Abstract
Objective To examine whether patients invited to review their clinicians’ notes continue to access them and to assess the impact of reminders on whether patients continued to view notes.
Materials and methods We followed OpenNotes trial participants for 2 years at Beth Israel Deaconess Medical Center (BIDMC) and Geisinger Health System (GHS). Electronic invitations alerting patients to signed notes stopped at GHS after year 1, creating a natural experiment to assess the impact of reminders. We used generalized linear models to measure whether notes were viewed within 30 days of availability.
Results We identified 14 360 patients (49 271 visits); mean age 52.2; 57.8% female. In year 1, patients viewed 57.5% of their notes, and their interest in viewing notes persisted over time. In year 2, BIDMC patients viewed notes with similar frequency. In contrast, GHS patients viewed notes far less frequently, a change starting when invitations ceased (RR 0.29 [0.26–0.32]) and persisting to the end of the study (RR 0.20 [0.17–0.23]). A subanalysis of BIDMC patients revealed that black and other/multiracial patients also continued to view notes, although they were overall less likely to view notes compared with whites (RR 0.75 [0.67–0.83] and 0.93 [0.89–0.98], respectively).
Discussion As millions of patients nationwide increasingly gain access to clinicians’ notes, explicit email invitations to review notes may be important for fostering patient engagement and patient-doctor communication.
Conclusion Note viewing persists when accompanied by email alerts, but may decline substantially in their absence. Non-white patients at BIDMC viewed notes less frequently than whites, although their interest also persisted.
Keywords: patient engagement, patient activation, electronic health records, reminder systems, medical records
Fostering active and constructive patient engagement is central to many efforts designed to improve the quality of healthcare.1,2,3 However, many factors hinder patients from taking charge of their health and healthcare, and among them is suboptimal recall and learning associated with a clinical encounter. For example, patients surveyed immediately after visiting their doctors forgot between 40 and 80% of the medical information provided by the doctor.4,5 Partly intended to improve patient engagement and patient-doctor communication, Meaningful Use legislation has invested billions to incentivize the use of electronic health records and online patient portals, including communication tools such as after-visit summaries.6 However, after-visit summaries are often sparse and have not led to improved patient recall of content or satisfaction with the information provided.7
In 2010, with the goal of improving communication and patient engagement, 105 primary care physicians (PCPs) at Beth Israel Deaconess Medical Center (BIDMC) in Boston, Massachusetts, Geisinger Health System (GHS) in Danville, Pennsylvania, and Harborview Medical Center (HMC) in Seattle, Washington volunteered to invite 19 371 of their patients registered on portals to review their signed visit notes, and to do so through individual emailed alerts.8,9 Initial findings of the project, called the OpenNotes trial, demonstrated considerable patient enthusiasm, improved recall of the medical plan, self-reported clinical benefits, and little impact on PCP workflow. Since publication, many providers have moved to offer fully transparent records to their patients, and in 2015 more than 5 million Americans have ready access to their clinicians’ notes.10 However, while the original trial demonstrated substantial initial enthusiasm among patients, whether interest in viewing notes persists beyond the first visit or beyond the start of the trial was not known.
To address this question, we examined note-viewing behavior among groups of patients within two of the three original cohorts in the initial OpenNotes research and evaluation project. We developed two hypotheses: (1) As novelty wore off, interest in viewing notes would decline after the first visit note and over 2 years’ time and (2) patients who received email alerts when their notes became available would view notes more frequently.
MATERIALS AND METHODS
At each of the three OpenNotes sites, patients registered on secure electronic portals received electronic messages inviting them to read their primary care doctors’ notes. Institutional upgrades to the electronic medical record system at HMC caused the site to revoke access to notes after 1 year (it is now resuming), but with no doctors opting out of the project, BIDMC and GHS continued to allow patients to view their notes at the end of the 1-year trial period. Patients received two email invitations to view each signed visit note, once within 24 h of the doctor signing the note, and a second one 5–7 days before a next scheduled visit, accompanied by a suggestion to review the note in preparation for their upcoming visit (See the Online Supplement for our patient message templates). During the study period, BIDMC required doctors to sign their notes within 30 days of the visit, and GHS required doctors to sign their notes within 48 h of the visit. At GHS, notifications were programmed to stop automatically after 1 year. Therefore, in year 2, GHS patients no longer received electronic invitations. While notes continued to be visible, patients were not notified that the reminders would cease.
In this study, we evaluated patients whose primary care doctors participated in the intervention arm of the OpenNotes trial at BIDMC and GHS. While our original study9 included any patient with a note available (including non-visit-based telephone encounters or letters that PCPs wrote to their patients; e.g., regarding laboratory test results), for this inquiry we included only patients who had one or more visits during the trial period (June 2010 to June 2011 at BIDMC, and July 2010 to July 2011 at GHS), and in the 1 year following the trial’s completion (June 2011 to June 2012). Due to a software upgrade of the EHR at GHS after 11 months of year 2, OpenNotes user data became unavailable. Therefore, the second year of the GHS analysis period ends after 11 instead of 12 months. Both the BIDMC Committee on Human Studies and the GHS Institutional Review Board approved this study.
Data Collection
We used information systems data from the respective patient portals to identify which notes patients accessed, when they accessed them, and how many times they accessed each note. We used claims and online registration records to obtain demographic and clinical data, including visit dates and ICD-9-CM diagnostic codes associated with each visit. Administrative race data was obtained by clinical registration staff, who categorized patients as either white, black or other/multiracial.
Primary Outcome: Note Viewing
The primary outcome was notes viewed, defined as whether the patient viewed the note within 30 days of its availability. We chose to focus on the period soon after the visit, hypothesizing that this is likely the most important time to influence adherence to the medical plan.
Exposures of Interest
With the first doctor visit serving as the patient’s first exposure to OpenNotes, we evaluated whether note viewing persists beyond the first visit, as well as whether viewing persists over time. For this, we examined 3-month time intervals over the 2-year study period. Because electronic notifications to view notes stopped at GHS after year 1 and persisted at BIDMC, we used this “natural experiment” to assess the impact of reminders on patients’ viewing patterns.
Potential Confounders
We identified several potential confounders of viewing notes, including age, sex, site, note availability (a function of when the PCP signed note), and the presence of chronic health conditions in our primary analysis. We characterized chronic health conditions using a modified list of diagnoses originally described by Charlson et al., based on the International Classification of Diseases, Clinical Modification, Ninth Revision (ICD-9-CM). Our final list included 11 conditions: cardiovascular disease, cerebrovascular disease, chronic lung disease, rheumatologic disease, diabetes mellitus, liver/kidney disease, cancer, Human Immunodeficiency Virus (HIV), hypertension, hyperlipidemia, and back pain.11,12 Because GHS patients were predominately white,8 we assessed for disparities by evaluating the influence of race/ethnicity on viewing notes only in the BIDMC sample, and we also evaluated whether note viewing persisted over time stratified by race/ethnicity.
Statistical Analysis
We conducted a repeated measures analysis, with the patient visit as the unit of analysis. For our bivariable analysis, we used generalized linear models in order to compare categorical variables while also accounting for patient clustering. Additionally, we assessed the exchangeable correlation coefficient, which measures the degree of patient clustering, or more precisely, the correlation of note viewing probabilities for the same patient. Because the frequency of our outcome was relatively high (57.5% of notes were viewed within 30 days of availability), we present relative risk ratios (RR) instead of odds ratios in order to prevent any exaggeration of effect size.
Next, we used multivariable generalized linear models, focusing on number of previous visits and time in 3-month intervals as the primary exposures of interest. We also adjusted for the potential confounders outlined above, and in addition, our models adjusted for doctors as a fixed effect. Because invitations ceased at GHS but continued at BIDMC at the end of year 1, comparing predictors among these now differing sites in year 2 became problematic. Therefore, we stratified our multivariable analysis by site when evaluating year 2 of the study.
RESULTS
Baseline Characteristics
We identified 7853 patients from BIDMC and 6507 patients from GHS, for a total of 14 360 patients who made a total of 49 271 visits during the 2-year study period. Table 1 summarizes baseline demographic characteristics stratified by site.
Table 1:
Baseline patient characteristics (%)
| Factor sample no. of patients | BIDMC, n = 6813 | GHS, n = 5858 |
|---|---|---|
| Age, mean (SD) | 51.3 (13.3) | 53.2 (14.7) |
| Percent female | 60.1 | 55.1 |
| Number of visits | ||
| June 2010 to September 2010 | 4238 (32.3) | 3562 (24.4) |
| September 2010 to December 2010 | 3357 (25.6) | 3880 (26.5) |
| December 2010 to March 2011 | 3039 (23.1) | 3568 (24.4) |
| March 2011 to June 2011 | 2491 (19.0) | 3578 (24.5) |
| Comorbidities per patient | ||
| Cardiovascular disease | 153 (2.5) | 156 (2.8) |
| Cerebrovascular disease | 78 (1.3) | 56 (1.0) |
| Chronic lung disease | 402 (6.5) | 331 (6.0) |
| Rheumatologic disease | 68 (1.1) | 49 (0.9) |
| Diabetes mellitus | 593 (9.5) | 772 (14.0) |
| Liver/kidney disease | 143 (2.3) | 120 (2.2) |
| Cancer | 451 (7.3) | 213 (3.9) |
| HIV | 64 (1.0) | 2 (0.04) |
| Hypertension | 1834 (29.5) | 937 (17.0) |
| Hyperlipidemia | 1926 (31.0) | 593 (10.7) |
| Back pain | 757 (12.2) | 554 (10.0) |
| Race/ethnicitya | ||
| White | 4990 (75.1) | – |
| Black | 299 (5.2) | – |
| Other/multiracial | 1287 (19.7) | – |
aRace/ethnicity was recorded by clinic registration staff and was missing 2.1% of the time. Because GHS patients were almost exclusively white, we focused our race/ethnicity analysis on BIDMC patients.
Abbreviations: BIDMC, Beth Israel Deaconess Medical Center; GHS, Geisinger Health System; SD, standard deviation.
The mean age was 52.2 years, and 57.8% of patients were female. Chronic disease was common in the sample, with 23.6% of patients having hypertension, 21.5% with hyperlipidemia, and 11.6% with diabetes mellitus.
Note Viewing Over Time
During year 1, 57.5% of signed notes were viewed within 30 days of their availability (53.7% at BIDMC and 60.9% at GHS). Patients with multiple visits (58.5% of sample) generally tended to read their subsequent notes, with a correlation coefficient of 37.4%. During the first year of the trial, the probability of note viewing did not decline over time; however, patients with three or more visits were slightly less likely to view any of their notes when compared to patients with 1 visit RR 0.93 [95% CI, 0.91–0.96]. Figure 1 identifies unadjusted proportions of notes viewed over 2 years, and Figure 2 presents the multivariable adjusted probability over 2 years of note viewing over time, stratified by site. Comparing the second year to the first year, BIDMC patients continued to view their notes persistently, except for a slight decline in the probability of viewing notes in the final quarter of year 2, RR 0.94 [95% CI, 0.89-1.00]. In contrast, after year 1, GHS patients viewed notes far less frequently, starting with the time invitations ceased (RR 0.29 [95% CI, 0.26–0.32]) and persisting until the end of the study period (RR 0.20 [95% CI, 0.17–0.23]).
Figure 1:
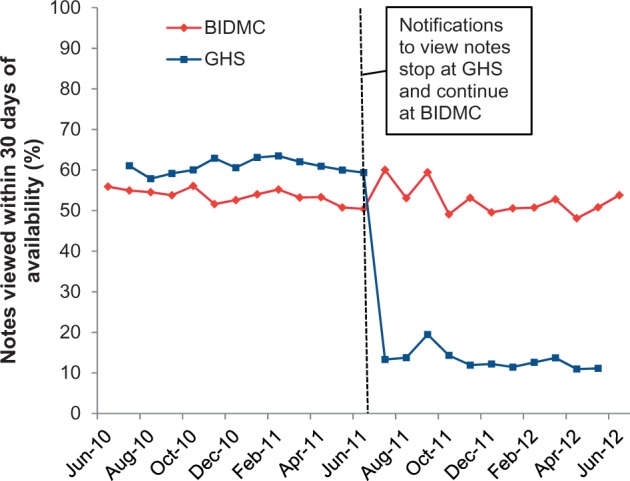
Unadjusted (Invitations ceased without clarification that access to notes would continue.) Note viewing over 2 years at both sites (BIDMC, Beth Israel Deaconess Medical Center; GHS, Geisinger Health System)
Figure 2:
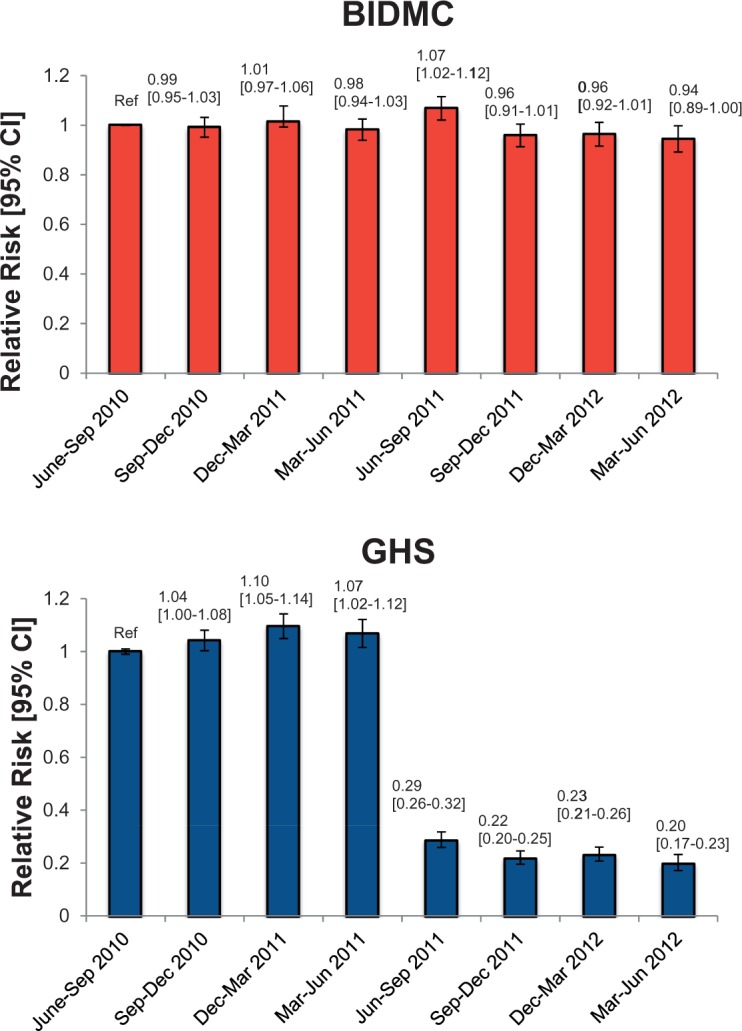
Multivariable adjusted (models adjust for age, sex, PCP, number of previous visits, delay in note signing, 11 comorbid conditions, time, and accounted for clustering among patients) probability of note viewing over 2 years (BIDMC, Beth Israel Deaconess Medical Center; GHS, Geisinger Health System; Ref, reference; CI, confidence interval)
Race/ethnicity Sub-analysis
Figure 3 presents unadjusted frequencies of viewing notes at BIDMC, stratified by race/ethnicity. Compared to white patients, black patients viewed notes less frequently (55.1% vs 36.3%, respectively, P < .001) and other/multiracial patients viewed notes less frequently (55.1% vs 50.2%, respectively, P < .001). After multivariable adjustment, results remained similar: black and other/multiracial patients were less likely to view notes compared with white patients (RR 0.75 [95% CI, 0.67–0.83] and RR 0.93 [95% CI, 0.89–0.98], respectively). Nonetheless, race/ethnicity did not affect the persistence of notes viewed over time: black and other/multiracial subgroups continued to view notes with similar frequencies over time during the 2-year period (P = .82 and P = .89 for interaction, respectively).
Figure 3:
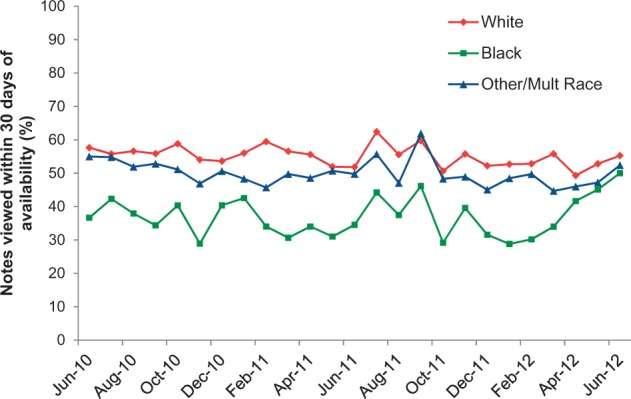
Unadjusted frequencies of note viewing at BIDMC over 2 years stratified by race/ethnicity (BIDMC, Beth Israel Deaconess Medical Center).
DISCUSSION
In two systems of primary care we examined whether patients would persist in viewing them beyond a first visit, and whether they would continue to do so, given the fairly radical change in practice of inviting patients to read their visit notes. The analysis revealed three major findings. First, in the presence of invitations and reminders to view notes, interest is high and remains durable. Second, email invitations and reminders are powerful motivators for patients to view their notes; without such reminders, patients are far less likely to do so. Third, in a BIDMC subanalysis using administrative race data, patients of black or other/multiracial race/ethnicity were less likely to view notes compared with white patients.
In our analysis, the majority of patients viewed their visit notes, and note viewing generally persisted so long as ongoing invitations continued. Of note, the discrepancy between this study’s finding that 57% of notes were viewed, vs 82% of patients viewing at least one note in prior reports of the OpenNotes study,9 is explained by our current study’s more restrictive definition of note viewing. In our prior work, we defined note viewing as any patient who accessed a note at least once (including a non-visit based note). In this study, we defined note viewing per visit and more restrictively, counting only a visit note accessed within 30 days of the note being signed and available to read.
While patients continued to view notes at BIDMC, we found a substantial drop at GHS where, unaccompanied by notifications that access to notes would continue, invitations ceased abruptly at the end of year 1. Some patients may have assumed that subsequent notes would once again be hidden. However, it is unlikely that patients would recall that the trial would last for 12 months, as they were told this only once at the beginning of the trial. Given an extensive literature indicating that invitations are important for changing patient behavior,12–14 the discontinuation of invitations likely played a substantial role in the decline in note viewing at GHS.
To our knowledge, only six US institutions are currently reminding patients by email to read their doctors’ notes: BIDMC, Stanford Healthcare, Kaiser Permanente Northwest, Mosaic Life Care, The Vancouver Clinic, and GHS, with the latter group resuming the practice partly due to the findings of this analysis. In each system, patients receive an automated electronic notification that the note is ready to be viewed once signed by a clinician (now including many medical and surgical specialists, trainees, and clinicians who are not doctors). Patients have responded favorably to receiving these invitations. For example, when Kaiser Permanente Northwest surveyed their portal users about OpenNotes, 93% of patients reported that they desired electronic alerts notifying them that their visit notes were available to review.16
Emerging data suggest that portal-based alerts may reduce office no-show rates and diminish care gaps in preventive and chronic disease management, and that they do not lead to patient alert fatigue.17,18 A recent study of OpenNotes participants at GHS revealed that invitations to view notes improved adherence to anti-hypertensive medications.19 Such data support invitations to view notes, though meta-analyses on whether portals in general (most of which do not offer access to clinical notes) lead to improved health outcomes remain inconclusive.20,21 Moreover, invitations to read notes could help healthcare organizations fulfill Meaningful Use requirements for portal participation and engagement.22
In our sub-analysis, black and other/multiracial race/ethnicity patients were less likely to view notes compared with white patients. These results are consistent with prior studies demonstrating racial, ethnic, and socioeconomic disparities in online portal use in general.23–26 For many vulnerable groups, increasing the rates of portal participation and engagement may require targeted strategies such as face-to-face education sessions in waiting rooms, mobile phone/text message-based outreach, and using language that is culturally appropriate, in the preferred language, and at the appropriate reading level.15,21,27,28 As access to transparent records spreads to involve underserved populations subject to widening health disparities, it becomes especially important to assess the impact of inviting such patients to read their clinicians’ notes and to develop alternative strategies to engage racial and ethnic minorities.
Our study has limitations. It was non-randomized, and therefore we cannot exclude the possibility of residual confounding. Furthermore, study patients at GHS and BIDMC were already registered on the portals, and some have had access to the portals for >10 years. Study participants therefore may not be representative of all patients seeking care at these institutions, or of the nation as a whole. However, there was no further patient self-selection beyond prior registration on portals. Doctors (as opposed to patients) made the decision whether their patients were able to participate in the OpenNotes intervention, and these doctors were demographically comparable to other doctors in the practices.8
CONCLUSION
Many patients choose to read their primary care doctors’ notes when offered ready access, and they persist in doing so as long as they continue to receive email invitations to view their notes. In this burgeoning area of inquiry, future studies should compare multiple reminder types to determine the best method for engaging patients in their own care. In addition, future efforts should develop targeted strategies to engage non-whites, as black and other/multiracial BIDMC patients viewed notes less frequently than white patients, though their interest in viewing notes also persisted. As this relatively novel practice takes root and millions of patients nationwide gain ready access to their clinicians’ notes, explicit invitations and reminders to review notes may prove highly important in helping patients engage and communicate more effectively with those offering care.
Acknowledgments
We thank George Silva, B.A. (BIDMC), Chris Dries, B.A. (GHS), Melissa Anselmo, M.P.H. (BIDMC), and the OpenNotes team for their data collection, organization, and administrative support.
CONTRIBUTORS
J.M., H.F., C.W., T.D., and J.W. were involved with study conception. J.M., C.W., R.M., and L.N. were involved in study analysis, and all authors were involved with writing, editing, and final approval of the manuscript. All authors contributed to study design and data collection.
FUNDING
This work was supported by the National Research Service Award (NRSA) training grant (T32HP12706) from the US Health Services and Research Administration and the Ryoichi Sasakawa Fellowship Fund (J.M.); a midcareer mentorship award from the National Institutes of Health (K24DK087932) (C.W.); the Robert Wood Johnson Foundation’s grant 65921 (J.D., T.D., H.F., L.N., J.W., and R.M.); and the Drane Family Fund and the Richard and Florence Koplow Charitable Foundation (T.D. and J.W.).
COMPETING INTERESTS
The authors declare no competing interests.
REFERENCES
- 1.Hibbard JH, Mahoney ER, Stock R, et al. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42:1443–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stacey D, Légaré F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;(10):CD001431. [DOI] [PubMed] [Google Scholar]
- 3.Mafi J, Rotherberg M, Sepucha K, Barry M. Time for Quality Measurement to get Personal. Jt Comm J Qual Saf. 2016; In Press. [DOI] [PubMed] [Google Scholar]
- 4.Kessels RP. Patients' memory for medical information. JRSM. 2003;96:219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson JL, Dodman S, Kopelman M, et al. Patient information recall in a rheumatology clinic. Rheumatol Rehabil. 1979;18:18–22. [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal D. Implementation of the federal health information technology initiative. N Engl J Med. 2011;365:2426–2431. [DOI] [PubMed] [Google Scholar]
- 7.Pavlik V, Brown AE, Nash S, et al. Association of patient recall, satisfaction, and adherence to content of an electronic health record (EHR)-generated after visit summary: a randomized clinical trial. J Am Board Fam Med. 2014;27:209–218. [DOI] [PubMed] [Google Scholar]
- 8.Walker J, Leveille SG, Ngo L, et al. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155:811–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead. Ann Intern Med. 2012;157:461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker J, Meltsner M, Delbanco T. US experience with doctors and patients sharing clinical notes. BMJ (Clinical research ed). 2015;350:g7785. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 12.Deyo R. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. JCE. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 13.Lau AYS, Sintchenko V, Crimmins J, et al. Impact of a web-based personally controlled health management system on influenza vaccination and health services utilization rates: a randomized controlled trial. J Am Med Inform Assoc. 2012;19:719–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright A, Poon EG, Wald J, et al. Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. J Gen Intern Med. 2012;27(1):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Druss BG, Ji X, Glick G, et al. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014;171:360–368. [DOI] [PubMed] [Google Scholar]
- 16.Unitan R, Johnson LW, McLeod M, et al. Sharing Visit Notes Online – Patient Experience with Kaiser Permanente Northwest's Big-Bang Implementation of OpenNotes (June 2015). Abstract presented at the 2015 AcademyHealth Annual Research Meeting; Minneapolis, MN. [Google Scholar]
- 17.Hess R, Fischer GS, Sullivan SM, et al. Patterns of response to patient-centered decision support through a personal health record. Telemed J E. 2014;20:984–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horvath M, Levy J, L'Engle P, et al. Impact of health portal enrollment with email reminders on adherence to clinic appointments: a pilot study. J Med Internet Res. 2011;13:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wright E, Darer J, Tang X, Thompson J, Tusing L, Fossa A, et al. Sharing Physician Notes Through an Electronic Portal is Associated With Improved Medication Adherence: Quasi-Experimental Study. J Med Internet Res. 2015;17(10):e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to Meaningful Use: a systematic review. J Med Internet Res. 2015;17:e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159:677–687. [DOI] [PubMed] [Google Scholar]
- 22.Neuner J, Fedders M, Caravella M, et al. Meaningful use and the patient portal: patient enrollment, use, and satisfaction with patient portals at a later-adopting center. Am J Med Qual. 2015;30:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goel M, Brown T, Williams A, et al. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26(10):1112–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171(6):568–574. [DOI] [PubMed] [Google Scholar]
- 25.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mishuris RG, Stewart M, Fix GM, et al. Barriers to patient portal access among veterans receiving home-based primary care: a qualitative study. Health Expect. 2014; doi: 10.1111/hex.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015;17:e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sequist TD. Health information technology and disparities in quality of care. J Gen Intern Med. 2011;26(10):1084–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]


