and 108 to 83 per 1,000, respectively, whereas from 1989 to 2008, neonatal mortality increased by 2 per 1,000 while infant and under-five mortality further declined by 6 per 1,000 and 17 per 1,000, respectively. However, the observed declines were not statistically significant except for under-five mortality; thus, the proportion of infant and under-five mortality attributed to neonatal death has increased. Most intervention programs implemented to address childhood mortality seem not to have been implemented comprehensively.
Conclusion
Progress towards attaining MDG 4 in Ghana was below the targeted rate, particularly for neonatal mortality as most health policies and programs targeted infant and under-five mortality. Implementing neonatal-specific interventions and improving existing programs will be essential to attain SDG 3.2 in Ghana and beyond.
Keywords: neonatal, infant, under-five mortality, Ghana
Introduction
Early childhood mortality continues to remain a prominent global health issue even though Millennium Development Goal 4 (MDG 4) was universally adopted to reduce under-five mortality by two-thirds between 1990 and 2015 (1). Also, several ‘calls for action’ to reduce neonatal mortality have been made (2–5), and in response, both governmental and non-governmental bodies have committed considerable resources to this public health challenge. Similar to other low- and middle-income countries (LMICs), post-adoption of MDG 4 in Ghana has witnessed formulation and implementation of maternal and child health policies and intervention programs towards actualizing MDG 4. For example, from 1988 to 1998, the Safe Motherhood Program (SMP) (6), Life Saving Skills (LSS) program (7), and Integrated Management of Childhood Illness (IMCI) program (8) were initiated. The SMP aims to secure safe delivery for women and improve child health services while the LSS (7) seeks to sharpen the clinical skills of midwives. Similarly, the IMCI (8) targets to improve child survival through the provision of clinical guidelines for management of childhood illnesses, health system strengthening, and improving community health practices. In the subsequent decade, from 1998 to 2008, some additional intervention programs and policies implemented were the Community-Based Health Planning and Services (CHPS) (9), User Fees Exemption for Delivery (UFED) (10), Focused Antenatal Care (FANC) (11), and National Health Insurance Scheme (NHIS) (12). The CHPS program aims to bring healthcare closer to the people through primary health care service while the UFED (10) and NHIS programs seek to ease the financial burden of healthcare service and reduce inequality in healthcare uptake. The FANC pursues improvement in maternal and child survival through individualized antenatal care that entails a comprehensive assessment of pregnant women in terms of their socio-cultural beliefs, lifestyle, and medical characteristics to improve early detection and treatment of illness and pregnancy complications. In addition to these national programs and policies, various regions also implemented different intervention programs, for example, the Kybele program in the Greater Accra region (13, 14), Accelerated Child Survival and Development (ACSD) (15) sponsored by United Nation Children and Education Fund (UNICEF) in the Northern, Upper East, and Upper West regions, and Kangaroo Mother Care (KMC) (16) which commenced in six regions in 2007. Although the deadline for the attainment of MDG 4 has elapsed, 99% of childhood mortality still occurs in LMICs (5, 17), with Africa accounting for about 50% (18). Assessment of progress made so far is of utmost importance to inform policy makers and healthcare planners tasked to realize the newly adopted Sustainable Development Goal 3.2 (SDG 3.2) that seeks to end preventable deaths of newborns and under-five children by 2030.
Thus, this study aimed to 1) compare the temporal trends in neonatal, infant, and under-five mortality in Ghana from 1988 to 2008; 2) describe the trends in the proportion of infant and under-five mortality attributed to neonatal deaths in Ghana over the same period; 3) compare national and regional trends in neonatal mortality over the same period; and 4) identify the impact and challenges of health policies and intervention programs implemented in Ghana during this time period.
Methods
Setting
Ghana is located in sub-Saharan Africa, along the Gulf of Guinea with a total population of about 24.4 million (19). It has an annual growth rate of about 2.4% per year (20). Ghana has 10 administrative regions, namely Greater Accra, Western, Central, Volta, Eastern, Ashanti, Brong-Ahafo, Northern, Upper East, and Upper West. It has about 100 ethnic groups with different languages but the major ethnic groups are Akan, Ewe, Mole-Dagbane, Guan, and Ga-Adangbe (21).
Design of data collection
This longitudinal study compared the trends in neonatal mortality, infant and under-five mortality, and described the trends in the proportion of infant and under-five mortality attributed to neonatal deaths in Ghana, from 1988 to 2008, using Ghana Demographic and Health Survey (GDHS) datasets obtained in 1988, 1993, 1998, 2003, and 2008 (22). These datasets were collected by the ICF Macro in conjunction with the Ghana Statistical Service and the Ministry of Health/Ghana Health Service. All the GDHSs followed the same sampling technique; households were randomly sampled for interview by applying a stratified, two-stage cluster random sampling technique. All women and men in all the selected households, within the age range 15–49 and 15–59 years, respectively, were targeted for face-to-face interview using questionnaires. Prior to the interview, informed consent was obtained from every participant. The datasets are nationally representative with an individual response rate of 95–97% and a household response rate of 97–99%. The datasets were weighted to have a better representation of the study population. In GDHS, neonatal mortality was defined as the probability of dying within the first month of life, infant mortality was defined as the probability of dying before the age of 12 months, and under-five mortality was defined as the probability of dying before the age of 60 months. Detailed information on the sampling techniques and procedures for the data collection has been published elsewhere (22). In order to highlight the impact and challenges of health policies and intervention programs implemented in Ghana from 1988 to 2008, MEDLINE, EMBASE, Google Scholar, African Index Medicus, and Ghana Medical Journal were searched, and the articles that assessed the impact and challenges of these interventions implemented from 1988 to 2008 in Ghana were identified and reviewed.
Statistical analysis
Neonatal, infant, and under-five mortality rates estimated at national and regional level from each GDHS were used to perform trend analysis. Temporal trend patterns were depicted by plotting the number of neonatal deaths per 1,000 live births against the year when the data were captured; infant and under-five mortality underwent a similar analysis at national level. Also, temporal trend pattern of neonatal mortality at the national level was compared with that of regions. Likewise, the proportion of infant and under-five mortality attributed to neonatal mortality was examined by plotting the percentage of infant and under-five mortality attributed to neonatal death against the year when the data were captured. In order to quantify the trends objectively, a Poisson regression analysis was applied to quantify the incidence rate ratios of the trends. Statistical significance was determined by two-tailed Wald test at significant level of alpha equal to 5%; all analyses were performed in Stata statistical software package version 11 (23).
Ethical approval
Anonymous publicly available data were utilized in this study. Thus, no ethical approval is required.
Results
Descriptive statistics
Table 1 shows the total number of live births captured per each GDHS and the number of neonatal, infant, and under-five deaths. Over this period, five demographic and health surveys were conducted in Ghana for which a total of 16,474 live births (average 3,295 live births per GDHS) were captured. Total neonatal, infant, and under-five deaths captured over this period was 673 (average 135 deaths per GDHS), 1,013 (average 203 deaths per GDHS), and 1,378 (average 276 deaths per GDHS), respectively. The average rates of decline per year for neonatal, infant, and under-five mortality were 0.6, 1.0, and 2.1%, respectively.
Table 1.
Neonatal, infant, and under-five deaths, 1988–2008 Ghana Demographic and Health Survey
| Total live births | Neonatal deaths | Infant deaths | Under-five deaths | |
|---|---|---|---|---|
| GDHS | Number (n) | Number (rate) | Number (rate) | Number (rate) |
| GDHS 1988 | 4,136 | 198 (47.9) | 299 (72.3) | 446 (107.8) |
| GDHS 1993 | 2,204 | 94 (42.6) | 130 (59.0) | 148 (67.2) |
| GDHS 1998 | 3,298 | 109 (33.1) | 192 (58.2) | 272 (82.5) |
| GDHS 2003 | 3,844 | 166 (43.2) | 235 (61.1) | 314 (81.7) |
| GDHS 2008 | 2,992 | 106 (35.4) | 157 (52.5) | 198 (66.2) |
Average rate of decline per year: neonatal mortality 0.6%, infant mortality 1.0%, and under-five mortality 2.1%. GDHS: Ghana Demographic and Health Survey.
National trends in neonatal, infant, and under-five mortality
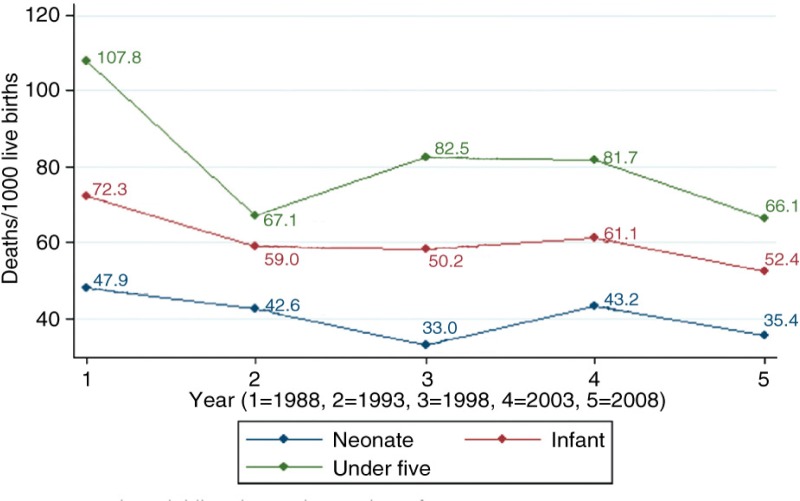
Figure 1 shows the trends in neonatal, infant, and under-five mortality from the 1988 to the 2008 GDHS while Table 2 reports the results of Poisson regression analysis that quantified the changes in the trends observed in Fig. 1. From 1988 to 1998, neonatal mortality declined from 47.9 per 1,000 to 33.1 per 1,000 and by 2008 neonatal mortality increased to 35.4 per 1,000. Considering the results in Table 2, neonatal mortality has not witnessed any significant decline over this period.
Fig. 1.
Trends in childhood mortality in Ghana from 1988 to 2008.
Table 2.
Poisson regression analyses of the trend in neonatal, infant, and under-five mortality, 1988–2008 Ghana Demographic and Health Survey
| Neonatal death | Infant death | Under-five death | |
|---|---|---|---|
| Year | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) |
| 1988 GDHS | 1 (reference) | 1 (reference) | 1 (reference) |
| 1993 GDHS | 0.90 (0.60–1.35) | 0.82 (0.58–1.15) | 0.62 (0.46–0.84)** |
| 1998 GDHS | 0.69 (0.44–1.07) | 0.81 (0.57–1.14) | 0.76 (0.57–1.01) |
| 2003 GDHS | 0.90 (0.59–1.35) | 0.85 (0.60–1.19) | 0.76 (0.57–1.01) |
| 2008 GDHS | 0.73 (0.47–1.12) | 0.72 (0.50–1.03) | 0.61 (0.45–0.83)** |
CI: confidence interval; GDHS: Ghana Demographic and Health Survey; IRR: incidence risk ratio;
p<0.01.
Infant mortality declined from 72.3 per 1,000 to 58.2 per 1,000 from 1988 to 1998 and by 2008 infant mortality dropped to 52.5 per 1,000. However, the results in Table 2 shows that the decline observed in infant mortality from 1988 to 2008 was not statistically significant. From 1988 to 1998, under-five mortality declined from 107.8 per 1,000 to 82.5 per 1,000 and by 2008 under-five mortality had further declined to 66.2 per 1,000. Over the same period, the results in Table 2 shows that under-five mortality was significantly lower in 1993 and 2008 when compared with 1988. In 1993 and 2008, the risk of under-five death was reduced by 38% (IRR=0.62; 95% CI: 0.46–0.84) and 39% (IRR=0.61; 95% CI: 0.45–0.83), respectively, when compared with that of 1988.
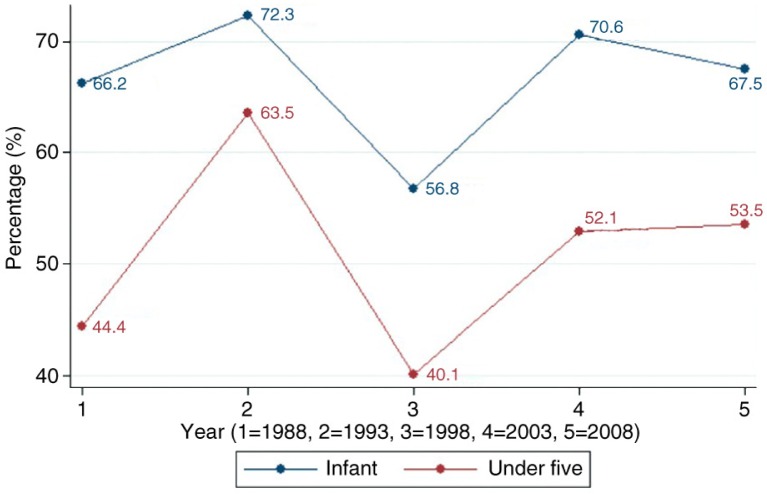
Figure 2 depicts the trends in the proportion of infant and under-five mortality attributable to neonatal deaths. From 1988 to 1998, the percentage of infant mortality attributed to neonatal mortality declined from 66 to 57%; however, by 2008, it increased to 67%. Likewise, from 1988 to 1998, the proportion of under-five mortality attributable to neonatal deaths reduced from 44 to 40%; however, by 2008 it increased to 53%.
Fig. 2.
Trends in proportion of infant and under-five mortality attributed to neonatal death.
Regional trends in neonatal mortality
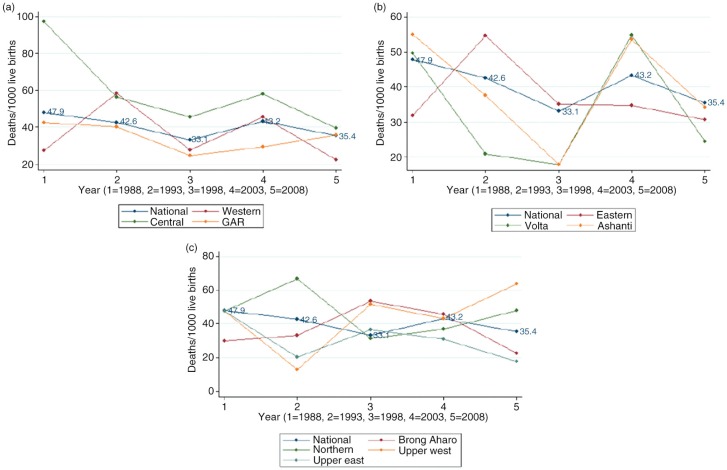
The regional trends of neonatal mortality are shown in Fig. 3. In 1988, neonatal mortality rates in the Central, Volta, and Ashanti regions were above the national rate (48 neonatal deaths per 1,000 live births); in 1998, Central, Eastern, Brong Ahafo, Upper East, and Upper West regions had a higher neonatal rate than the national average (33 neonatal deaths per 1,000 live births). By 2008 the Central, Upper West, and Northern regions exceeded the national neonatal mortality rate (35 neonatal deaths per 1,000 live births). The neonatal mortality in the Central region was persistently higher than the national average, whereas neonatal mortality in the Greater Accra region (GAR) stayed below the national average from 1988 to 2008.
Fig. 3.
National and regional trends in neonatal mortality in Ghana.
Impact of implemented health policies and intervention programs on MDG 4 in Ghana
Following the adoption of the MGDs in Ghana, the Ghanaian government in collaboration with international donors implemented several intervention programs and health policies aimed at accelerating attainment of MDG 4 and MDG 5 in Ghana. We examined the impact and limitations of national health policies that were implemented post-adoption of MDG 4 until 2008. Findings of studies that have assessed the policies quantitatively and/ or qualitatively have been summarized in Table 3. At the national level, the LSS (7), SMP (6), and IMCI (8) programs were initiated between 1988 and 1998 and subsequently scaled up thereafter.
Table 3.
Overview of National Health Policies implemented to address childhood mortality in Ghana from 1988 to 2008
| National Health policy | Activities | Time of assessment | Findings of studies assessing the effectiveness of national health policy programs |
|---|---|---|---|
| Safe Motherhood (6) Program (SMP) | Ghana SMP entails primary health care, antenatal care, essential obstetric care, clean/safe delivery, family planning and equity for women. (Launched in 1993 and scaled up in 2000.) | After scale-up | Okiwelu et al. showed that some donors were implementing other interventions outside the objectives of the SMP, and the authors concluded that such action might dilute the expected effect of the policy (35). |
| Anderson et al. identified migration of care providers (medical doctors) out of Ghana as one of the main factors that hampered the SMP in Ghana (36). | |||
| Maine et al. in his review on the SMP showed that the policy was not well-defined and most policy makers believed that most of the components of SMP were already implemented prior to the SMP (37). | |||
| Community-Based Health Planning and Services (9) (CHPS) | Community health officer (CHO) provides the following services: treatment of minor illness, health education, family planning, skilled delivery, and antenatal and postnatal care. Community volunteers are trained to carry out community mobilization. (First piloted in 1999, adopted nationwide in 2005.) | Prior to scale-up (experimental phase) | Prior to policy implementation at the national level, Phillips et al. showed that the CHPS program decreased childhood mortality and fertility rate (24). |
| Prior to scale-up | Prior to policy implementation at the national level, Debpuur et al. showed that the CHPS program increased women's knowledge of contraception, willingness for birth spacing, and usage of contraception (38). | ||
| Before the policy was adopted nationally, Pence et al. showed that the CHPS program decreased childhood mortality (39). | |||
| Before the CHPS program was adopted, Binka et al. found that the program decreased childhood mortality and improved parental health-seeking behavior (40). | |||
| Phillips et al. observed that CHPS improved contraceptive usage before the policy was adopted nationwide (41). | |||
| Prior to the adoption of the policy, Awoonor-Williams et al. showed that CHPS increased usage of contraception, skilled antenatal delivery, and postnatal attendants (42). | |||
| During scale up, | During the scale-up phase, Awoonor-Williams et al. observed the following challenges: inadequate funding, less preparedness of community health officer, inadequate community engagement, shortage of manpower and equipment and inadequate monitoring (31). | ||
| After the adoption of the policy | Assessment of the CHPS initiative by Adongo et al. after its adoption showed that the program improved the acceptance of family planning (43). | ||
| Following adoption of the CHPS, Adongo et al. observed that the implementation of the program in urban areas was difficult due to contextual differences between rural (where the CHPS was tested) and urban areas, suggesting further modification of the implementation strategies (44). | |||
| Post-adoption of CHPS initiative | During post-adoption of CHPS, Nyonator et al. identified the following: inadequate community engagement, lack of funds made health managers to perceive CHPS as an administrative burden (9). | ||
| User Fees Exemption for Delivery Care (UFEDC) (10) | Exemption for pregnant women from paying delivery fees in order to increase skilled delivery. Public, private, and mission health care providers were receiving reimbursement for service rendered (Initiated in 2003, scaled up in 2005) | Prior to scale up | Before the policy was adopted, Asante et al. reported that the policy decreased catastrophic out-of-pocket payment (45). Before the policy was scaled up, Bosu et al. showed that the policy had no statistically significant effect on maternal mortality (25). Before the scaling up of the policy, Penfold et al. observed that the policy increased skilled delivery and reduced inequality in the utilization of maternal healthcare service (46). McKinnon et al. observed that facility-based delivery increased while neonatal mortality decreased (47). |
| After scale up | Witter et al. reported that the stakeholders believed that the policy was a cost-effective initiative that can reduce inequality in the utilization of maternal healthcare service. Insufficient funding, inadequate management, irregular reimbursement, increased workload without any increase in staff strength subsequently hampered the quality of maternal healthcare (29). | ||
| Witter et al. reported that the stakeholders believed that the policy was a good initiative to improve skilled delivery. The study showed improvement in early antenatal registrants but regions were not well consulted in terms of reimbursement. Consequently, reimbursement was erratic and insufficient (30). | |||
| The study conducted by Witter et al. showed that the policy was well accepted as an effective strategy to improve safe delivery; contents of the policy were clear but insufficient; erratic funding delayed inadequate reimbursement; increased workload without incentive or any corresponding increase in the number of care providers militate against the sustainability of the policy (34). | |||
| Meessen et al. observed 1) Agenda setting: It was not clear whether the policy was adopted as a result of pressure from donors or taking the advantage of the offer of being a “low resource setting”. 2) Policy formulation: Assessment of this policy based on good practices in policy formulation showed that the objectives of the policy were clear and the stakeholders welcomed the policy but its formulation was not free from donor's influence. Important policy formulation good practices such as situation analysis, assessment of different policy options, and stakeholders’ involvement were not observed. 3) Implementation stage: suffered from erratic and insufficient funding (27). | |||
| Focused Antenatal Care (FANC) (11) | Individualized care for pregnant women to improve efficiency and safe delivery.It involves early detection of complication, pre-existing morbidity, birth preparedness, health education, and health promotion. For a healthy woman, four antenatal visits at <16, 26, 32, and 36 weeks were recommended. (Implemented in 2002) | During policy implementation | Increased antenatal registrants, increased early antenatal registrants, improved patient–doctor interaction, reduced waiting time, improved quality of antenatal care, increased health facility delivery, reduced stillbirth, and increased postnatal care utilization were observed by Deganus et al. following the implementation of FANC (26). Nyarko et al. reported that both patients and healthcare providers accepted the policy. It improved the quality of antenatal care. However, there was no difference between the intervention facilities and the control facilities in terms of birth preparedness, complication readiness, and postnatal care. In addition, some intervention facilities were unable to implement some of the components of FANC due to lack of equipment (33). |
| National Health Insurance Scheme (12) (NHIS) | National health insurance for pregnant women: six antenatal visits, delivery (incl. obstetrics complications), two postnatal visits within 6 weeks post-delivery, neonatal care up to age 3 months. (Implemented in 2008) | Following the implementation of NHIS | Witter et al. showed that the policy makers did not learn from errors of free delivery policy; NHIS policy formulation was top-down, politically induced by donors, no well-prepared policy guidelines, no proper consultation, poor communication of the policy, no proper costing, no additional funds were made available, no long-time financial plan, erratic and insufficient reimbursement. Sub-optimal implementation, lack of adequate monitoring and evaluation, increased workload with a negative impact on healthcare quality. Despite these limitations implementation of the NHIS increased access to healthcare (32). |
| Integrated Management of Childhood Illness (8) (IMCI) | Aims to improve case management at primary level of care, management of childhood illnesses, and family and community childcare practices. It involves antenatal, delivery, and postnatal services; treatment and prevention of infectious diseases (pneumonia, diarrhea, malaria, measles, HIV/AIDS); improves nutrition (improves breastfeeding, reduces malnutrition), vaccination, and psychosocial development. (Started in 1998, by 2000 all districts started IMCI.) | Following the implementation of IMCI | Baiden et al. observed that many of the care providers were yet to receive training on IMCI. The study showed a significant level of non-compliance with the IMCI guidelines; all the 11 items in the IMCI checklist were observed in just 1% of the children. 95% of them received antimalarial treatment but only 11% underwent laboratory investigation (28). |
Maine et al. provided assessment was a general assessment of the SMP.
Additional interventions such as the CHPS (9), User Fees Exemption for Delivery Care (UFEDC) (10), FANC (11), and the NHIS (12) were implemented from 1999 onward to complement the impact of the existing programs so as to accelerate attainment MDG 4 and MDG 5. Maternal and child policies reviewed (Table 3) showed that most of the policies were directed at maternal, infant, and under-five mortality rather than neonatal mortality. Results presented indicate that these policies seem to have a greater effect on maternal healthcare utilization and maternal and childhood mortality and morbidity during the initiation phase than the scale-up phase (24–26, 48). Factors consistently identified to have a negative impact on the effectiveness of the various interventions were: deviation from good standard practice in policy formulation and implementation, erratic funding, insufficient community engagement, lack of proper monitoring, and inadequate manpower and equipment.
Discussion
This study compared the trends in neonatal, infant, and under-five mortality from 1988 to 2008 in Ghana. It also identified the impact and challenges of various health policies and programs implemented during this time period to attain MDG 4. Despite the global attention on childhood mortality, we noticed that from 1988 to 2008 in Ghana, the decline rates in neonatal, infant, and under-five mortality were far below the expectation of a 4% annual decline to attain MDG 4 globally (49) and less than the 7% annual reduction stipulated to achieve MDG 4 in sub-Saharan Africa (50).
Similar to what Baiden et al. (51) and Welaga et al. (52) observed in the Kassena-Nankana district of Northern Ghana, the observed trends in childhood mortality cannot be directly attributed to the various overlapping policies and programs implemented. However, some important observations were noticed. Health policies and intervention programs implemented from 1988 to 1998 (SMP (6), LSS for midwives (7), and IMCI (8)) were observed to have a larger effect on childhood mortality than those implemented from 1998 to 2008 (UFEDC (10), Focus Antenatal Care (FANC) (11), NHIS (12), and CHPS (9)).
Generally, the decline rates in neonatal, infant, and under-five mortality were far below expectations, and the implemented health policies and intervention programs appeared to have had more impact on under-five mortality than on neonatal and infant mortality. Due to the paltry decline in neonatal mortality, the proportion of infant and under-five mortality attributed to neonatal mortality has increased; this mimics global and SSA observations (49, 53). In addition, we identified in our review factors that were responsible for the slow decline observed in neonatal, infant, and under-five mortality. Studies that have evaluated health policies and intervention programs implemented in Ghana repeatedly showed that factors such as deviation from good standard practice in policy formulation and implementation (27, 28), erratic funding (29, 30), insufficient community engagement (9), inadequate monitoring (31, 32), and inadequate manpower and equipment (29, 33) are major challenges of health policies and programs that might have hindered a more pronounced decline in childhood mortality. Our observation was corroborated by a previous multi-country study that identified factors such as inadequate policy formulation and implementation, poor financing, shortage of health human resources, lack of re-training of staff, inadequate medical products and technologies as the major constraints to scale up intervention programs to improve survival in early life (54).
At the regional level, we observed some degree of variation in neonatal mortality trends. This observation may partly be explained by differences in implementation of national health policies and programs in conjunction with the disparities in additional programs implemented in the regions; examples of such regional differences are the Kybele program in the Greater Accra region (13, 14), kangaroo mother care (55), UNICEF-sponsored ACSD (15) in Northern Ghana, High Impact Rapid Delivery (HIRD) (56), and Project Five Alive (57, 58). The variation may also be driven by differences in baseline rate of neonatal mortality across the regions.
Recommendation
Considering the slow rate of decline in childhood mortality, particularly in neonatal mortality, implementation of cost-effective, neonatal-specific interventions, such as newborn resuscitation, exclusive breastfeeding, use of partograph, kangaroo mother care, use of micronutrients, tetanus toxoid immunization, will be needed to successfully address attainment of SDG 3.2 (2, 5, 59). In addition, implemented interventions to tackle childhood mortality should be reformed based on the recurrent defects identified in policy formulation and implementation to accelerate attainment of SDG 3.2 (9, 31, 34).
Study limitations and strengths
This is the first study in Ghana that utilized nationally representative data to examine trends in childhood mortality, allowing us to generalize our findings. GDHS data are generally regarded as high-quality data because of the sampling technique and the excellent household and respondent response rates (22). We went beyond the traditional graphical description of the mortality trends by applying Poisson regression to quantify the risk of dying over time. However, we are aware that there may have been the possibility of underreporting and misclassification in childhood mortality as a result of recall bias (60). In addition, non-sampling error such as misunderstanding of the question on the part of the participant or the interviewer could have occurred. As the current study was based on published articles, some valuable information on the impact and challenges of the intervention programs implemented and reported in the grey literature may not have been fully captured in this study. Also, most articles that assessed the implemented intervention programs were not properly designed to evaluate the effectiveness of these intervention programs.
Conclusion
This study compared the trends in neonatal, infant, and under-five mortality over two decades in Ghana. The observed decline rates were generally slow, particularly for neonatal mortality. This could be attributed to the short-comings identified for health policies and intervention programs formulation and implementation, particularly with regard to neonatal mortality. Implementation of a sustainable evidence-based neonatal-specific intervention and improving other existing interventions will be a prerequisite to actualize SDG 3.2 in Ghana and beyond.
Summary
What's known: Interventions were implemented in Ghana to achieve MDG 4 but the impact and challenges have not been assessed to inform SDG 3.2.
What's new: Since 1988, the decline in childhood mortality in Ghana was below the expected rate and the proportion of infant and under-five mortality attributed to neonatal death has increased because implementation of most intervention programs was suboptimum and newborns less considered. Implications: Implement neonatal-specific interventions and improve existing programs.
Acknowledgements
We appreciate Measures DHS for permitting us to analyze Ghana DHS. We also grateful for the financial support from the Netherlands Organization for Scientific Research/WOTRO Science for Development (Grant Number: 07.45.102.00) toward the completion of this study.
Authors' contributions
GAK, DEG, HD, and KKG designed the study, whereas GAK carried out data collection, literature review, data analysis, and also drafted the first version of the manuscript. All authors reviewed and approved the final version of the manuscript.
Conflict of interest and funding
The authors declare that they have no competing interests.
Paper context
Since the adoption of Millennium Development Goal 4 in Ghana to reduce under-five mortality by two-thirds between 1990 and 2015, efforts were made towards attainment. However, impacts and challenges of implemented intervention programs have not been examined to inform implementation of SDG 3.2. This study examined what has been achieved in neonatal, infant and under-five mortality over two decades and highlighted the impacts and challenges of intervention programs implemented. This study provided important information that policy makers can utilize towards actualizing SDG 3.2.
References
- 1.United Nations Millennium Declaration. Available from: http://www.unorg/millennium/declaration/ares552epdf [cited 14 Febrauary 2014]
- 2.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–88. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 3.Knippenberg R, Lawn JE, Darmstadt GL, Begkoyian G, Fogstad H, Walelign N, et al. Systematic scaling up of neonatal care in countries. Lancet. 2005;365:1087–98. doi: 10.1016/S0140-6736(05)71145-4. [DOI] [PubMed] [Google Scholar]
- 4.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? where? why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 5.Martines J, Paul VK, Bhutta ZA, Koblinsky M, Soucat A, Walker N, et al. Neonatal survival: a call for action. Lancet. 2005;365:1189–97. doi: 10.1016/S0140-6736(05)71882-1. [DOI] [PubMed] [Google Scholar]
- 6.The safe motherhood action agenda: priorities for the next decade. Available from: http://files.givewell.org/files/DWDA 2009/Interventions/Maternal Mortality/SafeMotherhoodActionAgenda.pdf [cited 23 April 2015]
- 7.Overview of ACNM's Life Saving Skills Program (LSS) Available from: http://www.midwife.org/Life-Saving-Skills-LSS [cited 14 September 2014]
- 8.Integrated Management of Childhood Illness (IMCI) Available from: http://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCYQFjAA&url=http%3A%2F%2Fwww.afro.who.int%2Findex.php%3Foption%3Dcom_docman&task%3Ddoc_download%26gid%3D1594%26amp;ei=CNQ4VbL5EorgaO-dgMAF&usg=AFQjCNGZapepAsyvI9tVeiqXLrWDkFJNfw [cited 23 April 2015]
- 9.Nyonator FK, Woonor-Williams JK, Phillips JF, Jones TC, Miller RA. The Ghana community-based health planning and services initiative for scaling up service delivery innovation. Health Policy Plan. 2005;20:25–34. doi: 10.1093/heapol/czi003. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health. Guidelines for implementing the exemption policy on maternal deliveries. Accra: Ministry of Health; 2004. Report No. MoH/Policy, Planning, Monitoring and Evaluation-59. 2015. [Google Scholar]
- 11.Focused Antenatal Care. Available from: http://www.who.int/pmnch/media/publications/aonsectionIII_2.pdf [cited 23 April 2015]
- 12.Ghana National Health Insurance Act (Act 650) 2003. Available from: http://www.social-protection.org/gess/ResourcePDF.do?resource.ressourcel [cited 6 July 2016]
- 13.Engmann C, Olufolabi A, Srofenyoh E, Owen M. Multidisciplinary team partnerships to improve maternal and neonatal outcomes: the Kybele experience. Int Anesthesiol Clin. 2010;48:109–22. doi: 10.1097/AIA.0b013e3181dd4f13. [DOI] [PubMed] [Google Scholar]
- 14.Srofenyoh E, Ivester T, Engmann C, Olufolabi A, Bookman L, Owen M. Advancing obstetric and neonatal care in a regional hospital in Ghana via continuous quality improvement. Int J Gynaecol Obstet. 2012;116:17–21. doi: 10.1016/j.ijgo.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Ghana Accelerated Child Survival and Developement Approach (ACSD) Available from: http://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCYQFjAA&url=http%3A%2F%2Fwww.unicef.org%2Finnovations%2Ffiles%2Fghana.doc&ei=GP04VePxDcf7arOfgdAH&usg=AFQjCNFviowYjuuXq2IjhvMR__tExTTFbQ&bvm=bv.91427555 [cited 23 April 2015]
- 16.Kangaroo Mother Care in Ghana. Available from: http://www.unicef.org/sowc09/docs/SOWC09-Panel-3.5-EN.pdf [cited 24 April 2015]
- 17.You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet. 2015;386:2275–86. doi: 10.1016/S0140-6736(15)00120-8. [DOI] [PubMed] [Google Scholar]
- 18.MDG 2014 Report: assessing progress in Africa towards the Millennium Development Goals: United Nations. Available from: http://www.afdb.org/fileadmin/uploads/afdb/Documents/Publications/MDG_Report_2014_11_2014.pdf [cited 24 April 2015]
- 19.World Bank Data: Ghana. Available from: http://data.worldbank.org/country/ghana [cited 21 January 2013]
- 20.World Bank Data: population growth. Available from: http://search.worldbank.org/data?qterm=ghana population growth rate&language=EN [cited 9 January 2013]
- 21.Ghana: ethnic groups. Available from: http://www.ghanaweb.com/GhanaHomePage/tribes/ [cited 11 January 2013]
- 22.Measure Demographic and Health Survey. Available from: http://www.measuredhs.com [cited 4 June 2013]
- 23.StataSE 11. Available from: www.stata.com [cited 13 May 2013]
- 24.Phillips JF, Bawah AA, Binka FN. Accelerating reproductive and child health programme impact with community-based services: the Navrongo experiment in Ghana. Bull World Health Organ. 2006;84:949–55. doi: 10.2471/blt.06.030064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bosu W, Bell JS, Rmar-Klemesu M, Tornui JA. Effect of delivery care user fee exemption policy on institutional maternal deaths in the central and volta regions of Ghana. Ghana Med J. 2007;41:118–24. doi: 10.4314/gmj.v41i3.55278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The maternal and neonatal health program's ‘Champions for change: improving maternal and newborn survival’. Available from: http://pdf.usaid.gov/pdf_docs/PNADA618.pdf [cited 12 July 2014.
- 27. Meessen B, Hercot D, Noirhomme M, Ridde V, Tibouti A, Tashobya CK, et al. Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Policy Plan. 2011;26(Suppl 2):ii6–29. doi: 10.1093/heapol/czr062. [DOI] [PubMed] [Google Scholar]
- 28.Baiden F, Owusu-Agyei S, Bawah J, Bruce J, Tivura M, Delmini R, et al. An evaluation of the clinical assessments of under-five febrile children presenting to primary health facilities in rural Ghana. PLoS One. 2011;6:e28944. doi: 10.1371/journal.pone.0028944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Witter S, Adjei S, Rmar-Klemesu M, Graham W. Providing free maternal health care: ten lessons from an evaluation of the national delivery exemption policy in Ghana. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1881. 1881, doi: http://dx.doi.org/10.3402/gha.v2i0.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Witter S, Adjei S. Start-stop funding, its causes and consequences: a case study of the delivery exemptions policy in Ghana. Int J Health Plann Manage. 2007;22(2):133–43. doi: 10.1002/hpm.867. [DOI] [PubMed] [Google Scholar]
- 31.Awoonor-Williams JK, Sory EK, Nyonator FK, Phillips JF, Wang E, Schmitt ML. Lessons learned from scaling up a community-based health program in the Upper East Region of Northern Ghana. Glob Health Sci Pract. 2013;1:117–33. doi: 10.9745/GHSP-D-12-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Witter S, Garshong B, Ridde V. An exploratory study of the policy process and early implementation of the free NHIS coverage for pregnant women in Ghana. Int J Equity Health. 2013;12:16. doi: 10.1186/1475-9276-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acceptability and feasibility of introducing the WHO focused antenatal care package in Ghana. Available from: http://www.popcouncil.org/uploads/pdfs/frontiers/FR_FinalReports/ghana_who_anc.pdf [cited 14 Febrauary 2014]
- 34.Witter S, Arhinful DK, Kusi A, Zakariah-Akoto S. The experience of Ghana in implementing a user fee exemption policy to provide free delivery care. Reprod Health Matters. 2007;15:61–71. doi: 10.1016/S0968-8080(07)30325-X. [DOI] [PubMed] [Google Scholar]
- 35.Okiwelu T, Hussein J, Adjei S, Arhinful D, Rmar-Klemesu M. Safe motherhood in Ghana: still on the agenda? Health Policy. 2007;84:359–67. doi: 10.1016/j.healthpol.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Anderson FW, Mutchnick I, Kwawukume EY, Danso KA, Klufio CA, Clinton Y, et al. Who will be there when women deliver? Assuring retention of obstetric providers. Obstet Gynecol. 2007;110:1012–16. doi: 10.1097/01.AOG.0000287064.63051.1c. [DOI] [PubMed] [Google Scholar]
- 37.Maine D, Rosenfield A. The safe motherhood initiative: why has it stalled? Am J Public Health. 1999;89:480–2. doi: 10.2105/ajph.89.4.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Debpuur C, Phillips JF, Jackson EF, Nazzar A, Ngom P, Binka FN. The impact of the Navrongo Project on contraceptive knowledge and use, reproductive preferences, and fertility. Stud Fam Plann. 2002;33:141–64. doi: 10.1111/j.1728-4465.2002.00141.x. [DOI] [PubMed] [Google Scholar]
- 39.Pence BW, Nyarko P, Phillips JF, Debpuur C. The effect of community nurses and health volunteers on child mortality: the Navrongo Community Health and Family Planning Project. Scand J Public Health. 2007;35:599–608. doi: 10.1080/14034940701349225. [DOI] [PubMed] [Google Scholar]
- 40.Binka FN, Bawah AA, Phillips JF, Hodgson A, Adjuik M, MacLeod B. Rapid achievement of the child survival millennium development goal: evidence from the Navrongo experiment in Northern Ghana. Trop Med Int Health. 2007;12:578–83. doi: 10.1111/j.1365-3156.2007.01826.x. [DOI] [PubMed] [Google Scholar]
- 41.Phillips JF, Jackson EF, Bawah AA, MacLeod B, Adongo P, Baynes C, et al. The long-term fertility impact of the Navrongo project in northern Ghana. Stud Fam Plann. 2012;43:175–90. doi: 10.1111/j.1728-4465.2012.00316.x. [DOI] [PubMed] [Google Scholar]
- 42.Awoonor-Williams JK, Feinglass ES, Tobey R, Vaughan-Smith MN, Nyonator FK, Jones TC. Bridging the gap between evidence-based innovation and national health-sector reform in Ghana. Stud Fam Plann. 2004;35:161–77. doi: 10.1111/j.1728-4465.2004.00020.x. [DOI] [PubMed] [Google Scholar]
- 43.Adongo PB, Tapsoba P, Phillips JF, Tabong PT, Stone A, Kuffour E, et al. The role of community-based health planning and services strategy in involving males in the provision of family planning services: a qualitative study in Southern Ghana. Reprod Health. 2013;10:36. doi: 10.1186/1742-4755-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adongo PB, Phillips JF, Aikins M, Arhin DA, Schmitt M, Nwameme AU, et al. Does the design and implementation of proven innovations for delivering basic primary health care services in rural communities fit the urban setting: the case of Ghana's Community-based Health Planning and Services (CHPS) Health Res Policy Syst. 2014;12:16. doi: 10.1186/1478-4505-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Asante F, Chikwama C, Daniels A, Rmar-Klemesu M. Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in Ghana. Ghana Med J. 2007;41:110–17. doi: 10.4314/gmj.v41i3.55277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery fee exemption policy in Ghana: population estimates of changes in delivery service utilization in two regions. Ghana Med J. 2007;41:100–9. [PMC free article] [PubMed] [Google Scholar]
- 47.McKinnon B, Harper S, Kaufman JS, Bergevin Y. Removing user fees for facility-based delivery services: a difference-in-differences evaluation from ten sub-Saharan African countries. Health Policy Plan. 2015;30:432–41. doi: 10.1093/heapol/czu027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dzakpasu S, Soremekun S, Manu A, Ten AG, Tawiah C, Hurt L, et al. Impact of free delivery care on health facility delivery and insurance coverage in Ghana's Brong Ahafo Region. PLoS One. 2012;7:e49430. doi: 10.1371/journal.pone.0049430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 50.United Nation. The Millennium Development Goals Report 2009. New York: United Nation; 2009. [Google Scholar]
- 51.Baiden F, Hodgson A, Adjuik M, Adongo P, Ayaga B, Binka F. Trend and causes of neonatal mortality in the Kassena-Nankana district of northern Ghana, 1995–2002. Trop Med Int Health. 2006;11:532–9. doi: 10.1111/j.1365-3156.2006.01582.x. [DOI] [PubMed] [Google Scholar]
- 52.Welaga P, Moyer CA, Aborigo R, Adongo P, Williams J, Hodgson A, et al. Why are babies dying in the first month after birth? A 7-year study of neonatal mortality in northern Ghana. PLoS One. 2013;8:e58924. doi: 10.1371/journal.pone.0058924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, Cousens S, et al. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. PLoS Med. 2011;8:e1001080. doi: 10.1371/journal.pmed.1001080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dickson KE, Simen-Kapeu A, Kinney MV, Huicho L, Vesel L, Lackritz E, et al. Every newborn: health-systems bottlenecks and strategies to to accelerate scale-up in countries. Lancet. 2014;384:438–54. doi: 10.1016/S0140-6736(14)60582-1. [DOI] [PubMed] [Google Scholar]
- 55.Nguah S, Wobil P, Obeng R, Yakubu A, Kerber K, Lawn J, et al. Perception and practice of Kangaroo Mother Care after discharge from hospital in Kumasi, Ghana: a longitudinal study. BMC Pregnancy Childbirth. 2011;11:99. doi: 10.1186/1471-2393-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ghana Ministry of Health. High impact rapid delivery. Available from: http://www.moh-ghana.org/UploadFiles/Publications/HIRD120506090346.pdf [cited 11 July 2014]
- 57.Twum-Danso NAY, Akanlu GB, Osafo E, Sodzi-Tettey S, Boadu RO, Atinbire S, et al. A nationwide quality improvement project to accelerate Ghana's progress toward Millennium Development Goal Four: design and implementation progress. Int J Qual Health Care. 2012;24:601–11. doi: 10.1093/intqhc/mzs060. [DOI] [PubMed] [Google Scholar]
- 58.Singh K, Speizer I, Handa S, Boadu RO, Atinbire S, Barker PM, et al. Impact evaluation of a quality improvement intervention on maternal and child health outcomes in Northern Ghana: early assessment of a national scale-up project. Int J Qual Health Care. 2013;25:477–87. doi: 10.1093/intqhc/mzt054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mangiaterra V, Mattero M, Dunkelberg E. Why and how to invest in neonatal health. Semin Fetal Neonatal Med. 2006;11:37–47. doi: 10.1016/j.siny.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 60.Assessment of the quality of data used for direct estimation of infant and under-five mortality in DHS-II surveys: demographic and health surveys. Available from: http://www.dhsprogram.com/pubs/pdf/OP3/OP3.pdf [cited 21 July 2014]