Abstract
Athletes are at increased risk of developing soft-tissue lesions of the lower limbs. Although the majority of these will be benign, the differential diagnosis is broad and increasingly, doctors are turning to magnetic resonance imaging (MRI) as a first-line investigation when presented with these sorts of lesions, both to narrow the differential diagnosis and exclude malignancy. We report the case of a 28-year-old Caucasian man who presented with 2 soft-tissue lesions of the right foot. History and examination of the nodules fitted with a diagnosis of surfers' knots, an unusual form of acquired, benign, connective tissue nodule that may appear over the tibial tuberosities, dorsum of the feet, and occasionally on the chest of surfers in association with repetitive microtrauma during surfing. MRI findings were consistent with this diagnosis with both lesions exhibiting T1 hypointensity and speckled T2 hypointensity with no significant blooming artifact on gradient echo imaging. When imaged with gadolinium, they demonstrated only mild contrast enhancement. MRI is a valuable tool when investigating athletes with soft-tissue lesions over the lower limbs where the possibility of malignancy must be addressed. In selected cases, MRI may be sufficient to permit a conservative approach to the management of these patients.
Keywords: Case report, Surfer, Knot, Nodule, Lump
Introduction
Surfers' knots (also known as surfers' knobs or surf bumps) are a form of acquired fibrotic connective tissue nodule that develop in response to repetitive low-grade trauma, typically over the tibial tuberosities, dorsum of the feet, and occasionally on the chest of surfers [1]. They were first reported in the 1960s in warmer regions when surfers predominantly paddled larger, heavier surfboards while sitting on their knees and where wetsuits that protected knees and ankles were less common [2]. According to the literature published since then, surfers' knots are nearly always benign, resolving in most cases with cessation or modification of activity. Just occasionally, surfers' knots become permanent, infected, and/or painful [3]. In these circumstances, they can be surgically excised [4].
The incidence of surfers' knots has substantially declined since the short-board revolution, in which average surfboard dimensions fell from 290 × 56 cm, to just 198 × 51 cm, presumably because surfers began paddling prone rather than on their knees [5], [6]. As a consequence, surfers' knots may now present a diagnostic dilemma to doctors who encounter them. The differential diagnosis for soft-tissue nodules on the lower extremities is wide and includes tophaceous gout, rheumatoid arthritis nodules, foreign body granulomas, synovial cysts, pigmented villonodular synovitis, Morton's neuroma, lipoma, soft-tissue chondroma, synovial sarcoma, leiomyosarcoma, and giant cell tumor of tendon sheath [7]. Histologic analysis is required for definitive diagnosis in many cases [8]. An increasingly common alternative approach in selected cases is to use magnetic resonance imaging (MRI) as a first-line investigation both to narrow the differential diagnosis and in particular to exclude malignancy [9]. In support of this approach, we report a case in which MRI was used to exclude aggressive pathology and support the unusual diagnosis of surfers' knots.
Clinical presentation
A 28-year-old Caucasian man presented to an outpatient orthopedic clinic in Geelong, Victoria, Australia, in May 2015 with 2 soft-tissue “lumps” on his right foot of uncertain significance (Fig. 1). The largest of these, located medially at the base of the right great toe arose 5 years before presentation. The smaller of the 2 masses, on the medial aspect of the patient's midfoot, arose 10 years before presentation. The patient attributed both foot lesions to repeated microtrauma during surfing, explaining that when he flexed his knee beyond 90 degrees while riding a wave his foot rubbed against his 180 × 45-cm2-epoxy fiberglass-reinforced board. Both lumps had grown slowly since first noticed but had changed size minimally over the past few years. From time-to-time, the growths made shoes feel tight, but they were never a source of significant pain, never bled, and never showed signs of infection.
Fig. 1.
Appearance of a 28-year-old man's right foot exhibiting 2 lumps for investigation. The first and largest of these lumps is evident medially over the base of the great toe, at the level of the first metatarsalphalangeal joint. The smaller lesion appears over the medial aspect of the patient's midfoot, in approximation with the navicular.
On further questioning, the patient described 2 further lumps, located on the anterior surface of his chest. Again, the patient attributed the lumps to microtrauma during surfing. The chest lumps became more pronounced after surfing trips to Bali where the patient surfed without use of a wetsuit.
The young man had surfed between 2 to 3 times per week for 2 to 3 hours at a time, since the age of 13 years. He had no medical history, did not take any medication regularly, had no allergies, and had never smoked. He denied a family history of connective tissue disorders or malignancy and had worked only as an electrician since the age of 18 years.
On examination, a 4 × 2-cm nodule was noted medial and plantar to the first right metatarsophalangeal joint (MTPJ). A second nodule was located medial to the right navicular and measured approximately 3 × 1 cm in size. Both lesions were smooth, nontender, soft but nonfluctuant and free of overlying erythema or skin breakdown. The chest lumps were smaller, the largest measuring less than 1 cm in diameter and were located in the midclavicular line over the 12th ribs bilaterally.
Imaging findings
MRI of the right foot was performed on a Siemens Treo 3 Tesla scanner (Erlangen, Germany) initially without, then with intravenous gadolinium to help elucidate the nature of the foot lumps and rule out malignancy. The larger foot lesion abutting the first MTPJ measured 36 × 22 mm and exhibited ill-defined T1 hypointensity and speckled T2 hypointensity (Fig. 2). No high T2 signal or fluid signal was present. There was no significant blooming artefact to suggest hemosiderin deposition. No joint erosions, infiltration of adjacent joints, or other structures was evident. No marrow signal abnormalities were seen. Only mild enhancement was noted after contrast administration, similar to adjacent soft tissues. A small joint effusion of the first MTPJ was noted, but the joint otherwise appeared normal. The smaller foot nodule over the navicular measured 27 × 11 mm and exhibited similar signal characteristics (Fig. 3).
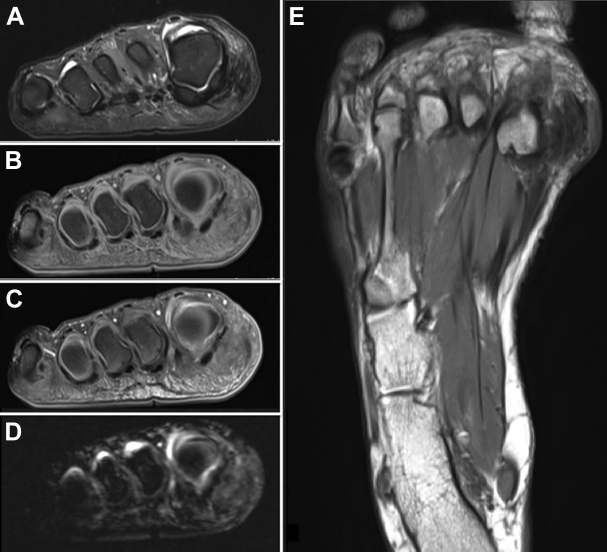
Fig. 2.
MRI appearance of surfers' knot medial to the patients' first MTPJ of the right foot. (A) Coronal T2-fat-saturated acquisition; (B) coronal T1-fat-saturated acquisition; (C) coronal T1-fat-saturated, postcontrast acquisition; (D) coronal gradient echo acquisition; (E) axial proton density-weighted acquisition. The lesion exhibits ill-defined T1 hypointensity and speckled T2 hypointensity, with only mild enhancement after contrast administration. No blooming artifact is evident on gradient echo imaging.
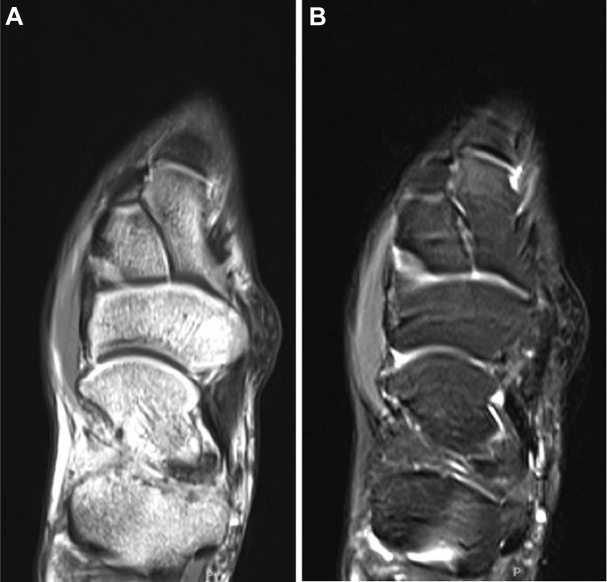
Fig. 3.
MRI appearance of surfers' knot medial to the patients' navicular. (A) Axial proton density-weighted acquisition; (B) Axial T2-fat-saturated acquisition. The lesion exhibits ill-defined T1 hypointensity and speckled T2 hypointensity similar to the metatarsophalygeal lesion.
Discussion
The majority of neoplasms of the foot and ankle are benign [6], [9]. As a result, malignant tumors are at increased risk of being missed especially in younger patients with long-standing symptoms [9]. Where the potential for malignancy exists but is unlikely, MRI offers clinicians a means of investigating tumor-like lesions without the risks associated with biopsy or surgical resection. Most important, although MRI lacks the specificity of biopsy and histologic analysis, MRI imaging features can frequently help in correctly distinguishing malignant from benign lesions [6], [7].
In our study, the absence of high T2 signal or marked contrast enhancement argues strongly against synovial sarcoma, the most common malignant tumor of the foot and ankle [9], [10]. Clear-cell carcinoma, a slow growing malignancy with a predilection for the lower extremities in younger adults is also unlikely in view of the absence of either hyperintensity on T1-weighted images or an aggressive growth pattern [6], [9]. Deep fibromatosis, another rare but potential malignant differential is unlikely in view of the lack of invasion and low T2-signal intensity [9]. Other malignancies, such as liposarcoma, plexiform fibrohistiocytic tumor, and extraskeletal chondosarcoma do not fit the morphologic appearance of our lesions (Table 1) [10].
Table 1.
Reported MR features for selected benign foot lesions.
| Lesion type | T1-weighted intensity | T2-weighted intensity | Contrast enhancement | Other MR features |
|---|---|---|---|---|
| Gouty tophi | Isointense-to-muscle [11], homogenously low-to-intermediate T1 signal | Heterogenous low-to-intermediate T2 signals [10], [11] | Variable appearance with gadolinium [11] | First metatarsophalyngeal or other joint may show evidence of articular gout including articular erosions, cartilage sparing, periarticular edema, joint effusions [10], [11] |
| Rheumatoid nodules | Low T1 signal [12] | High T2 signal [12] | — | Features of rheumatoid arthritis such as joint effusions, marrow edema, subchondral cyst, cartilage thinning, and pannus formation may be present [12]. Typically nodules appear in patients with advanced disease who have concommitant corticosteroid-induced osteopenia [12] |
| Pigmented villonodular synovitis | Inhomogenous low T1 signal [13] | Low T2 signal [13] | — | Predilection for location between digits and characteristic blooming on gradient echo imaging [8] |
| Hemangioma | Low-to-intermediate T1 signal [8] | High T2 intensity [8] | Marked enhancement [8] | Often appear morphologically as multilobed, septate lesions [8] |
| Angiomyoma | Low T1 signal [8] | Heterogenous T2 signal [8], [13] | — | Hypointense lining may be evident due to presence of cystic capsule [9] |
| Plantar fibromatosis | Iso-to-low T1 signal | Low-to-intermediate T2 signal [14] | Variable enhancement [14] | Nodules afflict plantar aponeurosis [14] |
| Morton's neuroma | Low-to-intermediate T1 signal [8] | Low T2 signal [8] | Mild contrast enhancement [12] | Perineurally located usually [5], classically at metatarsal head of second and third digits [8], [9] |
Surfers' knots can be differentiated from most other benign foot lesions because they exhibit ill-defined T1 hypointensity and speckled T2 hypointensity, with only mild enhancement after contrast administration. They are distinguished from pigmented villonodular synovitis, which exhibits similar signal characteristics, because blooming artifact is not evident on gradient echo imaging.
Common benign causes of foot nodules such as gout, rheumatoid arthritis, and pigmented villonodular synovitis were also effectively excluded by MRI. Gouty tophi would be expected to exhibit periarticular erosions and synovial thickening whereas rheumatoid nodules typically exhibit high rather than low signal [12]. Pigmented villonodular synovitis, a reasonable differential given it is associated with repeated trauma and its prevalence in 20- to 40-year olds, usually presents with susceptibility on gradient echo sequences and bone erosions (Table 2) [10].
Table 2.
Reported MR features for selected malignant foot lesions.
| Lesion type | T1-weighted intensity | T2-weighted intensity | Contrast enhancement | Other MR features |
|---|---|---|---|---|
| Synocial sarcoma | Inhomogenous low-to-intermediate T1 signal [8], [13] | Hyperintense, isointense, and hypointense T2 signal [13] | Intense enhancement where tissues remain viable [8], [13] | Relatively well-defined lesions typically found intermuscularly [5], with peritendinous growth [1]. May demonstrate infiltrative growth, and may exhibit septated areas of hemorrhage and necrosis [8], [13]. |
| Clear-cell carcinoma | Increased signal on T1 relative to muscle [8] | Variable T2 signal [8] | Strong and diffuse enhancement [10] | Preponderance for heels, of young to middle aged adults [10]. Often well-defined and relatively homogenous on MR 10; shortening of T1 and T2 relaxation times may be seen where melanin is present [13]. |
| Deep fibromatosis | Low-to-intermediate T1 signal [8] | High T2 signal [8] | Moderate-to-marked enhancement [8], [13] | Aggressive growth pattern, no metastases, patients typically in their third decade [8], [13]. Characteristic intralesional bands of low signal that do not enhance are seen on all pulse sequences [8], [13]. |
| Liposarcoma | High T1 signal for lipomatous tumor portions and isointense to muscle for nonlipomatous portions [10] | T2 intensities higher than fat for nonlipomatous tumor portions [10] | — | MR appearance varies throughout tumor reflecting inclusion of lipomatous and nonlipomatous portions. The degree of lipomatous tumor can change with the degree of differentiation [10]. |
| Plexiform fibrohistiocytic tumor | Low-to-intermediate T1 signal [10] | Low-to-intermediate T2 signal [10] | — | Appear in younger patients, as if composed of small nodules of tumor that rarely metastasize [10]. |
| Extraskeletal chondrosarcoma | Low-to-isointense T1 signal [10] | Variable T2 signal but usually higher than muscle [10] | Heterogenous enhancement [10] | Appear as extraskeletal cartilage. More common in middle aged patients though rare in feet [10]. |
Surfers' knots do not exhibit aggressive features such as joint erosions, infiltration of adjacent joints or other structures, marrow signal abnormalities, or marked contrast enhancement.
When biopsied, surfers' knots are generally found to contain thickening of the reticular dermis as a result of increased deposition of collagen [7], [15]. Proliferation of collagen bundles may come at the cost of perieccrine and subcutaneous adipose tissue [15]. Epidermal hyperkeratosis and acanthosis are sometimes also noted [7]. Increased collagen bundling may be accompanied by increases in vascular elements, though this feature is also variable [7], [16]. The MRI findings that we report are consistent with the MRI findings for collagenoma of the upper limb [17], supporting a diagnosis of surfers' knots.
Although not confirmed histologically, the history and examination findings presented here also strongly suggested a diagnosis of surfers' knots. In this case, the association of surfers' knots with short-board surfing is not classic but likely reflects the prevalence of short-board surfing and that long-board surfers now rarely paddle in a kneeling position. This is a good example of the importance of relevant clinical history for the consulting clinician and the radiologist. In conjunction with MRI findings being consistent with the known histology of surfers' knots and not demonstrating features concerning for an aggressive process, conservative management with serial observation of these lesions is sound, particularly given the absence of significant symptoms associated with the foot lumps. Accordingly, the patient described here is under surveillance.
As access to MRI improves, and the body of information on the MRI appearance of various lower limb lesions grows, assessing lower limb lesions primarily via MRI seems an increasingly sound approach to narrow the differential diagnosis. In selected cases, it may be sufficient to prevent unnecessary invasive histologic or surgical interventions.
Learning points
-
(1)
Surfers' knots are a rare form of acquired connective tissue nodule that develop over the tibial tuberosities, dorsum of the feet, and occasionally on the chest of surfers in response to repetitive low-grade trauma during long- and short-board surfing.
-
(2)
Surfers' knots display T1 hypointensity and speckled T2 hypointensity without significant contrast enhancement, joint erosions, infiltration of adjacent joints, or other malignant features when imaged on MRI.
-
(3)
In selected cases, MRI may be used as a first-line investigation when presented with lower limb lesions and may be sufficient to prevent unnecessary invasive histologic or surgical interventions.
Footnotes
Consent: Written informed consent was obtained from the patient for publication of this case report including accompanying images.
Competing Interests: The authors declare that they have no competing interests.
Authors' contributions: L.J.M. was responsible for patient history and examination, prepared images for publication, drafted the manuscript, and revised it according to the critical appraisal of all contributors. A.T. made initial contact with patient, was responsible for acquisition of magnetic resonance images, and participated in manuscript review and revision. A.W. conceived of the case study, was instrumental in analysis of imaging, as well as manuscript review and revision. All authors read and approved the final manuscript.
References
- 1.Tashima C.K. Letter: Surfer's chest knots. JAMA. 1973;226(4):468. doi: 10.1001/jama.1973.03230040042024. [DOI] [PubMed] [Google Scholar]
- 2.Swift S. Surfers' “knots”. JAMA. 1965;192:223–224. doi: 10.1001/jama.1965.03080160043011. [DOI] [PubMed] [Google Scholar]
- 3.Cragg J. Surfers' nodules. Br J Clin Pract. 1973;27(11):418–419. [PubMed] [Google Scholar]
- 4.Cohen P.R., Eliezri Y.D., Silvers D.N. Athlete's nodules. Treatment by surgical excision. Sports Med. 1990;10(3):198–203. doi: 10.2165/00007256-199010030-00005. [DOI] [PubMed] [Google Scholar]
- 5.Freeman J., MacGillivray G., Kampion D., Witzig J. 2011. Shortboard revolution, in The Encyclopaedia of Surfing.http://encyclopediaofsurfing.com/entries/shortboard-revolution [accessed 29.03.16] [Google Scholar]
- 6.Stoner R. 2011. Surfer's knots, in The Encyclopaedia of Surfing.http://encyclopediaofsurfing.com/search-results/?search=knots&send= [accessed 12.06.15] [Google Scholar]
- 7.Cohen P.R., Eliezri Y.D., Silvers D.N. Athlete's nodules: sports-related connective tissue nevi of the collagen type (collagenomas) Cutis. 1992;50(2):131–135. [PubMed] [Google Scholar]
- 8.Waldt S., Rechl H., Rummeny E.J., Woertler K. Imaging of benign and malignant soft tissue masses of the foot. Eur Radiol. 2003;13(5):1125–1136. doi: 10.1007/s00330-002-1604-y. [DOI] [PubMed] [Google Scholar]
- 9.Bancroft L.W., Peterson J.J., Kransdorf M.J. Imaging of soft tissue lesions of the foot and ankle. Radiol Clin North Am. 2008;46(6):1093–1103. doi: 10.1016/j.rcl.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Gentili A., Sorenson S., Masih S. MR imaging of soft-tissue masses of the foot. Semin musculoskel radiol. 2002;6(2):141–152. doi: 10.1055/s-2002-32360. [DOI] [PubMed] [Google Scholar]
- 11.Jelinek J., Pearl A.B., Kominsky S.J., Schultz P.M. Magnetic resonance imaging of the foot. Rheumatologic disorders mimicking osteomyelitis. J Am Podiatr Med Assoc. 1996;86(5):228–231. doi: 10.7547/87507315-86-5-228. [DOI] [PubMed] [Google Scholar]
- 12.Khoo J.N., Tan S.C. MR imaging of tophaceous gout revisited. Singapore Med J. 2011;52(11):840–846. [PubMed] [Google Scholar]
- 13.Woertler K. Soft tissue masses in the foot and ankle: characteristics on MR imaging. Semin Musculoskelet Radiol. 2005;9(3):227–242. doi: 10.1055/s-2005-921942. [DOI] [PubMed] [Google Scholar]
- 14.Blacksin M.F., White L.M., Hameed M., Kandel R., Patterson F.R., Benevenia J. Granular cell tumor of the extremity: magnetic resonance imaging characteristics with pathologic correlation. Skeletal Radiol. 2005;34(10):625–631. doi: 10.1007/s00256-005-0925-8. [DOI] [PubMed] [Google Scholar]
- 15.Kieliszak C.R., Junkins-Hopkins J.M. Athlete's nodule in a figure skater: an unusual presentation. Am J Dermatopathol. 2015;37(2):e21–e25. doi: 10.1097/DAD.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 16.Erickson J.G., von Gemmingen G.R. Surfer's nodules and other complications of surfboarding. JAMA. 1967;201(2):134–136. [PubMed] [Google Scholar]
- 17.Al-Qattan M.M. Collagenoma in a child with tuberous sclerosis complex causing carpal tunnel syndrome and thumb overgrowth: case report. J Hand Surg Am. 2013;38(10):1976–1979. doi: 10.1016/j.jhsa.2013.07.004. [DOI] [PubMed] [Google Scholar]