Abstract
The median arcuate ligament (MAL) can rarely compress both the celiac axis and superior mesenteric artery. We present a case of a 70-year male who presented with isolated episodes of upper abdominal pain and diarrhea associated with sweats and nausea. Angiography images demonstrated complete occlusion of the celiac axis and compression of the superior mesenteric artery during the expiration phases. The celiac axis was reconstituted distal to its origin by a patent Arc of Buhler. Other reported cases of multivessel MALs have produced severe symptoms in young adults requiring surgical and/or endovascular intervention. In this case, our patient's Arc of Buhler was protective against more severe chronic mesenteric ischemia. We suggest that a patent Arc of Buhler is protective against symptoms in a single vessel MALs patient. A significant percentage of patients receiving surgical intervention for MALs do not have relief of symptoms. There should be a search for an Arc of Buhler before surgical management of patients suspected to have single vessel MALs.
Keyword: Multivessel MALS, Median Arcuate Ligament, Arc of Buhler
Introduction
The median arcuate ligament (MAL) can compress the celiac axis causing symptoms of chronic mesenteric ischemia. This condition is referred to as median arcuate ligament syndrome (MALS) and poses a diagnostic challenge. MALS is predominantly understood as a syndrome of celiac artery compression. In fact, MALS is also referred to as celiac artery compression syndrome. The MAL can also compress the ostium of the superior mesenteric artery (SMA), although this is quite uncommon. A rare connection between the celiac axis and the SMA is the Arc of Buhler [1], [2]. The Arc of Buhler has been described as protective in cases of mesenteric ischemia [2]. There are very few cases in the literature describing MAL compression of both the celiac trunk and SMA. To our knowledge, there are no cases in the literature describing multivessel compression by the MAL with an Arc of Buhler. We present a case of celiac axis occlusion and variable compression of the SMA by the MAL in a 70-year-old man with a prominent Arc of Buhler and symptoms of intermittent intestinal angina.
Case report
A 70-year-old man presented with isolated episodes of upper abdominal pain and diarrhea associated with sweats and nausea. These episodes had a duration of 30 minutes and were intermittent in nature. The patient was known for having chronic abdominal pain, which was diagnosed as “irritable bowel syndrome”. Other pertinent medical history included a longstanding history of hypertension and mitral valve prolapse. The patient was referred to the gastroenterology service for evaluation of his symptoms. A computed tomography scan was ordered to search for anatomic or mechanical causes of the diarrhea.
The computed tomography scan demonstrated complete occlusion of the celiac axis and stenosis of the ostium of the SMA by the MAL (Fig. 1).
Fig. 1.
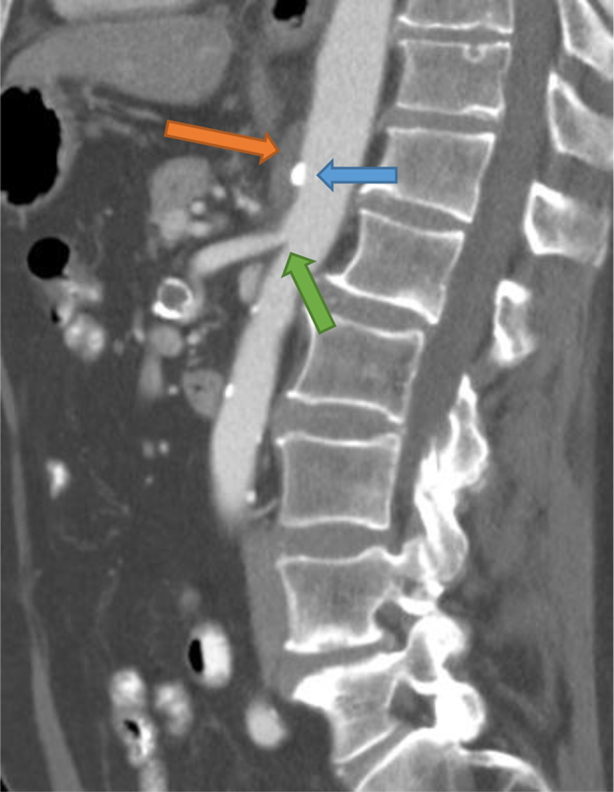
Sagittal CT angiogram demonstrating complete occlusion of the celiac axis at its ostium (blue arrow) and apparent narrowing of the SMA (green arrow) by the MAL (orange arrow). CT, computed tomography; MAL, median arcuate ligament; SMA, superior mesentric artery.
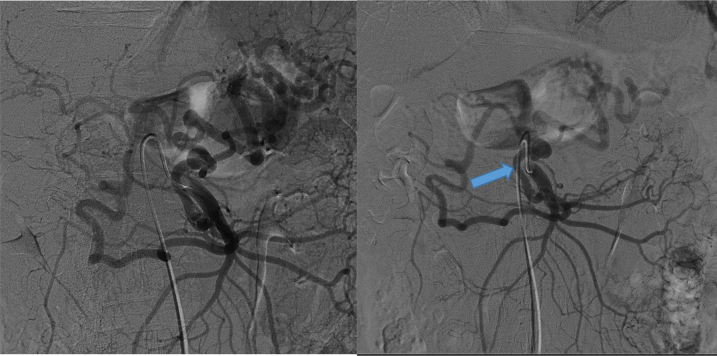
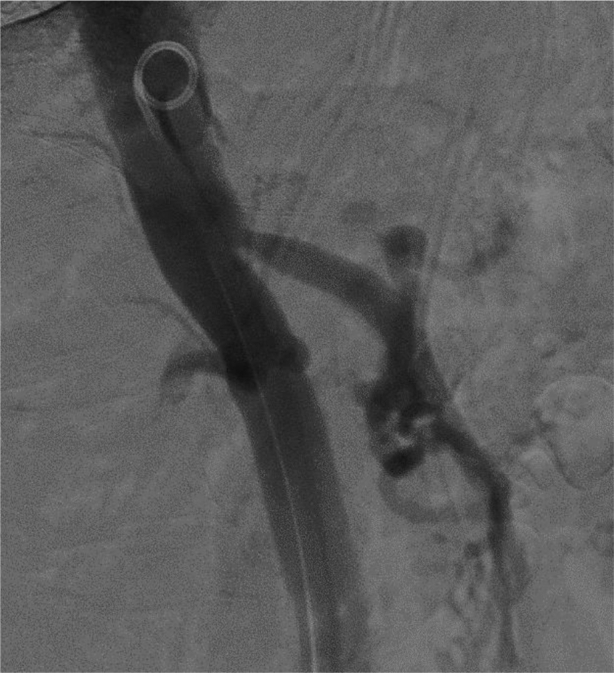
The patient was referred to interventional radiology for further evaluation of the celiac axis and SMA. The angiography images again demonstrated a complete occlusion of the celiac axis at its origin and compression of the SMA during the expiration phases. During the inspiration phase of the arteriogram, the SMA appeared widely patent (Fig. 2); however, during the expiration phase, there was a significant compression of the SMA (Fig. 3). The celiac axis was reconstituted distal to its origin by a dilated and widely patent Arc of Buhler (Fig. 4).
Fig. 2.
Angiography of the SMA during inspiration. SMA, superior mesentric artery.
Fig. 3.

Angiography of the SMA during expiration. SMA, superior mesentric artery.
Fig. 4.
Angiography of Arc of Buhler (blue arrow) connecting the SMA with the celiac axis. SMA, superior mesentric artery.
Discussion
The MALS is a rare vascular disorder caused by fibrous bands connecting the left and right crus of the diaphragm. The bands comprise the MAL and usually pass over the aorta superior to the celiac artery at the level of the first lumbar vertebrae. In MALS, the visceral vessels are compressed by the crossing of the MAL. A diagnosis of MALS can be challenging and is often one of exclusion [3], [4]. Chronic visceral ischemia is usually caused by gradual narrowing or occlusion of at least 2 of the 3 major arteries supplying the stomach and small bowel. Compression of the celiac artery by the MAL of the diaphragm is an uncommon cause of mesenteric ischemia.
A rare connection between the celiac axis and the SMA is the Arc of Buhler. The incidence of an Arc of Buhler has been reported as 3.3% in the general population [1], [2]. This has been described as protective in cases of mesenteric ischemia allowing for collateral flow in cases of occlusion or external compression of either artery [2].
This case of a 70-year-old man with complete occlusion of the celiac axis and variable compression of the SMA demonstrates a very rare condition, which is referred to as multivessel MALS.
Other reported cases of multivessel MALS have produced more severe symptoms in younger adults, each of which required surgical and/or endovascular intervention [5], [6], [7], [8].
In this case, our patient's Arc of Buhler was protective against more severe chronic mesenteric ischemia. The patient may have had gradual complete occlusion of his celiac artery, but his widely patent Arc of Buhler protected him from more severe symptoms of traditional single-vessel MALS. As the patients' SMA was compressed, he likely began to develop intermittent abdominal pain characteristic of intestinal angina. His chronic symptoms of intermittent mesenteric angina may have been underlying his diagnosis of irritable bowel syndrome.
It is our belief that a patent Arc of Buhler is protective against symptoms in a traditional single-vessel MALS patient. The late presentation and relatively mild symptoms of our patient demonstrates this protective effect. We suggest that there should be a search for an Arc of Buhler before surgical management of patients suspected to have single-vessel MALS. A dedicated search for an Arc of Buhler is not currently part of the traditional workup for MALS [3], [4]. If there is an Arc of Buhler present, although rare, it is unlikely that the MAL compression of the celiac axis is the cause of the patient's intermittent abdominal pain. A significant number of patients receiving surgical intervention do not have relief of symptoms [4], [9]. An interesting further investigation may be done into how many patients with persistent symptoms after surgical intervention had an Arc of Buhler.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Saad W.E.A. Arc of Buhler: incidence and diameter in asymptomatic individuals. Vasc Endovascular Surg. 2005;39(4):347–349. doi: 10.1177/153857440503900407. [DOI] [PubMed] [Google Scholar]
- 2.Schneider T.A., Longo W.E., Ure T., Vernava A.M. Mesenteric ischemia. Dis Colon Rectum. 1994;37(11):1163–1174. doi: 10.1007/BF02049824. [DOI] [PubMed] [Google Scholar]
- 3.Duffy A.J., Panait L., Eisenberg D., Bell R.L., Roberts K.E., Sumpio B. Management of median arcuate ligament syndrome: a new paradigm. Ann Vasc Surg. 2009;23(6):778–784. doi: 10.1016/j.avsg.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Mak G.Z., Speaker C., Anderson K., Stiles-Shields C., Lorenz J., Drossos T. Median arcuate ligament syndrome in the pediatric population. J Pediatr Surg. 2013;48(11):2261–2270. doi: 10.1016/j.jpedsurg.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyle A.J., Chandra A. Chronic mesenteric ischemia in a 26-year-old man: multivessel median arcuate ligament compression syndrome. Ann Vasc Surg. 2012;26(1):108–111e5. doi: 10.1016/j.avsg.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Kopecky K.K., Stine S.B., Dalsing M.C., Gottlieb K. Median arcuate ligament syndrome with multivessel involvement: diagnosis with spiral CT angiography. Abdom Imaging. 1997;22(3):318–320. doi: 10.1007/s002619900199. [DOI] [PubMed] [Google Scholar]
- 7.Stein J., Costanza M.J., Rivero M., Gahtan V., Amankwah K.S. External compression of the superior mesenteric artery by the median arcuate ligament. Vasc Endovascular Surg. 2011;45(6):1538. doi: 10.1177/1538574411412827. [DOI] [PubMed] [Google Scholar]
- 8.Lawson J.D., Ochsner J.L. Median arcuate ligament syndrome with severe two-vessel involvement. Arch Surg. 1984;119(2):226–227. doi: 10.1001/archsurg.1984.01390140082015. [DOI] [PubMed] [Google Scholar]
- 9.Tulloch A.W., Jimenez J.C., Lawrence P.F., Dutson E.P., Moore W.S., Rigberg D.A. Laparoscopic versus open celiac ganglionectomy in patients with median arcuate ligament syndrome. J Vasc Surg. 2010;52(5):1283–1289. doi: 10.1016/j.jvs.2010.05.083. [DOI] [PubMed] [Google Scholar]