Abstract
A four-day-old boy presented with persistent bilious vomiting, bloody stained stool, and mild abdominal distension. Transabdominal ultrasound demonstrated a round soft-tissue mass-like structure in the right upper quadrant. With color Doppler ultrasound, the whirlpool sign was observed. Abdominal radiograph showed nonspecific findings. Upper gastrointestinal series revealed upper gastrointestinal tract obstruction at the level of distal duodenum. The diagnosis of intestinal malrotation with midgut volvulus was established and the treated surgically. Intestinal malrotation is congenital abnormal positioning of the bowel loops within the peritoneal cavity resulting in abnormal shortening of mesenteric root that is predisposed to midgut volvulus. Neonates and infants with persistent bilious vomiting should undergo diagnostic workup and preferably ultrasound as the first step. With classic sonographic appearance of whirlpool sign, even further imaging investigations is often not needed, and the surgeon should be alerted to plan surgery.
Keywords: Intestinal malrotation, Midgut volvulus, Upper gastrointestinal obstruction
Case presentation
A four-day-old boy presented with persistent bilious vomiting, bloody stained stool, and mild abdominal distension. The neonate was dehydrated and looked ill. He weighed 3.2 kg, and his vital signs were as follows: temperature, 38°C; pulse rate, 162/min; and respiratory rate, 59/min.
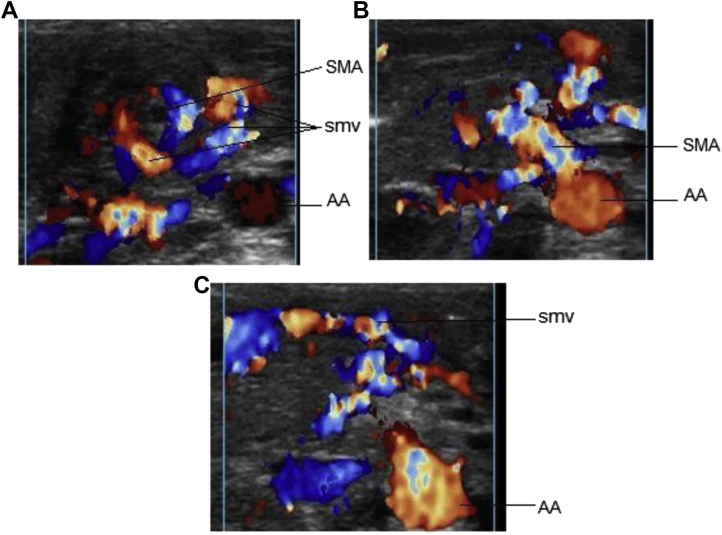
Abdominal ultrasound demonstrated a round soft-tissue mass-like structure in the right upper quadrant (Fig. 1A). With color Doppler ultrasound, the superior mesenteric artery (SMA) was seen coming from abdominal aorta and going to the center of this round mass-like structure (Figs 1A and B). Superior mesenteric vein (SMV) was turning around SMA in a clockwise fashion, and then following its course toward portal vein (Figs 1A and C).
Fig. 1.
Color Doppler abdominal ultrasound with high frequency linear transducer: superior mesenteric artery (SMA) arises from abdominal aorta (AA) (B) and goes to the center of a round mass-like structure—the twisted mesentery. SMA turns around superior mesenteric vein (SMV) in a clockwise fashion (A) than follows its way toward the portal vein (C).
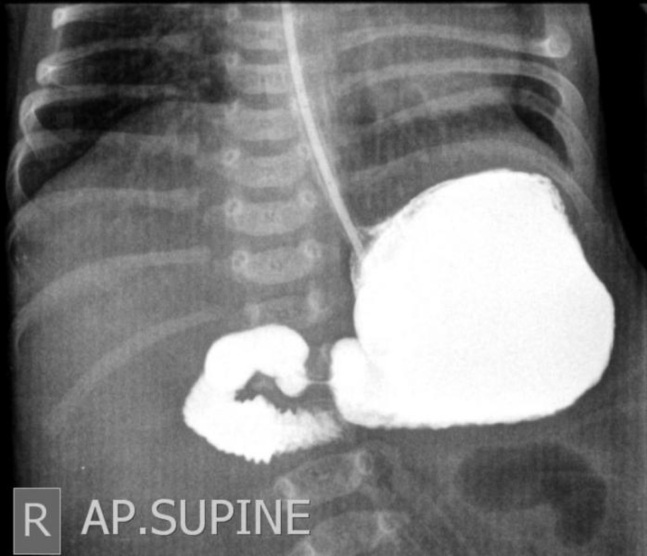
Abdominal radiograph showed nonspecific findings; no colonic gas was seen in right hemiabdomen (Fig. 2).
Fig. 2.

Anteroposterior abdominal radiograph: no colonic gas in right hemiabdomen (as the duodenal loops located in the right hemiabdomen). Colonic gas is seen in the left hemiabdomen.
Upper gastrointestinal (GI) series depicted that the stomach and proximal parts of duodenum were slightly distended (Fig. 3). No distal passage of contrast was seen to jejunal loops. The duodenojejunal flexure (DJF), however, not opacified during the examination but can be estimated that it is located lower than its normal position.
Fig. 3.
Upper GI series: stomach and proximal 3 parts of duodenum are slightly distended. The DJF, however, not opacified but can be estimated that it is located lower than its normal position. No distal contrast passage.
With these sonographic and radiographic features, the diagnosis of intestinal malrotation and midgut volvulus was established, and the patient underwent surgery.
During the open surgery procedure, the entire intestine was seen free in abdominal cavity. Mild distension of stomach and duodenum was observed while jejunum and proximal ileal loops together with peritoneal folds made a mass-like structure. These loops were rotated around mesentery in a counterclockwise direction representing midgut malrotation and volvulus. No ladd bands were seen. Necrotic changes in the some of the proximal jejunal loops were noted (Fig. 4). Colons were collapsed and mainly located in the right hemiabdomen. Cecum was also located in the left upper quadrant.
Fig. 4.
Necrotic jejunal loops twisted around the mesentery.
The volvulus was reduced surgically, the peritoneal folds were incised, approximately 20 cm of gangrenous jejunal loops were resected and subsequent jejunojejunostomy performed. Cecopexy was also performed for the free cecum lying in the paravertebral region. No appendectomy was done.
Patient was followed for 1 month, and no serious problem or complication was observed. Thereafter, the patient was lost to follow-up.
Discussion
Background
Bilious vomiting in neonatal period is primary sign of intestinal obstruction. The main causes for neonatal intestinal obstruction resulting in bilious vomiting are duodenal atresia, jejunoileal atresia, midgut malrotation and volvulus, necrotizing enterocolitis, and meconium ileus [1].
Intestinal malrotation is described as abnormal positioning of the bowel loops within the peritoneal cavity in the intrauterine life [2]. It is caused by defective rotation of primitive intestinal loop around the axis of SMA during embryogenesis [3] that results in abnormal short mesenteric root which predisposes small bowel to twist around it and lead to in midgut volvulus [4].
Clinical perspective
Classic clinical presentation of malrotation in a newborn is bilious vomiting with or without abdominal distention [2]. Its major complication; the midgut volvulus results in proximal bowel obstruction and ischemia that may occasionally present with bloody stool [5].
Rapid imaging workup is needed in neonates presenting with these symptoms.
Imaging perspective
The imaging workup of neonatal bilious vomiting classically consists of plain abdominal radiograph and/or contrast studies [1]. However, due to limited access to prenatal sonographic screening in our country (Afghanistan), we usually perform abdominal ultrasound for all neonates and infants suspected for any intra-abdominal abnormality, not only to detect the main problem (in this case the cause of bilious vomiting) but also to look for simultaneous abnormalities.
In cases midgut volvulus, ultrasound can be the first noninvasive, radiation free, mostly available, and inexpensive imaging modality to start with. It can give clue about abnormal position of SMA and SMV; as in 60% of individuals the relative positions of SMV and SMA are reversed in midgut malrotation [6], [7]. More important, it can depict the classic sonographic appearance of midgut volvulus: “whirlpool sign.”
Whirlpool sign can be detected on transverse abdominal sonograms of newborns and young infants with swirling shape created by SMV and mesentery wrapping around SMA in a clockwise direction [3], [8].
Findings of radiograph are not so specific, but it can give clues about proximal bowel obstruction as well as abnormal location of small and large intestine.
Conventionally, the diagnosis of malrotation is made by upper GI contrast studies documenting the position of the DJF.
Patients with malrotation will have a DJF to the right of or below the normal position that is to the left of vertebral pedicles at the level of duodenal bulb on an anteroposterior view of a well-positioned patient.
The associated obstruction may be complete or partial so further passage of contrast to the small bowel may not be sometimes seen.
The pathognomonic feature of volvulus on upper GI series is “corkscrew pattern” of the twisted duodenum and jejunum [9].
Outcome
Intestinal malrotation due to its life-threatening complication; midgut volvulus if not promptly diagnosed and treated, can lead to death or a lifelong dependence on total parenteral nutrition in survivors so surgical correction is the mainstay of treatment.
Take home message
Neonates and infants with persistent bilious vomiting should undergo diagnostic workup and preferably ultrasound as the first step. For neonates with classic appearance of whirlpool sign, even further imaging investigations is often not needed, and the surgeon should be alerted to plan surgery [3].
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Kimura K., Loening-Baucke V. Bilious vomiting in the newborn: rapid diagnosis of intestinal obstruction. American Family Physician. 2000;61(9):2791–2798. [PubMed] [Google Scholar]
- 2.Applegate K.E., Anderson J.M., Klatte E.C. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26(5):1485–1500. doi: 10.1148/rg.265055167. [DOI] [PubMed] [Google Scholar]
- 3.Epelman M. The whirlpool sign. Radiology. 2006;240(3):910–911. doi: 10.1148/radiol.2403040370. [DOI] [PubMed] [Google Scholar]
- 4.Peterson C.M., Anderson J.S., Hara A.K., Carenza J.W., Menias C.O. Volvulus of the gastrointestinal tract: appearances at multimodality imaging. Radiographics. 2009;29(5):1281–1293. doi: 10.1148/rg.295095011. [DOI] [PubMed] [Google Scholar]
- 5.Knipe H, Gaillard F. Midgut volvulus. Available at: http://radiopaedia.org/articles/midgut-volvulus. (accessed June 11, 2016).
- 6.Zerin J.M., DiPietro M.A. Mesenteric vascular anatomy at CT: normal and abnormal appearances. Radiology. 1991;179(3):739–742. doi: 10.1148/radiology.179.3.2027985. [DOI] [PubMed] [Google Scholar]
- 7.Zerin J.M., DiPietro M.A. Superior mesenteric vascular anatomy at US in patients with surgically proved malrotation of the midgut. Radiology. 1992;183(3):693–694. doi: 10.1148/radiology.183.3.1584922. [DOI] [PubMed] [Google Scholar]
- 8.Pracros J.P., Sann L., Genin G., Tran-Minh V.A., Morin de Finfe C.H., Foray P. Ultrasound diagnosis of midgut volvulus: the “whirlpool” sign. Pediatr Radiol. 1992;22(1):18–20. doi: 10.1007/BF02011603. [DOI] [PubMed] [Google Scholar]
- 9.Buonomo C., Taylor G.A., Share J.C., Kirks D.T. In: Practical pediatric imaging. Gastrointestinal tract. Kirks D.R., Griscom N.T., editors. Lippincott-Raven; Philadelphia, PA: 1998. pp. 857–865. [Google Scholar]