Abstract
Glomus tumors are rare benign hamartomas arising from the neuromyoarterial glomus body, a highly specialized arteriovenous anastomosis responsible for thermoregulation. Although classically associated with a subungual location, less common extradigital glomus tumors can present a diagnostic challenge because of their rarity and nonspecific presentation. This case report adds to the literature of proven extradigital glomus tumors with documented pathologic and magnetic resonance imaging characteristics and describes their place in the differential for soft tissue mass of the wrist. Occasionally, a combination of imaging findings and clinical history as described may help suggest the diagnosis prospectively.
Keywords: extradigital glomus, wrist, magnetic resonance imaging
Introduction
Glomus bodies represent a highly specialized arteriovenous anastomosis responsible for thermoregulation and consist of an afferent arteriole, tortuous arteriovenous anastomosis, system of collecting veins, and neurovascular reticulum that regulates blood flow through the anastomosis [1]. Glomus bodies are present in the stratum reticularis of the dermis throughout the body but are most highly concentrated in the skin of the digits, palms, and soles of the feet [1]. Although glomus tumors may occur throughout the body, up to 75% occur in the hand with 50%-65% of these occurring in the fingertips and/or subungual location [1], [2]. A retrospective case review from the Mayo Clinics documented 4 extradigital glomus tumors located in the wrist over a 20-year period [3].
We present a case of extradigital glomus tumor of the wrist, review the magnetic resonance imaging (MRI) appearance of classic subungual glomus tumors and previously documented extradigital glomus tumors, and suggest a constellation of MRI findings and clinical history, which may permit inclusion of extradigital glomus tumor in the differential for wrist soft tissue mass prospectively.
Case report
The patient is an otherwise healthy 33-year-old man presenting with complaints of a tender mass on the ulnar aspect of the right wrist. He reported the mass first appeared approximately 2 years prior as a small tender palpable nodule occurring shortly after an injury to the site with associated glass foreign-body debris. The mass had been growing progressively larger over time. Tenderness in the area was present since onset of the mass but had grown progressively worse in the 3-4 months before presentation, with the patient ultimately presenting to the emergency department (ED) for painful wrist mass.
On initial presentation to the ED, there was concern for a fluid collection, and the mass was lanced with only mild bloody drainage and no evidence of abscess. Subsequent radiograph of the right wrist demonstrated a 2.1 × 1.7-cm rounded area of soft tissue density along the ulnar aspect of the distal ulna (Fig. 1). No osseous abnormality was seen and no radiopaque foreign body was identified. The patient was ultimately discharged from the ED with referral to orthopedic surgery for further evaluation.
Fig. 1.
Radiograph of the right wrist demonstrates a 2.1 × 1.7-cm rounded area of soft tissue density along the ulnar aspect of the distal ulna. No associated osseous abnormality or soft tissue calcification is present.
Orthopedic evaluation revealed a soft, somewhat mobile, very tender mass over the ulnar aspect of the right wrist without overlying warmth or erythema. A small skin incision was identified superficially consistent with recent ED drainage attempt. Neurovascular function was intact. Orthopedic work-up included contrast-enhanced MRI of the wrist as well as ultrasound (US)-guided biopsy by interventional radiology.
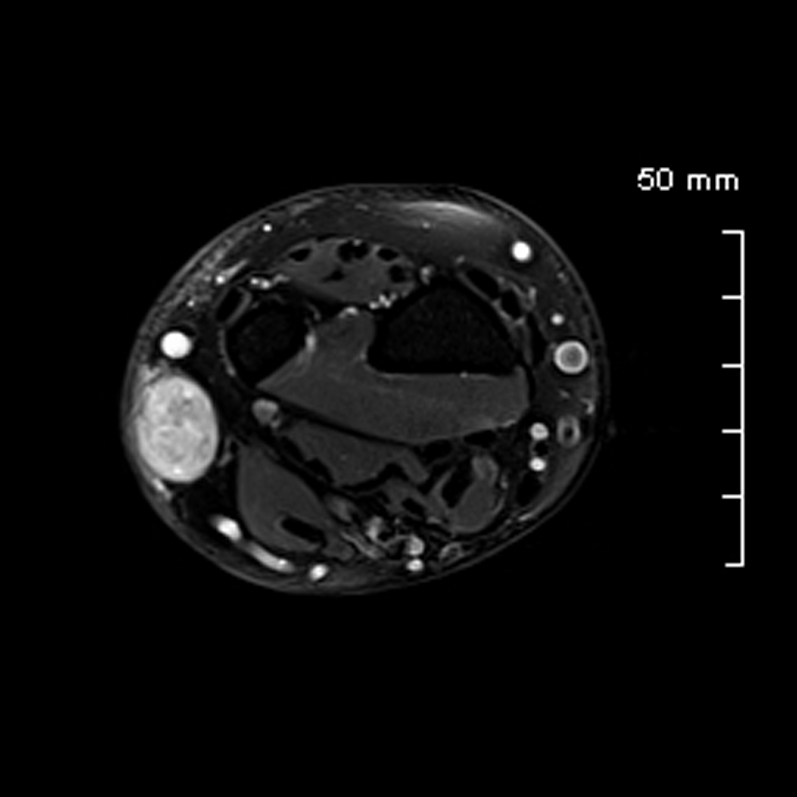
MRI of the wrist revealed a well-circumscribed lobulated, septated soft tissue mass along the ulnar aspect of the wrist centered in the subcutaneous fat, measuring 2.1 × 1.3 × 1.6 cm. The mass demonstrated hyperintense T2 signal, isointense T1 signal, and avid postcontrast enhancement (Fig. 2, Fig. 3, Fig. 4). Central areas of internal T2 hypointensity and nonenhancement were favored to represent blood products from recent ED biopsy vs internal tumoral hemorrhage or necrosis (Fig. 5). Tiny internal foci of T1 shortening were also identified which were felt to represent additional hemorrhage vs small internal vessels or fat (Fig. 5A). There was no evidence of association with the adjacent bones, muscles, nerves, tendons, or vascular structures. Findings were reported as nonspecific but suspicious for sarcoma and further evaluation with tissue biopsy or excision was recommended.
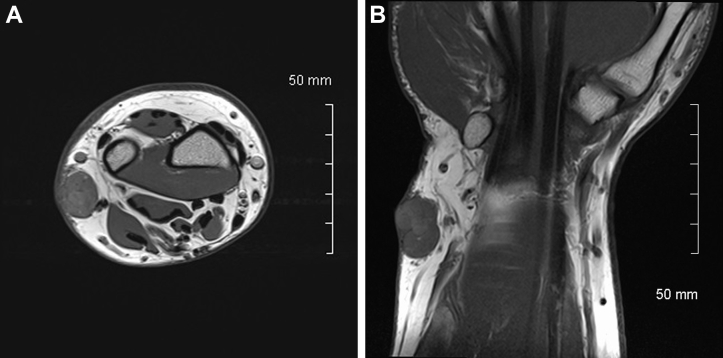
Fig. 2.
T1 (A) axial and (B) coronal images demonstrate a well-circumscribed slightly lobulated soft tissue mass along the ulnar aspect of the wrist centered in the subcutaneous fat, measuring 2.1 × 1.3 × 1.6 cm. The mass demonstrates T1 signal isointense to muscle.
Fig. 3.
Axial T2-weighted sequence demonstrates a well-circumscribed soft tissue mass along the ulnar aspect of the wrist with hyperintense T2 signal.
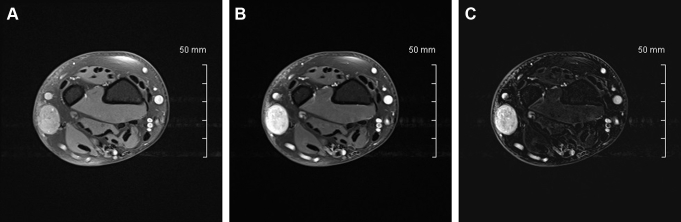
Fig. 4.
Axial (A) precontrast T1 fat-sat, (B) postcontrast T1 fat-sat, and (C) postcontrast subtraction sequences demonstrate a well-circumscribed strongly enhancing soft tissue mass along the ulnar aspect of the wrist centered in the subcutaneous fat. Axial (A) precontrast T1 fat-sat image demonstrates a tiny focus of T1 shortening favored to represent hemorrhage or a small vessel vs unsuppressed fat.
Fig. 5.
Coronal (A) T1, (B) short tau inversion recovery, and (C) postcontrast T1 fat-sat sequences demonstrate areas of internal T2 hypointensity and nonenhancement favored to represent blood products from recently attempted ED aspiration vs internal tumoral hemorrhage or necrosis. Coronal (A) precontrast T1 image demonstrates a tiny focus of T1 shortening favored to represent hemorrhage or a small vessel vs fat.
US-guided biopsy was subsequently performed by interventional radiology with six 18-gauge core biopsies obtained, resulting in 4 direct smear slides and 2 cell block slides. Pathologic evaluation revealed proliferation of rather homogenous cells with round nuclei and intact nuclear cytoplasmic ratio in a perivascular distribution, with immunoperoxidase stains positive for SMA and vimentin. Rare scattered desmin-positive cells and CD34-positive vascular cells were also present in the sample. Staining profile in conjunction with histologic morphology was considered diagnostic of a glomus tumor.
The lesion was subsequently excised via an 8-cm elliptical incision around the palpable mass and adjacent skin (Fig. 6). Gross pathology revealed a sharply demarcated, ovoid, multifocally hemorrhagic, gray subcutaneous soft tissue mass within the dermis and superficial subcutis measuring 2.0 × 1.6 × 1.5 cm with negative gross margins and an area of hemorrhage consistent with recent biopsy (Fig. 7).
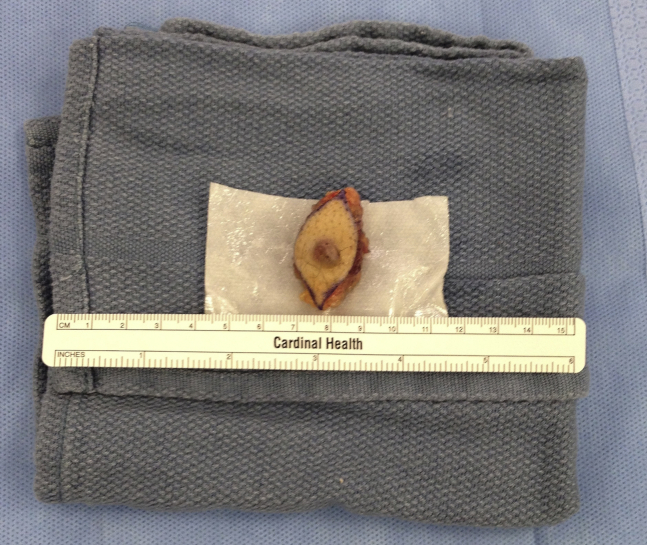
Fig. 6.
Intraoperative photograph demonstrating the mass excised via 8-cm elliptical incision around the palpable mass and adjacent skin. A small area of reddish-purple discoloration of the dermis superficial to the lesion is apparent.
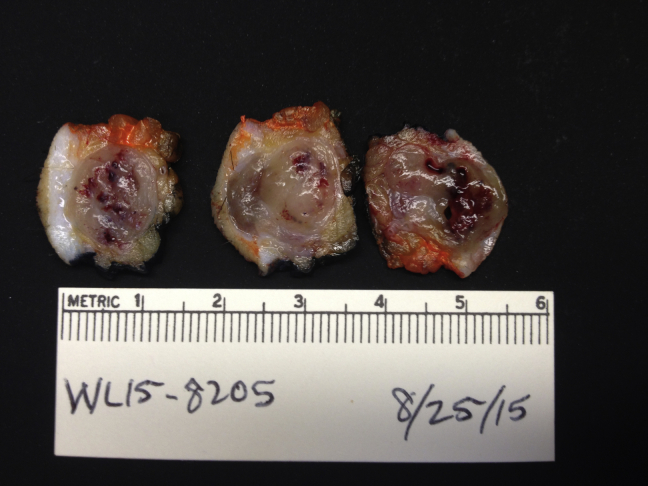
Fig. 7.
Gross pathology photograph reveals a sharply demarcated, ovoid, multifocally hemorrhagic, gray subcutaneous soft tissue mass within the dermis and superficial subcutis measuring 2.0 × 1.6 × 1.5 cm with an area of hemorrhage consistent with recent biopsy.
Histologic evaluation demonstrated a cellular neoplasm composed of sheets of monotonous small round cells with intervening thin- and thick-walled vascular channels, characteristic of a glomus tumor (Fig. 8, Fig. 9, Fig. 10). No evidence of nuclear pleomorphism, mitotic activity, or a spindle cell component was identified. Final pathologic diagnosis was total resection with negative margins of a 2.0 cm glomus tumor.
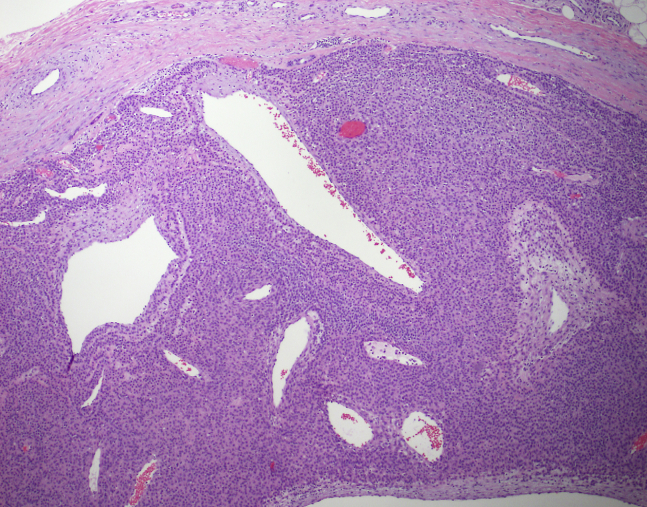
Fig. 8.
Low power view demonstrating a well-circumscribed tumor with numerous ectatic vessels (H and E stain, 4× original magnification).
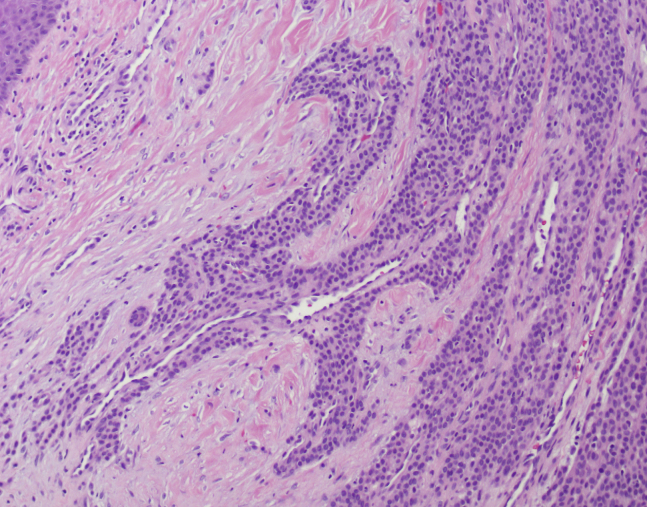
Fig. 9.
Tumor cell cuffing of vascular channels at the periphery of the tumor (H and E stain, 10× original magnification).
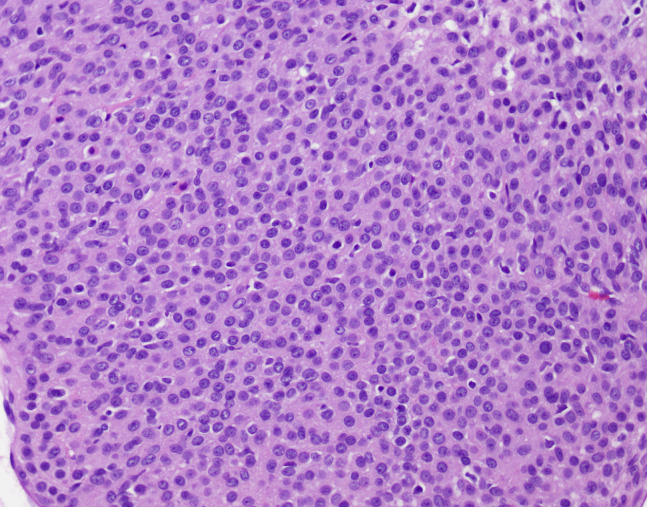
Fig. 10.
High power view showing dense cellularity with uniform round cells (H and E stain, 20× original magnification).
Discussion
Glomus tumors are rare overall but well described as a cause of pain in the subungual regions of the hand with well-documented US and MRI findings [1]. Extradigital tumors account for a minority of glomus tumors with only a few having been described located at the wrist, predominantly in the surgical literature [2], [3], [4], [5], [6].
Classic clinical manifestations of subungual glomus tumors include a solitary painful lesion with significant tenderness to palpation, dark red-purple or bluish skin discoloration, and sensitivity to cold [1], [2], [7]. Skin discoloration and cold hypersensitivity are less reliable with extradigital locations, however, being variable depending on the depth of the lesion. Pain and focally tender mass were the most consistent clinical findings associated with extradigital glomus tumors described in the literature [2], [3], [4], [6], [8], [9]. Previous trauma or injury to the lesion area has been reported in 20%-30% of cases before symptom onset [2].
Glomus tumors are typically benign. Rarely, locally aggressive features including osseous destruction can be seen and very rare cases of malignant and metastatic potential have been reported in the literature [5], [7]. Treatment is complete surgical excision with success rates greater than 95% as measured by negative margins and resolution of symptoms. Local recurrence rates are often less than 5% at 2 years after excision [7].
Sonographic findings for subungual glomus tumors include nonspecific grayscale appearance of a solid hypoechoic mass beneath the nail, with associated hypervascularity on color Doppler, which can be specific for the diagnosis in this location [1]. Characteristic MRI features of subungual glomus tumors include intermediate or low T1 signal intensity, marked T2 hyperintensity, and strong postcontrast enhancement [1], [10], [11]. MR angiography has also been described as a useful adjunct for diagnosis of very small recurrent subungual glomus tumors, with typical MR angiographic findings including areas of strong enhancement in the arterial phase and tumor blush, which increases in size on the delayed phase [1], [11].
The literature documenting MRI characteristics for extradigital glomus tumors is less extensive. Prior case reports of extradigital glomus tumors of the wrist exist, predominantly in the surgical literature, but discussion of imaging characteristics is limited; one case report limited description to a heterogeneous subcutaneous mass with increased T2 signal intensity [2] and another only described the lesion as intermediate T1 signal and hyperintense T2 signal [4].
Lee et al [8] published perhaps the most thorough review of extradigital glomus tumor imaging characteristics in their 2010 case report of an extradigital glomus tumor of the forearm. In addition to their own case documenting noncontrast MRI findings of a well-marginated T1 hypointense, T2 and short tau inversion recovery hyperintense 1.4-cm forearm glomus tumor, the authors also performed a review of the English language literature for extradigital glomus tumors of any location. Their search found 10 published case reports with documented MRI findings, comprising 4 contrast-enhanced MRI studies and 6 noncontrast MRI studies. All 4 studies receiving contrast documented postcontrast enhancement. Nine of 10 of the articles documented hypointense or isointense T1 signal and hyperintense T2 signal; the outlying 10th article described T1 hyperintensity but was performed with only T1 sequences [8].
Three additional case reports of extradigital glomus tumors with described MR findings were identified in a review of the literature subsequent to the publication by Lee et al in 2010. All 3 of these more recent case reports also document T2 hyperintensity [12], [13], [14]; one of the 3 did not document T1 signal intensity [12], the other 2 described isointense or hypointense T1 signal. The one study performed with contrast did demonstrate postcontrast enhancement [13].
Overall, the body of documented MRI characteristics for extradigital glomus tumors appears similar to the more established subungual MRI appearance: relatively homogenous T1 iso-to-hypointensity and T2 hyperintensity and strong postcontrast enhancement. Our own case demonstrated MR findings congruent with this when taking into consideration the attempted aspiration and subsequent hemorrhage during ED work-up before imaging.
In isolation, these MRI characteristics are nonspecific. As performed routinely in practice, however, the differential can be narrowed by location and relationship to the relevant adjacent anatomy. Given a subcutaneous location as the most frequent presentation [15], it may be possible to identify the lesion as distinct from the bone, cartilage, joint, muscle, tendon, nerve, and/or vascular tissue, thus eliminating many lesions arising from those tissues. The absence of cystic or fat components can also help eliminate multiple lesions.
Remaining primary differential considerations would include chondroma, soft tissue hemangioma, foreign body granuloma, or sarcoma. Strong relatively homogenous postcontrast enhancement can help differentiate glomus tumors from the septal or peripheral enhancement of soft tissue chondromas [16]. Infiltrative borders, fat component on T1, significant T1, T2, and postcontrast heterogeneity, prominent internal flow voids, and/or the presence of phleboliths on plain film could all suggest the diagnosis of soft tissue hemangioma [16]. Early foreign body granuloma would fit a history of prior injury to the site and could demonstrate T2 hyperintensity and enhancement; however, a focus of internal low signal intensity representing the foreign body would be expected on both T1 and T2 sequences [16].
MRI features of malignant soft tissue tumors of the hand and wrist are nonspecific. Poorly defined margins, inhomogeneity of T2-weighted images, irregular postcontrast enhancement, the presence of necrosis, and a large lesion should all raise concern for a malignant process. Tissue diagnosis should be considered anytime there is not an unequivocal benign diagnosis [17].
Clinically, a prominent history of painful/focally tender mass often accompanies glomus tumors. In the absence of compelling alternative diagnoses or aggressive features, this history in conjunction with the imaging findings described previously may facilitate including extradigital glomus tumor in the differential preoperatively. Excision or biopsy would remain necessary to exclude the possibility of malignancy with subsequent pathologic evaluation ultimately providing the definitive diagnosis.
Conclusion
Extradigital glomus tumors represent a rare etiology for soft tissue mass and in isolation, the imaging findings are nonspecific making prospective diagnosis difficult. MRI characteristics, however, remain fairly consistent (relatively homogenous T1 iso-to-hypointensity, relatively homogenous T2 hyperintensity, and strong postcontrast enhancement) in the published literature and are similar to the more classic subungual location. If alternative differential diagnoses can be excluded, clinical correlation with a history of prominent pain/focally tender mass may facilitate including extradigital glomus tumor in the differential preoperatively. Complete surgical excision with pathologic evaluation provides both definitive diagnosis and treatment.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Baek H., Lee S., Cho K., Choo J., Lee S., Lee H. Subungual tumors: clinicopathologic correlation with US and MR imaging findings. Radiographics. 2010;30:1621–1636. doi: 10.1148/rg.306105514. [DOI] [PubMed] [Google Scholar]
- 2.Balaram A., Hsu A., Rapp T., Mehta V., Bindra R. Large solitary glomus tumor of the wrist involving the radial artery. Am J Orthop. 2014;43(12):567–570. [PubMed] [Google Scholar]
- 3.Schiefer T., Parker W., Anakwenze O., Amadio P., Inwards C., Spinner R. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81(10):1337–1344. doi: 10.4065/81.10.1337. [DOI] [PubMed] [Google Scholar]
- 4.Chim H., Lahiri A., Chew W. Atypical glomus tumour of the wrist: a case report. Hand Surg. 2009;14(2-3):121–123. doi: 10.1142/S0218810409004347. [DOI] [PubMed] [Google Scholar]
- 5.Folpe A., Fanburg-Smith J., Miettinen M., Weiss S. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25(1):1–12. doi: 10.1097/00000478-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 6.White C., Jewer D. Atypical presentation of a glomus tumour: a case report. Can J Plast Surg. 2006;14(4):237–238. doi: 10.1177/229255030601400402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Geertruyden J., Lorea P., Goldschmidt D., de Fontaine S., Schuind F., Kinnen L. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21(2):257–360. doi: 10.1016/s0266-7681(96)80110-0. [DOI] [PubMed] [Google Scholar]
- 8.Lee S., Le H., Munk P., Malfair D., Lee C., Clarkson P. Glomus tumour in the forearm: a case report and review of MRI findings. JBR-BTR. 2010;93:292–295. doi: 10.5334/jbr-btr.342. [DOI] [PubMed] [Google Scholar]
- 9.Glazebrook K., Most M., Schiefer T., Inwards C., Sim F. Multiple glomus tumors of the lower leg. J Ultrasound Med. 2010;29:667–670. doi: 10.7863/jum.2010.29.4.667. [DOI] [PubMed] [Google Scholar]
- 10.Drape J., Idy-Peretti I., Goettmann S., Wolfram-Gabel R., Dion E. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995;195(2):507–515. doi: 10.1148/radiology.195.2.7724775. [DOI] [PubMed] [Google Scholar]
- 11.Theumann N., Goettmann S., Le Viet D., Resnick D., Chung C. Recurrent glomus tumors of fingertips: MR imaging evaluation. Radiology. 2002;223(1):143–151. doi: 10.1148/radiol.2231010977. [DOI] [PubMed] [Google Scholar]
- 12.Venugopal P. Extradigital glomus tumor–a rare cause for undiagnosed chronic pain in unusual sites. Indian J Surg. 2015;77(Suppl 3):910–912. doi: 10.1007/s12262-014-1062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong T., Harik L., Macaulay W. Extradigital glomus tumor in the knee: excision with ultrasound guided needle localization. Skeletal Radiology. 2015;44(11):1689–1693. doi: 10.1007/s00256-015-2202-9. [DOI] [PubMed] [Google Scholar]
- 14.Goncalves R., Lopes A., Julio C., Durao C., Andrade de Mello R. Knee glomangioma: a rare location for a glomus tumor. Rare Tumors. 2014;6(4):5588. doi: 10.4081/rt.2014.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takei T., Nalebuff E. Extradigital glomus tumor. J Hand Surg Br. 1995;20B:409–412. doi: 10.1016/s0266-7681(05)80105-6. [DOI] [PubMed] [Google Scholar]
- 16.Ergun T., Lakadamyali H., Derincek A., Tarhan N., Ozturk A. Magnetic resonance imaging in the visualization of benign tumors and tumor-like lesions of hand and wrist. Curr Probl Diagn Radiol. 2010;39(1):1–16. doi: 10.1067/j.cpradiol.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Teh J., Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol. 2007;80(949):47–63. doi: 10.1259/bjr/53596176. [DOI] [PubMed] [Google Scholar]