Abstract
Observational studies of thyroid function and dementia have reported conflicting results. We reviewed cohort and case-control studies from MEDLINE, EMBASE, Web of Science and the Cochrane Library that focused on the association between serum thyroxine, thyrotropin and dementia. A total of 24,952 participants from three case-control and eight cohort studies were included. The relationships between dementia and the per standard deviation (SD) increment of free thyroxine (FT4) (random relative ratio (RR) = 1.08, 95% confidence interval (CI) 1.00–1.17) and thyroid-stimulating hormone (TSH) (fixed RR = 0.91, 95% CI 0.84–0.99) were well established. TSH levels in the low category were associated with an increased risk of dementia (fixed RR = 1.60, 95% CI 1.27–2.00). However, the positive association was confined to TSH levels below the normal range (fixed RR = 1.77, 95% CI 1.31–2.39), not those in the lower tertile of the normal range (fixed RR = 1.39, 95% CI 0.98–1.97). Additionally, dementia was not significantly associated with high TSH levels (fixed RR = 0.99, 95% CI 0.76–1.29). Furthermore, there was no positive association between dementia and the low or high categories of TSH in men. Thus, individuals with higher FT4 levels or those with TSH levels below the normal range have an increased risk of dementia.
Dementia is a clinical syndrome characterized by a cluster of symptoms and signs that results in complex cognitive decline; it has emerged as one of the greatest health threats during old age and has substantial socioeconomic costs. Alzheimer’s disease (AD), which is the most common type of dementia, constitutes 50–70% of cases1 and is one of the top 8 major health problems in the world2. Despite recent advances in research, major scientific gaps remain in the understanding of the intrinsic mechanism of dementia. In the absence of medications that effectively cure or slow the progression of these diseases, especially AD3,4, considerable challenges associated with early intervention remain. The development of preventive measures for dementia requires a greater understanding of the risk factors for this disease. Accordingly, we may prevent the elderly from further cognitive decline.
Thyroid hormone (TH) regulates metabolic processes that are essential for normal growth and development as well as neurocognitive function after development5. Thyroid-stimulating hormone (TSH) targets the thyroid gland and triggers the release of thyroxine (T4) and triiodothyronine (T3) when stimulated by the hypothalamic secretion of thyrotropin-releasing hormone (TRH)6. The relationship between thyroid-related hormones and dementia is controversial, especially regarding TSH (whether outside or within the normal range)7,8,9,10. According to laboratory tests, thyroid dysfunction can be classified as overt, with both abnormal TSH and free T4 (FT4) levels, or as subclinical, with abnormal TSH but normal FT4 levels. Some studies have demonstrated a relationship between overt thyroid disease and cognitive disturbances11,12. However, the influence of subclinical thyroid disease on cognition remains unclear. Since Wahlin et al.13 first reported an association between poor cognition and low serum TSH levels within the normal range, more researchers have become interested in the impact of thyroid hormone levels (within the normal range) on cognition7,14. Moreover, the role of FT4 levels in the development or progression of dementia remains controversial. Certain large prospective studies have observed that higher FT4 levels are related to dementia15,16, whereas other studies have not reported this association10,17. Therefore, it is necessary to conduct a systematic review and meta-analysis to summarize the published findings and to obtain a better understanding of the association between FT4, TSH and dementia.
Results
Eligible studies and characteristics
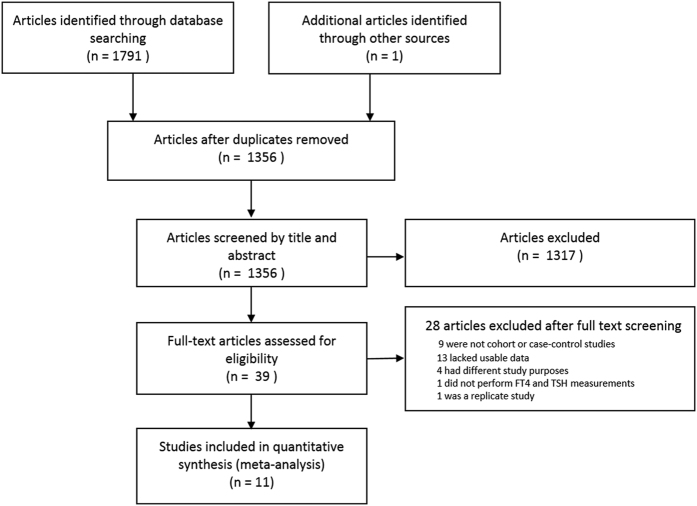
The search strategy identified 1791 citations for evaluation. A manual review of the study references yielded one additional study. After carefully scanning the titles and abstracts, 39 articles that were potentially eligible for inclusion were retrieved. After reading the full texts, 28 articles were excluded for the following reasons: nine studies were not cohort or case-control studies18,19,20,21,22,23,24,25,26; 13 lacked usable data13,14,17,27,28,29,30,31,32,33,34,35,36; four had different study purposes37,38,39,40; one did not perform FT4 and TSH measurements41; and one was a replicate study with a shorter follow-up42 than that by de Jong et al.10 (Fig. 1). Eleven studies published from 2003 to 2016 that evaluated a total of 24,952 participants, including 1526 patients with dementia, were finally included. The detailed information is provided in Table 1. Among the included studies, three43,44,45 were case-control studies, and eight7,8,9,10,15,16,46,47 were cohort studies. Specifically, the work by Tan et al.9 was analyzed by gender and was treated as two individual studies. Additionally, two studies15,16 included only men. Most studies controlled for some conventional risk factors, including age (n = 11), gender (n = 11) and thyroid medication (n = 7). Most of the included studies were of high quality and scored from 7 to 9 on the Newcastle Ottawa Scale (NOS). Only one was of moderate quality, with a score of 6 (Supplementary Table 1). The average score was 7.3, and the follow-up duration ranged from 4 to 17 years.
Figure 1. Flow diagram of study retrieval and selection.
Table 1. Characteristics of included case-control and cohort studies.
| First author | Country (race) | Study size (females, %) | Mean age (range) | Follow up (years) | Covariates | Results | NOS score |
|---|---|---|---|---|---|---|---|
| Case-control studies | |||||||
| Dobert 200343 | Germany (Caucasian) | 77 dementia (46.8%); 42 controls (47.6%) | AD, 69.8 Control, 63.9 | — | Age, sex, thyroid mediation | Positive association between lower TSH and dementia. | 7 |
| van Osch 200444 | UK (Caucasian) | 178 AD (43.0%); 291 controls (48.0%) | 73.7 | — | Age, sex, education, APOEε4, Hcy, depression, Cr, thyroid mediation | Positive association between lower TSH and AD. | 7 |
| Hu 201645 | China (Asian) | 154 AD (46.8%); 77 controls (44.2%) | AD, 63.5 Controls, 64.1 | — | Age, sex, education, BMI | Negative association between AD and hypothyroidism and SH. | 6 |
| Cohort studies | |||||||
| de Jong 200610 | Netherlands (Caucasian) | 1,025 communities (51.2%) | 72.3 (60–90) | 5.5 | Age, sex, education, smoking, Hcy depression, smoking, Cr, APOEε4, DM, AF, BMI, medication use, cholesterol, | Negative association between TSH/FT4 and dementia. | 9 |
| Tan 20089 | USA (Caucasian) | 1864 communities (59.0%) | 71 | 12.7 | Age, stroke, education, Hcy, BMI, AF | Positive association between low/high TSH and AD in women. | 7 |
| de Jong16 | Hawaii (Japanese -American) | 665 communities (0%) | 77.3–78.6 (71–93) | 4.7 | Age, education, depression, albumin, BMI, TC, HDL-C, DM, smoking, thyroid mediation, SBP, DBP | Positive association between higher FT4 and dementia. | 7 |
| Annerbo 200946 | Sweden (Caucasian) | 200 communities (79.5%) | 81.0 (75–93) | 6.7 | Age, sex, education | Negative association between TSH and dementia. | 7 |
| Forti 20118 | Italy (Asian) | 660 communities (52.9%) | 73.3 (65–91) | 4 | Age, gender, education, BMI, hypertension, cholesterol, Hcy, DM, CVD, GDS | Negative association between TSH and AD. | 7 |
| Vadiveloo 201147 | UK (Caucasian) | 12,115 communities (NR) | 66.5 | 5.6 | Age, gender, history of dementia and psychiatric disorders, thyroid medication | Positive association between SH and dementia. | 7 |
| Yeap 201215 | Australia (Caucasian) | 3401 communities (0%) | (70–89) | 5.9 (median) | Age, BMI, smoking, education, DM, CVD, hypertension, MMSE, social support, sensorial impairment, thyroid medication | Positive association between higher FT4 and dementia in men. | 9 |
| Cappola 20157 | USA (African18.6%, Caucasian 81.4%) | 2843 communities (56.2%) | 74.5 | 17 | Age, sex, race, thyroid medication, hypertension, DM, current smoking, alcohol, BMI, TC, stroke, APOEε4, claudication | Positive association between higher TSH and lower incidence of dementia. | 7 |
Key: NOS: Newcastle Ottawa Scale AD, Alzheimer’s disease; Hcy, homocysteine; BMI, body mass index; SH: subclinical hyperthyroidism; Cr, creatinine; DM, diabetes; AF, atrial fibrillation; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; CVD, cardiovascular disease; GDS, Geriatric Depression Scale score; NR, not reported; MMSE, minimum mental state examination.
Meta-analysis
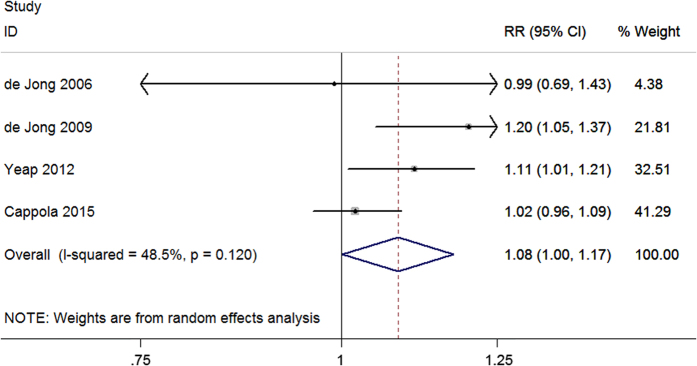
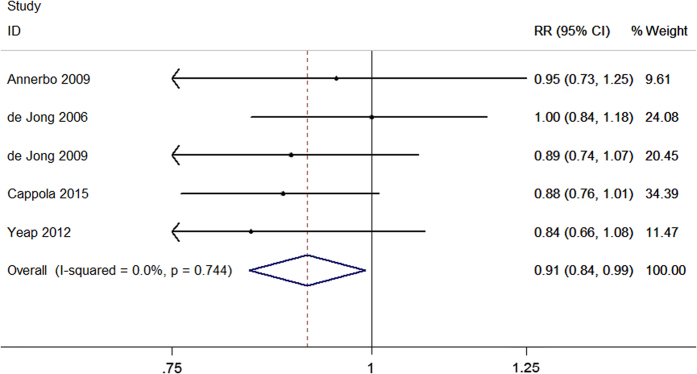
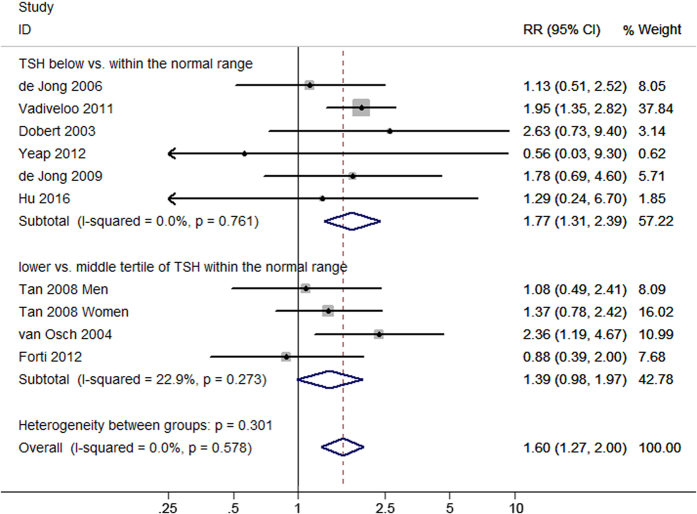
Four studies evaluated the association between serum FT4 concentration and dementia. The pooled results revealed that the per standard deviation (SD) increment of FT4 was associated with an increased risk of dementia (relative ratio (RR) = 1.08, 95% confidence interval (CI) 1.00–1.17) with a heterogeneity (I2) of 48.5% (P = 0.120) using the random effect model (Fig. 2). Five studies considered TSH level as a continuous variable to analyze its association with dementia. Meta-analysis using a fixed effect model showed a significant association between the per SD increment of TSH and dementia (fixed RR = 0.91, 95% CI 0.84–0.99; I2 = 0%, P = 0.744) (Fig. 3). Moreover, ten studies evaluated the risk estimates of different TSH categories and dementia. When comparing the low and middle categories of TSH levels, the fixed model showed that low TSH levels were significantly associated with an increased risk of dementia (fixed RR = 1.60, 95% CI 1.27–2.00; I2 = 0%, P = 0.578) (Fig. 4). Furthermore, the risk estimates for the high and middle categories of TSH levels indicated an inverse but insignificant association between high TSH levels and dementia (fixed RR = 0.99, 95% CI 0.76–1.29; I2 = 17.0%, P = 0.291) (Supplementary Figure 1).
Figure 2. Forest plot of FT4 per SD increment and dementia.
The estimated RRs and 95% CIs are plotted with boxes and horizontal lines.
Figure 3. Forest plot of TSH per SD increment and dementia.
The estimated RRs and 95% CIs are plotted with boxes and horizontal lines.
Figure 4. Forest plot of the low vs. middle categories of TSH levels and dementia.
Two subgroups were analyzed: TSH levels below vs. within the normal range and the lower vs. middle tertiles of TSH levels within the normal range. The estimated RRs and 95% CIs are plotted with boxes and horizontal lines.
Subgroup analyses
Subgroup analyses were performed on studies with a similar study design (cohort or case-control) and data on TSH levels and gender. Stratified analyses were not performed using the per SD increment of FT4 and TSH levels model because all the included studies were cohort studies. When low and middle categories of TSH levels were compared, the results of analyses stratified by study design were consistent with the overall trend. Additionally, case-control studies showed a positive association between high TSH levels and dementia (fixed RR = 0.54, 95% CI 0.30–1.00; I2 = 0%, P = 0.440), while cohort studies did not show this association. For data types regarding TSH levels, there were two low categories: the lower tertile of TSH levels within the normal range and TSH levels below the normal range. Likewise, there were two high categories: the upper tertile of TSH levels within the normal range and TSH levels above the normal range. Subgroup analyses revealed that only TSH levels below the normal range (fixed RR = 1.77, 95% CI 1.31–2.39; I2 = 0%, P = 0.761, not those in the lower tertile of the normal range (fixed RR = 1.39, 95% CI 0.98–1.97; I2 = 22.9%, P = 0.273) or those in the two high categories, were associated with dementia. Three studies evaluated the relationship between TSH and dementia in men; meta-analyses of the low and high categories of TSH levels showed no association with dementia in men (Supplementary Figure 2). The detailed results are provided in Table 2.
Table 2. Stratified analysis of the association between TSH and dementia.
| Subgroup | N | Risk estimate |
Heterogeneity |
||
|---|---|---|---|---|---|
| Pooled RR (95% CI) | P1 | I2 | P2 | ||
| TSH: low category vs. middle category | 10 | 1.6 (1.27, 2.00) | <0.001 | 0.00 | 0.58 |
| Study type | |||||
| Cohort | 7 | 1.5 (1.17, 1.92) | 0.001 | 0.00 | 0.49 |
| Case-control | 3 | 2.25 (1.28, 3.96) | 0.005 | 0.00 | 0.78 |
| Data type | |||||
| TSH below vs. within the normal range | 6 | 1.77 (1.31, 2.39) | <0.001 | 0.00 | 0.76 |
| Lower vs. middle tertile of TSH within the normal range | 4 | 1.39 (0.98, 1.97) | 0.062 | 0.23 | 0.27 |
| TSH: high category vs. middle category | 9 | 0.99 (0.76, 1.29) | 0.923 | 0.17 | 0.29 |
| Study type | |||||
| Cohort | 6 | 1.14 (0.85, 1.54) | 0.385 | 0.00 | 0.65 |
| Case-control | 3 | 0.54 (0.30, 1.00) | 0.048 | 0.00 | 0.44 |
| Data type | |||||
| TSH above vs. within the normal range | 6 | 0.91 (0.61, 1.34) | 0.619 | 0.00 | 0.77 |
| Upper vs. middle tertile of TSH within the normal range | 3 | 1.07 (0.74, 1.54) | 0.734 | 0.70 | 0.03 |
| Gender: male | |||||
| Low category vs. middle category of TSH | 3 | 1.28 (0.70, 2.32) | 0.419 | 0.00 | 0.62 |
| High category vs. middle category of TSH | 3 | 0.92 (0.60, 1.43) | 0.722 | 0.00 | 0.57 |
Key: N, number of studies. P1 is an evaluation of the statistical significance level of the risk estimate, while P2 is an evaluation of the heterogeneity among included studies. Subgroup analyses were performed by study design (cohort or case-control) and data types of TSH levels. Three studies evaluating the relationship between TSH and dementia in men were analyzed separately.
Sensitivity analysis and publication bias
All of the models demonstrated stability in the sensitivity analysis when each study was individually omitted (Supplementary Figure 3). Visual inspection of the funnel plots for each model did not show asymmetry, except for the model of the per SD increment of FT4 (Supplementary Figure 4); however, Egger’s test found no statistical evidence of publication bias for all models (per SD increment of FT4, P = 0.621; per SD increment of TSH, P = 0.972; low vs. middle categories of TSH levels, P = 0.252; high vs. middle categories of TSH levels, P = 0.480). Funnel plot and Egger’s test were not evaluated for subgroup analyses in men, because the numbers of included studies were small.
Discussion
To the best of our knowledge, this study is the first meta-analysis assessing the relationship between FT4 and dementia. In the model of per SD increment of FT4 and dementia, we found an association between higher FT4 levels and an increased risk of dementia in community-dwelling elderly from four prospective studies with high quality. Additionally, FT4 was reported to be related to brain atrophy of the hippocampus and amygdala10, which is strongly associated with the risk of dementia48.
Furthermore, the relationship between the per SD increment of TSH and dementia was well established, showing that lower TSH levels are related to an increased risk of dementia. This finding was supported by the risk estimate of the low category of TSH levels and dementia. Notably, we performed a further subgroup analysis based on the type of data on TSH levels. Interestingly, we found that the positive association between low TSH levels and a high risk of dementia was confined to TSH levels below the normal range, rather than those within the normal range. Due to the limited number of studies on various tertiles of TSH within the normal range, more large studies are urgently needed to obtain a comprehensive and precise conclusion.
In addition, dementia was not significantly associated with TSH levels in the high categories (above the normal range or in the upper tertile within the normal range). Stratified analysis by case-control study showed high TSH levels had a protective tendency for dementia, while the analysis by cohort study showed no association between high TSH levels and dementia, indicating that this association still needs to be investigated. Our observation was also consistent with the two placebo-controlled, double-blind randomized clinical trials of T4 medication administered for 1 year49,50. The two studies both failed to show the effect of T4 replacement therapy on improving cognitive function.
Furthermore, a differential risk by gender in the TSH analyses existed in several studies9,36,51. These studies collectively indicated that women were more susceptible to the effects of TSH on cognition. In our study, the result of the subgroup analysis of gender in three studies showed no relationship between TSH and dementia in men in the high or low categories of TSH levels; however, considering the limited number of studies, caution should be taken when concluding a negative association; additional well-designed studies stratified by gender should be conducted.
Remarkably, some scholars have suggested that low TSH and high FT4 levels may be biomarkers of age, and both parameters are associated with other diseases that occur in patients of advanced age, including dementia. In addition, low TSH levels might be a consequence of AD-related neurodegeneration, which could reduce the secretion of TRH by the hypothalamus or decrease the responsiveness of the pituitary gland to TRH52. Moreover, other studies have demonstrated a relationship between thyroid hormone and amyloid, which has an essential role in AD development. These findings raise the question of whether low TSH and high FT4 levels are contributors to, rather than biomarkers or even consequences of, poor cognitive outcomes in older adults. However, our study explored positive associations between higher FT4 levels and TSH levels below the normal range and dementia, and a lack of association between high TSH levels and dementia was noted.
Our meta-analysis had some limitations. First, although bias may exist due to the observational nature of the included studies and different data collection methods (prospective or retrospective), the relatively large combined sample size and good quality of the included studies potentially strengthen the power of the analysis. Second, the methods used to detect thyroid function and covariates differed among the studies. No specific reference range of hormone levels was provided. Moreover, three RRs in the TSH model were calculated manually based on the available data in the respective studies, whereas other data were extracted from the most adjusted regression models. A more precise analysis should be conducted when individual data are available. Third, a subgroup analysis by age was not performed because of insufficient data. The incidence of AD differs with age, and the prevalence doubles every five years after the age of 6053. Fourth, the prevalence of high TSH concentrations is higher in individuals of Caucasian descent than in those of African descent; this difference indicates a genetic influence on TSH secretion54. Most individuals included in our study were Caucasians. Thus, a subgroup analysis by race was not conducted.
In conclusion, this report is the first meta-analysis illustrating the contribution of TSH and FT4 to dementia. Based on 24,952 participants including 1526 patients with dementia, an increased risk of dementia in individuals with higher serum FT4 levels and in those with TSH levels below the normal range was found. The present study implied T4 replacement therapy may be administered cautiously, as no specific relationship was shown between high TSH levels and dementia. Moreover, individuals receiving T4 replacement therapy may develop a low or even a suppressed TSH level55, which could consequently lead to an increased risk of dementia. However, additional large, prospective, cohort studies and randomized controlled trials are still needed to determine the causal association between thyroid hormones and dementia.
Methods
This meta-analysis was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 Checklist (http://www.prismastatement.org/statement.htm) and the Meta-analysis of Observational Studies in Epidemiology group (MOOSE)56.
Search strategy and study selection
We searched Medline, Embase, Web of Science and the Cochrane Library for all published studies up to June 7, 2016, that evaluated the relationship between thyroid function and cognitive decline without any restrictions. The key search terms were “thyroxine (T4)”, “thyrotropin (TSH)”, “triiodothyronine (T3)”, “hyperthyroidism”, “hypothyroidism”, “euthyroidism”, “subclinical hyperthyroidism”, “subclinical hypothyroidism”, “thyroid dysfunction or disorders”, “dementia”, “Alzheimer’s disease (AD)”, “cognitive decline or impairment or defect”, “mild cognitive impairment (MCI)” and “cohort or case-control or longitudinal or follow-up”. Supplementary Figure 5 contains the MEDLINE search terms. We also manually searched the bibliographies of all qualified studies for other potential articles. Wu Y and Pei Y independently evaluated the retrieved studies by thoroughly reading the titles and abstracts with pre-designed inclusion criteria. Full texts were further checked if necessary. If the required data were not reported in a potential article, we contacted the corresponding author for more details. Any disagreement between the two investigators was resolved by consensus or by discussion with a third reviewer, Wang F.
Studies were initially included in the detailed assessment if they met the following criteria: 1) sufficient information on the study population; 2) cohort or case-control studies; 3) clear criteria for the outcome (dementia or AD) diagnosed according to internationally accepted criteria for dementia (DSM-III-R57 or DSM-IV58) and AD (NINCDS-ADRDA59), by a multi-disciplinary team (neurologists, psychiatrists, and psychologists) or by record linkage; 4) sufficient data on risk estimates of the association between FT4 or TSH levels and dementia or AD: RR, hazard ratio (HR), or odds ratio (OR) with 95% CIs or the number of outcome events; 5) adjustments for potential confounders; and 6) valid measurements of FT4 and TSH. We excluded studies that were cross-sectional, lacked usable data, or focused on vascular dementia or dementia secondary to other diseases. If multiple reports used the same population, the study with the longest follow-up was included. Reviews, case reports, abstracts and conference proceedings were excluded.
Data extraction and quality assessment
Two investigators (Wu Y and Pei Y) independently extracted the data from the eligible studies with a common form. The outcome was dementia or AD. The following data were extracted: first author, publication year, study type, country or race, study size, age of participants, gender distribution, duration of follow-up, covariates, and results (Table 1). Generally, the levels of TSH can be divided into three categories: TSH below the normal range, TSH within the normal range, and TSH above the normal range. While in the normal range, TSH levels can be further divided into three tertiles: lower, middle and upper. Thus, the overall TSH levels were classified into three categories in our meta-analysis models: TSH below the normal range or the lower tertile within the normal range, denoted as low; TSH within the normal range or the middle tertile within the normal range, denoted as middle; and TSH above the normal range or the upper tertile within the normal range, denoted as high. Because the data regarding thyroid function varied among the studies, we extracted the following information for the meta-analysis: 1) risk estimates per SD increment of FT4/TSH levels; 2) risk estimates for TSH levels below or above the normal range compared with TSH levels within the normal range; and 3) risk estimates for lower or upper tertiles compared with the middle tertile of TSH levels within the normal range. Of the studies that reported risk estimates with multiple-level adjustments, we included those that adjusted for the most covariates.
The Newcastle Ottawa Scale, a measure of the quality of observational studies, was used to assess the quality of the selected studies. This scale consists of three domains, including the selection of cases, comparability of populations, and ascertainment of exposure. Scores of 0–3, 4–6, and 7–9 indicate low, moderate, and high quality, respectively. Two investigators independently performed the quality assessment, and disagreements were resolved by discussion.
Data synthesis and statistical analyses
Dichotomous data were calculated as the OR and 95% CI. In the meta-analysis, the RRs were used for risk estimates. ORs and HRs were also treated as RRs. Heterogeneity between studies was assessed using the I2 statistic: I2 < 25%, low; between 25 and 50%, moderate; and >50%, high60. If moderate or high heterogeneity was found, a random effect model was used61; otherwise, the fixed effect model was applied62. Subgroup analyses based on study design, data type regarding TSH levels and gender were performed to explore the sources of heterogeneity. To assess the stability of the results, a one-way sensitivity analysis was performed by omitting each study in turn from the analysis. Publication bias was assessed by funnel plots and Egger’s linear regression test63. All analyses were conducted using STATA 12.0 (StataCorp, College Station, TX, USA), and a two-sided P < 0.05 was considered significant, except for Egger’s test, in which the P value was set at 0.10 to be more conservative.
Additional Information
How to cite this article: Wu, Y. et al. Higher FT4 or TSH below the normal range are associated with increased risk of dementia: a meta-analysis of 11 studies. Sci. Rep. 6, 31975; doi: 10.1038/srep31975 (2016).
Supplementary Material
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81071418 and No. 81472029) and the Peking Union Medical College Innovation Fund for Graduate Students (No. 2015-1002-01-02).
Footnotes
Author Contributions Y.W. contributed to the study design, data analysis and interpretation; drafted part of the manuscript; and prepared the tables and figures. Y.P. participated in collecting and analyzing the data and drafting part of the manuscript. F.W. revised the manuscript. D.X. searched the related papers and extracted data. W.C. designed this study and revised the manuscript. All the authors reviewed the manuscript.
References
- Burns A. & Iliffe S. Dementia. Bmj 338, b75 (2009). [DOI] [PubMed] [Google Scholar]
- Cornutiu G. The Epidemiological Scale of Alzheimer’s Disease. J. Clin. Med. Res. 7, 657–666 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell S. L. Clinical Practice. Advanced Dementia. N. Engl. J. Med. 372, 2533–2540 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas M. et al. The European Medicines Agency’s strategies to meet the challenges of Alzheimer disease. Nat. Rev. Drug Discov. 14, 221–222 (2015). [DOI] [PubMed] [Google Scholar]
- Cheng S. Y., Leonard J. L. & Davis P. J. Molecular aspects of thyroid hormone actions. Endocr. Rev. 31, 139–170 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie M. & Yeap B. B. Thyroid hormone: Influences on mood and cognition in adults. Maturitas 81, 266–275 (2015). [DOI] [PubMed] [Google Scholar]
- Cappola A. R. et al. Thyroid function in the euthyroid range and adverse outcomes in older adults. J. Clin. Endocrinol. Metab. 100, 1088–1096 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forti P. et al. Serum thyroid-stimulating hormone as a predictor of cognitive impairment in an elderly cohort. Gerontology 58, 41–49 (2012). [DOI] [PubMed] [Google Scholar]
- Tan Z. S. et al. Thyroid function and the risk of Alzheimer disease: the Framingham study. Arch. Intern. Med. 168, 1514–1520 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong F. J. et al. Thyroid hormones, dementia, and atrophy of the medial temporal lobe. J. Clin. Endocrinol. Metab. 91, 2569–2573 (2006). [DOI] [PubMed] [Google Scholar]
- Tan Z. S. & Vasan R. S. Thyroid function and Alzheimer’s disease. J. Alzheimers Dis. 16, 503–507 (2009). [DOI] [PubMed] [Google Scholar]
- Davis J. D. & Tremont G. Neuropsychiatric aspects of hypothyroidism and treatment reversibility. Minerva Endocrinol. 32, 49–65 (2007). [PubMed] [Google Scholar]
- Wahlin A., Bunce D. & Wahlin T. B. R. Longitudinal evidence of the impact of normal thyroid stimulating hormone variations on cognitive functioning in very old age. Psychoneuroendocrinology 30, 625–637 (2005). [DOI] [PubMed] [Google Scholar]
- Moon J. H. et al. Lower-but-normal serum TSH level is associated with the development or progression of cognitive impairment in elderly: Korean longitudinal study on health and aging (KLOSHA). J. Clin. Endocrinol. Metab. 99, 424–432 (2014). [DOI] [PubMed] [Google Scholar]
- Yeap B. B. et al. Higher free thyroxine levels predict increased incidence of dementia in older men: the Health in Men Study. J. Clin. Endocrinol. Metab. 97, E2230–E2237 (2012). [DOI] [PubMed] [Google Scholar]
- de Jong F. J. et al. Thyroid function, the risk of dementia and neuropathologic changes: the Honolulu-Asia Aging Study. Neurobiol. Aging 30, 600–606 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gussekloo J. et al. Thyroid status, disability and cognitive function, and survival in old age. JAMA 292, 2591–2599 (2004). [DOI] [PubMed] [Google Scholar]
- Park Y. J. et al. Subclinical hypothyroidism (SCH) is not associated with metabolic derangement, cognitive impairment, depression or poor quality of life (QoL) in elderly subjects. Arch. Gerontol. Geriatr. 50, e68–e73 (2010). [DOI] [PubMed] [Google Scholar]
- Ganguli M., Burmeister L. A., Seaberg E. C., Belle S. & DeKosky S. T. Association between dementia and elevated TSH: A community-based study. Biol. Psychiatry 40, 714–725 (1996). [DOI] [PubMed] [Google Scholar]
- Luboshitzky R., Oberman A. S., Kaufman N., Reichman N. & Flatau E. Prevalence of cognitive dysfunction and hypothyroidism in an elderly community population. Isr. J. Med. Sci. 32, 60–65 (1996). [PubMed] [Google Scholar]
- Prinz P. N. et al. Thyroid hormones: positive relationships with cognition in healthy, euthyroid older men. J. Gerontol. A Biol. Sci. Med. Sci. 54, M111–M116 (1999). [DOI] [PubMed] [Google Scholar]
- Resta F. et al. Subclinical hypothyroidism and cognitive dysfunction in the elderly. Endocr. Metab. Immune Disord. Drug Targets 12, 260–267 (2012). [DOI] [PubMed] [Google Scholar]
- Stern R. A. et al. Preliminary study of the relationship between thyroid status and cognitive and neuropsychiatric functioning in euthyroid patients with Alzheimer dementia. Cogn. Behav. Neurol. 17, 219–223 (2004). [PubMed] [Google Scholar]
- van Boxtel M. P., Menheere P. P., Bekers O., Hogervorst E. & Jolles J. Thyroid function, depressed mood, and cognitive performance in older individuals: the Maastricht Aging Study. Psychoneuroendocrinology 29, 891–898 (2004). [DOI] [PubMed] [Google Scholar]
- Kim J. M. et al. Thyroid stimulating hormone, cognitive impairment and depression in an older Korean population. Psychiatry Investig. 7, 264–269 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojala A. K., Schalin-Jäntti C., Pitkälä K. H., Tilvis R. S. & Strandberg T. E. Serum thyroid-stimulating hormone and cognition in older people. Age Ageing 45, 155–157 (2016). [DOI] [PubMed] [Google Scholar]
- Wijsman L. W. et al. Subclinical thyroid dysfunction and cognitive decline in old age. PLoS One 8, e59199 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Formiga F. et al. Thyroid status and functional and cognitive status at baseline and survival after 3 years of follow-up: the OCTABAIX study. Eur. J. Endocrinol. 170, 69–75 (2014). [DOI] [PubMed] [Google Scholar]
- Formiga F. et al. Predictors of cognitive decline in 85-year-old patients without cognitive impairment at baseline: 2-year follow-up of the Octabaix study. Am. J. Alzheimers Dis. Other Demen. 28, 147–153 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jongh R. T. et al. Endogenous subclinical thyroid disorders, physical and cognitive function, depression, and mortality in older individuals. Eur. J. Endocrinol. 165, 545–554 (2011). [DOI] [PubMed] [Google Scholar]
- Yong-Hong L., Xiao-Dong P., Chang-Quan H., Bo Y. & Qing-Xiu L. Hypothalamic-pituitary-thyroid axis in patients with Alzheimer disease (AD). J. Investig. Med. 61, 578–581 (2013). [DOI] [PubMed] [Google Scholar]
- Lillevang-Johansen M., Petersen I., Christensen K., Hegedus L. & Brix T. H. Is previous hyperthyroidism associated with long-term cognitive dysfunction? A twin study. Clin. Endocrinol. (Oxf) 80, 290–295 (2014). [DOI] [PubMed] [Google Scholar]
- Nuray Ulusu N. et al. A comparative study on thyroid function in Alzheimer’s disease: Results from a Turkish multi-centre study. J. Neurol. Sci. Turk. 32, 335–347 (2015). [Google Scholar]
- Castellano C. A. et al. Thyroid function and cognition in the euthyroid elderly: a case-control study embedded in Quebec longitudinal study - NuAge. Psychoneuroendocrinology 38, 1772–1776 (2013). [DOI] [PubMed] [Google Scholar]
- Zhang N., Du H. J., Wang J. H. & Cheng Y. A pilot study on the relationship between thyroid status and neuropsychiatric symptoms in patients with Alzheimer disease. Chin. Med. J. (Engl) 125, 3211–3216 (2012). [PubMed] [Google Scholar]
- Beydoun M. A. et al. Thyroid hormones are associated with longitudinal cognitive change in an urban adult population. Neurobiol. Aging 36, 3056–3066 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogervorst E., Huppert F., Matthews F. E. & Brayne C. Thyroid function and cognitive decline in the MRC Cognitive Function and Ageing Study. Psychoneuroendocrinology 33, 1013–1022 (2008). [DOI] [PubMed] [Google Scholar]
- Volpato S. et al. Serum thyroxine level and cognitive decline in euthyroid older women. Neurology 58, 1055–1061 (2002). [DOI] [PubMed] [Google Scholar]
- Annerbo S., Wahlund L. O. & Lokk J. The significance of thyroid-stimulating hormone and homocysteine in the development of Alzheimer’s disease in mild cognitive impairment: a 6-year follow-up study. Am. J. Alzheimers Dis. Other Demen. 21, 182–188 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinlan P. et al. Thyroid hormones are associated with poorer cognition in mild cognitive impairment. Dement. Geriatr. Cogn. Disord. 30, 205–211 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suhanov A. V. et al. Risk factors for Alzheimer’s disease in Russia: a case-control study. Eur. J. Neurol. 13, 990–995 (2006). [DOI] [PubMed] [Google Scholar]
- Kalmijn S. et al. Subclinical hyperthyroidism and the risk of dementia. The Rotterdam study. Clin. Endocrinol. (Oxf) 53, 733–737 (2000). [DOI] [PubMed] [Google Scholar]
- Dobert N. et al. Subclinical hyperthyroidism in dementia and correlation of the metabolic index in FDG-PET. Acta Med. Austriaca 30, 130–133 (2003). [PubMed] [Google Scholar]
- Van Osch L. A. D. M., Hogervorst E., Combrinck M. & Smith A. D. Low thyroid-stimulating hormone as an independent risk factor for Alzheimer disease. Neurology 62, 1967–1971 (2004). [DOI] [PubMed] [Google Scholar]
- Hu Y., Wang Z. C., Guo Q. H., Cheng W. & Chen Y. W. Is thyroid status associated with cognitive impairment in elderly patients in China? BMC Endocr. Disord. 16, 11 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annerbo S., Kivipelto M. & Lokk J. A prospective study on the development of alzheimer’s disease with regard to thyroid-stimulating hormone and homocysteine. Dement. Geriatr. Cogn. Disord. 28, 275–280 (2009). [DOI] [PubMed] [Google Scholar]
- Vadiveloo T., Donnan P. T., Cochrane L. & Leese G. P. The Thyroid Epidemiology, Audit, and Research Study (TEARS): morbidity in patients with endogenous subclinical hyperthyroidism. J. Clin. Endocrinol. Metab. 96, 1344–1351 (2011). [DOI] [PubMed] [Google Scholar]
- den Heijer T. et al. Use of hippocampal and amygdalar volumes on magnetic resonance imaging to predict dementia in cognitively intact elderly people. Arch. Gen. Psychiatry 63, 57–62 (2006). [DOI] [PubMed] [Google Scholar]
- Parle J. et al. A randomized controlled trial of the effect of thyroxine replacement on cognitive function in community-living elderly subjects with subclinical hypothyroidism: the Birmingham Elderly Thyroid study. J. Clin. Endocrinol. Metab. 95, 3623–3632 (2010). [DOI] [PubMed] [Google Scholar]
- Jorde R. et al. Neuropsychological function and symptoms in subjects with subclinical hypothyroidism and the effect of thyroxine treatment. J. Clin. Endocrinol. Metab. 91, 145–153 (2006). [DOI] [PubMed] [Google Scholar]
- Chaker L. et al. Thyroid function and the risk of dementia. The Rotterdam Study. Thyroid 25, A3–A4 (2015). [Google Scholar]
- Luo L., Yano N., Mao Q., Jackson I. M. & Stopa E. G. Thyrotropin releasing hormone (TRH) in the hippocampus of Alzheimer patients. J Alzheimers Dis 4, 97–103 (2002). [DOI] [PubMed] [Google Scholar]
- Nussbaum R. L. & Ellis C. E. Alzheimer’s disease and Parkinson’s disease. N. Engl. J. Med. 348, 1356–1364 (2003). [DOI] [PubMed] [Google Scholar]
- Hollowell J. G. et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 87, 489–499 (2002). [DOI] [PubMed] [Google Scholar]
- Taylor P. N. et al. Falling threshold for treatment of borderline elevated thyrotropin levels-balancing benefits and risks: evidence from a large community-based study. JAMA Intern. Med. 174, 32–39 (2014). [DOI] [PubMed] [Google Scholar]
- Stroup D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000). [DOI] [PubMed] [Google Scholar]
- Association Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Revised third Edition. Washington, DC: American Psychiatric Association (1987). [Google Scholar]
- Association Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. DSM-IV. Washington, DC: American Psychiatric Association (1994). [Google Scholar]
- McKhann G. et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34, 939–944 (1984). [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J. & Altman D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R. & Laird N. Meta-analysis in clinical trials. Control. Clin. Trials 7, 177–188 (1986). [DOI] [PubMed] [Google Scholar]
- Mantel N. & Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 22, 719–748 (1959). [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M. & Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.